Abstract
The obligate intracellular pathogen Leishmania major survives and multiplies in professional phagocytes. The evasion strategy to circumvent killing by host phagocytes and establish a productive infection is poorly understood. Here we report that the virulent inoculum of Leishmania promastigotes contains a high ratio of annexin A5-binding apoptotic parasites. This subpopulation of parasites is characterized by a round body shape, a swollen kinetoplast, nuclear condensation, and a lack of multiplication and represents dying or already dead parasites. After depleting the apoptotic parasites from a virulent population, Leishmania do not survive in phagocytes in vitro and lose their disease-inducing ability in vivo. TGF-β induced by apoptotic parasites is likely to mediate the silencing of phagocytes and lead to survival of infectious Leishmania populations. The data demonstrate that apoptotic promastigotes, in an altruistic way, enable the intracellular survival of the viable parasites.
Keywords: apoptosis, immune evasion, neutrophils, parasitic, protozoan, phosphatidyl serine
Leishmaniasis is caused by the cutaneous infection with promastigotes of the genus Leishmania upon the bite of an infected sandfly. In the sandfly midgut, two developmental stages, termed procyclic and metacyclic parasites, have been defined (1). Procyclic stage parasites attach to the epithelial cells of the midgut and have a low virulence. Metacyclic stage parasites are the virulent and disease-inducing form of Leishmania. Because peanut agglutinin (PNA) agglutinates preferentially procyclic but not metacyclic promastigotes, agglutination with PNA can be used to separate procyclic from metacyclic populations (2). Differences in the structure of the surface lipophosphoglycan (LPG) were shown to be the basis for the differential PNA binding of procyclic and metacyclic parasites. Consequently, LPG was suggested as an important virulence factor of Leishmania (3). In vitro development of virulent Leishmania promastigotes is characterized by two growth stages (1). In the logarithmic growth phase (log. phase), parasites have a low virulence; in the later stationary growth phase (stat. phase), parasites exert a high disease-developing potential. The high virulence of stat. phase parasites was attributed to the high ratio of metacyclic parasites in this growth phase (1).
In the mammalian hosts, Leishmania are obligate intracellular pathogens, preferring phagocytes as host cells. The first phagocytic cells that infiltrate the s.c. site of experimental infection with L. major promastigotes are polymorphonuclear neutrophil granulocytes (PMN), followed by a wave of macrophages (MF; ref. 4). PMN serve as intermediate host cells immediately after infection (5, 6). Inside PMN, L. major remain in the promastigote stage without multiplication (6). Subsequently, promastigotes use apoptotic PMN as a Trojan horse for silent entry into its final host, the MF (6). The prerequisite of survival in these professional phagocytes, however, is the inhibition of antimicrobial effector mechanisms. Because various LPG mutants or complete LPG-deficient promastigotes are still able to infect MF and survive intracellularly (7), molecules other than LPG must be involved in silencing the phagocyte defense systems.
The best-characterized example of an immune-silencing phagocytotic process is the uptake of apoptotic cells (8, 9). Phagocyte functions are suppressed by the recognition of phosphatidylserine (PS) on the membrane of apoptotic cells. This step is characterized by the release of antiinflammatory cytokines such as TGF-β and IL-10 and down-regulation of the proinflammatory cytokine TNF-α. Consequently, recognition of PS prevents immune responses against abundantly internalized and processed proteins of the apoptotic remains (10, 11). A common method of detecting PS on a cell surface is the use of the PS-binding protein annexin A5 (AnxA5). AnxA5 binds in a Ca2+-dependent manner with anionic phospholipids present in membranes of apoptotic cells. AnxA5 binds with high affinity to PS (12). A recent study demonstrated that, in addition to AnxA5, serum protein S specifically binds PS. Protein S acts by binding with its glutamic acid-rich positively charged N terminus to the negatively charged PS in a Ca2+-dependent manner (13, 14). Moreover, a mAb was developed recognizing PS (15). Interestingly, recent in vivo experiments showed disease exacerbation when Leishmania were injected together with apoptotic cells. This disease-promoting effect was found to depend on PS recognition and TGF-β production by MF (16).
L. major possesses its own apoptotic program involving cysteine proteinase activation, mitochondrion permeabilization, and DNA degradation (17). This process is initiated in stat. phase cultures of promastigotes (18). Data on PS expression as the early sign of apoptosis on Leishmania are inconclusive. One study demonstrates that a parasite mutant lacking ether phospholipids (alkyl-acyl-bound phospholipids species) was still able to silence MF and survive intracellularly (19). This study does not, however, exclude the presence of other PS-containing lipids, such as lyso-acyl or diacyl-bound PS species on apoptotic Leishmania. At the same time, it was hypothesized that PS-positive amastigotes use PS as a form of apoptotic mimicry. Data suggested that Leishmania amastigotes can express PS on their outer membrane leaflet without subsequent apoptotic death. PS-positive amastigotes induced TGF-β and IL-10 production by murine MF (20). However, this study does not exclude the possibility that PS-positive amastigotes bear other apoptotic markers such as DNA degradation and in fact are dying because of apoptosis. Moreover, it was suggested that Leishmania tropica promastigotes uniformly express PS in their stat. phase (21). This study, however, lacks a control where the Leishmania promastigotes were incubated with AnxA5 in the absence of Ca2+. Therefore, nonspecific AnxA5 binding cannot be excluded.
In the present study, we investigated PS appearance on the disease-inducing promastigote form of L. major. We observed that in both the in vitro culture and the sandfly vector, infectious Leishmania populations contain AnxA5-positive (AnxA5+) parasites. The AnxA5+ promastigotes were found to be apoptotic, and in vivo, in a cutaneous infection model, disease development was found to depend on the presence of apoptotic parasites. AnxA5+ promastigotes were able to silence effector functions of the first host cell for promastigotes, human PMN, enabling the intracellular survival of nonapoptotic parasites in vitro. These data suggest that the presence of apoptotic Leishmania is crucial for both disease development and survival of the parasite as a population.
