Abstract
Avian influenza A H5N1 viruses continue to spread globally among birds, resulting in occasional transmission of virus from infected poultry to humans. Probable human-to-human transmission has been documented rarely, but H5N1 viruses have not yet acquired the ability to transmit efficiently among humans, an essential property of a pandemic virus. The pandemics of 1957 and 1968 were caused by avian–human reassortant influenza viruses that had acquired human virus-like receptor binding properties. However, the relative contribution of human internal protein genes or other molecular changes to the efficient transmission of influenza viruses among humans remains poorly understood. Here, we report on a comparative ferret model that parallels the efficient transmission of H3N2 human viruses and the poor transmission of H5N1 avian viruses in humans. In this model, an H3N2 reassortant virus with avian virus internal protein genes exhibited efficient replication but inefficient transmission, whereas H5N1 reassortant viruses with four or six human virus internal protein genes exhibited reduced replication and no transmission. These findings indicate that the human virus H3N2 surface protein genes alone did not confer efficient transmissibility and that acquisition of human virus internal protein genes alone was insufficient for this 1997 H5N1 virus to develop pandemic capabilities, even after serial passages in a mammalian host. These results highlight the complexity of the genetic basis of influenza virus transmissibility and suggest that H5N1 viruses may require further adaptation to acquire this essential pandemic trait.
Keywords: transmissibility, pandemic virus properties, pandemic influenza, animal model, receptor specificity
Highly pathogenic avian influenza (HPAI) H5N1 viruses are now enzootic in several countries and are presently undergoing unprecedented geographic expansion among wild and domestic birds. Since 1997, when HPAI H5N1 viruses first emerged in Hong Kong to cause human respiratory illness and death, >200 laboratory-confirmed human infections have been reported, primarily as a result of transmission of the H5N1 virus from domestic poultry to humans (1–4). Despite limited instances of probable human-to-human transmission (5, 6), H5N1 viruses have not yet acquired the ability to transmit efficiently among humans. The viral properties that confer transmissibility of influenza viruses among humans, and mammalian species in general, remains poorly understood, yet are clearly key factors that determine whether a novel subtype introduced into an immunologically naïve human population will result in a pandemic. The continuing occurrence of human H5N1 infections underscores the ongoing public health threat and the urgent need to better understand the potential of H5N1 viruses to acquire properties that would confer efficient transmissibility among humans.
Pandemic viruses of the 20th century arose in two ways. The 1918 H1N1 virus likely derived all eight genes from an avian virus and accumulated mutations during adaptation in a mammalian host (7, 8). In contrast, the H2N2 and H3N2 viruses that caused pandemics in 1957 and 1968, respectively, were the result of reassortment between avian and human influenza A viruses, acquiring the neuraminidase (NA) and/or hemagglutinin (HA), and PB1 gene from an avian virus and other genes from the previously circulating human strain (9). However, the earliest human H2 and H3 isolates differed from their avian counterparts in key receptor-binding residues that resulted in preferred binding of the human virus HA to sialic acid (SA) α2,6 receptors, suggesting that a shift from avian virus SA α2,3 to human virus SA α2,6 receptor-binding specificity is critical for efficient replication and spread of a pandemic strain (10). H5N1 viruses isolated from humans to date possess all eight gene segments that are entirely avian in origin, and with only a few exceptions, have retained a receptor-binding site sequence in the HA that is typical of the avian virus preference for binding SA α2,3 (11–13). Therefore, despite considerable genetic diversity in H5N1 viruses isolated from humans since 1997, no consistent adaptation to the human host has been identified (14).
Person-to-person transmission of human influenza viruses occurs either through contact (direct or indirect) or respiratory droplet (droplet or droplet nuclei) transmission (15). Although the exact contribution of each of these modes of transmission is not known, transmission of respiratory droplets, expelled when infected persons cough or sneeze, is likely the major mode of sustained viral spread in community settings during epidemics and pandemics (15). Several animal models have been used to investigate factors that contribute to influenza virus transmissibility (16–19). Ferrets, like humans, have a predominance of α2,6 SA and a lesser amount of α2,3 SA on respiratory tract epithelial cells, exhibit preferential binding of H5N1 viruses in the lower respiratory tract similar to humans (20–24), and have been used previously to investigate transmissibility of human influenza viruses (17–19, 25). Here, we conduct both contact and respiratory droplet transmission studies in ferrets to establish a model that reflects the relative transmissibility of H3N2 and H5N1 viruses in humans. We use this model to evaluate the transmissibility of various avian H5N1 and human H3N2 reassortant viruses in ferrets to assess the pandemic potential of such viruses. All H5N1 avian–human reassortant viruses generated exhibited reduced replication efficiency compared with the parental H5N1 virus and were not capable of efficient respiratory droplet transmission between ferrets.
