Abstract
Immunized BP2 mice developed an acute bronchoconstriction in vivo and airway muscle contraction in vitro in response to ovalbumin (OA) and these contractions were dose dependent.
Methysergide or atropine inhibited OA-induced bronchoconstriction in vivo and airway muscle contraction in vitro.
Neostigmine potentiated the OA-induced bronchoconstriction in vivo and airway muscle contraction in vitro of BP2 mice. This potentiation was markedly reduced by the administration of methysergide or atropine and when the two antagonists were administered together, the responses were completely inhibited.
Neostigmine also potentiated the serotonin (5-HT)- and acetylcholine (ACh)-induced bronchoconstriction and this potentiation was significantly reversed by atropine.
These results indicate that OA provokes a bronchoconstriction in immunized BP2 mice by stimulating the release of 5-HT, which in turn acts via the cholinergic mediator, ACh.
Keywords: Anaphylactic bronchoconstriction, mice, 5-HT, atropine, methysergide, ACh, neostigmine
Introduction
A number of studies have shown that lungs of rats (Church et al., 1972) and mice (Levitt & Mitzner, 1989) are responsive to 5-HT and ACh. In the rat, the response to 5-HT is mediated by a direct action of this agonist on airway smooth muscle (Pauwels et al., 1985). In contrast, in the mouse, the effect of 5-HT may be mediated by indirect mechanisms, such as the release of ACh. In fact, Levitt & Mitzner (1989) showed that in certain inbred strains of mice, which are very responsive to 5-HT, the bronchoconstriction induced by 5-HT was blocked by atropine. These data implicated an interaction of 5-HT with the nervous system and cholinergic mechanisms.
In sensitized mice, the ovalbumin dose-dependent contractions have been reported to be associated with the release of 5-HT (Iff & Vaz, 1966; Lima, 1967). Larsen and co-workers (1994) showed that repeated airway exposure to an allergen and the development of an IgE-responsive state lead to an altered neural control of airways with an increase in ACh release from nerve terminals. These in vitro data supported similar observations suggesting a link between elevated IgE titers in mice and airway hyper-responsiveness to contractile agents (Saloga et al., 1994; Weinmann et al., 1990). These results provided evidence for the hypothesis that an ovalbumin-induced bronchoconstriction in mice may be due to the direct contractile effect on airway muscle of ACh which is released by 5-HT. However, no studies have been performed which demonstrate that this series of physiological events occurred in any one of the proposed animal models of airway hyper-reactivity. Therefore, the aim of this investigation was to examine the ovalbumin induced bronchoconstriction in a mouse model where an elevated serum IgE titer and airway hyper-responsiveness have been reported (Eum et al., 1995).
Methods
Mice and immunization procedure
Female BP2 mice were obtained from the ‘Centre d'Elevage R. Janvier' (BP5, 53940 Le Genest Saint-Isle, France). Mice from 8–11 weeks were used in the experiments. These BP2 mice, a selection of Biozzi mice, produce high titers of antibodies (Biozzi et al., 1979) including IgE (Eum et al., 1995). These animals were derived from Swiss mice which were bred for the production of either high or low amounts of antibodies against selective antigens. After 16 generations the animals differed by 280-fold in mean agglutinin titers of antibodies produced against sheep erythrocytes (Biozzi et al., 1970).
Mice were immunized by injecting 0.4 ml of an OA solution (s.c. 250 μg ml−1) mixed with A1(OH)3 (4 mg ml−1) twice at an interval of 7 days. Mice were utilized after 1 week following the second injection.
Evaluation of bronchoconstriction in vivo and airway muscle contraction in vitro
Bronchoconstriction in vivo was measured by the methods described by Eum et al. (1995) and the contraction of isolated trachea in vitro by Norel et al. (1993). Briefly, in the in vivo experiments, immunized mice were anaesthetized with ethyl carbamate (i.p., 1.5 mg g−1). The trachea was cannulated and prepared for recording of dynamic compliance and airway resistance, by adapting the equipment of the computerized pulmonary analyser (Mumed PR800 system, U.K.) to mice airways at a tidal volume of 2.10−2 ml g−1 and a frequency of 100 breaths min−1. The animals were paralysed with pancuronium bromide (Pavulon®, 10 μg kg−1 i.v.) and airway resistance was calculated from the differential pressure between the airways and pleural cavity and the airflow. Control basal values of resistance were 500±20 (cm water (1 sec−1)−1) for n=20 animals (mean±s.e.mean). Depending on the protocol used, the data were expressed either as per cent increase of resistance (% increase), or as the increase above basal resistance. The per cent increase was calculated as follows: ((resistance after treatment–basal resistance)/basal resistance)×100%. In the protocols using neostigmine the data are shown as the resistance measured after treatment–basal resistance after neostigmine.