Results
Infective L. major Populations from in Vitro Cultures and from Sandflies Harbor AnxA5+ Promastigotes.
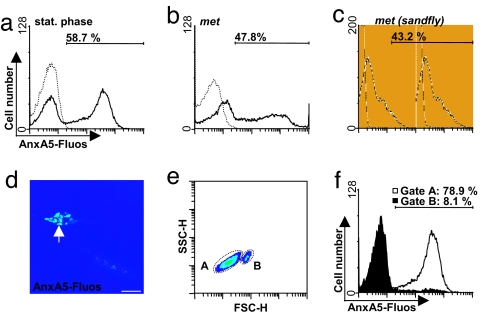
To study the presence of PS on the surface, L. major promastigotes in the stat. growth phase were stained with AnxA5-Fluos. Quantitative analysis by using flow cytometry showed that >50% (58.7 ± 6%) of the stat. phase parasites bound AnxA5 on their surface (Fig. 1a). Metacyclic promastigotes were purified from stat. phase cultures (22). Interestingly, almost 50% of metacyclic parasites were AnxA5+ (Fig. 1b). The different shape curves in Fig. 1 a–c reflect PNA removal of noninfectious parasites. To investigate whether AnxA5+ Leishmania are relevant for disease development after natural infection, we checked whether metacyclic populations in sandflies contain AnxA5+ parasites. We could demonstrate that the infectious metacyclic parasites purified from the midgut of infected Phlebotomus duboscqi sandflies contain a major population of AnxA5+ parasites. The ratio of AnxA5+ parasites in the sandfly was similar to that of stat. phase promastigotes grown in vitro and to that of metacyclic promastigotes (Fig. 1c).
Fig. 1.
AnxA5 binding to L. major promastigotes. Populations of L. major promastigotes were stained with AnxA5-Fluos. Flow cytometry histogram profiles of stat. phase promastigotes (black line, a) and of stat. phase-derived metacyclic promastigotes (met, black line, b). The dotted lines (a and b) show the control staining in the absence of Ca2+. (c) Metacyclic promastigotes derived from P. duboscqi sandflies (black line) as described (22). The dotted line shows the unstained control. (d) Confocal micrograph (0.15-μM slice) of a promastigote-stained positive with AnxA5 (arrow) and an AnxA5− promastigote. (Scale bar, 5 μm.) (e) Flow cytometry densitoblot showing forward scatter (FSC-H) and sideward scatter (SSC-H) analysis of the stat. phase promastigotes. (f) AnxA5-Fluos binding of the population A in e (white histogram) and population B in e (filled histogram).
Fluorescence microscopy confirmed that a major population of the stat. phase parasites was AnxA5+ (Fig. 1d). Similar to apoptotic cells (23), a patched staining pattern was observed (Fig. 1d). AnxA5+ parasites had a round body shape as compared to the elongated shape of AnxA5-negative (AnxA5−) promastigotes (Fig. 1d). Size measurement of the stat. phase parasites with flow cytometry revealed two parasite populations, a population of smaller (Fig. 1e, gate A) and a population of larger (Fig. 1e, gate B) promastigotes. Whereas most of the smaller parasites (gate A in Fig. 1e) were AnxA5+, the larger promastigotes (gate B in Fig. 1e) were AnxA5−. This finding corresponds to the microscopical observation showing that the AnxA5+ parasites are smaller, whereas the AnxA5− ones have an elongated body shape. The specificity of the AnxA5 staining was confirmed by the lack of binding in the absence of Ca2+ (Fig. 1a). Because AnxA5 can also bind anionic phospholipids other then PS, we used additional markers described to recognize PS. Staining with protein S and a PS-specific mAb confirmed our AnxA5 data, demonstrating that round body-shaped promastigotes were PS-positive (Fig. 7, which is published as supporting information on the PNAS web site). Protein S binding to promastigotes was Ca2+-dependent and could be blocked with antibodies directed against the phospholipid-binding domain of protein S (data not shown; ref. 14). Even though our data strongly suggest that a subpopulation of virulent promastigotes cultures expresses PS, we cannot exclude the possibility that AnxA5 and protein S bind another anionic phospholipid. Therefore, we termed these parasites AnxA5+.
AnxA5+ L. major Promastigotes Are Apoptotic.
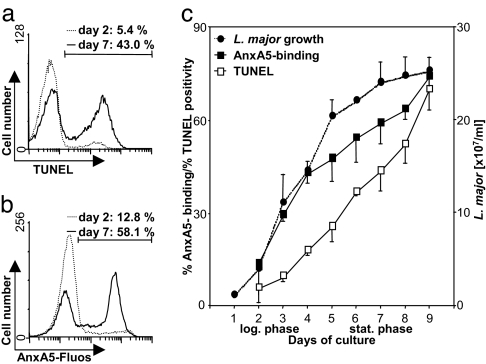
In a previous study, the appearance of PS on the surface of Leishmania amastigotes was observed without any other sign of apoptosis (20). Based on this finding, it was suggested that Leishmania use “apoptotic mimicry” as an evasion mechanism. The TUNEL assay was used to assess nuclear DNA fragmentation, a sign of late apoptosis, in AnxA5+ L. major promastigotes. Flow cytometry analysis revealed that 43.0 ± 6% of stat. phase parasites were TUNEL+ (Fig. 2a). Most TUNEL+ parasites were found in the population of AnxA5+ smaller promastigotes (gate A in Fig. 1e; data not shown). Therefore, most AnxA5+ parasites are also TUNEL+, i.e., apoptotic.
