Abstract
Mental health provider attitudes toward adoption of innovation in general, and toward evidence-based practice (EBP) in particular, are important in considering how best to disseminate and implement EBPs. This article first explores the role of attitudes in acceptance of innovation and proposes a model of organizational and individual factors that may affect or be affected by attitudes toward adoption of EBP. Next, a recently developed measure of mental health provider attitudes toward adoption of EBP is presented along with a summary of preliminary reliability and validity findings. Attitudes toward adoption of EBP are then discussed in regard to provider individual differences and the context of mental health services. Finally, potential applications of attitude research to adoption of EBP are discussed.
Introduction
There is increasing concern that technologies for treating child & adolescent mental health disorders be evidence-based[1][2][3][4][5][6][7]. Evidence-based practices (EBPs) for youths and families are a subset of child & adolescent interventions with empirical support for their efficacy and/or effectiveness and recent definitions include not only scientific rigor, but also clinical judgment and consumer preference[8]. While large scale studies have found that system changes may fail to improve service outcomes[9], interventions with demonstrated efficacy and/or effectiveness hold promise in regard to improving outcomes for youths and families who receive mental health services[10][11][12].
The building momentum in the United States for the dissemination and adoption of EBP in both private and public mental health service settings is bringing pressure on providers to adopt EBP, ready or not. The sources of such pressure for mental health service providers are many including government agencies, mental health authorities, agency directors, health management organizations, insurance companies, supervisors, peers, and consumers[13]. However, little is known about attitudes that may facilitate or impede adoption of EBP among behavioral health service providers.
Invoking attitude change as a way to change behavior has shown promise. For example, in medical settings experiential learning including clinical experience is more effective in changing attitudes compared to didactic learning[14][15]. This parallels marketing studies demonstrating greater attitude change and attitude-behavior consistency for product experience versus advertising alone[16]. The sequencing and affective quality of information provided to change attitudes also needs to be considered. For example, when a large amount of information is to be provided, information that is affectively congruent is best presented early in the sequence[17]. There is a need to refine measurement in order to better understand the relationship of beliefs, attitudes, and behavior[18] and little attention has been given to measurement of mental heath provider attitudes toward adoption of EBP.
In contrast to mechanical innovations and technological innovations such as computer hardware or software, behavioral health service technologies are considered to be “soft” technologies. Soft technologies are especially vulnerable to characteristics of the individual adopter and the implementation context for faithful implementation[10][19]. Individual providers bring their own characteristics including such factors as education, training, beliefs, and personality. The context of mental health services also varies and includes the structures, processes, and procedures of organizations that can affect worker attitudes. Thus, both provider characteristics and organizational context are important in understanding how to effectively move EBPs into real world settings, and attitudes likely play a role.
Attitudes toward organizational change have been shown to be important in the dynamics of innovation[20]. Organizational readiness to change encompasses both structures (e.g., availability of computer resources) and processes (e.g., cohesion, pressure for change) that may be related to attitudes toward adoption of EBPs[21]. One qualitative study in the public sector including stakeholders across organizational levels from agency directors to consumers found multiple factors that impact the acceptability and likelihood of implementation of EBPs in community mental health settings (e.g., perceived fit of the EBP with current practice, organization and staff priorities;[22] and such factors are likely to be associated with attitudes toward adoption of EBPs. The study of attitudes is also important because individual provider attitudes toward adoption of EBPs vary with individual difference factors as well as organizational characteristics[23].
The Role of Attitudes in Models of Innovation Acceptance
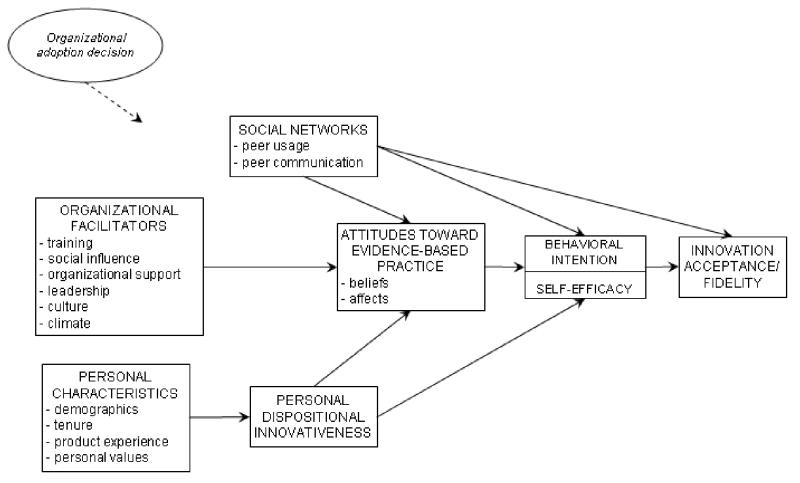
Attitudes toward innovation can be a facilitating or limiting factor in the dissemination and implementation of new technologies[24][25]. Attitudes can be a precursor to the decision of whether or not to try a new practice and the affective component of attitudes can impact decision processes regarding innovation[26][25][27]. The conceptual model in Figure 1 illustrates proposed roles for attitudes in EBP acceptance and provides a useful heuristic in two ways. First, it identifies factors likely to influence attitudes toward EBP. Second, it illustrates the role of attitudes in acceptance of EBP. These factors can increase or decrease the likelihood that new technologies or services will be implemented as intended[25]. As shown in Figure 1, attitudes toward adoption of EBP are proposed to be influenced by organizational facilitators, individual provider characteristics, provider dispositional innovativeness, and social networks. Attitudes are then proposed to be associated with behavioral intentions and self-efficacy, and to affect innovation acceptance and fidelity with which EBPs are applied in practice. The constructs in this heuristic model are now briefly described.