In the in vitro experiments, tracheal preparations were set up in the 10 ml organ baths containing Tyrode's solution (concentration in mM): NaCl 139.2, KCl 2.7, CaCl2 1.8, MgCl2 0.49, NaHCO3 11.9, NaH2PO4 0.4 and glucose 5.5; pH 7.4; gassed with 95% O2/5% CO2 under initial loads (1 g). These loads ensured that responses to contractile agonists were optimal. Isometric force displacement transducers (Narco F-60) and physiographs (Linseis) were used to record the changes in force. The tissues were allowed to equilibrate for 90 min and the bath fluid was exchanged every 15 min with fresh Tyrode's solution. After this period, all tracheal preparations were contracted with carbachol (3 μM). The tissues were washed with fresh Tyrode's solution and allowed to return passively to their resting tone. When resting tone was established, the preparations were incubated for 30 min in Tyrode's solution or Tyrode's solution containing either neostigmine (0.1 μM), atropine (1 μM) or methysergide (1 μM) and the response to an individual dose of OA or the relationship to 5-HT was determined.
Drug treatment
Drugs used to study the mechanisms of anaphylactic bronchonconstriction were injected in 0.9% NaCl (saline) through the cannulated jugular vein before OA injection. After the animals were prepared on the Mumed system (see ‘Evaluation of bronchoconstriction in vivo'), drugs were injected in the following order at 5 min intervals; ACh (80 μg kg−1), 5-HT (40 μg kg−1), saline or neostigmine (10 μg kg−1), 5-HT (40 μg kg−1), OA (50 mg kg−1) and ACh (80 μg kg−1). In order to determine the effects of each drug on OA-induced bronchoconstriction, either methysergide (200 μg kg−1), atropine (10 μg kg−1; 200 μg kg−1), or methysergide (200 μg kg−1)+atropine (10 μg kg−1) were injected after the injection of saline or neostigmine and prior to the second injection of 5-HT.
Materials
Ovalbumin (5× crystallized) was from Immunobiological (Costa Mesa, U.S.A.). Aluminium hydroxide was from Merck (Darmstadt, Germany). 5-Hydroxytryptamine (5-HT), ethyl carbamate, neostigmine, atropine, carbachol and acetylcholine were from Sigma (St. Louis, MO, U.S.A.). Pancuronium bromide (Pavulon) was from Organon Teknika (France). Methysergide was from Sandoz (Bâle, Swiss).
Statistical analysis
The results of each measurement are reported as means ±s.e.mean. Values significantly different between experimental and control groups were analysed by the Student's t-test (unpaired) and P values of less than 0.05 were considered to be significant.
Results
OA-induced bronchoconstriction and contractions of isolated trachea in immunized BP2 mice
Intravenous challenge with OA in immunized BP2 mice induced a dose-dependent augmentation of bronchial resistance, the maximal effect (approximately 160% augmentation) was reached at 50 mg kg−1 (Figure 1a). Saline-challenged mice (controls) showed no significant augmentation in bronchial resistance. The addition of OA to the organ bath containing trachea from immunized BP2 mice also induced dose-dependent contractions, which were approximately 40% of the carbachol effect (carbachol, 1 μM: 1.70±0.11 g, n=45: Figure 1b).
Figure 1.
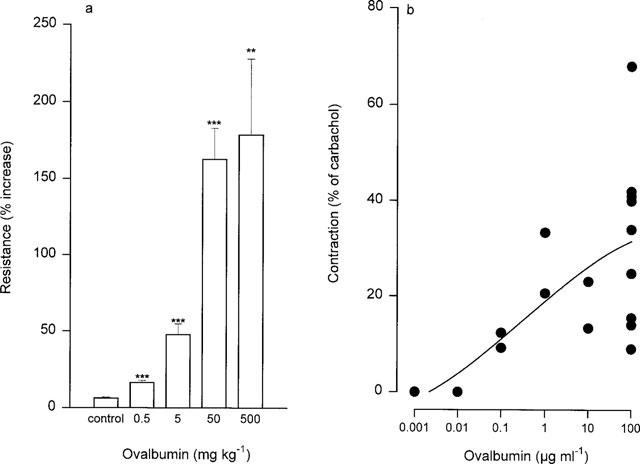
In immunized BP2 mice OA-induced bronchoconstriction in vivo (a) and airway muscle contraction in vitro (b). The values are in (a) means±s.e.mean derived from 4–20 mice whereas in (b) data were from individual animals. **P<0.01, ***P<0.001 compared with the control group (saline challenged mice).