Results
Transmissibility of H3N2 Human Influenza Viruses.
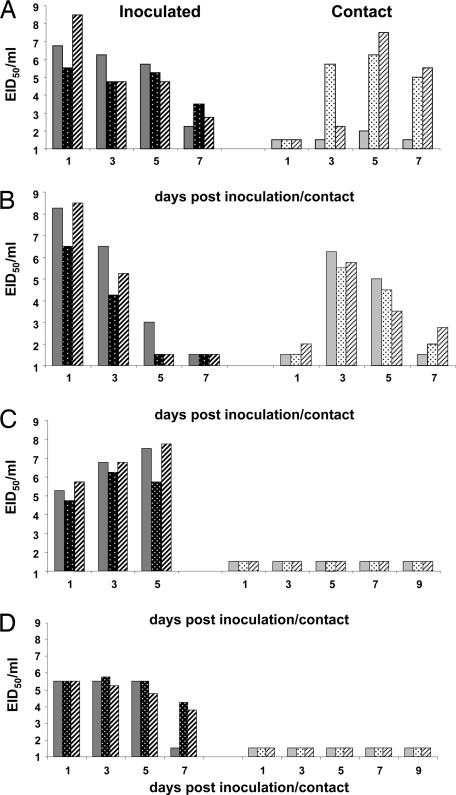
To establish our ferret transmission model, we first evaluated the ability of two human H3N2 influenza viruses, A/Panama/2007/99 (Pan99) and A/Victoria/3/75 (Vic75), to undergo efficient respiratory droplet transmission by housing ferrets in adjacent cages, each with a perforated side wall that prevented direct contact but allowed spread of virus through the air. Three ferrets were inoculated intranasally (i.n.) with 104 50% ferret infectious dose (FID50) of Pan99 [105.2 50% egg infectious dose (EID50)] or Vic75 (104.5 EID50), and 24 h later three naive ferrets were each placed in a transmission cage adjacent to an inoculated ferret. Inoculated ferrets achieved peak mean titers in nasal washes of 6.9 ± 1.5 or 7.8 ± 1.1 log10 EID50/ml, respectively on day 1 postinoculation (p.i.) (Fig. 1 A and B); and exhibited modest signs of illness, including sneezing beginning on day 2 p.i. (Table 1). Both viruses were efficiently transmitted to each of the three contact ferrets by day 3 or 5 postcontact (p.c.) as demonstrated by detection of virus in nasal secretions and seroconversion for hemagglutination inhibition (HI) antibody 14 days p.c. in all contact animals (Fig. 1 A and B and Table 1). These data indicate that both human H3N2 viruses were efficiently transmitted from inoculated to naive ferrets in a situation that did not allow for direct contact between animals or indirect contact with virus-contaminated food or surfaces. These results reflect the general transmissibility of human H3N2 influenza viruses in humans by respiratory droplets.
Fig. 1.
Respiratory droplet transmissibility of H3N2 and H5N1 viruses. Three ferrets were inoculated with 104 FID50 of Pan99 (A), Vic75 (B), HK486 (C), or 106 EID50 of HK213 (D), and nasal washes were collected from each ferret on alternating days for at least 5 days p.i. (Left). Twenty-four hours after inoculation, a naive ferret was placed in each of the adjacent cages with adjoining perforated walls that only allowed transfer of virus between ferrets through the air. Nasal washes were collected from the contact ferrets on alternating days for at least 7 days p.c. (Right). Solid, dotted, and hatched bars each represent a separate ferret pair. The limit of virus detection was 101.5 EID50/ml.
Table 1.
Clinical signs, virus replication, seroconversion, and transmission in ferrets inoculated with WT influenza viruses
| Virus | Subtype | No. of inoculated ferrets/total number |
No. of contact ferrets/total number |
Transmission | ||||
|---|---|---|---|---|---|---|---|---|
| Clinical signs |
Peak mean log10 nasal wash titer (day p.i.) | Seroconversion (HI titer range)† | Virus detected in nasal wash | Seroconversion (HI titer range)† | ||||
| Weight loss (%)* | Sneezing (day of onset) | |||||||
| Pan99 | H3N2 | 3/3 (7.9) | 3/3 (2) | 6.9 (1) | 3/3 (1,280–2,560) | 3/3 | 3/3 (20–640) | Efficient (RD) |
| Vic75 | H3N2 | 3/3 (9.5) | 3/3 (2) | 7.8 (1) | 3/3 (160–320) | 3/3 | 3/3 (40–1,280) | Efficient (RD) |
| HK486 | H5N1 | 3/3 (16.5) | 1/3 (4) | 7.0 (5) | 2/2‡ (1,280) | 0/3 | 2/3 (160–320) | Inefficient (RD) |
| HK213 | H5N1 | 3/3 (8.8) | 0/3 | 5.5 (1, 3) | 2/2‡ (1,280) | 0/3 | 0/3 | None (RD) |
| Indon05 | H5N1 | 3/3 (18.8) | 0/3 | 6.6 (3) | ND§ | 0/3 | 0/3 | None (C) |
| VN30408 | H5N1 | 3/3 (9.9) | 0/3 | 5.2 (3) | 3/3 (40–160) | 0/3 | 0/3 | None (C) |
RD, respiratory droplet; C, contact transmission.