Figure 1.
Conceptual Framework of the Role of Attitudes in Innovation Acceptance and Evidence-Based Practice Implementation in Organizations (adapted from Frambach & Schillewaert, 2002, used with permission from Elsevier)
Organizational Facilitators include training, social influences, organizational support for EBP, leadership, and organizational culture and climate that can increase or decrease the likelihood that new technologies or services will be implemented as intended[25]. Organizational support for innovation has not been well studied in human service agencies but can be defined as the extent to which employees perceive that they are supported in new ideas or in applying innovation[28]. Organizational support is thought to include support for creativity, tolerance of differences, and personal commitment[29].
Leadership affects many aspects of an organization’s environment including overall organizational functioning and team and individual functioning[30]. Leadership is important in effective operation of human service organizations and good leadership is associated with higher levels of service provider organizational commitment and job satisfaction[31][32]. Leadership also influences provider ratings of working alliance in youth mental health programs through its influence on organizational climate[33].
Organizational culture can be defined as the implicit norms, values, shared behavioral expectations, and assumptions that guide behaviors of members of a work unit[34]. Organizational culture can impact how readily new technologies will be considered and adopted in practice[35] and there is concern that public sector service organizations have cultures that are resistant to innovation[36][37]. However, technology transfer may be facilitated by adjusting an implementation plan to the culture of a human service agency[38]. For example, where programs have a conceptual adherence to certain principles of working with clients, new technologies or procedures might be framed as ancillary, rather than a replacement to current technologies being employed. In human services, organizational culture influences provider attitudes, perceptions, and behaviors[39]. Carmazzi and Aarons[40] found that negative organizational culture was associated with providers’ negative attitudes toward adoption of EBP while positive culture was associated with openness to adoption of EBP.
Organizational climate refers to employees’ perceptions and affective responses to their work environment[41][42][43]. Climate includes perceptions of job characteristics (e.g. autonomy, variety, feedback, role clarity) and the work group (e.g. cooperation, warmth/intimacy)[31]. Glisson and Hemmelgarn[44] demonstrated that organizational climate significantly impacted clinical outcomes for youth in publicly funded human services. Aarons and colleagues[33] found that the effect of leadership on working alliance was mediated by organizational climate, and climate for innovation is a factor in human service organizational openness to change[45]. West [46] proposed four factors related to climate for innovation: vision, participative safety, task orientation, and support for innovation[47].
Social influence includes “processes by which individuals are affected by others’ social construction of…events, ideas, objects, and behaviors and are subject to pressure to conform their behavior, attitudes, and beliefs to that social reality”[48] (pgs. 343–344). Four social norms in the workplace are positively associated with group innovation: 1) support for creativity and risk taking 2) teamwork, 3) speed of action, and 4) tolerance of mistakes[49]. Norms within workgroups can be influential in shaping behaviors and this can occur through social processes in organizations. Such social influence norms identify socially acceptable behavior in which adherence to rules provides social approval and rejection avoidance[50]. It follows that agencies with social processes supporting innovation would be more likely to have employees likely to accept variation in work routines tied to EBP.
Personal characteristics include demographic factors such as age, ethnicity, level of education, training, primary discipline, and amount of professional experience. These have been identified as potentially important in adoption of innovation. For example, factors such as level of education and level of professional experience have been found to be associated with attitudes toward adoption of EBP[23].
Personal Dispositional Innovativeness represents an individual’s willingness and desire to experiment with new procedures, new tasks, or new ways of helping clients. While organizational context and demand characteristics can impact staff innovativeness[46] individuals bring with them personality characteristic and behavior patterns. Personal dispositional characteristics of adaptability and willingness to lead change are associated with more positive attitudes toward adoption of EBP[51].
Social networks have to do with both peer use of EBPs and communication about the EBPs. This includes the increase in perceived value and probability of adoption of an innovation as a critical mass of similar or interrelated organizations adopt the innovation[25][52]. It follows that as the number of mental health providers and agencies implementing an EBP increases, and they have a positive experience, attitudes toward the EBP will become more favorable and the probability of additional providers and agencies adopting the EBP should also increase.
Attitudes, along with behavioral intention and self-efficacy, often precede behavior and can predict behavior change[53][54][55][56]. In the heuristic model shown in Figure 1, the effect of attitudes on innovation acceptance and fidelity is associated with behavioral intention and self-efficacy. It is likely, however, that additional factors (e.g., provider conscientiousness) also come into play in determining overall provider effectiveness[57][58].
The way in which innovation acceptance is operationalized varies with the type of innovation. For EBPs, results of effectiveness trials suggest that successful translation of laboratory models into the field depends upon maintaining fidelity to the intervention model. The extent to which an EBP is successful in generating expected outcomes will likely be affected by the degree to which it is implemented correctly as well as by contextual influences[59][60].