Drug modulation of anaphylactic bronchoconstriction in vivo and on OA contractions of isolated trachea in vitro
Anaphylactic bronchoconstriction was markedly attenuated by methysergide (200 μg kg−1) and atropine (10 μg kg−1: Figure 2a). In addition, a higher dose of atropine (200 μg kg−1) completely abolished the OA response in these animals (n=3; data not shown). Neostigmine significantly potentiated the OA-induced bronchoconstriction (Figure 3). This potentiation was blocked by methysergide or atropine (10 μg kg−1) co-administered with neostigmine (Figure 3). When the drug combination of methysergide and atropine (10 μg kg−1) was administered, the anaphylactic bronchoconstriction in the presence of neostigmine was suppressed (data not shown). In isolated trachea, the OA-induced contraction was also inhibited by either methysergide or atropine (Figure 2b). This contraction was potentiated by neostigmine (approximately 100%, n=8) and the combined injection of methysergide and atropine inhibited this contraction (n=3; data not shown).
Figure 2.
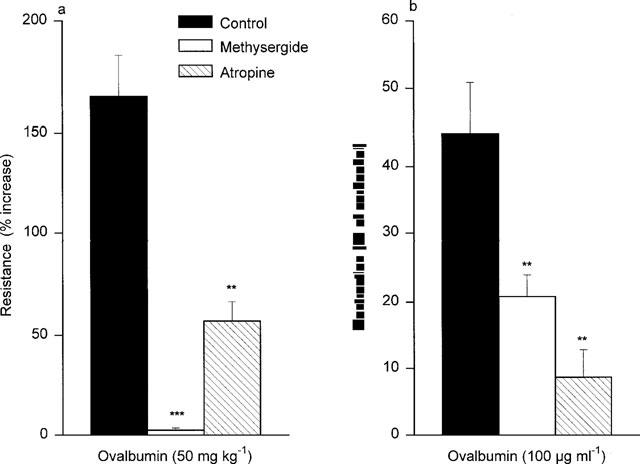
The effects of methysergide (200 μg kg−1) and atropine (10 μg kg−1) on ovalbumin induced bronchoconstriction in vivo (a) and on airway muscle contraction in vitro (b) in immunized BP2 mice. The values are means±s.e.mean derived from 5–10 mice. **P<0.01, ***P<0.001 compared with controls (OA challenged).
Figure 3.
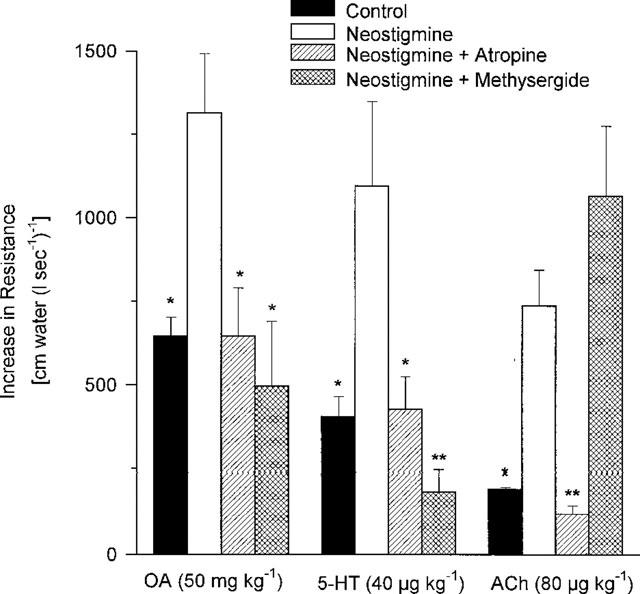
The effect of atropine and methysergide in combination with neostigmine on bronchoconstriction in vivo induced by different agents in immunized BP2 mice. Bronchoconstriction (control: agonist in absence of drugs) and in presence of neostigmine (10 μg kg−1) or neostigmine (10 μg kg−1)+atropine (10 μg kg−1) or neostigmine (10 μg kg−1)+methysergide (200 μg kg−1) are shown. The agonist challenges were: acetylcholine (ACh), serotonin (5-HT) and ovalbumin (OA). Values are means±s.e.mean derived from 4–6 mice. *P<0.05, **P<0.01 compared with neostigmine group.