Fig. 2.
TUNEL and AnxA5 staining of L. major promastigotes in the log. and stat. growth phases. Parasites were stained with the TUNEL method (a) or by using AnxA5-Fluos (b) and analyzed with flow cytometry. The histogram profiles of early log. phase (dotted line) and stat. phase (black line) parasites are shown. (c) Parasite growth (dotted line) and percentage of AnxA5+ (black line, filled squares) and TUNEL+ promastigotes (black line, open squares) during the course of in vitro parasite growth. The histograms are representative for four independent experiments. Data of four independent experiments are depicted as mean ± SD.
The Ratio of AnxA5+ Apoptotic Parasites Correlates with the Virulence of L. major Populations.
We compared the ratio of AnxA5+ apoptotic parasites in early log. phase (day 2) and stat. phase (day 7) cultures. Whereas >50% of stat. phase parasites were AnxA5+, in the early log. phase, only (13.2 ± 2%) of the parasites expressed PS on their surface (Fig. 2b). TUNEL staining had similar results. As compared to the high (43.0 ± 6%) rate of TUNEL+ parasites in the stat. growth phase, solely 5.4 ± 2% of promastigotes in the early log. growth phase were TUNEL+ (Fig. 2a). The rate of apoptosis, characterized by both PS expression and TUNEL positivity, increases during in vitro culture (Fig. 2c) and therefore correlates with the virulence of the parasites.
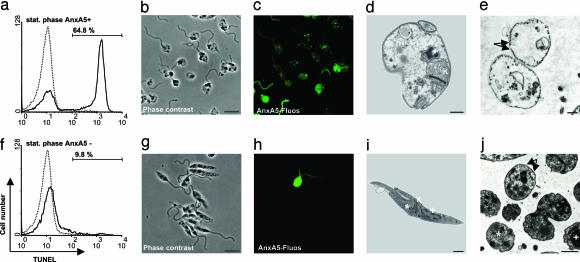
Apoptotic Promastigotes Have an Aberrant Morphology and Are Not Able to Multiply.
To investigate the features of AnxA5+ vs. AnxA5− parasites, an AnxA5-based magnetic cell sorting (MACS)-sorting technique was developed to separate AnxA5+ from AnxA5− promastigotes in a population of stat. phase parasites that contained 58.7 ± 6% AnxA5+ parasites. Using this method, a 94 ± 2% (n = 4) AnxA5+ population was obtained. The AnxA5− population contained as low as 7 ± 2% (n = 4) AnxA5+ parasites. Purified AnxA5+ promastigotes (65% ± 9%, n = 4) were TUNEL+ (Fig. 3a). DNA staining using Syto-16 (0.1 μM, Molecular Probes, Eugene, OR) revealed that approximately one-third of the AnxA5+ promastigotes do not contain DNA (data not shown). We suggest that these “ghosts” represent parasites at a late stage of apoptosis, where the fragmentation of nuclear DNA reached a level where DNA can no longer be stained in the cell. These “ghosts,” in the absence of DNA, do not appear as TUNEL+. That 65% of the AnxA5+ promastigotes are TUNEL+ and the remaining one-third are “ghosts” indicates all of the AnxA5+ parasites are apoptotic. In comparison, only 10 ± 2% (n = 4) of purified AnxA5− promastigotes were TUNEL+ (Fig. 3f). All AnxA5− promastigotes stained DNA-positive (data not shown). Fluorescence microscopy confirmed that promastigotes in the AnxA5+ population had a round body shape and patchy AnxA5 staining (Fig. 3 b and c), whereas the AnxA5− population contained parasites with an elongated body shape (Fig. 3 g and h). Electron microscopy revealed that AnxA5+ samples contained mainly parasites with an aberrant structure characterized by a swollen mitochondrion and a lack of tubular organization, nuclear structures, and granular-like structures as compared to parasites from AnxA5− populations (Fig. 3 d and e and i and j). Electron micrographs confirmed an increased parasite body width for AnxA5+ parasites (Fig. 3 d and e).
Fig. 3.
Separation of AnxA5+ promastigotes from AnxA5− parasites. In vitro cultured stat. phase promastigotes were separated into AnxA5+ (stat. phase AnxA5+) and AnxA5− (stat. phase AnxA5−) populations by using AnxA5-based MACS. Parasites were stained with the TUNEL method (a and f) and analyzed with flow cytometry. The histogram profiles of AnxA5+ (black line, a) and AnxA5− (black line, f) parasites are shown. The dotted lines show the TUNEL control staining, with fluorescent label added without addition of terminal deoxynucleotidyl transferase. Phase-contrast micrograph of AnxA5+ (b) and AnxA5− (g) populations. (Scale bar, 5 μm.) AnxA5-Fluos-staining of AnxA5+ (c) and AnxA5− (h) populations. Electron micrographs of longitudinal parasite sections (d and i) or transverse parasite sections (e and j) of purified AnxA5+ (d and e) and purified AnxA5− (i and j) parasites showing the mitochondrion/kinetoplast structure (K) at the end of the flagella pocket, nuclear structure (+), cytoplasmic granular-like structures (∗), and tubular organization (arrows). Micrographs and electron micrographs are representative of four independent experiments.
Because apoptotic cells do not multiply, in vitro culture was used to assess the viability of the parasites. A fixed number of AnxA5+ or AnxA5− promastigotes was applied in an end-point dilution assay. From the last dilution with parasitic growth, the percentage of viable parasites was calculated. The assays revealed that, whereas most of the MACS-separated AnxA5− population were able to grow, only a minor population (6.3%, range 1.6 −25%, n = 4) of the parasites in the AnxA5+ population grew in culture. These data indicate that the AnxA5+ L. major are apoptotic with an aberrant morphology, are not able to multiply, and therefore represent dying or already dead parasites.