As illustrated above and in Figure 1, attitudes are proposed to function in a complex context. For example, studies have shown that organizational culture and climate affect provider work attitudes, service quality, and outcomes[33][44][39]. In addition, organizational context can impact staff attitudes towards innovation[46]. Attitudes are part of a complex interaction of context, beliefs, intentions, and behavior[55]; however, there has been little research to date on identifying provider attitudes toward adoption of EBP. The next section describes proposed domains of attitudes toward adoption of EBP.
Four Proposed Domains of Attitudes toward Adoption of EBP
Four domains of attitudes to adoption of EBP have recently been identified. These include attitudes related to the appeal of an EBP, requirements to adopt an EBP, openness to innovation in general, and perceived divergence between current work processes and those of the EBP.
Appeal of EBP
Studies of persuasion processes and provider self-efficacy support the notion that attitudes and attitude change are sensitive to the information source and the valence or appeal of information[50][61][62]. For example, providers are more at ease with information derived from colleagues in contrast to research articles or books[63][64]. This is important in considering the likely attractiveness of innovations including EBPs[25].
Requirements to Adopt EBP
Attitudes toward requirements to change practice also vary from person to person. For example, a recent study found variability in provider attitudes and compliance with new required assessment practices for using a particular set of standardized measures[65]. While some providers may be more or less compliant with required changes, individual and organizational variability can affect the degree to which innovations are adopted and sustained in practice[19][27].
Openness to Innovation
Openness to change in general has been identified as an important component of workplace climate that can impact innovation in mental health service programs[45]. Openness to innovation is considered an important characteristic of staff in “learning organizations” and such organizations are more responsive and adaptive to contingencies[45][66][67][68]. Personal dispositional innovativeness represents one’s general openness to innovation and willingness to experiment with new technologies[25]. This general openness is akin to the personality characteristic of openness[69]. Provider adaptability is also associated with more positive attitudes toward adoption of EBP[51]. However, general openness to innovation is not conditional on the appeal of an EBP.
Perceived Divergence
Problems in dissemination and implementation of EBP are likely to occur when there is a perceived difference between current and new practices and current practice has a more positive valence. For example, mandated use of evidence-based assessment protocols are often perceived as incongruent or unneeded in clinical practice[65]. Interventions developed in academic or research based settings may be perceived to lack real-world clinical validity and utility. Even where systems are in place to make the use of an EBP relatively seamless there may be perceived divergence.
In order to better understand the role of provider attitudes in adoption of EBP, reliable and valid measures of provider attitudes toward adoption of EBP are needed. The next section describes such a measure and summarizes preliminary findings.
The Evidence-Based Practice Attitude Scale (EBPAS)
The EBPAS is a very brief (15-item) measure that assesses four general attitudes toward adoption of EBP[23]. The development of the scale was based on literature reviews, discussions with providers and researchers, item generation, data collection, and exploratory and confirmatory factor analyses. Reliability and validity analyses were also conducted and are summarized below[23]. The EBPAS and scoring instructions are presented in Appendix 1. Please contact the author for permission to use the EBPAS.
The EBPAS consists of four theoretically derived subscales of attitudes toward adoption of EBP including Appeal, Requirements, Openness, Divergence, and the EBPAS total scale score. The Appeal scale represents the extent to which the provider would adopt an EBP if it were intuitively appealing, could be used correctly, or was being used by colleagues who were happy with it. The Requirements scale assesses the extent to which the provider would adopt an EBP if it were required by an agency, supervisor, or state. The Openness scale assesses the extent to which the provider is generally open to trying new interventions and would be willing to try or use EBPs. The Divergence scale assesses the extent to which the provider perceives EBPs as not clinically useful and less important than clinical experience. The EBPAS total scale score represents one’s global attitude toward adoption of EBP. The overall Cronbach’s alpha reliability for the EBPAS is good (alpha=.77) and subscale alphas range from .90 to .59[23].
Preliminary EBPAS validity analyses suggest that scale scores vary with important provider and organizational characteristics. For example, interns were more likely to score higher on Appeal, Openness, and total EBPAS scales indicating more openness to innovation compared to more experienced professionals. Interns also tended to score lower on the Divergence scale indicating less perceived difference between EBP and usual practice compared to more experienced professionals [23].
Higher educational attainment was associated with higher scores on the EBPAS Appeal dimension. Level of education and intern status overlap and are clearly related, but represent qualitatively different aspects of a mental health provider’s professional developmental trajectory. This relationship suggests that while more professional education is associated with openness to EBPs, professional internships may be an especially opportune stage of a service provider’s professional development in which to introduce and reinforce the value of the use of EBPs[23]. This is congruent with studies showing that during pre-professional status, workers may be particularly predisposed to the acquisition of new practices[70][71][72].
In addition to provider characteristics, organizational characteristics were related to attitudes toward adoption of EBP. For example providers working in differing types of agencies endorsed different levels of attitudes to EBP. In contrast to outpatient clinic providers, providers working in wraparound programs endorsed more open attitudes to adoption of EBP and providers working in case management programs were less open to adoption of EBPs. This suggests that it is important to consider the programmatic context into which EBPs are to be disseminated and implemented[23].