Intravenous injection of neostigmine also potentiated the 5-HT-induced bronchoconstriction. This augmentation was blocked by either methysergide or atropine (Figure 3) and the simultaneous injection of both antagonists blocked the responses to 5-HT (data not shown). The ACh-induced bronchoconstriction was also increased by neostigmine and this was blocked by atropine, but not by methysergide (Figure 3). In isolated trachea, the 5-HT-induced contraction was also increased by neostigmine, but was not significantly inhibited by atropine (Figure 4).
Figure 4.
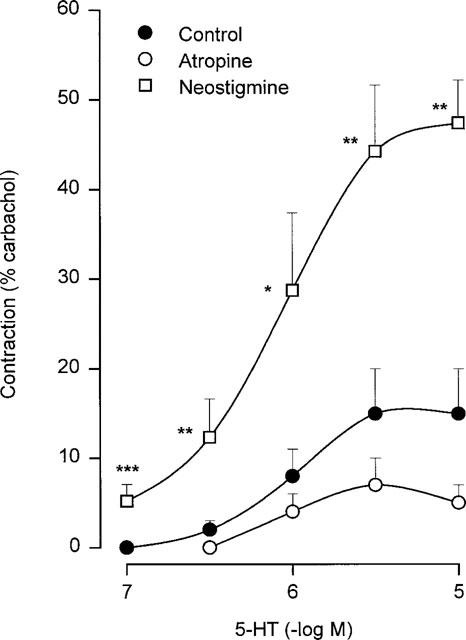
The 5-HT contractions in presence of either Tyrode's solution (Control), neostigmine (0.1 μM) or atropine (1 μM) in airway muscle derived from immunized BP2 mice. The values are means ±s.e.mean derived from 4–10 tracheal strips. *P<0.05, **P<0.01, ***P<0.001 compared with control group.
Discussion
OA produced a dose-dependent contraction of airway muscle both in vivo and in vitro (present report) in immunized BP2 mice. These airway muscle responses were blocked by treating the animals or tissues with methysergide or atropine, suggesting that 5-HT and ACh were involved in the con-traction. In addition, neostigmine potentiated the bronchoconstriction to OA, 5-HT and ACh, an effect markedly inhibited in each case by atropine. These data support the hypothesis that ovalbumin provoked a bronchoconstriction by stimulating the release of 5-HT and the direct contractile effect on airway smooth muscle was due to ACh. Thus the present study shows that in hyper-responsive BP2 mice, antigen-induced anaphylactic bronchoconstriction has a dual mediator release profile. While 5-HT and ACh measurements were not performed, the antagonist data indirectly support the involvement of both agents.
5-HT is released from mast cells (Kitamura, 1989) upon activation by antigen-specific IgE or by antigen binding T cell factors in mice. In rats 5-HT is the major mediator of antigen-induced anaphylactic bronchoconstriction (Church et al., 1972) and airway smooth muscle contraction (Nagase et al., 1995). In this study, methysergide suppressed the OA-induced bronchoconstriction, indicating that 5-HT is also a major mediator of OA-induced anaphylactic bronchoconstriction in BP2 mice. This observation is in agreement with that of Church et al. (1972) who also showed that antigen-induced bronchoconstriction is suppressed by methysergide in the rat. In BP2 mice (present report) methysergide also inhibited the OA-induced tracheal contractions in vitro. Church et al. (1972) initially demonstrated that atropine is inactive against the antigen-induced bronchoconstriction in the rat suggesting a direct action of this amine on the airway smooth muscle. OA-induced bronchoconstriction in vivo (present report) was significantly inhibited by atropine. Furthermore, atropine at a higher dose completely abolished the OA-induced constriction in vivo. These data suggest a cholinergic participation in the airway anaphylactic responses in BP2 mice. Previous reports have demonstrated that 5-HT facilitates cholinergic nerve-mediated contraction of the airways in a number of species including the rat (Aas, 1983; Szarek et al., 1993), mouse (Van-Oosterhout et al., 1991), the guinea-pig (Rizzo et al., 1993), and man (Takahashi et al., 1995). In mice, atropine inhibited the airway response to 5-HT (Levitt & Mitzner, 1989). These data suggest that 5-HT acts via a cholinergic pathway.
