Abstract
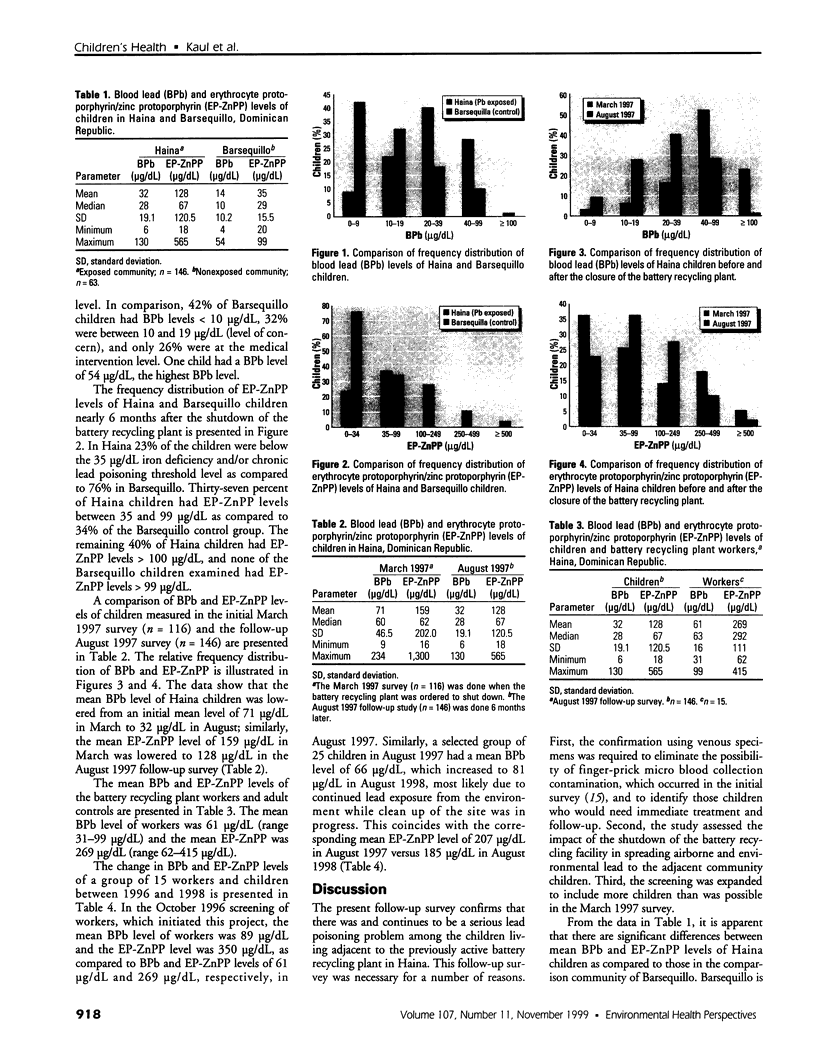
In August 1997 we performed a follow-up survey of 146 lead-poisoned children from a community near a previously active auto battery recycling smelter in Haina near Santo Domingo, Dominican Republic. Our follow-up survey confirmed a severe incidence of elevated blood lead (BPb) and erythrocyte protoporphyrin/zinc protoporphyrin (EP-ZnPP) levels. The mean BPb level was 32 micrograms/dL and the mean EP-ZnPP level was 128 micrograms/dL. The frequency distribution of BPb showed that only 9% of the children had BPb levels below the currently acceptable 10 micrograms/dL threshold level, 23% had between 10 and 19 micrograms/dL, 40% had between 20 and 39 micrograms/dL, 27% had between 40 and 99 micrograms/dL, and the remainder had > 100 micrograms/dL. These findings are significantly greater than the mean BPb and EP-ZnPP levels of 14 and 35 micrograms/dL, respectively, in a comparison group of 63 children in Barsequillo, 4 miles away. BPb frequency distributions for these groups were < 10 micrograms/dL (42%), 10-19 micrograms/dL (32%), and 20-39 micrograms/dL (16%); in the remaining 10%, BPb levels were between 40 and 99 micrograms/dL. Similarly, the corresponding frequency distribution of EP-ZnPP levels in Haina children were proportional to the severity of lead poisoning and significantly higher than those of the Barsequillo comparison group. This study reveals that at least 28% of Haina children require immediate treatment; of these, 5% with lead levels > 70 micrograms/dL are also at risk for severe neurologic sequelae, and urgent action is imperative.
