SYNOPSIS
Tobacco use rates are high among college students, and while many of them try to quit every year, only a small percentage are successful at maintaining abstinence. Most colleges have campus health centers that offer treatment for tobacco cessation, but few students access these resources. Little is known about how to motivate young adult college students to seek treatment or assist them in their attempts to quit smoking.
In the context of a comprehensive, group-randomized intervention study to decrease smoking among college students, a case-based tobacco cessation training program for campus health center providers and staff was developed and conducted at 14 intervention colleges during the 2003–2004 academic year. Six case studies were created for this training, using responses from 39 student elicitation interviews conducted at 12 colleges in Spring 2002. Common themes relating to smoking, quitting, and relapse experiences reported by students in the elicitation interviews were woven into the cases and integrated into the training program.
Tobacco use among college students and other young adults increased throughout the 1990s1–3 and smoking prevalence among those 18–24 years old is currently the highest of all adult age groups at 29%.4 While college students smoke less than their non-college peers, 23% of full-time college students are current smokers, posing a significant health threat to this population.1 The majority (70% to 80%) of college students who smoke report an intention or desire to quit, and over half (54%) make quit attempts each year.3,5 Unfortunately, relatively few remain abstinent. One study showed that of 82% of student smokers who had tried to quit, 75% remained smokers.6 Another study found that 87% of college freshmen and sophomores who smoked daily were still smoking four years later.7
Nearly all universities and residential colleges have a campus health center (CHC), yet a national survey of student health service directors found that 44% of CHCs did not offer group smoking cessation programs, and those with programs reported extremely low student participation.8 Another study at 50 state universities showed that while some form of treatment for tobacco use was available at all CHCs, medical insurance coverage for this service was limited; 70% of plans covered office visits, but only 18% provided coverage for both visits and medications.9 Thus, while it is clear that college students want to quit and would benefit greatly from quitting, CHCs appear to be underutilized as a resource for tobacco cessation.
There are no published studies specifically focused on developing effective smoking cessation programs within a student health clinic setting; thus, little is known about how CHCs can tailor programs to attract students and address their cessation needs. An evidence-based Clinical Practice Guideline is available for treating tobacco dependence in adults;10 however, young adults are often in the earlier stages of developing a tobacco habit, compared to older adults, which can affect the potential impact of the standard treatment described in the Guideline. For example, nicotine replacement therapy (NRT) has been shown to be less effective for those with occasional (non-daily) or light (<10 cigarettes per day) smoking patterns,10 both more common among college students.5
In light of these considerations, a tailored tobacco-cessation training program was created as one component of a National Cancer Institute-funded group-randomized trial testing a comprehensive intervention to reduce smoking among college students at 30 four-year colleges in the Pacific Northwest (Washington, Oregon, and Idaho). The training consisted of two modules: a case-based continuing medical education (CME) course for health care providers (HCPs), and a clinic systems training for other CHC staff. This article describes the process of developing and delivering the CME training to clinicians at the intervention colleges, with a focus on the creation and integration of the case studies.
PROGRAM DEVELOPMENT
An initial qualitative phase of the larger study took place in 12 Washington and Oregon colleges in Spring 2002.11 Of the 12 colleges, six are public universities and six are private. Seven of the 12 universities are located in urban settings and five in rural settings. Six of the colleges are considered small (less than 3,000 students) and six are large (more than 5,000 students). The developed CME training was implemented at the 15 randomly selected intervention campuses in the larger trial.
Elicitation interviews
Open-ended, exploratory interviews were used to collect data for development of questionnaires, intervention activities, and materials for the trial, following the recommendation of Rimer12 and Thompson.13 Research staff conducted 40 elicitation interviews with eligible college students who were either current tobacco users or had quit within the past two months. Students were asked about their tobacco use initiation and history, attitudes and beliefs about smoking and campus policies, influences on their smoking, quitting, and relapse, and use of the CHC. We analyzed responses to the interview questions that focused on students' smoking history, motivation for and barriers to cessation, experience with the CHC, and knowledge and attitudes about resources to support a quit attempt. Themes that emerged from these responses, in conjunction with findings and recommendations from the Clinical Practice Guideline, were used to develop the case studies, course content, and materials for the health care provider (HCP) and clinic staff training modules.
