In The Health of Canadians — the Federal Role, which is better known as the Kirby Report, the Standing Senate Committee on Social Affairs, Science and Technology said it was “convinced that addressing the issues relating to human resources in health care must be amongst the top health care policy priorities for all levels of government.”1 The Kirby Report is not alone. In A Framework for Reform: Report of the Premier's Advisory Council on Health for Alberta, better known as the Mazankowski Report, it is asserted that “we need to do a better job of anticipating future demands and changes to the [health care] professions, and matching that with capacity in post-secondary education and training programs.”2 It states further (p. 33) that “while it is difficult to predict future supply and demand of health providers, many suggest we should be able to do a better job of preparing integrated health workforce plans and anticipating future needs.”
We are concerned here with anticipating future needs — more specifically with the effects of population change on future requirements for physicians and the services that they provide. An important aspect of population change is population aging, something that has attracted much attention and is often associated in the public mind and popular press with increases in health care costs and shortages of personnel. In fact, population aging has had little to do with either. (Most of the growth in health care budgets and resources has been associated not with increased numbers of older people but with other factors, including increases in the average number of services provided to patients at each age.3,4,5) Nevertheless, the aging process continues and will be a fact of life in the coming decades. What that will mean for the health care system is thus an important consideration in predicting future requirements. But increases in population size are also important; we have shown elsewhere5 that, overall, the effects of population growth on physician requirements have exceeded the effects of aging, and that is likely to be the case for the next 3 decades. On the other hand, as we emphasize here, aging will play an important role in determining how future requirements are distributed among categories of physician.
The way in which physician services are currently used is reflected in what we term age–utilization profiles. The profiles that we have developed are based on Ontario Health Insurance Plan (OHIP) payments made to fee-for-service physicians. They show, as a good approximation, how (on average) physicians allocate their time to the population at different ages. (In the year to which the profiles relate, fee-for-service payments accounted for 98% of total payments to physicians in Ontario.)
It is no surprise that the profiles reveal that average service requirements increase with age for most categories of physician. For example, women's use of general practitioner time is about twice as great at the age of 80 years as at 30, and use by men is 4 times as great at 80 years as at 30. There are exceptions, such as pediatric and obstetric/gynecological services. Psychiatric services, which are provided in large part to middle-aged patients (especially women), are another. Nonetheless, for most categories of physician the typical pattern is one in which use increases with a patient's age, at least until the very oldest ages. A peak typically occurs somewhere between when patients are in their early seventies and their mid-eighties for both medical and surgical specialties, which is followed by a decline at more advanced ages. For general practice, increases are observed even up to the oldest age group. (The profiles and further analyses are provided elsewhere;6,7 other related studies using profiles from an earlier period are available also.8,9,10)
No one expects the profiles to remain fixed, of course. Changes in medical technology and practice, how service delivery is shared across physician categories and with nonphysician health care professionals, and other factors will affect requirements as they are perceived in the future. But how the profiles will change cannot be known, and it is natural to ask how many physicians will be required in the years ahead — and, for comparison, how many would have been required in the past — to meet population needs if current service delivery patterns are maintained.
By combining the profiles with population numbers, past or projected, we can assess the “pure” effects of population change on requirements — “pure” in the sense that all other factors are held constant. In that way, we have calculated requirements both historically (back to 1970) and for the future (to 2030, with alternative population projections). All projections indicate that the population will continue to grow (though more slowly than in the past) and to age. What are the implications for physician requirements?
Three points stand out. The first is that, as a result of population change alone, overall requirements are likely to increase less in the future than in the past. In the 3 decades ending in 2000, requirements rose by 72%; in the next 3 they will increase by only 50% in our “standard” projection, which represents a continuation of current demographic trends, and at most by 59% in our “slower-aging” projection, which assumes a return to somewhat higher fertility. This contrasts with widely held views and concerns about the effects of population aging on the health care system, and in particular on future physician requirements.
The second point is that, historically, population growth has been more important than population aging in accounting for overall increases in requirements. (In our introduction, we noted that population aging has had little to do with the observed increase in physician numbers. Here we observe that the overall effect of population change — growth as well as aging, but mostly growth — was to increase requirements by 72% between 1970 and 2000. By comparison, the actual number of physicians — “active civilian physicians, excluding interns and residents,” reported in the Southam Medical Database, available through the Canadian Institute for Health Information — increased by 116%.)
Third, population growth is likely to continue to dominate aging in its impact on requirements. In our standard projection the overall increase in requirements declines decade by decade, and population aging becomes relatively more important. Even so, by the third decade of this century, growth still accounts for more than six-tenths of the total.
The effects of population change on requirements by category of physician are shown in Fig. 1, for the standard projection. There are 19 categories: 8 medical, 9 surgical, plus general practice and laboratory medicine. Although the projected effect of population change is to increase requirements by some 50% between 2000 and 2030 (as indicated by the solid “all categories” bar in the lower panel), there is much variation among the categories. For example, the requirements for thoracic and cardiovascular surgery show the most rapid growth (more than 90%), followed closely by ophthalmology (86%) and urology (80%). The slowest growth is projected for pediatrics (8%), obstetrics and gynecology (18%), and psychiatry (26%). The upper panel emphasizes that the increases in requirements were much greater in the earlier period; indeed, that was true not only overall but for every category. Fig. 1 shows also that the population-induced increases in requirements for some categories in the projection period are much smaller than before. (The much slower growth in obstetrics and gynecology and psychiatry are conspicuous examples.)