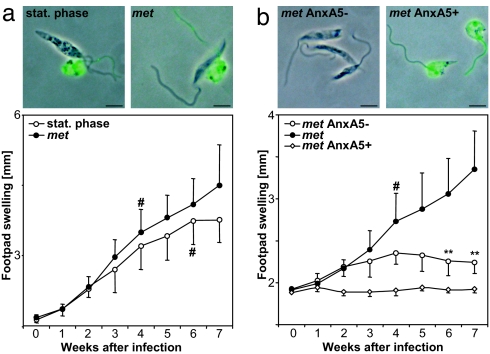
The Presence of AnxA5+ Apoptotic Parasites Is Required for Disease Development.
The murine L. major infection model was applied to investigate whether the apoptotic parasites play a role in disease development. Using fluorescence microscopy, we found that both metacyclic as well as stat. phase promastigote samples contained a mixture of round body-shaped AnxA5+ and elongated AnxA5− parasites (Fig. 4a). We found that metacyclic promastigotes induced a more severe disease with an earlier onset of footpad necrosis, as compared to stat. phase promastigotes (Fig. 4a). These data confirm that metacyclic promastigotes are more virulent in an in vivo infection model (1). The more virulent metacyclic population contained a high ratio (46.8 ± 11%) of AnxA5+ parasites. To investigate the role of AnxA5+ parasites for disease development, AnxA5+ parasites were depleted from this population by using MACS; resulting metacyclic AnxA5− populations contained as few as 14.2 ± 1% AnxA5+ parasites (n = 3). The metacyclic promastigotes containing a high ratio of AnxA5+ parasites lead to the development of severe disease (Fig. 4b). Animals injected with the metacyclic AnxA5− population, i.e., with viable parasites containing only few apoptotic promastigotes, did not develop serious disease. Mice infected with 100% apoptotic metacyclic parasites (see Methods) did not develop disease symptoms (Fig. 4b).
Fig. 4.
PS-dependent disease development in mice. (a) AnxA5-Fluos staining combined with phase-contrast micrographs are depicted of stat. phase promastigotes (stat. phase, Upper Left) and stat. phase-derived metacyclic L. major promastigotes (met, Upper Right). (Scale bar, 5 μm.) Mice were infected with 1 × 106 stat. phase promastigotes (stat. phase, open circles) or stat. phase-derived metacyclic L. major promastigotes (met, filled circles). Disease development was assessed by measuring the swelling of the infected footpad. (b) Micrographs (as in a) are depicted of metacyclic-derived AnxA5− (met AnxA5 −, Upper Left) and metacyclic derived AnxA5+ (met AnxA5 +, Upper Right). (Scale bar, 5 μm.) Mice were infected with 1 × 106 metacyclic L. major promastigotes (met, filled circles) as well as from this population-derived AnxA5− positive (met AnxA5 +, open squares) or AnxA5− (met AnxA5−, open circles) parasites. Data (mean ± SD) are from one representative experiment with eight mice per group of three experiments performed. # indicates onset of footpad necrosis, and ∗∗ indicates P < 0.0005.
Apoptotic Promastigotes Contribute to the Intraneutrophilic Survival of Nonapoptotic Promastigotes.
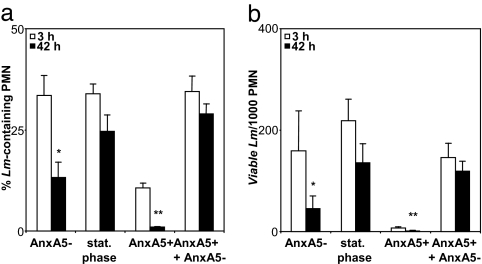
The above findings indicated that the presence of apoptotic parasites in the population of L. major is crucial for disease development. PMN are the first preliminary host cells for L. major promastigotes (4); therefore, we focused on promastigote interactions with PMN. Having observed the two populations, e.g., AnxA5+ apoptotic/dead and AnxA5−/viable parasites, we investigated to what extent these parasites are phagocytosed by PMN. The internalization rates of AnxA5−, stat. phase, and 1:1 mixture of AnxA5− and AnxA5+ promastigotes were similar (Fig. 5a). After phagocytosing stat. phase promastigotes or the mixture of AnxA5− and AnxA5+ promastigotes, most infected PMN still contained parasites after 42 h of incubation. However, the percentage of infected PMN decreased significantly (P < 0.05) if the AnxA5+ apoptotic parasites were depleted before the phagocytosis. In addition, the AnxA5+ parasites alone did not result in PMN infection (Fig. 5a). This suggests that the parasites were killed inside PMN when no apoptotic parasites were present during infection. The intraneutrophilic viability of L. major was assessed 3 and 42 h after the phagocytosis of AnxA5−, stat. phase, AnxA5+, or a 1:1 mixture of AnxA5− and AnxA5+ populations. End-point in vitro culture revealed that the number of viable parasites in PMN was significantly less (P < 0.05) when no apoptotic promastigotes were present in the phagocytosed parasite population (Fig. 5b). This finding confirms that parasites are killed inside PMN if they are ingested in the absence of apoptotic promastigotes.
Fig. 5.
Intracellular presence and survival L. major promastigote populations in human PMN. PMN were coincubated with stat. phase, stat. phase-derived purified AnxA5− or AnxA5+, or a 1:1 mixture of AnxA5+ and AnxA5− promastigotes. (a) The percentage of PMN-containing intracellular parasites was determined 3 and 42 h after coincubation using microscopical analysis of Giemsa-stained preparates. (b) Intraneutrophilic parasite survival 3 and 42 h after coincubation was assessed by using end-point titration and is depicted as the number of parasites per 1,000 PMN. Data show mean ± SD of three independent experiments. ∗, P < 0.05; ∗∗, P < 0.005.