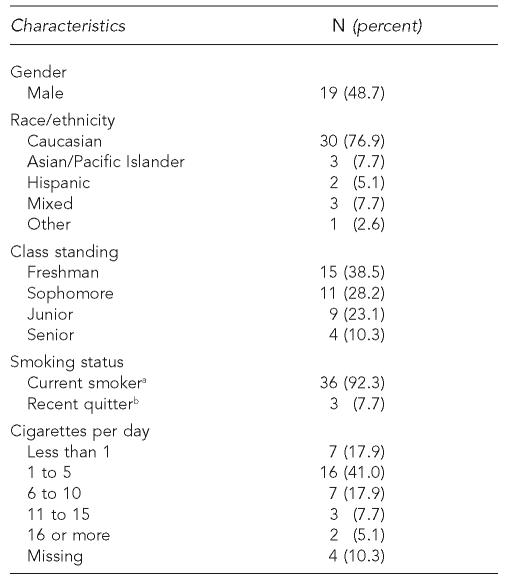
Characteristics of interview respondents.
Of the 39 students whose interviews were completed and taped, half were male, three-quarters were Caucasian, and two-thirds were freshmen or sophomores (Table). All but three (92%) met the project definition of current smoker (smoked at least one cigarette in the past 30 days) and the remainder were recent quitters (abstinent less than two months). Most students who were current smokers (80%) reported that they smoked daily, although few daily smokers (18%) reported smoking more than 10 cigarettes per day. Fifteen percent initiated smoking and 36% became regular smokers at or after 18 years of age, indicating that half were in the early stages of a smoking habit. Twenty-eight percent of those who met the project's definition of a current smoker did not consider themselves to be smokers, even though a number of them smoked daily.
Table.
Characteristics of students interviewed (N = 39)
Smoked at least one cigarette in past 30 days
Quit less than two months ago
CHC experience and resources for cessation.
All 39 students reported that their school had a CHC. Although it was determined from college staff informants that cessation resources were available at all the CHCs, less than half (40%) of the respondents were aware of these resources. Thirty students (77%) reported that they had been seen at the CHC at least once. Of those students, nearly two-thirds (64%) reported that they had been asked about their smoking status; however, only half of those who were asked said that they were advised to quit smoking.
Students were asked about the types of smoking cessation resources they would prefer and the likelihood they would access such resources. They were also prompted by interviewers to give their views on specific types of cessation resources, including a telephone quit line, a web site, nicotine replacement therapy, and any other on-campus services of which the student might take advantage. Of the 37 students who were asked this question, 60% reported that they would not seek cessation assistance, although with prompting, a fifth of those said they would use nicotine replacement, especially if it was free, and a few mentioned they might seek social support from friends or the help of a health professional.
Influences on quitting and relapse.
All those interviewed except for one student had made at least one quit attempt with abstinence greater than 24 hours. The majority (70%) had remained abstinent for a week or longer and three had been abstinent for over 30 days. Of the factors students cited as influencing past quit attempts, or reasons they would consider quitting in the future, general health concerns were most frequent, with a specific personal health issue cited as the main reason for quitting in several cases, including two of the three subjects who were currently abstinent. Social factors were the second most frequently cited reason for quitting, including pressure from family members or significant others to quit smoking, or being in an environment where smoking was not thought to be socially acceptable. Relapse back to smoking was most often attributed to being around friends who smoked, or in social situations and environments that were associated with previous smoking experience, such as parties and going out to bars, or back to college after a vacation or summer break.