*The percentage mean maximum weight loss is shown.
†HI assays were performed with homologous virus and RBCs derived from either horse for H5 viruses or turkey for H3 viruses.
‡Only two ferrets survived and were tested.
§ND, not determined because no ferrets survived beyond 7 days p.i.
Transmissibility of H5N1 Avian Influenza Viruses.
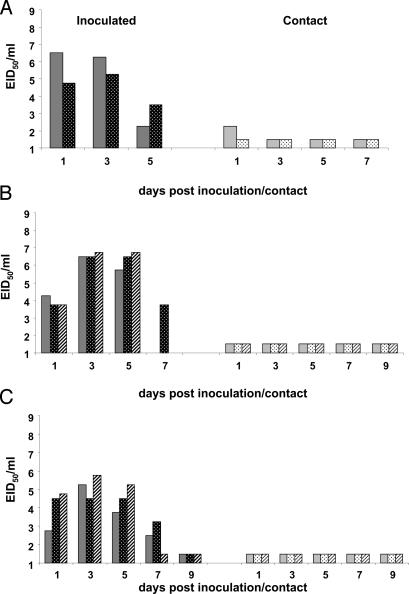
We next evaluated the ability of avian H5N1 influenza viruses to undergo respiratory droplet transmission between ferrets by inoculating three ferrets i.n. with 104 FID50 (106 EID50) of A/Hong Kong/486/97 (HK486), an H5N1 virus isolated from a human case patient in 1997. Mean nasal wash virus titers of the HK486-infected ferrets reached a maximal of 7.0 ± 1.1 log10 EID50/ml on day 5 p.i. (Fig. 1C), and signs of severe illness were observed (Table 1). The mean maximum weight loss in HK486-infected ferrets was 16.5% on days 2–7 p.i.; sneezing was observed only in one of three ferrets on day 4 p.i. (Table 1), and one of the ferrets was humanely killed on day 7 p.i. because of the onset of neurological symptoms. Virus was not detected in the nasal washes from any of the contact ferrets through day 9 p.c. (Fig. 1C). However, anti-HK486 HI antibody titers of 160 or 320 were detected in two of the three contact ferrets 17 days p.c., indicating that HK486 virus was transmitted to two of the contact ferrets in the absence of detectable virus in nasal secretions (Table 1). To determine whether HK486 virus would transmit more efficiently between cohoused ferrets, we next inoculated two animals i.n. with the same dose of HK486, and 24 h later we placed a naive ferret in the same cage with each inoculated animal. A low level of virus (102.3 EID50/ml) was recovered on day 1 p.c. from one of the contact ferrets that had been cohoused with an inoculated animal that shed peak virus titers of 106.5 EID50/ml (Fig. 2A), although both contact ferrets seroconverted with titers of 320 or 640 (data not shown). Two additional ferrets inoculated with a lower dose of HK486 virus (103 EID50) shed peak virus titers approximately three logs lower than the ferrets inoculated with the higher dose and failed to transmit virus to their cage mates, because the contact animals did not shed virus and did not seroconvert (data not shown).
Fig. 2.
Direct contact transmissibility of H5N1 viruses. (A) Two ferrets were inoculated with 104 FID50 (106 EID50) of HK486 virus, and nasal washes were collected on days 1, 3, and 5 p.i. (Left). Twenty-four hours later, a naive ferret was placed in the same cage as each of the inoculated ferrets, and nasal washes were collected on days 1, 3, 5 and 7 p.c. (Right). (B) Three ferrets were inoculated with 106 EID50 of Indo05, and nasal washes were collected on days 1, 3, 5, and 7 p.i. (Left). Twenty-four hours later, a naive ferret was placed in the same cage as each of the inoculated ferrets, and nasal washes were collected on days 1, 3, 5, 7, and 9 p.c. (Right). (C) Three ferrets were inoculated with 106 EID50 of VN30408, and nasal washes were collected on days 1, 3, 5, 7, and 9 p.i. (Left). Twenty-four hours later, a naive ferret was placed in the same cage as each of the inoculated ferrets, and nasal washes were collected on days 1, 3, 5, 7, and 9 p.c. (Right). Solid, dotted, and hatched bars each represent a separate ferret pair. The limit of virus detection was 101.5 EID50/ml.