Organizational structure and formalization of clinic procedures should also be considered in regard to their effect on attitudes[73][19]. For example, providers working in mental health programs with low levels of bureaucracy endorsed more positive attitudes to adoption of EBPs. Some programs institute policies regarding interventions to be used for specific problems or disorders. The presence of such policies acquaints providers with a higher degree of procedural specification that is similar to that required by many EBPs. Providers working in programs with formalized practice policies endorsed more positive attitudes toward adoption of EBPs[23]. While this finding may appear discordant with studies reporting that top-down models of imposing new procedures may engender resistance[65], the internal written policies noted here were part of a culture of objectivism in considering how best to match interventions to presenting problems. Given these findings, it will be important to determine if the relationship of provider attitudes, provider characteristics, and organizational characteristics can be better understood in order to facilitate EBP adoption.
Adopter Characteristics and Attitudes to EBP
In regard to adoption of innovation, five groups have been delineated including innovators, early adopters, the early majority, the late majority, and “laggards”[27]. Innovators are those who have curiosity and keen interest in new technologies. Early adopters are more cautious than innovators but are still willing to experiment when a new technology shows promise. The early majority is still more cautious, waiting until some promise of a technology is shown through the experiences of early adopters. The late majority is even more cautious and risk averse, waiting until there is ample evidence that the risks of adopting the technology are low and benefits are evident. Laggards, on the other hand, are unlikely to adopt a new technology unless it is absolutely necessary or an extremely convincing case has been made for adoption. For research on dissemination and implementation of particular EBPs it will likely be important to understand where along the adoption likelihood dimension a behavioral health service provider resides and how to bridge the gap between adopter groups to promote diffusion and adoption of EBP[74].
Measurement of attitudes toward adoption of EBP may provide an index of likelihood of actual adoption and help to generate testable hypotheses. For example, providers scoring high on the EBPAS Appeal and Openness scales might fall into the innovator or early adopter categories. In contrast, those scoring low on the EBPAS Appeal, Openness, and Requirements scales and high on the Divergence scale would likely fall into the late majority or laggard groups. However, as with the study of dissemination and implementation of EBP[75], the measurement of attitudes toward adoption of EBP and application to other models is in its infancy and these hypotheses remain to be tested.
Learning Organizations and Incentives for Change
Evidence-based practice dissemination and implementation efforts should address attitudes of staff and specific operational contexts. Some providers and organizations may be poised to respond to environmental contingencies such as changes in contracting and practice demands, while others may be less flexible in regard to changes in policies or procedures. The notion of the organization as an adaptive system extends the research on learning organizations and holds promise as an explanatory model of change in behavioral health services[76]. The development of a learning organization depends not only on adaptive processes, but also on cultivating positive provider attitudes, and having technology and structure that promotes communication and change.
Future Directions
Evidence-based practices hold the promise of improving a provider’s ability to help clients and patients and to improve cost-effectiveness[10]. To reach providers, marketing strategies that present new interventions as appealing, effective and in demand with colleagues and from consumers may be helpful in promoting positive attitudes toward adopting EBPs. Another likely lever for increasing positive provider attitudes toward adoption of EBPs is the notion that special expertise derived from learning an EBP can improve self-perceptions of professional accomplishment and self-efficacy to effectively work with clients, to gain employment, and to promote one’s practice.
There are a number of areas ripe for research on the contribution of attitudes to DI of EBPs. It will be important to identify additional factors associated with improving attitudes toward adoption of EBPs. Such factors include identifying those who are most likely to seek out and use EBPs and addressing concerns of those who are not. Researchers often perceive EBPs as necessary for effective service delivery, but providers may be more reserved and cautious about what it means to adopt a new practice[65]. While frequently juggling overwhelming clinical and administrative responsibilities, taking on new and different job tasks may be seen as a difficult endeavor with questionable rewards. The impact of mental health clinic culture and climate on attitudes toward EBP should be considered[39]. For example, an organizational culture that engenders negative attitudes to change suggests the need to address resistance not only to EBP but to organizational change in general. Including staff in discussions about changes in practice and how EBP is congruent with current approaches may decrease perceived divergence between current and new practice and facilitate change[68].
Little is known regarding the interaction of organizational characteristics and provider characteristics when an EBP is implemented. For example, organizational culture provides norms for behavior within an organization. If attitudes toward adoption of EBP are weak and culture is strong, then the effect of culture may overpower attitudes. However, strong attitudes can be congruent or incongruent with organizational norms[77]. To the degree that attitudes toward adoption of EBP are at odds with organizational norms and proposed organizational change, staff may perceive the climate as stressful and poor work attitudes, poor job performance, and staff turnover may result[78][79]. This is just one example of how organizational and individual factors can interact and more study of such factors is needed.
The effectiveness of implementation efforts will likely be impacted by provider attitudes toward EBP, the specific type of EBP, organizational climate for innovation, and the fit between personal values and those of the organization. This “innovation-values fit” can be maximized by providing a strong implementation climate, ensuring skill in the innovation, providing incentives for its use, and removing obstacles to use of the innovation[80]. An organization can provide incentives for employees through praise, encouragement by supervisors, and the provision of tangible and valued rewards[28]. Obstacles can be removed by including participative decision making about the innovation, allowing ample time for learning about the innovation, and responding to questions and complaints about the innovation by employees[28][80]. A good innovation-values fit can also be facilitated through strong commitment to and support of the innovation by the organization, communication and information sharing throughout the organization, the inclusion of “champions” or respected individuals who actively promote the innovation, and the existence of a strong social network that allows for increased positive interaction between employees[28][25][81].