Case study development
The utilization of case studies in medical education has been shown by Cox and others to be an effective means for promoting active and collaborative learning, presenting multiple perspectives, and bringing real-world complexities to the classroom.14–16 Cases facilitate the translation of theoretical frameworks and newly acquired evidence-based medical information to clinical practice by structuring knowledge within a context that aids in later recall and allows generalization of rules for reasoning about novel situations. In addition, by demanding decision-making and resolution, cases assist clinicians in anticipating a multitude of relevant factors that may affect implementation of a proposed treatment plan, an especially important consideration in treating tobacco dependence.
Case studies for our training were modeled after those used in an on-line CME course offered by the University of Wisconsin School of Medicine,17 adapted to a younger adult population. The cases for this study were derived from analyses of responses to the college student elicitation interviews, illustrating typical student social concerns, short-term health effects, smoking patterns, potential motivations to quit, and relapse triggers. Similar to the older adult cases, the student cases were designed to provide opportunities for clinicians to apply knowledge learned in the didactic portion of the training (such as indication for and use of pharmacotherapy) and to practice the basic elements of treatment while maximizing relevance to the college population.
IMPLEMENTATION
The main objective of the training program was to provide a concise, interactive, and practical course that was pertinent to the college student population and easy to implement in a CHC setting. To facilitate attendance, the training was conducted at each CHC and scheduled at a time when the maximum number of clinicians could attend; one hour of continuing medical education (CME) credit was available to participants. The training was offered to all 15 intervention condition colleges during the 2003–2004 academic year; HCPs from 14 (93%) of the schools participated in the training. The remaining university elected to receive a similar Guideline-based training conducted by a local health department trainer that did not include the college student case studies.
Didactic element
The first half of the one-hour HCP tobacco cessation training course covered general treatment material from the Clinical Practice Guideline as well as specific information about tobacco use trends among college students, how the campus environment may influence tobacco use, and the potential role of the CHC in supporting cessation. This section included a review of the “5 As” (Ask, Advise, Assess, Assist, Arrange) for smokers who are ready to quit, and the “5 Rs” (Relevance, Risks, Rewards, Roadblocks, Repetition) for those who are not willing to make a quit attempt at that time. Indications for and usage of pharmacotherapy were covered, along with Basic Motivational Interviewing (BMI) techniques, which are used to help students identify the risks of their behavior, benefits of quitting, and internal resources for making the desired change.10 After this didactic portion, the six composite case studies were presented and discussed.
Case study integration
Since health concerns were the most frequently identified theme in the elicitation interviews for facilitating cessation, and play a role in virtually all visits to a CHC, each case study centered around a common medical issue that could assist participants in identifying and taking advantage of “teachable moments” that are likely to arise in encounters with students who smoke. These situations enable clinicians to personalize advice to quit, help students relate their smoking to a health effect or threat that is relevant to them, and provide a focus for discussion about the benefits of not using tobacco.
Two cases focused on reproductive health issues in women, one involving an abnormal pap smear and the other about oral contraceptive use in a student with borderline hypertension and a family history of stroke. Two other cases revolved around respiratory problems, including recurrent bronchitis in a heavy smoker and an acute upper respiratory infection in a “social” smoker; both of these students also gave a history of increased tobacco use associated with partying on weekends, a pattern typical among college students. The remaining two cases included a chewing tobacco-using athlete with allergic rhinitis and oral leukoplakia and a student presenting with an acute depressive episode (and smoking relapse) precipitated by the breakup of a romantic relationship.