The HK486 virus is genetically distinct from H5N1 viruses isolated since 1997; therefore, we also evaluated a 2003 and two 2005 H5N1 viruses for their ability to transmit between ferrets. A/Hong Kong/213/03 (HK213) contains a mutation at residue 223 (H5 numbering; residue 227 by H3 numbering) within the receptor-binding domain of the HA and was shown to bind to both α2,6 and α2,3 SA in vitro (13). Therefore, three ferrets were inoculated i.n. with 106 EID50 of HK213, and the next day three naïve ferrets were placed in adjacent transmission cages. HK213-infected ferrets achieved mean virus titers of 5.5 ± 0.3 log10 EID50/ml on days 1 and 3 p.i. (Fig. 1D) and exhibited some weight loss and lethargy but no sneezing (Table 1). Virus was not detected in the nasal washes from the contact ferrets nor was seroconversion detected by HI analysis of convalescent sera. A/Indonesia/5/05 (Indon05) and A/Vietnam/HN30408/05 (VN30408) are representative of the two distinct genetic clades of H5N1 viruses (clades 2 and 1, respectively) (14) that circulated in Asia during 2004–2005 and were isolated from human cases that had been associated with family clusters of H5N1 illness (4). In a contact transmission experiment, ferrets infected with 106 EID50 of Indon05 virus exhibited severe illness with substantial weight loss (18.8% mean maximum 7 days p.i.) and dyspnea but no sneezing; none of the ferrets survived past day 7 p.i. (Table 1). Although high titers of infectious virus were detected in the upper respiratory tract of Indon05-inoculated ferrets, virus was not detected in any of the nasal washes from the contact ferrets through day 9 p.c. (Fig. 2B), and convalescent sera collected from the contact animals lacked anti-Indon05 HI antibodies (Table 1). Ferrets infected with the same dose of VN30408 virus exhibited less severe illness and also failed to transmit the virus to contact animals (Table 1 and Fig. 2C). Taken together, these data demonstrate the lack of efficient transmission of H5N1 viruses in ferrets.
Characterization of Avian–Human Reassortant Influenza Viruses.
To evaluate the pandemic potential of H5N1 reassortant viruses and better understand the relative contribution of avian or human virus surface and internal protein genes to transmissibility, reassortant viruses containing various gene constellations from the avian H5N1 virus, HK486, and the human H3N2 virus, Vic75, were generated by using plasmid-based reverse genetics (rg). The parental viruses, containing all eight genes of either Vic75 (rgVic) or HK486 (rg486), were generated and their genetic identities were confirmed; the parental rg viruses exhibited virulence and transmissibility properties in ferrets similar to their WT counterparts (Table 2 and data not shown). To assess the contribution of the influenza virus internal protein genes, we first generated the reassortant virus, rgVic:486HANA, containing all six human virus internal protein genes and the avian virus H5 and N1 surface protein genes, and the reciprocal, rg486:VicHANA, containing avian virus internal protein genes and human H3 and N2 surface protein genes, and evaluated their infectivity for Madin-Darby canine kidney (MDCK) cells and eggs (Table 2). Although these two reassortant viruses had comparable infectivity titers in eggs, rgVic:486HANA achieved a titer that was 100-fold lower than that for the parental rg486 in MDCK cells, whereas rg486:VicHANA replicated as efficiently as the parental rgVic. An additional H5N1 reassortant virus, rg486:VicRNP, which contained the human virus ribonucleoprotein (RNP) genes (PB2, PB1, PA, NP), was generated and found to replicate to a higher titer in MDCK cells than rgVic:486HANA, although the infectivity of the two reassortants in embryonated eggs was similar (Table 2). Reassortant viruses, rg486:VicHANA and rg486:VicRNP, also exhibited higher infectivity for ferrets than rgVic:486HANA virus, and therefore had lower FID50 values (1.5 and 1.5 compared with 3.0, respectively; expressed as the log10 EID50 required to give 1 FID50). For comparison, WT Vic75 had an FID50 value of 0.5, whereas HK486 had an FID50 of 2.0. The data suggest that the infectivity for ferrets and MDCK cells of reassortant viruses bearing the HK486 HA and NA genes may be enhanced by the presence of the HK486 M and NS gene. In contrast, the reassortant virus bearing the Vic HA and NA genes replicated efficiently even when all internal genes, including the M and NS genes, were of avian virus origin. Certain gene constellations, such as rgVic:486HANAPB1 and rgVic:486HAPB1, which reflect the gene constellations of the viruses responsible for the 1957 and 1968 pandemics, respectively, could not be rescued even after multiple attempts, although the same plasmids were used to successfully rescue other reassortant combinations. These results suggest that certain combinations of genes from the avian and human influenza viruses used in this study may not be compatible for virus viability.