In the isolated trachea from Swiss mice, contractions were potentiated during electrical field stimulation, after the addition of 5-HT and this potentiation was suppressed by atropine (Van-Oosterhout et al., 1991). These results suggested that ACh was released by stimulation of 5-HT receptors in trachea from these mice, specifically since 5-HT failed to affect the response to exogenously applied ACh. A similar phenomenon has also been observed in human and guinea-pig airways by Takahashi et al. (1995). Such data strengthen the observation (present report) that OA-induced contractions of trachea were inhibited by atropine. Two observations further support a cholinergic pathway. First, neostigmine, a cholinesterase inhibitor, potentiated the anaphylactic bronchoconstriction of BP2 mice in vivo and in vitro, and this potentiation was markedly reduced by atropine. Secondly, neostigmine also potentiated 5-HT-induced bronchoconstriction and tracheal contraction in these mice, supporting ACh release upon stimulation of 5-HT.
Increased release of ACh induced by antigen challenge from airway parasympathetic nerve endings can contribute to increases in airway responsiveness (Larsen et al., 1994). These investigators measured the release of ACh in electrically stimulated tracheal preparation derived from sensitized mice. The quantities detected were markedly different than results observed in unsensitized mice. This increased release of ACh may be due either to the absence of inhibitory prejunctional M2 receptors or the presence of a 5-HT prejunctional facilitory receptor on the parasympatic neuronal fibres. Another possible explanation may be a decrease in cholinesterase activity. Previous studies have shown a modification of cholinesterase activity in dog (Mitchell et al., 1991) and pig (Taisne et al., 1997) airways related to the anaphylactic release of mediators. The findings (present report) suggest that ovalbumin-induced bronchoconstriction in BP2 mice may be due to the direct contractile effect on airway smooth muscle of ACh which is released by 5-HT.
Abbreviations
- ACh
Acetylcholine
- BP2 mice
Biozzi prepared hyperreactive mice
- OA
Ovalbumin
- 5-HT
Serotonin
References
- AAS P. Serotonin induced release of acetylcholine from neurons in the bronchial smooth muscle of the rat. Acta. Physiol. Scand. 1983;117:477–480. doi: 10.1111/j.1748-1716.1983.tb00026.x. [DOI] [PubMed] [Google Scholar]
- BIOZZI G., ASOFSKY R., LIEBERMAN R., STIFFEL C., MOUTON D., BENACERRAF B. Serum concentrations and allotypes of immunoglobulins in two lines of mice genetically selected for ‘high' or ‘low' antibody synthesis. J. Exp. Med. 1970;132:752–764. doi: 10.1084/jem.132.4.752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BIOZZI G., MOUTON D., SAINT'ANNA O.A., PASSOS H.C., GENNARI M., REIS M.H., FERREIRA V.C.A., HEUMANN A.M., BOUTHILLIER Y., IBANEZ O.M., STIFFEL C., SIQUEIRA M. Genetics of immunoresponsiveness to natural antigens in the mouse. Curr. Top. Microbiol. Immunol. 1979;85:31–98. [PubMed] [Google Scholar]
- CHURCH M.K., COLLIER H.O.J., JAMES W.L. The inhibition by dexamethasone and disodium cromoglycate of anaphylactic bronchoconstriction in the rat. Br. J. Pharmacol. 1972;46:56–65. doi: 10.1111/j.1476-5381.1972.tb06848.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EUM S.Y., HAILE S., LEFORT J., HUERRE M., VARGAFTIG B.B. Eosinophil recruitment into the respiratory epithelium following antigenic challenge in hyper-IgE mice is accompanied by interleukin-5-dependent bronchial hyperresponsiveness. Proc. Natl. Acad. Sci., U.S.A. 1995;92:12290–12294. doi: 10.1073/pnas.92.26.12290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IFF E.T., VAZ N.M. Mechanisms of anaphylaxis in the mouse. Int. Arch. Allergy. 1966;30:313–322. doi: 10.1159/000229815. [DOI] [PubMed] [Google Scholar]