Social influences on tobacco use comprised another common theme that emerged from the elicitation interviews. These were found to facilitate both smoking and cessation among our respondents and were incorporated into all of the cases. Having a significant other or friends who smoked, going out or partying, and “taking a break” were particularly salient facilitators of smoking and, correspondingly, barriers to cessation. Conversely, having a girlfriend or boyfriend who didn't smoke, or feeling that smoking was not acceptable to friends or family, often facilitated abstinence from smoking. In one case, a non-smoking fiancée was a motivator for one woman to quit; in a second case, a woman who smoked but was willing to try to quit provided potential support for her boyfriend. The case involving relapse precipitated by breakup with a girlfriend who didn't smoke illustrated both facilitation of a long abstinence period and a barrier to staying quit; additionally, this case provided an opportunity to explore the interaction between mood and tobacco use, which is known to be a strong influence on young adult smokers.7
Several of those interviewed reported having a close relative who had suffered or died from a tobacco-related illness; thus, family influence themes were woven into three of the case studies. For instance, in one case, a student who was a heavy smoker lost his father to lung cancer; in another, a young woman being seen for a birth-control consult had a grandmother who had died from a stroke. These cases were used to highlight the students' individual risk for developing similar diseases and their personal experience of seeing the adverse effects of smoking on someone close to them, both of which can make the potential harm of smoking more “real” to students and help them overcome their denial that this could happen to them. We also heard from the elicitation interviews that some students abstained from smoking when they were with their families, due to either parental disapproval (not wanting to disappoint or be hassled by their parents) or fear that younger siblings might emulate their behavior; one of the case studies embodied these concepts.
Consistent with the high percentage of students in our study who made quit attempts and were smoking again, a relapse component was built into four of the six cases. The fictitious students, similar to those we interviewed, experienced varying lengths of abstinence, and returned to tobacco use for a variety of reasons. Discussion of a previous quit attempt is a standard motivational technique for reinforcing self-efficacy and identifying benefits of not smoking and triggers for relapse—all of which can help prepare a student for their next try and increase their chances for success. In one case, a student relapsed when she gained more weight than she was comfortable with; in another, relapse was precipitated by a breakup with a non-smoking girlfriend; in a third, relapse was attributed to the stresses of school and being in an environment where smoking was socially normative. The relapse cases were designed to give the HCP an opportunity to practice helping a student remember the positive feelings and experiences he or she had during a period of abstinence, reinforce the short- and long-term health benefits of remaining smoke free, and develop strategies to avoid or cope with triggers that would inevitably be encountered again.
Among the elicitation interview students, 30% did not express a current desire to quit. This was reflected in two case studies where the student, on assessment by the HCP, was not willing to make a quit attempt, thus giving those participating in the training an opportunity to practice the 5 Rs. In one case, the student had physical findings of a tobacco-related condition with a risk of progression to a more dangerous disorder, as well as some misperceptions about the physical benefits of using tobacco. The other student, a non-daily social smoker, who presented with an upper respiratory tract infection after a weekend of partying, felt that she didn't smoke enough to cause herself harm and could quit whenever she wanted to. Using the 5 Rs enables the provider to raise questions that challenge a student's internal inconsistencies, ambivalence about their tobacco habit, and denial of their risks. In both cases, after providing relevant medical information, the provider could help the student identify facilitators for cessation by starting with the question, “If you were to quit now, what would be possible reasons for doing so?” In the second case, challenging the student to abstain from smoking the following weekend could be used to force a realization that “quitting whenever she wants” is likely to be harder than she thinks.
EVALUATION
The program was enthusiastically received and well attended by providers (n = 46), allied health professionals (n = 62), and office staff (n = 15) from the 14 colleges that received the training. Providers and nursing staff participated actively in case-study discussions, and of the 79 participants who completed evaluation forms after the course, 96% agreed (n = 36) or strongly agreed (n = 40) that the CME activity improved their ability to effectively treat, manage, and communicate with patients regarding their tobacco use. Key informants interviewed at the end of the study reported an increase in student utilization of the CHC for tobacco treatment at 14 of the 15 intervention schools over the past two years, compared to three out of 15 of the control schools. Similarly, the amount and variety of treatment was reported to have increased at all 15 intervention CHCs, while only five of the control college informants reported this experience.