To promote diffusion of EBP, strategies from marketing and organizational literatures could be considered. Innovators and early adopters are more likely to have positive attitudes toward innovation and to be less concerned with how current behaviors diverge from those required for the new technology[74]. Innovators and early adopters of EBPs could be encouraged to communicate with other more reticent mental health professionals. Indeed, more attention should be given to bridging the gap between adopter groups[74][27]. In particular, the communication and spread of enthusiasm and positive experiences of innovators and early adopters could be facilitated. The most effective means by which such communication takes place should be identified and exploited. Identification of factors that promote or inhibit adoption of EBP will improve our ability to tailor implementation efforts to the characteristics and needs of specific mental health service providers and organizations.
The degree to which provider attitudes toward adoption of EBP are important in models of DI remains to be tested. However, the long history of attitudes as a factor in behavior change suggests that they will contribute to understanding and improving the EBP DI process. For the present, models of DI should include attitudes as one factor that may influence EBP acceptance, fidelity, and outcomes.
Acknowledgments
Author Note
This work was supported by National Institute of Mental Health Grant number MH01695. The author thanks the program managers, clinicians, and case managers who participated in the scale development study.
Appendix 1: Evidence-Based Practice Attitude Scale Items and Scoring Instructions[23]
Instructions
The following questions ask about your feelings about using new types of therapy, interventions, or treatments. Manualized therapy, treatment, or intervention refers to any intervention that has specific guidelines and/or components that are outlined in a manual and/or that are to be followed in a structured or predetermined way. Indicate the extent to which you agree with each item using the following scale:
| 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Not at All | To a Slight Extent | To a Moderate Extent | To a Great Extent | To a Very Great Extent |
| Item | Subscale | Question |
|---|---|---|
| 1. | 3 | I like to use new types of therapy/interventions to help my clients. |
| 2. | 3 | I am willing to try new types of therapy/interventions even if I have to follow a treatment manual. |
| 3. | 4 | I know better than academic researchers how to care for my clients. |
| 4. | 3 | I am willing to use new and different types of therapy/interventions developed by researchers. |
| 5. | 4 | Research based treatments/interventions are not clinically useful. |
| 6. | 4 | Clinical experience is more important than using manualized therapy/interventions. |
| 7. | 4 | I would not use manualized therapy/interventions. |
| 8. | 3 | I would try a new therapy/intervention even if it were very different from what I am used to doing. |
| For questions 9–15: If you received training in a therapy or intervention that was new to you, how likely would you be to adopt it if: | ||
| 9. | 2 | it was intuitively appealing? |
| 10. | 2 | it “made sense” to you? |
| 11. | 1 | it was required by your supervisor? |
| 12. | 1 | it was required by your agency? |
| 13. | 1 | it was required by your state? |
| 14. | 2 | it was being used by colleagues who were happy with it? |
| 15. | 2 | you felt you had enough training to use it correctly? |
Note: Subscale 1 = Requirements; 2 = Appeal; 3 = Openness; 4 = Divergence.
Scoring the Subscales
The score for each subscale is created by computing a mean score for the items that load on a given subscale. For example, items 11, 12, and 13 constitute subscale 1.
Computing the Total Scale Score
For the total score, all items from the Divergence subscale (Subscale 4) must be reverse scored before being used in computing the overall EBPAS mean score.
Please contact the author for permission to use the EBPAS and for more detailed instructions.
References
- 1.Hebert R. NIMH strategies for moving evidence-based mental illness treatments from laboratory to real-world therapies. Observer. 2003;16:21–4. [Google Scholar]
- 2.Hoagwood K, Olin S. The NIMH blueprint for change report: research priorities in child and adolescent mental health. J Am Acad Child Adolesc Psychiatry. 2002;41:760–7. doi: 10.1097/00004583-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Jensen PS. Commentary: the next generation is overdue. J Am Acad Child Adolesc Psychiatry. 2003;42:527–30. doi: 10.1097/01.CHI.0000046837.90931.A0. [DOI] [PubMed] [Google Scholar]
- 4.Kazdin AE, Weisz JR. Identifying and developing empirically supported child and adolescent treatments. J Consult Clin Psychol. 1998;66:19–36. doi: 10.1037//0022-006x.66.1.19. [DOI] [PubMed] [Google Scholar]
- 5.National Institute of Mental Health. Bridging science and service. Bethesda, MD: National Institutes of Health; 1999(No. 99–4353).
- 6.National Institute of Mental Health. What Do We Know About Implementing Evidence-Based Practices (EBPs) and Where Can We Go From Here? Baltimore, MD: 2002.
- 7.National Institute of Mental Health. Translating behavioral science into action: report of the national advisory mental health council behavioral science workgroup. Bethesda, MD: National Institutes of Health; 2000(No. 00–4699).