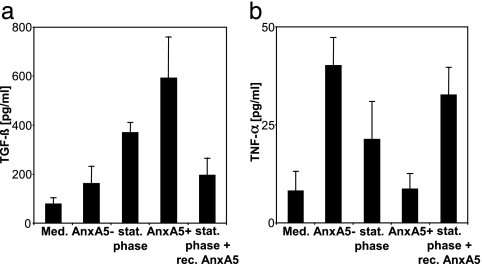
Apoptotic Promastigotes Induce TGF-β Production and Down-Regulate TNF-α Production by PMN.
The release of TGF-β and TNF-α was measured in supernatants of human PMN after coculture with stat. phase as well as with MACS-separated AnxA5− and AnxA5+ L. major promastigotes. The nonseparated stat. phase promastigotes induced the release of high levels of TGF-β (Fig. 6a). The amount of TGF-β clearly correlated with the ratio of AnxA5+ parasites, because the AnxA5+ parasites induce high amounts, whereas the AnxA5− parasites low amounts, of this antiinflammatory cytokine (Fig. 6a). In addition to TGF-β as a typical antiinflammatory mediator, we assessed the production IL-10 as another typical antiinflammatory mediator, but no detectable amounts of IL-10 were found in PMN supernatants (data not shown). An inverse correlation was observed between the ratio of AnxA5+ parasites and TNF-α release (Fig. 6b). The AnxA5− parasites induced high levels and the AnxA5+ parasites low levels of TNF-α release (Fig. 6b). Blocking experiments revealed a direct involvement of PS on the parasite surface in the induction of the above cytokines. Blocking PS with AnxA5 reduced the capacity of stat. phase promastigotes to induce TGF-β release (Fig. 6a), whereas the TNF-α release was enhanced after preincubation of the parasites with AnxA5 (Fig. 6b). Subsequently, we investigated whether the production of TGF-β and an antiinflammatory environment is beneficial for intraneutrophilic survival of L. major. We used stat. phase promastigotes coincubated with human PMN for 3 h. After removal of noningested parasites, we added either a TGF-β neutralizing mAb or an isotype-matched control. Treatment with the TGF-β neutralizing mAb resulted in a 35.2 ± 9.8% (n = 3) decrease of L. major containing PMN 42 h after infection. In addition, we found a similar decrease in the number of viable L. major per 1,000 PMN of 38.9 ± 9.6% (n = 3). These data suggest a causative link between L. major intraneutrophilic survival and production of TGF-β.
Fig. 6.
Cytokine production by human phagocytes after exposure to apoptotic and nonapoptotic L. major promastigotes. PMN (a and b) were cultured for 18 h in medium alone with stat. phase promastigotes, stat. phase-derived purified AnxA5− or AnxA5+ promastigotes, or with stat. phase promastigotes preincubated with 5 μg of recombinant annexin-V (Responsif; stat. phase + recAnxA5) at a parasite/PMN ratio of 5:1. The TGF-β (a) and TNF-α (b) content of the supernatants was measured by using an ELISA. Data show mean ± SD of four independent experiments.
Discussion
Whereas Leishmania promastigotes in the stationary growth phase are highly virulent, the parasites in the log. growth phase exert a limited disease-inducing capacity (1). Here we described that the presence of AnxA5+ apoptotic parasites in the promastigote population is a key factor determining virulence. The ratio of apoptotic parasites increases during in vitro culture and in the highly infectious stat. phase, >50% of the promastigotes are apoptotic. The nonapoptotic viable parasites alone, after depletion of the AnxA5+ parasites, are of limited virulence. The presence of AnxA5+ parasites enables the survival of nonapoptotic Leishmania in neutrophils, suggesting that apoptotic Leishmania silence PMN functions. We showed evidence that apoptotic parasites induce the release of TGF-β by neutrophils, which is likely to participate in the phagocyte-silencing effect. The data suggest the presence of apoptotic Leishmania provides survival advantage for the nonapoptotic parasites and, consequently, results in disease development. The finding that a major population of metacyclic promastigotes in the sandfly P. duboscqi is also AnxA5+ suggests a major disease-inducing role of apoptotic Leishmania after natural infection.
The most extensively studied example of “silent” phagocytosis is the uptake of apoptotic cells. Essential for the silent entry of apoptotic cells into phagocytes is the presence of the apoptotic “eat me” signal PS on the outer membrane leaflet of apoptotic cells (24). Ca2+-dependent AnxA5 binding to PS induces formation of trimers, hexamers, and bigger patch-like structures (25), which explains the observed patch-like structures found on AnxA5-stained promastigotes (see Fig. 1a). Because AnxA5 can also bind anionic phospholipids other then PS, we used additional ways to visualize PS such as stainings with a PS-specific mAb and with the PS-binding protein S. All these methods strongly suggest that a subpopulation of virulent promastigotes cultures expresses PS. However, we cannot exclude the possibility that AnxA5 and protein S bind another anionic phospholipid. Therefore, we termed these parasites AnxA5+. Mass spectrometry analyses on lipids purified from AnxA5+ promastigote membranes could solve this question.