CONCLUSIONS
College students, often living away from home for the first time, find themselves in an environment where smoking is commonly used to manage the social challenges and other stresses that accompany this major transition in their lives.18 While students are knowledgeable about the adverse health effects and risks of smoking and express a desire or plan to quit, the perceived positive functions of their smoking behavior cause them to underestimate their personal risks, thus undermining their motivation to quit.19 The elicitation interviews in this study demonstrated that students are largely unaware of the availability or value of cessation resources. They believe that they will be able to quit on their own when they want to and will not smoke enough to get sick; they often fail to even identify themselves as smokers.
Student health service providers may be discouraged from addressing tobacco cessation in light of students' apparent reluctance to quit, as well as the lack of training, tools, and evidence for effective treatment in this population; additionally, their time is short and they often have more immediate concerns about a student's health. In the absence of established evidence-based protocols for treating tobacco use in the young adult college student population, case studies were incorporated into this training program to reflect the medical, psycho-social, and behavioral issues that characterize college students' barriers to and facilitators for quitting tobacco use. Understanding the characteristics of college smokers helps provide a concrete basis for talking with students about their tobacco use. The training was intended to increase student health providers' motivation to address tobacco use and confidence in their ability to intervene by using real-life examples in a case-study format as a vehicle for sharing experience and practicing specific techniques.
Most students interviewed for this study stated that they would not seek assistance for quitting, although, when prompted, expressed interest in trying nicotine replacement therapy (NRT) products, indicating that it was possible to attract students to use cessation resources. This is consistent with previous findings from Hines and colleagues, who found that 95% of college students said they would choose an unassisted method for their next quit attempt, although if nicotine replacement patches or stop-smoking programs were free, over half stated they would try them.20 Our experience confirmed this; after conducting the trainings and supplying CHCs with free nicotine patches and gum, student health service directors and staff reported increased utilization of the CHC for tobacco treatment and NRT.
The CHC tobacco cessation training program described here was only one component of a comprehensive intervention utilizing multiple approaches to reduce tobacco use among college students through campus policy change, community outreach, education, and advocacy; thus it is not possible to separate the individual impact of this training on the tobacco-use reduction outcomes of the study. However, results are encouraging in terms of both the providers' self-reported attainment of educational goals on their evaluations, and the increased utilization of CHC treatment services by students at the intervention colleges as reported by key informants at the end of the study. In the context of the integrated environmental and individual approach used in our study, we are hopeful that students' increased access to and utilization of the resources offered by the CHCs will contribute to a reduction in tobacco use on these campuses, and can serve as a model for colleges across the nation.
Acknowledgments
This work was funded by the Tobacco Research Initiative for State and Community Interventions of the National Cancer Institute (Grant No. CA93967). The University of Wisconsin School of Medicine generously provided CME accreditation for the Campus Health Center Tobacco Cessation Training described in this paper, through an educational grant from the University of Wisconsin's Center for Tobacco Research and Intervention.
REFERENCES
- 1.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Volume II: college students and adults ages 19–45. Bethesda (MD): National Institute of Drug Abuse; 2004. Monitoring the future: national survey results on drug use, 1975-2003. [Google Scholar]