- 8.Institute of Medicine. Institute of Medicine Committee on the Quality of Health Care in America. Crossing the Quality Chasm: a New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
- 9.Bickman L. The evaluation of a children’s mental health managed care demonstration. J Ment Health Adm. 1996;23:7–15. doi: 10.1007/BF02518639. [DOI] [PubMed] [Google Scholar]
- 10.Barnoski R. Outcome Evaluation of Washington State’s Research-Based Programs for Juvenile Offenders. Olympia, WA: Washington State Institute for Public Policy; 2004.
- 11.Burns BJ. Children and evidence-based practice. Psychiatr Clin North Am. 2003;26:955–70. doi: 10.1016/s0193-953x(03)00071-6. [DOI] [PubMed] [Google Scholar]
- 12.Hoagwood K, Burns BJ, Kiser L, Ringeisen H, Schoenwald SK. Evidence-based practice in child and adolescent mental health services. Psychiatr Serv. 2001;52:1179–89. doi: 10.1176/appi.ps.52.9.1179. [DOI] [PubMed] [Google Scholar]
- 13.Essock SM, Goldman HH, Van Tosh L, et al. Evidence-based practices: setting the context and responding to concerns. Psychiatr Clin North Am. 2003;26:919–38. doi: 10.1016/s0193-953x(03)00069-8. [DOI] [PubMed] [Google Scholar]
- 14.Peters AS, Schimpfhauser FT, Cheng J, Daly SL, et al. Effect of a course in cancer prevention on students’ attitudes and clinical behavior. J Med Educ. 1987;62:592–600. doi: 10.1097/00001888-198707000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Warburg MM, Cleary PD, Rohman ME, Barnes HN, et al. Residents’ attitudes, knowledge, and behavior regarding diagnosis and treatment of alcoholism. J Med Educ. 1987;62:497–503. doi: 10.1097/00001888-198706000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Smith RE, Swinyard WR. Attitude-behavior consistency: the impact of product trial versus advertising. Journal of Marketing Research. 1983;20:257–67. [Google Scholar]
- 17.Jacoby J, Morrin M, Jaccard J, Gurhan Z, Kuss A, Maheswaran D. Mapping attitude formation as a function of information input: online processing models of attitude formation. Journal of Consumer Psychology. 2002;12:21–34. [Google Scholar]
- 18.Jaccard J, Radecki C, Wilson T, Dittus P. Methods for identifying consequential beliefs: implications for understanding attitude strength. In: Petty RE, Krosnick JA, editors. Attitude strength: antecedents and consequences. Ohio State University Series on Attitudes and Persuasion. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc. 1995;4:337–59. [Google Scholar]
- 19.Glisson C. The organizational context of children’s mental health services. Clin Child Fam Psychol Rev. 2002;5:233–53. doi: 10.1023/a:1020972906177. [DOI] [PubMed] [Google Scholar]
- 20.Dunham RB, Grube JA, Gardner DG, Pierce JL. The development of an attitude toward change instrument. 49th Annual Meeting of the Academy of Management: Washington, D. C.: 1989.
- 21.Lehman WEK, Greener JM, Simpson DD. Assessing organizational readiness for change. J Subst Abuse Treat. 2002;22:197–209. doi: 10.1016/s0740-5472(02)00233-7. [DOI] [PubMed] [Google Scholar]
- 22.Hurlburt M, Knapp P. The new consumers of evidence-based practices: reflections of providers and families. National Technical Assistance Center for Children’s Mental Health; Georgetown University Center for Child and Human Development; 2003 (Special Issue #6) p. 21–23.
- 23.Aarons GA. Mental health provider attitudes toward adoption of evidence-based practice: the Evidence-Based Practice Attitude Scale. Ment Health Serv Res. 2004;6:61–72. doi: 10.1023/b:mhsr.0000024351.12294.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Damanpour F. Organizational innovation: a meta-analysis of effects of determinants and moderators. Acad Manage J. 1991;34:555–90. [Google Scholar]
- 25.Frambach RT, Schillewaert N. Organizational innovation adoption: a multi-level framework of determinants and opportunities for future research. Journal of Business Research Special Issue: Marketing Theory in the Next Millennium. 2002;55:163–76. [Google Scholar]
- 26.Candel MJJM, Pennings JME. Attitude-based models for binary choices: a test for choices involving an innovation. Journal of Economic Psychology. 1999;20:547–69. [Google Scholar]
- 27.Rogers EM. Diffusion of Innovations, 4th edition. New York: The Free Press; 1995.
- 28.Ash J. Organizational factors that influence information technology diffusion in academic health sciences centers. J Am Med Inform Assoc. 1997;4:102–11. doi: 10.1136/jamia.1997.0040102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Siegel SM, Kaemmerer WF. Measuring the perceived support for innovation in organizations. J Appl Psychol. 1978;63:553–62. [Google Scholar]
- 30.Bass BM, Avolio BJ, Jung DI, Berson Y. Predicting unit performance by assessing transformational and transactional leadership. J Appl Psychol. 2003;88:207–18. doi: 10.1037/0021-9010.88.2.207. [DOI] [PubMed] [Google Scholar]
- 31.Glisson C. The effect of leadership on workers in human service organizations. Adm Soc Work. 1989;13:99–116. [Google Scholar]
- 32.Glisson C, Durick M. Predictors of job satisfaction and organizational commitment in human service organizations. Adm Sci Q. 1988;33:61–81. [Google Scholar]
- 33.Aarons GA, Woodbridge M, Carmazzi A. Examining leadership, organizational climate and service quality in a children’s system of care. In: Proceedings of the 15th Annual Research Conference. A System of Care for Children’s Mental Health: Examining the Research Base. Tampa, FL: 2003, p. 15–18.