Full text
PDF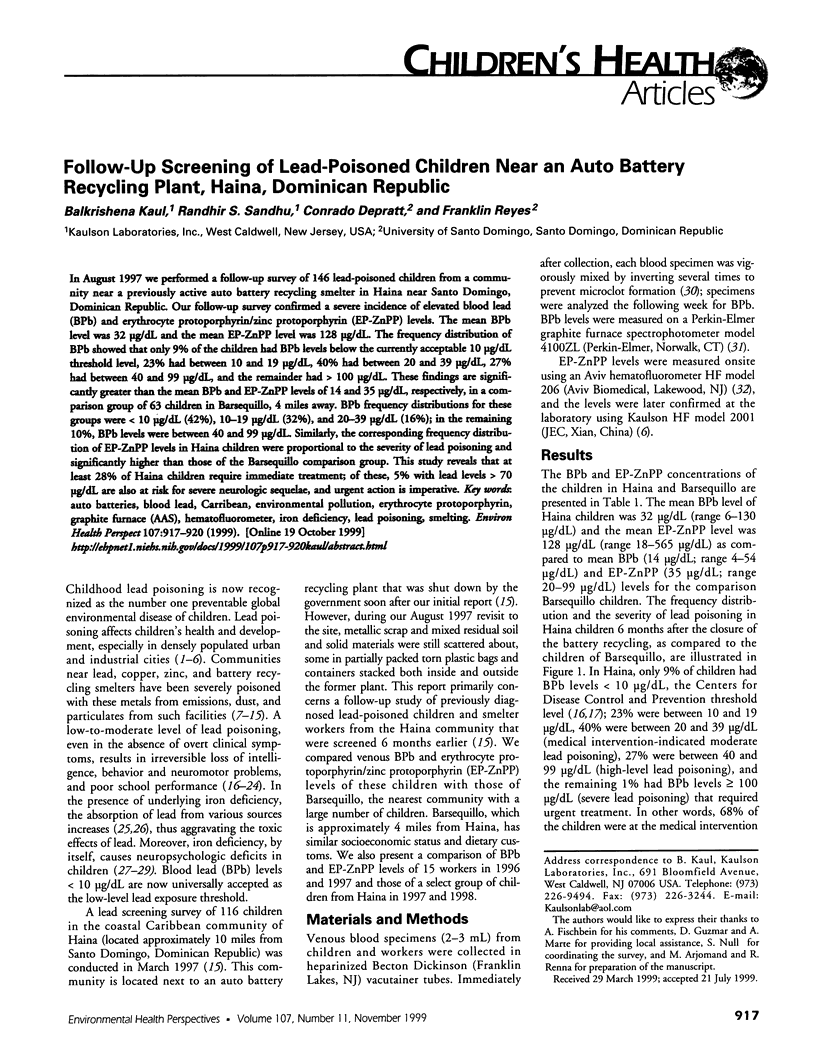


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bellinger D. C., Stiles K. M., Needleman H. L. Low-level lead exposure, intelligence and academic achievement: a long-term follow-up study. Pediatrics. 1992 Dec;90(6):855–861. [PubMed] [Google Scholar]
- Bellinger D., Leviton A., Waternaux C., Needleman H., Rabinowitz M. Longitudinal analyses of prenatal and postnatal lead exposure and early cognitive development. N Engl J Med. 1987 Apr 23;316(17):1037–1043. doi: 10.1056/NEJM198704233161701. [DOI] [PubMed] [Google Scholar]
- Bellinger D., Sloman J., Leviton A., Rabinowitz M., Needleman H. L., Waternaux C. Low-level lead exposure and children's cognitive function in the preschool years. Pediatrics. 1991 Feb;87(2):219–227. [PubMed] [Google Scholar]
- Brody D. J., Pirkle J. L., Kramer R. A., Flegal K. M., Matte T. D., Gunter E. W., Paschal D. C. Blood lead levels in the US population. Phase 1 of the Third National Health and Nutrition Examination Survey (NHANES III, 1988 to 1991) JAMA. 1994 Jul 27;272(4):277–283. doi: 10.1001/jama.272.4.277. [DOI] [PubMed] [Google Scholar]
- Graziano J. H., Popovac D., Factor-Litvak P., Shrout P., Kline J., Murphy M. J., Zhao Y. H., Mehmeti A., Ahmedi X., Rajovic B. Determinants of elevated blood lead during pregnancy in a population surrounding a lead smelter in Kosovo, Yugoslavia. Environ Health Perspect. 1990 Nov;89:95–100. doi: 10.1289/ehp.908995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartwell T. D., Handy R. W., Harris B. S., Williams S. R., Gehlbach S. H. Heavy metal exposure in populations living around zinc and copper smelters. Arch Environ Health. 1983 Sep-Oct;38(5):284–295. doi: 10.1080/00039896.1983.10544008. [DOI] [PubMed] [Google Scholar]
- Kaul B., Slavin G., Davidow B. Free erythrocyte protoporphyrin and zinc protoporphyrin measurements compared as primary screening methods for detection of lead poisoning. Clin Chem. 1983 Aug;29(8):1467–1470. [PubMed] [Google Scholar]
- Landrigan P. J., Gehlbach S. H., Rosenblum B. F., Shoults J. M., Candelaria R. M., Barthel W. F., Liddle J. A., Smrek A. L., Staehling N. W., Sanders J. F. Epidemic lead absorption near an ore smelter. The role of particulate lead. N Engl J Med. 1975 Jan 16;292(3):123–129. doi: 10.1056/NEJM197501162920302. [DOI] [PubMed] [Google Scholar]
- Lozoff B., Wolf A. W., Jimenez E. Iron-deficiency anemia and infant development: effects of extended oral iron therapy. J Pediatr. 1996 Sep;129(3):382–389. doi: 10.1016/s0022-3476(96)70070-7. [DOI] [PubMed] [Google Scholar]