- 2.Wechsler H, Rigotti NA, Gledhill-Hoyt J, Lee H. Increased levels of cigarette use among college students: a cause for national concern [published erratum appears in JAMA 1999 281:136] JAMA. 1998;280:1673–8. doi: 10.1001/jama.280.19.1673. [DOI] [PubMed] [Google Scholar]
- 3.Rigotti NA, Lee JE, Wechsler H. US college students' use of tobacco products: results of a national survey. JAMA. 2000;284:699–705. doi: 10.1001/jama.284.6.699. [DOI] [PubMed] [Google Scholar]
- 4.Cigarette smoking among adults—United States, 2002. MMWR Morb Mortal Weekly Rep. 2004;53(20):427–31. [PubMed] [Google Scholar]
- 5.Moran S, Wechsler H, Rigotti NA. Social smoking among US college students. Pediatrics. 2004;114:1028–34. doi: 10.1542/peds.2003-0558-L. [DOI] [PubMed] [Google Scholar]
- 6.Everett SA, Husten CG, Kann L, Warren CW, Sharp D, Crossett L. Smoking initiation and smoking patterns among US college students. J Am Coll Health. 1999;48:55–60. doi: 10.1080/07448489909595674. [DOI] [PubMed] [Google Scholar]
- 7.Wetter DW, Kenford SL, Welsch SK, Smith SS, Fouladi RT, Fiore MC, et al. Prevalence and predictors of transitions in smoking behavior among college students. Health Psychol. 2004;23:168–77. doi: 10.1037/0278-6133.23.2.168. [DOI] [PubMed] [Google Scholar]
- 8.Wechsler H, Kelley K, Seibring M, Kuo M, Rigotti NA. College smoking policies and smoking cessation programs: results of a survey of college health center directors. J Am Coll Health. 2001;49:205–12. doi: 10.1080/07448480109596305. [DOI] [PubMed] [Google Scholar]
- 9.Halperin AC, Rigotti NA. US public universities' compliance with recommended tobacco-control policies. J Am Coll Health. 2003;51:181–8. doi: 10.1080/07448480309596349. [DOI] [PubMed] [Google Scholar]
- 10.Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, et al. Bethesda (MD): Department of Health and Human Services (US), Public Health Service; 2000. Treating tobacco use and dependence: clinical practice guideline. [Google Scholar]
- 11.Thompson B, Thompson LA, Hymer JC, Halperin AC, Zbikowski S, Jaffe R. A qualitative study of attitudes, beliefs, and practices among 40 undergraduate smokers. J Am Coll Health. 2006. In press. [DOI] [PubMed]
- 12.Rimer BK. Interventions to increase breast screening. Lifespan and ethnicity issues. Cancer. 1994;74(1 Suppl):323–8. doi: 10.1002/cncr.2820741317. [DOI] [PubMed] [Google Scholar]
- 13.Thompson B, Montano DE, Mahloch J, Mullen M, Taylor V. Attitudes and beliefs toward mammography among women using an urban public hospital. J Health Care Poor Underserved. 1997;8:186–201. doi: 10.1353/hpu.2010.0320. [DOI] [PubMed] [Google Scholar]
- 14.Cox K. Stories as case knowledge: case knowledge as stories. Med Educ. 2001;35:862–6. doi: 10.1046/j.1365-2923.2001.01016.x. [DOI] [PubMed] [Google Scholar]
- 15.Dolmans DHJM, Snellen-Balendong H, Wolfhagen IHAP, van der Vleuten CPM. Seven principles of effective case design for a problem-based curriculum. Medical Teacher. 1997;19:185–9. [Google Scholar]
- 16.Schuwirth LW, Verheggen MM, van der Vleuten CP, Boshuizen HP, Dinant GJ. Do short cases elicit different thinking processes than factual knowledge questions do? Medical Education. 2001;35:348–56. doi: 10.1046/j.1365-2923.2001.00771.x. [DOI] [PubMed] [Google Scholar]
- 17.Fiore MC. Madison (WI): University of Wisconsin Medical School, Center for Tobacco Research and Intervention; [cited 2006 Mar 29]. Treating tobacco use and dependence. Available from: URL: http://www.ctri.wisc.edu\HC.Providers\healthcare.htm. [Google Scholar]
- 18.Morrison K, Banas J, Burke M. Understanding college students' salient attitudes and beliefs about smoking: distinctions between smokers, nonsmokers, and ex-smokers. Public Health Rev. 2003;31:95–109. [PubMed] [Google Scholar]
- 19.Weinstein ND, Marcus SE, Moser RP. Smokers' unrealistic optimism about their risk. Tob Control. 2005;14:55–9. doi: 10.1136/tc.2004.008375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hines D. Young smokers' attitudes about methods for quitting smoking: barriers and benefits to using assisted methods. Addict Behav. 1996;21:531–5. doi: 10.1016/0306-4603(95)00076-3. [DOI] [PubMed] [Google Scholar]