- 34.Cooke RA, Rousseau DM. Behavioral norms and expectations: a quantitative approach to the assessment of organizational culture. Group & Organization Studies. 1988;13:245–73. [Google Scholar]
- 35.Hemmelgarn AL, Glisson C, Dukes D. Emergency room culture and the emotional support component of family-centered care. Child Health Care. 2001;30:93–110. [Google Scholar]
- 36.Backer TE, David SL, Soucy GE, editors. Reviewing the Behavioral Science Knowledge Base on Technology Transfer (NIDA Research Monograph 155, NIH Publication No. 95–4035). Rockville, MD: National Institute on Drug Abuse; 1995. [PubMed]
- 37.Diamond MA. Innovation and diffusion of technology: a human process. Consulting Psychology Journal: Practice & Research. 1996;48:221–9. [Google Scholar]
- 38.Keller DS, Galanter M. Technology transfer of network therapy to community-based addictions counselors. J Subst Abuse Treat. 1999;16:183–9. doi: 10.1016/s0740-5472(98)00044-0. [DOI] [PubMed] [Google Scholar]
- 39.Glisson C, James LR. The cross-level effects of culture and climate in human service teams. Journal of Organizational Behavior. 2002;23:767–94. [Google Scholar]
- 40.Carmazzi A, Aarons GA. Organizational culture and attitudes toward adoption of evidence-based practice. Presented at the NAMSHPD Research Institute’s 2003 Conference on State Mental Health Agency Services Research, Program Evaluation, and Policy. Baltimore, MD:2003.
- 41.Joyce WF, Slocum JW. Climate discrepancy: refining the concepts of psychological and organizational climate. Human Relations. 1982;35:951–71. [Google Scholar]
- 42.Sells SB, James LR. Organizational climate. In: Nesselroade JR, Cattell, RB, editors. Handbook of Multivariate Experimental Psychology. Perspectives on Individual Differences, 2nd edition. New York: Plenum Press; 1988:915–37.
- 43.Srivastava SK, Bathla A. Correlational study of organizational climate and work adjustment among industrial workers. Social Science International. 1996;12:52–60. [Google Scholar]
- 44.Glisson C, Hemmelgarn A. The effects of organizational climate and interorganizational coordination on the quality and outcomes of children’s service systems. Child Abuse Negl. 1998;22:401–21. doi: 10.1016/s0145-2134(98)00005-2. [DOI] [PubMed] [Google Scholar]
- 45.Anderson NR, West MA. Measuring climate for work group innovation: development and validation of the Team Climate Inventory. Journal of Organizational Behavior. 1998;19:235–58. [Google Scholar]
- 46.West MA. The social psychology of innovation in groups. In: West MA, Farr JL, editors. Innovation and creativity at work: psychological and organizational strategies. Oxford, England: John Wiley & Sons; 1990:309–33.
- 47.West MA, Anderson NR. Innovation in top management teams. J Appl Psychol. 1996;81:680–93. [Google Scholar]
- 48.Lewis LK, Seibold DR. Innovation modification during intraorganizational adoption. Acad Manage Rev. 1993;18:322–54. [Google Scholar]
- 49.O’Reilly CA, Caldwell DF. The impact of normative social influence and cohesiveness on task perceptions and attitudes: a social information processing approach. Journal of Occupational Psychology. 1985;58:193–206. [Google Scholar]
- 50.Cialdini RB, Bator RJ, Guadagno RE. Normative influences in organizations. In: Thompson LL, Levine JM, Messick DM, editors. Shared cognition in organizations: the management of knowledge. Mahwah, New Jersey: Lawrence Erlbaum Associates; 1999:195–211.
- 51.Aarons GA. Service worker attitudes toward adoption of empirically supported treatments. Paper Presented at the NASMHPD Research Institute’s 2003 Conference on State Mental Health Agency Services Research, Program Evaluation, and Policy. Baltimore, MD: 2003.
- 52.Kraut RE, Rice RE, Cool C, Fish RS. Varieties of social influence: the role of utility and norms in the success of a new communication medium. Organization Science. 1998;9:437–53. [Google Scholar]
- 53.Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982:37. [Google Scholar]
- 54.Bandura A. Growing primacy of human agency in adaptation and change in the electronic era. European Psychologist. 2002;7:2–16. [Google Scholar]
- 55.Fishbein M, Azjen I. Belief, attitude, intentions, and behavior: an introduction to theory and research. Reading, MA: Addison-Wesley; 1975.