Even though the exact mechanism of PS recognition by specific receptors is unclear, the silencing effect of PS interactions on phagocytes and the immune system is evident and involves the production of TGF-β (8). TGF-β is arguably one of the most potent antiinflammatory cytokines. In the phagocytic clearance of apoptotic cells, TGF-β prevents immune responses against abundantly internalized and processed proteins of the apoptotic remains (8, 26). TGF-β has been demonstrated to enhance the infectivity of L. major in vivo (27). TGF-β transmits its silencing signals through the TGF-β receptor and cytoplasmic proteins called Smads (28). We found that TGF-β produced by PMN after coincubation with L. major was bioactive and resulted in Smad2 phosphorylation (data not shown). Moreover, we demonstrated that TGF-β neutralization decreased intraneutrophilic Leishmania survival.
The apoptotic program is a precise regulated process of cell suicide that is central to the development, homeostasis, and integrity of multicellular organisms (29). This argument also fits an apoptotic program for single-celled organisms when such organisms are regarded as a population. Apoptosis-like death has been described for several single-celled eukaryote organisms; these include Trypanosomas and both promastigote as well as amastigote forms of Leishmania (17, 30). The apoptosis-like phenotype of parasite death may reduce the onset of inflammation and favor parasite evasion from the immune system (29). Our results demonstrate that AnxA5+ apoptotic parasites provide a survival advantage for Leishmania promastigotes. However, our data contradict the suggestion that Leishmania can use PS as a form of apoptotic mimicry (20). The apoptotic mimicry hypothesis is based on experimental data using Leishmania amastigotes. We investigated Leishmania promastigotes, the form of the parasite transmitted by the bite of the insect vector and therefore the developmental stage responsible for causing disease. We showed that AnxA5+ Leishmania are apoptotic and destined to death.
That apoptotic Leishmania provide survival advantage for the viable parasites can be regarded as altruistic behavior. Altruism has already been described for the survival of populations of several single-celled organisms. The slime mold Dictyostelium discoideum (31) and also prokaryotes such as Streptomyces (32) and Bacillus subtilis (33) use an apoptosis-like program for one part of the colony where the other part develops in long-lived spores. In all three cases, it is presumed that nutrient shortage is the inductor of this altruistic behavior to help the survival of the population. With Leishmania, a nutrient shortage in the stat. phase of culture or in the sandfly gut seems a reasonable explanation for the onset of apoptosis accompanied by the appearance of PS on the parasite surface.
Methods
L. major Promastigotes.
L. major (MHOM/IL/81/FEBNI) promastigotes were cultured as described (34). Log. phase or stat. phase cultures were obtained after incubation at 27°C in a 5% CO2 humidified atmosphere for 2 or 7 days, respectively. In addition, promastigotes were obtained from the midgut of P. duboscqi sandflies on day 7 after infection with L. major, as described (22).
Promastigote Agglutination and MACS Separation.
Metacyclic L. major promastigotes (PNA-negative, termed met) were purified from stat. phase cultures by negative selection by using PNA (Vector, Burlingame, CA), as described (2). AnxA5− parasites, derived from either stat. phase or met promastigote populations, were obtained by magnetic cell separation (AutoMACS, Miltenyi Biotec, Bergisch Gladbach, Germany). AnxA5+ parasites were depleted by using AnxA5-labeled super paramagnetic microbeads. Subsequently, AnxA5+ parasites were washed in Ca2+-free PBS to dissociate bound AnxA5− beads. End-point titration in vitro culture was used to estimate the number of viable promastigotes in the parasite samples, as described (35). Briefly, 1.0 × 105 promastigotes were added in quadruplicate wells of 96-well plates, and a dilution factor of 1.5 was carried out. Parasites were grown for 1 week. The percentage of multiplying Leishmania was calculated from the last dilution (mean of quadruplicate wells) that had parasitic growth.
PS Detection and Apoptosis Assay.
Labeling of parasites with AnxA5-Fluos (Roche Molecular Biologicals, Mannheim, Germany) was performed in the presence of 5 mM Ca2+Cl2. As a negative control, AnxA5-Fluos was added to the parasites in the absence Ca2+. In addition, PS was detected by using an anti-PS mAb (Clone 1H6, IgG, Biomol, Hamburg, Germany; ref. 15). Purified mouse IgG (Sigma, Taufkirchen, Germany) was used as negative control. Labeling was visualized by using an anti-mouse-IgG mAb conjugated to Alexa-488 (Molecular Probes, Leiden, The Netherlands). Moreover, PS was detected by labeling parasites with 1 μg/ml protein S (Kordia Life Sciences, Leiden, The Netherlands) in the presence of 5 mM Ca2+Cl2 (14). As a negative control, protein S was added to the parasites in the absence Ca2+. Protein S binding was detected as described (36). For structural preservation electron microscopy, parasites were fixed and analyzed as described (6). The TUNEL assay (In Situ Cell Death Detection Kit, Roche Molecular Biologicals) was used to detect apoptotic cells (37). Labeled parasites were analyzed by using an Axioskop-2 fluorescence microscope or a LSM confocal laser-scanning microscope (both from Zeiss, Jena, Germany) or by flow cytometry by using a FACS-Calibur with CellQuest-Pro software (Becton Dickinson, San Diego, CA).
Experimental Infection of Mice.
Eight- to 12-week-old female BALB/c mice (Charles River Breeding Laboratories, Sulzfeld, Germany) were injected in the hind footpad with 1 × 106 stat. phase L. major promastigotes or purified metacyclic L. major promastigotes, as well as with 1 × 106 AnxA5− or AnxA5+ metacyclic populations. Parasite numbers given are based on the number of AnxA5− viable promastigotes in a sample (except for purified AnxA5+, dead parasites samples). To obtain 100% AnxA5+ apoptotic promastigotes, purified AnxA5+ metacyclic parasites were irradiated with 20-kJ UV light 24 h before infection. Disease development was assessed by measuring swelling of the infected footpad (38).
In Vitro Infection of Phagocytes.