Table 2.
In vitro and in vivo characteristics of avian–human reassortant influenza viruses
| Reassortant virus | Avian or human virus gene* |
EID50/ml, log10 | pfu/ml | No. of inoculated ferrets/total number |
Peak nasal wash titer (day)§ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PB2 | PB1 | PA | HA | NP | NA | M | NS | Weight loss (%)† | Sneezing (day of onset) | Virus detected in nasal wash (days p.i.)‡ | ||||
| rgVic | H | H | H | H | H | H | H | H | 9.3 | 5 × 106 | 2/3 (1.4) | 3/3 (2) | 3/3 (1–7) | 5.1 (1) |
| rg486 | A | A | A | A | A | A | A | A | 7.5 | 5 × 105 | 3/3 (21.1) | 0/3 | 3/3 (1–7+) | 6.2 (5) |
| rgVic:486HANA | H | H | H | A | H | A | H | H | 7.8 | 1 × 103 | 1/3 (2.2) | 0/3 | 3/3 (1–7+) | 3.7 (3) |
| rg486:VicHANA | A | A | A | H | A | H | A | A | 7.8 | 4 × 106 | 3/3 (4.1) | 3/3 (2) | 3/3 (1–5) | 5.2 (3) |
| rg486:VicRNP | H | H | H | A | H | A | A | A | 7.5 | 1 × 107 | 2/3 (1.7) | 0/3 | 3/3 (1–5) | 4.7 (3) |
| rg486:VicRNPF5¶ | H | H | H | A | H | A | A | A | 8.3 | 4 × 107 | 3/3 (0.3) | 2/3 (7) | 3/3 (1–5) | 5.1 (3) |
*Avian genes (A) are from HK486 (H5N1), and human genes (H) are from Vic75 (H3N2) virus.
†The percentage mean maximum weight loss is shown.
‡+, the endpoint of virus detection in nasal washes was not determined for all ferrets.
§Peak nasal wash titers are expressed as the mean log10 EID50/ml.
¶rg486:VicRNP was passaged five times in ferrets and then grown in eggs.
Transmissibility of Avian–Human Reassortant Influenza Viruses.
We next assessed the ability of the avian–human reassortant viruses to undergo respiratory droplet transmission in ferrets, because this is a key property of a pandemic virus. Three ferrets were inoculated i.n. with 104 FID50 of rgVic:486HANA or rg486:VicRNP (107 or 105.5 EID50, respectively), and the next day, three naïve ferrets were placed in adjacent transmission cages. Although all ferrets inoculated with either rgVic:486HANA or rg486:VicRNP shed virus in the upper respiratory tract for at least 5 days p.i. (Table 2), there was no evidence of transmission because contact animals did not shed virus or seroconvert (Table 3). In fact, the mean virus titers of each reassortant in nasal washes from ferrets were lower than titers observed with either parental strain (Table 2). Furthermore, the inoculated ferrets exhibited only minor weight loss, indicating that both reassortant viruses were substantially attenuated for ferrets compared with the rg486 parental strain, which caused a mean weight loss of 21% (Table 2).
Table 3.
Summary of respiratory droplet transmissibility of avian–human reassortant influenza viruses in ferrets
| Reassortant virus | No. of contact ferrets |
Respiratory droplet transmission | |||
|---|---|---|---|---|---|
| Weight loss (%)* | Sneezing | Virus detected in nasal wash | Sero-conversion (HI titer)† | ||
| rgVic:486HANA | 1/3 (0.8) | 0/3 | 0/3 | 0/3 | None |
| rg486:VicHANA | 1/3 (0.4) | 0/3 | 0/3 | 1/3 (40) | Inefficient |
| rg486:VicRNP | 3/3 (2.3) | 0/3 | 0/3 | 0/3 | None |
| rg486:VicRNPF5 | 0/3 | 0/3 | 0/3 | 0/3 | None |
*The percentage mean maximum weight loss is shown.
†HI assays were done by using Vic75 or HK486 and RBCs from turkey or horse, respectively.