- 56.Fishbein M, Hennessy M, Yzer M, Douglas J. Can we explain why some people do and some people do not act on their intentions? Psychology, Health & Medicine. 2003;8:3–18. doi: 10.1080/1354850021000059223. [DOI] [PubMed] [Google Scholar]
- 57.Mount MK, Barrick MR, Stewart GL. Five-Factor Model of personality and performance in jobs involving interpersonal interactions. Human Performance. 1998;11:145–65. [Google Scholar]
- 58.Witt L, Burke L, Barrick M, Mount M. The interactive effects of conscientiousness and agreeableness on job performance. J Appl Psychol. 2002;87:164–9. doi: 10.1037/0021-9010.87.1.164. [DOI] [PubMed] [Google Scholar]
- 59.Detrich R. Increasing treatment fidelity by matching interventions to contextual variables within the educational setting. School Psychology Review. 1999;28:608–20. [Google Scholar]
- 60.Schoenwald SK, Henggeler SW, Brondino MJ, Rowland MD. Multisystemic therapy: monitoring treatment fidelity. Fam Process. 2000;39:83–103. doi: 10.1111/j.1545-5300.2000.39109.x. [DOI] [PubMed] [Google Scholar]
- 61.Tormala ZL, Petty RE. What doesn’t kill me makes me stronger: the effects of resisting persuasion on attitude certainty. J Pers Soc Psychol. 2002;83:1298–1313. doi: 10.1037//0022-3514.83.6.1298. [DOI] [PubMed] [Google Scholar]
- 62.Watkins M. Principles of persuasion. Negotiation Journal. 2001;17:115–37. [Google Scholar]
- 63.Cohen L, Sargent M, Sechrest L. Use of psychotherapy research by professional psychologists. Am Psychol. 1986;41:198–206. doi: 10.1037//0003-066x.41.2.198. [DOI] [PubMed] [Google Scholar]
- 64.Morrow-Bradley C, Elliott R. Utilization of psychotherapy research by practicing psychotherapists. Am Psychol. 1986;41:188–97. doi: 10.1037//0003-066x.41.2.188. [DOI] [PubMed] [Google Scholar]
- 65.Garland AF, Kruse M, Aarons GA. Clinicians and outcome measurement: what’s the use? J Behav Health Serv Res. 2003;30:393–405. doi: 10.1007/BF02287427. [DOI] [PubMed] [Google Scholar]
- 66.Birleson P. Turning child and adolescent mental-health services into learning organizations. Clinical Child Psychology & Psychiatry. 1999;4:265–74. [Google Scholar]
- 67.Fiol CM, Lyles MA. Organizational learning. Acad Manage Rev. 1985;10:803–13. [Google Scholar]
- 68.Garvin DA. Building a learning organization. Harv Bus Rev. 1993;71:78–91. [PubMed] [Google Scholar]
- 69.McCrae RR, Costa PT. Validation of the five-factor model of personality across instruments and observers. J Pers Soc Psychol. 1987;52:81–90. doi: 10.1037//0022-3514.52.1.81. [DOI] [PubMed] [Google Scholar]
- 70.Day E, Arthur W, Gettman D. Knowledge structures and the acquisition of a complex skill. J Appl Psychol. 2001;86:1022–33. doi: 10.1037/0021-9010.86.5.1022. [DOI] [PubMed] [Google Scholar]
- 71.Klimoski R, Mohammed S. Team mental model: construct or metaphor? Journal of Management. 1994;20:403–37. [Google Scholar]
- 72.Rentsch JR, Klimoski RJ. Why do ‘great minds’ think alike?: antecedents of team member schema agreement. Journal of Organizational Behavior Special Issue: Shared Cognition. 2001;22:107–20. [Google Scholar]
- 73.Glisson C. Structure and technology in human service organizations. In: Hasenfeld Y, editor. Human services as complex organizations. Thousand Oaks, CA: Sage Publications, Inc.; 1992:184–202.
- 74.Moore GA. Crossing the chasm: marketing and selling high-tech products to mainstream customers. New York: HarperCollins Publishers Inc.; 2002.
- 75.Schoenwald SK, Sheidow AJ, Letourneau EJ, Liao JG. Transportability of multisystemic therapy: evidence for multilevel influences. Ment Health Serv Res. 2003;5:223–39. doi: 10.1023/a:1026229102151. [DOI] [PubMed] [Google Scholar]
- 76.Jankowicz D. From “learning organization” to “adaptive organization. Management Learning. 2000;31:471–90. [Google Scholar]
- 77.Harris SG, Mossholder KW. The affective implications of perceived congruence with culture dimensions during organizational transformation. Journal of Management. 1996;22:527–47. [Google Scholar]
- 78.Baron JN, Hannan MT, Burton MD. Labor pains: change in organizational models and employee turnover in young, high-tech firms. American Journal of Sociology. 2001;106:960–1012. [Google Scholar]
- 79.Gill S, Greenberg MT, Vazquez A. Changes in the service delivery model and home visitors’ job satisfaction and turnover in an Early Head Start program. Infant Mental Health Journal Special Issue: Early Head Start. 2002;23:182–96. [Google Scholar]
- 80.Klein KJ, Sorra JS. The challenge of innovation implementation. Acad Manage Rev. 1996;21:1055–80. [Google Scholar]
- 81.Pullig C, Maxham JGI, Hair JF., Jr Salesforce automation systems: an exploratory examination of organizational factors associated with effective implementation and salesforce productivity. Journal of Business Research Special Issue: Marketing Productivity. 2002;55:401–15. [Google Scholar]