PMN were isolated from buffy coat blood as described (34). PMN (1 × 107 ml) were coincubated with stat. phase L. major promastigotes with or without preincubation of 5 μg of recombinant AnxA5 (Responsif, Erlangen, Germany) or with MACS-purified AnxA5+, AnxA5−, or a 1:1 mixture of AnxA5+ and AnxA5− parasites, at 37°C at a AnxA5− parasite/PMN ratio of 5:1 in RPMI medium 1640 (Gibco, Grand Island, NY), supplemented with 5% heat-inactivated FCS/50 μM 2-mercaptoethanol/2 mM l-glutamine/10 mM Hepes/100 μg/ml penicillin/160 μg/ml gentamicin (all from Seromed-Biochrom, Berlin, Germany). Extracellular parasites were removed 3 h after coincubation (6). For TGF-β-neutralizing experiments, PMN were coincubated with 2 μg/ml TGF-β blocking mAb or an isotype-matched control mAb (MAB 240, IgG1 and MAB002, IgG1, respectively; R&D Systems, Wiesbaden, Germany). Cells and supernatants were collected after 18 and 42 h of coincubation for further analyses. The percentage of Leishmania containing PMN was determined 3, 18, and 42 h after coincubation by microscopical evaluation of >200 PMN after Giemsa staining of cytocentrifuge preparates. End-point titration experiments were carried out by using 1,000 PMN in quadruplicate wells and a dilution factor of 1.5. The number of viable L. major per 1,000 PMN was calculated from the last dilution that had parasitic growth and equals 1.5 exp (mean dilution with parasitic growth).
Cytokine Measurements.
TGF-β production by PMN was assessed by using a sandwich ELISA protocol as described (39). TNF-α and IL-10 production was assessed by ELISA (OptEIATM Set Human TNF-α and OptEIATM Set Human IL-10, respectively; BD Bioscience, San Diego, CA).
Statistical Analysis.
Data are depicted as mean value ± SD. To determine whether differences were statistically significant, Student’s t test was performed by using a two-tailed distribution with paired samples and Microsoft Excel 8.0 software. ∗ indicates statistically different at P < 0.05 (Fig. 5 a and b), and ∗∗ indicates statistically different at P < 0.005. (Figs. 4b and 5a and b).
Supplementary Material
Acknowledgments
We thank S. Möller and A. Hölscher for excellent technical assistance, Dr. C. van Kooten for critical review of the manuscript, and Drs. P. Schlenke and S. Görg (University of Lübeck) for providing the buffy coat material. This work was supported by Deutsche Forschungsgemeinschaft Grants SFB 367/B10 and La 1267/1-2.
Abbreviations
- PNA
peanut agglutinin
- LPG
lipophosphoglycan
- stat. phase
stationary growth phase
- log. phase
logarithmic growth phase
- PMN
polymorphonuclear neutrophil granulocytes
- MF
macrophages
- PS
phosphatidylserine
- MACS
magnetic cell sorting.
Footnotes
Conflict of interest statement: No conflicts declared.
This paper was submitted directly (Track II) to the PNAS office.
References
- 1.da Silva R, Sacks DL. Infect Immun. 1987;55:2802–2806. doi: 10.1128/iai.55.11.2802-2806.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sacks DL, Hieny S, Sher A. J Immunol. 1985;135:564–569. [PubMed] [Google Scholar]
- 3.Spath GF, Epstein L, Leader B, Singer SM, Avila HA, Turco SJ, Beverley SM. Proc Natl Acad Sci USA. 2000;97:9258–9263. doi: 10.1073/pnas.160257897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sunderkotter C, Kunz M, Steinbrink K, Meinardus-Hager G, Goebeler M, Bildau H, Sorg C. J Immunol. 1993;151:4891–4901. [PubMed] [Google Scholar]
- 5.Laufs H, Müller K, Fleischer J, Reiling N, Jahnke N, Jensenius JC, Solbach W, Laskay T. Infect Immun. 2002;70:826–835. doi: 10.1128/iai.70.2.826-835.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Zandbergen G, Klinger M, Müller A, Dannenberg S, Gebert A, Solbach W, Laskay T. J Immunol. 2004;173:6521–6525. doi: 10.4049/jimmunol.173.11.6521. [DOI] [PubMed] [Google Scholar]
- 7.Spath GF, Garraway LA, Turco SJ, Beverley SM. Proc Natl Acad Sci USA. 2003;100:9536–9541. doi: 10.1073/pnas.1530604100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Voll RE, Herrmann M, Roth EA, Stach C, Kalden JR, Girkontaite I. Nature. 1997;390:350–351. doi: 10.1038/37022. [DOI] [PubMed] [Google Scholar]
- 9.Henson PM. Immunity. 2004;21:604–606. doi: 10.1016/j.immuni.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Henson PM, Bratton DL, Fadok VA. Curr Biol. 2001;11:R795–R805. doi: 10.1016/s0960-9822(01)00474-2. [DOI] [PubMed] [Google Scholar]
- 11.Fadok VA, Bratton DL, Guthrie L, Henson PM. J Immunol. 2001;166:6847–6854. doi: 10.4049/jimmunol.166.11.6847. [DOI] [PubMed] [Google Scholar]