Because none of the reassortants possessing the HA and NA of the avian HK486 virus demonstrated the ability to transmit, we next determined whether the human virus HA and NA were required for transmission. Ferrets were inoculated with the same dose of the reassortant virus, rg486:VicHANA [104 FID50 (105.5 EID50)], and virus was recovered from all three infected animals with a mean peak virus titer of 5.2 ± 0.6 log10 EID50/ml, which was similar to titers achieved in ferrets inoculated with the rg parental virus, rgVic (Table 2). Nevertheless, the rg486:VicHANA virus failed to transmit as efficiently as rgVic; virus was not detected in the nasal washes collected from any of the rg486:VicHANA contact ferrets, and only one of three contact ferrets exhibited a modest rise in serum HI antibody on day 20 p.c., indicating that some transmission of the reassortant had occurred (Table 3). Interestingly, the contact animal that seroconverted was exposed to an inoculated ferret that had shed the highest level of virus detected from any of the reassortant-inoculated ferrets evaluated (105.5 EID50/ml). These data suggest that the avian internal protein genes of rg486:VicHANA virus reduce the transmission efficiency of the human H3N2 virus in ferrets without affecting the replication efficiency.
The acquisition of mutations, such as those that confer the human α2,6 SA receptor-binding preference, is likely to be important for an avian influenza virus or an avian–human reassortant virus to transmit efficiently among humans and is thought to occur during adaptation in the new host (10). To determine whether an H5N1 reassortant virus could acquire mutations that would enhance transmissibility through multiple rounds of replication in a mammalian host, we passaged rg486:VicRNP virus (the H5N1 reassortant that had replicated most efficiently in ferrets) five times in ferrets and tested the resulting virus, rg486:VicRNPF5, for its ability to undergo respiratory droplet transmission. Although peak nasal wash titers of rg486:VicRNPF5-inoculated animals were similar to those for ferrets inoculated with rgVic (5.1 ± 0.5 log10 EID50/ml) (Table 2), transmission of rg486:VicRNPF5 was not detected (Table 3). Sequence analysis of the complete rg486:VicRNPF5 genome revealed only a single amino acid change (S353F) within the NP gene. These data and the observation that most avian viruses isolated from humans retain their receptor preference for α2,3 SA (13, 26) suggest that there is a level of stability of receptor specificity among circulating H5N1 viruses.
Discussion
If H5N1 viruses acquire the ability to undergo efficient and sustained transmission among humans, a pandemic would be inevitable. An understanding of the molecular and biologic requirements for efficient transmissibility is critical for the early identification of a potential H5N1 pandemic virus and the application of optimal control measures. The results of this study demonstrate, that unlike human H3N2 viruses, avian H5N1 viruses isolated from humans in 1997, 2003, or 2005 lack the ability to transmit efficiently in the ferret model. Furthermore, reassortant viruses bearing 1997 avian H5N1 surface glycoproteins with four or six human virus internal protein genes do not transmit efficiently in ferrets and thus lack the key property that predicts pandemic spread.
We found that the rgVic:486HANA reassortant bearing the H5 HA and human virus M and NS exhibited reduced infectivity for MDCK cells and 10-fold lower viral titers in ferrets compared with rg486:VicRNP that possessed avian virus M and NS as well as HA and NA. Another reassortant that possessed seven avian virus genes and only the human virus M gene also exhibited reduced infectivity for MDCK cells (data not shown). These results suggest that the infectivity of reassortant viruses bearing the HK486 HA and NA genes may be enhanced by the presence of the HK486 M gene, a finding supported by Scholtissek et al. (27), who showed that reassortants bearing an avian virus HA and a human virus M gene were substantially compromised in their replication.
Transmissibility of influenza viruses in this model is likely associated with virus infectivity for ferrets, which is reflected in the FID50, and efficiency of virus replication in the upper respiratory tract, which directly affects the amount of virus shedding. Mutations in the NA that affect enzymatic activity and replication efficiency were shown to reduce direct contact transmission in ferrets (18, 28). In this study, WT or rg H3N2 parental viruses that achieved peak nasal wash viral titers ranging from 104.3 to 108.5 EID50/ml all exhibited efficient respiratory droplet transmission. The lack of SA α2,3 receptors in the upper respiratory tract of humans has been presented as a possible explanation for the lack of transmissibility of the H5N1 viruses (23, 24). However, high titers of virus (ranging from 106.3 to 107.8 EID50/ml) were recovered in nasal washes from ferrets inoculated with two of four WT H5N1 viruses evaluated in this study, yet efficient respiratory droplet or direct contact transmission was not observed. It is noteworthy that the HK213 H5N1 virus, which has been shown to have a moderate affinity for the SA α2,6 receptor (13), did not replicate as efficiently as the other H5N1 viruses tested and showed no enhanced respiratory droplet transmission. Likewise, rg486:VicHANA virus, possessing human H3N2 surface genes, replicated to a mean peak nasal wash virus titer comparable to that of the parental rgVic virus, but failed to transmit as efficiently, suggesting that although the amount of virus shed by an infected animal may enhance the likelihood of transmission, other molecular or biologic properties are critical for efficient transmissibility.