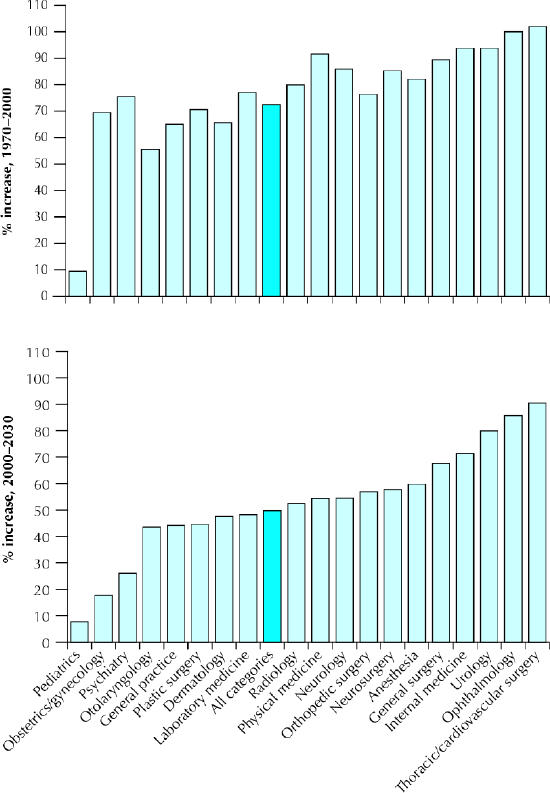
Fig. 1: Percent increase in physician requirements resulting from population change, by category of physician: historical, 1970–2000 (upper panel), and projected, 2000–2030 (lower panel).
To summarize, the overall requirements for physicians in consequence of population change alone are almost certain to increase by less in the future than in the past. That may seem surprising, given the continued aging of the population. In fact, whereas population aging can be confidently anticipated, and with it an increase in requirements for physicians, the rate of population growth is likely to decline, and that will compensate. Population growth accounted for more than seven-tenths of the overall population-related increase in requirements in the period 1970–2000, population aging for less than three-tenths. Unless there is a further substantial reduction in already low fertility levels, the decline in overall physician requirements associated with slower population growth will more than offset the increase associated with continued population aging. At the level of individual categories of physician, we find considerable variation in the effects of population change on requirements, both historically and in our 30-year projection. That is something that medical schools and their students may wish to take into account in their planning and decision-making.
Acknowledgments
We acknowledge with appreciation the help of Christine Feaver, who carried out the calculations reported in this paper, and the Canadian Institute for Health Information, which provided us with unpublished tabulations of the age–sex distributions of expenditures on physician services.
Footnotes
This article has been peer reviewed.
Contributors: Frank Denton, Amiram Gafni and Byron Spencer worked together in formulating the basic concepts for the paper, in specifying the simulation experiments to be conducted, and in drafting and revising the manuscript.
The work was carried out as part of the SEDAP (Social and Economic Dimensions of an Aging Population) Research Program supported by the Social Sciences and Humanities Research Council of Canada, Statistics Canada and the Canadian Institute for Health Information.
Competing interests: None declared.
Correspondence to: Dr. Byron G. Spencer, Department of Economics, McMaster University, Hamilton ON L8S 4M4; fax 905 521-8232; spencer@mcmaster.ca
References
- 1.Kirby MJL. The health of Canadians — the federal role. Interim report of the Standing Senate Committee on Social Affairs, Science and Technology. vol. 1. Ottawa: Senate of Canada; 2001. p. 91. Available: www.parl.gc.ca/37/1/parlbus/commbus/senate/com-E/SOCI-E/rep-e/repintmar01-e.htm (accessed 2003 May 12).
- 2.Mazankowski D. A framework for reform: report of the Premier's Advisory Council on Health for Alberta. 2001. p. 35. Available: www.premiersadvisory.com (accessed 2003 Mar 31).
- 3.Barer ML, Evans RG, Hertzman C. Demographic change and the cost of publicly funded health care. Can J Aging 1995;14:193-224.
- 4.Evans RG, McGrail KM, Morgan SG, Barer ML, Hertzman C. Apocalypse no: population aging and the future of health care systems. Can J Aging 2001; 20: (Suppl 1):160-91.
- 5.Denton FT, Byron GS. Demographic change and the cost of publicly funded health care. Can J Aging 1995;14,174-92.
- 6.Denton FT, Gafni A, Spencer BG. Population change and the requirements for physicians: the case of Ontario. Can Public Policy 2001;27:469-85.
- 7.Denton FT, Gafni A, Spencer BG. Exploring the effects of population change on the costs of physician services. J Health Econ 2002;21:781-803. [DOI] [PubMed]
- 8.Denton FT, Gafni A, Spencer BG. System for Health Area Resource Planning (SHARP): an application to Ontario medical school enrolment. CMAJ 1994;151(1):39-45. [PMC free article] [PubMed]
- 9.Denton FT, Gafni G, Spencer BG. Physician supply in Ontario: further observations on SHARP and the SHARP projections. CMAJ 1995;152(9):1389-91. [PMC free article] [PubMed]
- 10.Denton FT, Gafni A, Spencer BG. The SHARP way to plan health care services: a description of the system and some illustrative applications in nursing human resource planning. Socioecon Plann Sci 1995;29:125-37.