- 12.van Heerde WL, Poort S, van’t Veer C, Reutelingsperger CP, de Groot PG. Biochem J. 1994;302:305–312. doi: 10.1042/bj3020305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anderson HA, Maylock CA, Williams JA, Paweletz CP, Shu H, Shacter E. Nat Immunol. 2003;4:87–91. doi: 10.1038/ni871. [DOI] [PubMed] [Google Scholar]
- 14.Webb JH, Blom AM, Dahlback B. J Immunol. 2002;169:2580–2586. doi: 10.4049/jimmunol.169.5.2580. [DOI] [PubMed] [Google Scholar]
- 15.Mandinov L, Mandinova A, Kyurkchiev S, Kyurkchiev D, Kehayov I, Kolev V, Soldi R, Bagala C, de Muinck ED, Lindner V, et al. Proc Natl Acad Sci USA. 2003;100:6700–6705. doi: 10.1073/pnas.1231994100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ribeiro-Gomes FL, Otero AC, Gomes NA, Moniz-De-Souza MC, Cysne-Finkelstein L, Arnholdt AC, Calich VL, Coutinho SG, Lopes MF, DosReis GA. J Immunol. 2004;172:4454–4462. doi: 10.4049/jimmunol.172.7.4454. [DOI] [PubMed] [Google Scholar]
- 17.Lee N, Bertholet S, Debrabant A, Muller J, Duncan R, Nakhasi HL. Cell Death Differ. 2002;9:53–64. doi: 10.1038/sj.cdd.4400952. [DOI] [PubMed] [Google Scholar]
- 18.Arnoult D, Akarid K, Grodet A, Petit PX, Estaquier J, Ameisen JC. Cell Death Differ. 2002;9:65–81. doi: 10.1038/sj.cdd.4400951. [DOI] [PubMed] [Google Scholar]
- 19.Zufferey R, Allen S, Barron T, Sullivan DR, Denny PW, Almeida IC, Smith DF, Turco SJ, Ferguson MA, Beverley SM. J Biol Chem. 2003;278:44708–44718. doi: 10.1074/jbc.M308063200. [DOI] [PubMed] [Google Scholar]
- 20.de Freitas Balancoqq JM, Moreira ME, Bonomo A, Bozza PT, Marante-Mendes G, Pirmez C, Barcinski MA. Curr Biol. 2001;11:1870–1873. doi: 10.1016/s0960-9822(01)00563-2. [DOI] [PubMed] [Google Scholar]
- 21.Tripathi A, Gupta CM. Mol Biochem Parasitol. 2003;128:1–9. doi: 10.1016/s0166-6851(03)00024-0. [DOI] [PubMed] [Google Scholar]
- 22.Sacks DL, Perkins PV. Am J Trop Med Hyg. 1985;34:456–459. doi: 10.4269/ajtmh.1985.34.456. [DOI] [PubMed] [Google Scholar]
- 23.Sheriff A, Gaipl US, Franz S, Heyder P, Voll RE, Kalden JR, Herrmann M. Cytometry A. 2004;62:75–80. doi: 10.1002/cyto.a.20090. [DOI] [PubMed] [Google Scholar]
- 24.Lauber K, Blumenthal SG, Waibel M, Wesselborg S. Mol Cell. 2004;14:277–287. doi: 10.1016/s1097-2765(04)00237-0. [DOI] [PubMed] [Google Scholar]
- 25.Concha NO, Head JF, Kaetzel MA, Dedman JR, Seaton BA. FEBS Lett. 1992;314:159–162. doi: 10.1016/0014-5793(92)80964-i. [DOI] [PubMed] [Google Scholar]
- 26.Fadok VA, Bratton DL, Konowal A, Freed PW, Westcott JY, Henson PM. J Clin Invest. 1998;101:890–898. doi: 10.1172/JCI1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barral-Netto M, Barral A, Brownell CE, Skeiky YA, Ellingsworth LR, Twardzik DR, Reed SG. Science. 1992;257:545–548. doi: 10.1126/science.1636092. [DOI] [PubMed] [Google Scholar]
- 28.ten Dijke P, Hill CS. Trends Biochem Sci. 2004;29:65–273. doi: 10.1016/j.tibs.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 29.Ameisen JC. Cell Death Differ. 2002;9:367–393. doi: 10.1038/sj.cdd.4400950. [DOI] [PubMed] [Google Scholar]
- 30.Piacenza L, Peluffo G, Radi R. Proc Natl Acad Sci USA. 2001;98:7301–7306. doi: 10.1073/pnas.121520398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaiser D. Annu Rev Genet. 1986;20:539–566. doi: 10.1146/annurev.ge.20.120186.002543. [DOI] [PubMed] [Google Scholar]
- 32.Wildermuth H. J Gen Microbiol. 1970;60:43–50. doi: 10.1099/00221287-60-1-43. [DOI] [PubMed] [Google Scholar]
- 33.Kaiser D, Losick R. Cell. 1993;73:873–885. doi: 10.1016/0092-8674(93)90268-u. [DOI] [PubMed] [Google Scholar]
- 34.van Zandbergen G, Hermann N, Laufs H, Solbach W, Laskay T. Infect Immun. 2002;70:177–4184. doi: 10.1128/IAI.70.8.4177-4184.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bogdan C, Schroppel K, Lohoff M, Rollinghoff M, Solbach W. Eur J Immunol. 1990;20:2533–2540. doi: 10.1002/eji.1830201202. [DOI] [PubMed] [Google Scholar]
- 36.Dahlback B, Hildebrand B, Malm J. J Biol Chem. 1990;265:8127–8135. [PubMed] [Google Scholar]
- 37.Gorczyca W, Melamed MR, Darzynkiewicz Z. Toxicol Lett. 1993;67:249–258. doi: 10.1016/0378-4274(93)90060-b. [DOI] [PubMed] [Google Scholar]
- 38.Laskay T, Wittmann I, Diefenbach A, Rollinghoff M, Solbach W. J Immunol. 1997;158:1246–1253. [PubMed] [Google Scholar]
- 39.Szymkowiak CH, Mons I, Gross WL, Kekow J. J Immunol Methods. 1995;184:263–271. doi: 10.1016/0022-1759(95)00098-u. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.