Other biologic properties that may influence the ability of a virus to undergo efficient respiratory droplet transmission include the ability to elicit symptoms that promote expulsion from the host. Sneezing was consistently observed in all H3N2-infected ferrets, including those infected with rgVic and rg486:VicHANA, starting 2 days p.i. (Tables 1 and 2), but was only rarely observed in ferrets infected with WT or rg parental H5N1 viruses and was not detected in any ferrets infected with the H5N1 reassortant viruses. It is yet to be determined whether the molecular factors enhancing this biologic property also enhance efficient transmissibility in the ferret model.
Although these findings do not identify the precise genetic determinants responsible for influenza virus transmissibility, they provide an assessment of the risk of an H5N1 pandemic strain emerging through reassortment with a human influenza virus. Our results indicate that, within the context of the viruses used in this study, H5N1 avian–human reassortant viruses did not exhibit properties that would initiate a pandemic. Nevertheless, H5N1 viruses continue to spread geographically, infect a variety of mammals, and evolve rapidly. Therefore, further evaluation of the efficiency of replication and transmissibility of reassortants between contemporary H5N1 viruses and circulating human influenza viruses is an ongoing public health need. The ferret transmission model serves as a valuable tool for this purpose and the identification of molecular and biologic correlates of efficient transmissibility that may be used for early detection of a novel virus with pandemic capability.
Methods
Viruses.
The human H3N2 influenza A viruses Vic75 and Pan99 and the avian H5N1 influenza A viruses HK486, HK213, Indo05, and VN30408 were used in this study. Virus stocks were prepared in 10-day-old eggs as described (29) except that human viruses were incubated at 33.5°C for 48 h, whereas reassortant viruses were incubated at 37°C for 48 h. All research with H5N1 viruses or reassortant viruses was conducted under biosafety level 3 containment, including enhancements required by the U.S. Department of Agriculture and the Select Agent Program (see interim guidance at www.cdc.gov/flu/h2n2bsl3.htm).
Plasmids and Rescue of Reassortant Viruses.
Plasmid-based rg was used to generate the reassortant viruses used in this study. As described (30), all eight Vic75 genes were amplified and cloned into a viral RNA (vRNA) expression plasmid, and Vic75 PB2, PB1, PA, and NP genes were cloned into an mRNA expression plasmid. All eight genes of HK486 were amplified from vRNA by RT-PCR with a One-Step RT-PCR kit (Qiagen, Valencia, CA) and cloned into a bidirectional plasmid (pBD) that possesses vRNA expression elements from pPolISapIRib (31, 32) and mRNA expression elements from pCI (Promega, Madison, WI). Reassortant viruses were rescued as described (33) by using the 12-plasmid Vic75 system, the eight-plasmid HK486 system, or a combination of the two. The genetic makeup of each reassortant virus was confirmed by sequencing as described (29).
Inoculation of Ferrets.
Male Fitch ferrets, 6–12 months of age (Triple F Farms, Sayre, PA), that were serologically negative by HI assay for currently circulating influenza viruses were used in this study. Ferrets were housed throughout each experiment in cages within a Duo-Flo Bioclean mobile clean room (Lab Products, Seaford, DE). Baseline serum, temperature, and weight measurements were obtained before infection. Temperatures were measured with an s.c. implantable temperature transponder (BioMedic Data Systems, Seaford, DE). Ferrets were inoculated, and nasal washes were collected and analyzed as described (29). FID50 titers were determined by inoculating groups of nine ferrets i.n. with serial 10-fold dilutions of virus, calculated by using the method of Reed and Muench (34), and expressed as the EID50 value corresponding to 1 FID50.
Transmission Experiments.
For the respiratory droplet transmission experiments, ferrets were housed in adjacent transmission cages, each modified so that a side wall was replaced with a stainless-steel, perforated wall with holes 1–5 mm in diameter and spaced 3 mm apart to facilitate the transfer of respiratory droplets through the air while preventing direct contact between ferrets and indirect contact with the bedding and food of neighboring ferrets. The use of the term “respiratory droplet transmission” throughout this article refers to transmission in the absence of direct or indirect contact and does not imply an understanding of the droplet size involved in virus spread between ferrets. A total of six ferrets were used for each respiratory droplet transmission experiment. Three ferrets were inoculated with 104 FID50 of virus, unless otherwise stated, and each was placed in a separate cage. Twenty-four hours later (day 1 p.i. for the inoculated ferrets and day 0 p.c. for the contact ferrets), three naive ferrets were each placed in a cage adjacent to an inoculated ferret. To prevent inadvertent physical transmission of virus by the investigators, the contact ferrets were always handled first, and all items that came into contact with the ferrets or their bedding were decontaminated between each ferret. For contact transmission experiments, two or three ferrets were each placed in an unmodified cage with solid walls and inoculated i.n. with 104 FID50 of virus, unless otherwise stated. Twenty-four hours later, a naive ferret was placed in the same cage with each inoculated ferret. Clinical signs were monitored daily in all ferrets for at least 14 days p.i./p.c. If any ferret lost >25% of its body weight or exhibited neurologic symptoms, it was humanely killed.