- Matte T. D., Figueroa J. P., Ostrowski S., Burr G., Jackson-Hunt L., Keenlyside R. A., Baker E. L. Lead poisoning among household members exposed to lead-acid battery repair shops in Kingston, Jamaica. Int J Epidemiol. 1989 Dec;18(4):874–881. doi: 10.1093/ije/18.4.874. [DOI] [PubMed] [Google Scholar]
- Mushak P. New directions in the toxicokinetics of human lead exposure. Neurotoxicology. 1993 Summer-Fall;14(2-3):29–42. [PubMed] [Google Scholar]
- Needleman H. L., Gatsonis C. A. Low-level lead exposure and the IQ of children. A meta-analysis of modern studies. JAMA. 1990 Feb 2;263(5):673–678. [PubMed] [Google Scholar]
- Roberts T. M., Hutchinson T. C., Paciga J., Chattopadhyay A., Jervis R. E., VanLoon J., Parkinson D. K. Lead contamination around secondary smelters: estimation of dispersal and accumulation by humans. Science. 1974 Dec 20;186(4169):1120–1123. doi: 10.1126/science.186.4169.1120. [DOI] [PubMed] [Google Scholar]
- Ruff H. A., Markowitz M. E., Bijur P. E., Rosen J. F. Relationships among blood lead levels, iron deficiency, and cognitive development in two-year-old children. Environ Health Perspect. 1996 Feb;104(2):180–185. doi: 10.1289/ehp.96104180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sargent J. D. The role of nutrition in the prevention of lead poisoning in children. Pediatr Ann. 1994 Nov;23(11):636–642. doi: 10.3928/0090-4481-19941101-12. [DOI] [PubMed] [Google Scholar]
- Sciarillo W. G., Alexander G., Farrell K. P. Lead exposure and child behavior. Am J Public Health. 1992 Oct;82(10):1356–1360. doi: 10.2105/ajph.82.10.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silbergeld EK. The International Dimensions of Lead Exposure. Int J Occup Environ Health. 1995 Oct;1(4):336–348. doi: 10.1179/oeh.1995.1.4.336. [DOI] [PubMed] [Google Scholar]
- Steele M. J., Beck B. D., Murphy B. L., Strauss H. S. Assessing the contribution from lead in mining wastes to blood lead. Regul Toxicol Pharmacol. 1990 Apr;11(2):158–190. doi: 10.1016/0273-2300(90)90019-8. [DOI] [PubMed] [Google Scholar]
- Wasserman G. A., Graziano J. H., Factor-Litvak P., Popovac D., Morina N., Musabegovic A., Vrenezi N., Capuni-Paracka S., Lekic V., Preteni-Redjepi E. Consequences of lead exposure and iron supplementation on childhood development at age 4 years. Neurotoxicol Teratol. 1994 May-Jun;16(3):233–240. doi: 10.1016/0892-0362(94)90044-2. [DOI] [PubMed] [Google Scholar]
- Wasserman G., Graziano J. H., Factor-Litvak P., Popovac D., Morina N., Musabegovic A., Vrenezi N., Capuni-Paracka S., Lekic V., Preteni-Redjepi E. Independent effects of lead exposure and iron deficiency anemia on developmental outcome at age 2 years. J Pediatr. 1992 Nov;121(5 Pt 1):695–703. doi: 10.1016/s0022-3476(05)81895-5. [DOI] [PubMed] [Google Scholar]