- KITAMURA Y. Heterogeneity of mast cells and phenotypic change between subpopulations. Ann. Rev. Immunol. 1989;7:59–66. doi: 10.1146/annurev.iy.07.040189.000423. [DOI] [PubMed] [Google Scholar]
- LARSEN G.L., FAME T.M., RENZ H., LOADER J.E., GRAVES J., HILL M., GELFAND E.W. Increased acetylcholine release in tracheas from allergen-exposed IgE-immune mice. Am. J. Physiol. 1994;266:L263–L270. doi: 10.1152/ajplung.1994.266.3.L263. [DOI] [PubMed] [Google Scholar]
- LEVITT R.C., MITZNER W. Autosomal recessive inheritance of airway hyperreactivity to 5-hydroxytryptamine. J. Appl. Physiol. 1989;67:1125–1132. doi: 10.1152/jappl.1989.67.3.1125. [DOI] [PubMed] [Google Scholar]
- LIMA A.O. Pharmacologically active substances released during anaphylactic shock in the mouse. Int. Arch. Allergy. 1967;32:46–54. doi: 10.1159/000229915. [DOI] [PubMed] [Google Scholar]
- MITCHELL R.W., KELLY E., LEFF A.R. Reduced activity of acetylcholine-esterase in canine tracheal smooth muscle homogenates after active immune-sensitization. Am. J. Respir. Cell Mol. Biol. 1991;5:56–62. doi: 10.1165/ajrcmb/5.1.56. [DOI] [PubMed] [Google Scholar]
- NAGASE T., FUKUCHI Y., DALLAIRE M.J., MARTIN J.G., LUDWIG M.S. In vitro airway and tissue response to antigen in sensitized rats: role of serotonin and leukotriene D4. Am. J. Respir. Crit. Care Med. 1995;152:81–86. doi: 10.1164/ajrccm.152.1.7599867. [DOI] [PubMed] [Google Scholar]
- NOREL X., ANGRISANI M., LABAT C., GORENNE I., DULMET E., ROSSI F., BRINK C. Degradation of acetylcholine in human airways: role of butyrylcholinesterase. Br. J. Pharmacol. 1993;108:914–919. doi: 10.1111/j.1476-5381.1993.tb13486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PAUWELS R., VAN DER STRAETEN M., WEYNE J., BAZIN H. Genetics factors in non-specific bronchial reactivity in rats. Eur. J. Respir. Dis. 1985;66:98–104. [PubMed] [Google Scholar]
- RIZZO C.A., KREUTNER W., CHAPMAN R.W. 5-HT3 receptors augments neuronal, cholinergic contractions in guinea-pig trachea. Eur. J. Pharmacol. 1993;234:109–112. doi: 10.1016/0014-2999(93)90712-q. [DOI] [PubMed] [Google Scholar]
- SALOGA J., RENZ H., LARSEN G.L., GELFAND E.W. Increased airways responsiveness in mice depends on local challenge with antigen. Am. J. Respir. Crit. Care Med. 1994;149:65–70. doi: 10.1164/ajrccm.149.1.8111600. [DOI] [PubMed] [Google Scholar]
- SZAREK J.L., ZHANG J.Z., GRUETTER C.A. 5-HT2 receptors augment nerve-mediated contraction of rat bronchi. Eur. J. Pharmacol. 1993;231:339–346. doi: 10.1016/0014-2999(93)90108-t. [DOI] [PubMed] [Google Scholar]
- TAISNE C., NOREL X., WALCH L., LABAT C., VERRIEST C., MAZMANIAN G.M., BRINK C. Cholinesterase activity in pig airways and epithelial cells. Fundam. Clin. Pharmacol. 1997;11:201–205. doi: 10.1111/j.1472-8206.1997.tb00186.x. [DOI] [PubMed] [Google Scholar]
- TAKAHASHI T., WARD J.K., TADJKARIMI S., YACOUB M.H., BARNES P.J., BELVISI M.G. 5-Hydroxytryptamine facilitates cholinergic bronchoconstriction in human and guinea-pig airways. Am. J. Crit. Care Med. 1995;152:377–380. doi: 10.1164/ajrccm.152.1.7599849. [DOI] [PubMed] [Google Scholar]
- VAN OOSTERHOUT A.J.M., HOFMANN G., WOUTERSEN-VAN NIJNANTEN F.M.A., NIJKAMP F.P. 5-HT1-like receptors mediate potentiation of cholinergic nerve-mediated contraction of isolated mouse trachea. Eur. J. Pharmacol. 1991;209:237–244. doi: 10.1016/0014-2999(91)90175-p. [DOI] [PubMed] [Google Scholar]
- WEINMANN G.G., BLACK C.M., LEVITT R.C., HIRSHMAN C.A. In vitro tracheal responses from mice chosen for in vivo lung cholinergic sensitivity. J. Appl. Physiol. 1990;69:274–280. doi: 10.1152/jappl.1990.69.1.274. [DOI] [PubMed] [Google Scholar]