HI Assays.
HI analysis was conducted as described (35) by using convalescent sera collected from ferrets 14–33 days p.i./p.c. Sera collected from ferrets included in the transmission experiments with Vic75, Pan99, or reassortant H3N2 viruses were tested for H3-specific antibodies by using turkey RBCs and virus bearing the homologous HA. Ferret sera from the transmission experiments with HK486, Indon05, VN30408, or reassortant H5N1 viruses were tested for H5-specific antibodies by using virus bearing the homologous HA and horse RBCs as a means of more sensitive detection (35).
Acknowledgments
We thank Neal Van Hoeven for assistance with serological screening of ferrets, James Mitchell and Eddie Jackson for exceptional care of animals used in this study, and Patrick Blair for facilitating access to the clade 2 virus.
Abbreviations
- HA
hemagglutinin
- NA
neuraminidase
- SA
sialic acid
- Pan99
A/Panama/2007/99
- Vic75
A/Victoria/3/75
- i.n.
intranasally
- FID50
50% ferret infectious dose
- EID50
50% egg infectious dose
- p.i.
postinoculation
- p.c.
postcontact
- HI
hemagglutination inhibition
- HK486
A/Hong Kong/486/97
- HK213
A/Hong Kong/213/03
- Indon05
A/Indonesia/5/05
- VN30408
A/Vietnam/HN30408/05
- rg
reverse genetics
- MDCK
Madin-Darby canine kidney
- RNP
ribonucleoprotein
Footnotes
Conflict of interest statement: No conflicts declared.
References
- 1.de Jong J. C., Claas E. C., Osterhaus A. D., Webster R. G., Lim W. L. Nature. 1997;389:554. doi: 10.1038/39218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Subbarao K., Klimov A., Katz J., Regnery H., Lim W., Hall H., Perdue M., Swayne D., Bender C., Huang J., et al. Science. 1998;279:393–396. doi: 10.1126/science.279.5349.393. [DOI] [PubMed] [Google Scholar]
- 3.Peiris J. S., Yu W. C., Leung C. W., Cheung C. Y., Ng W. F., Nicholls J. M., Ng T. K., Chan K. H., Lai S. T., Lim W. L., et al. Lancet. 2004;363:617–619. doi: 10.1016/S0140-6736(04)15595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . Epidemic and Pandemic Alert and Response: Pandemic Influenza. Geneva: W.H.O.; 2006. [Google Scholar]
- 5.Ungchusak K., Auewarakul P., Dowell S. F., Kitphati R., Auwanit W., Puthavathana P., Uiprasertkul M., Boonnak K., Pittayawonganon C., Cox N. J., et al. N. Engl. J. Med. 2005;352:333–340. doi: 10.1056/NEJMoa044021. [DOI] [PubMed] [Google Scholar]
- 6.Olsen S. J., Ungchusak K., Sovann L., Uyeki T. M., Dowell S. F., Cox N. J., Aldis W., Chunsuttiwat S. Emerg. Infect. Dis. 2005;11:1799–1801. doi: 10.3201/eid1111.050646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reid A. H., Taubenberger J. K., Fanning T. G. Nat. Rev. Microbiol. 2004;2:909–914. doi: 10.1038/nrmicro1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taubenberger J. K., Reid A. H., Lourens R. M., Wang R., Jin G., Fanning T. G. Nature. 2005;437:889–893. doi: 10.1038/nature04230. [DOI] [PubMed] [Google Scholar]
- 9.Kawaoka Y., Krauss S., Webster R. G. J. Virol. 1989;63:4603–4608. doi: 10.1128/jvi.63.11.4603-4608.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matrosovich M., Tuzikov A., Bovin N., Gambaryan A., Klimov A., Castrucci M. R., Donatelli I., Kawaoka Y. J. Virol. 2000;74:8502–8512. doi: 10.1128/jvi.74.18.8502-8512.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matrosovich M., Zhou N., Kawaoka Y., Webster R. J. Virol. 1999;73:1146–1155. doi: 10.1128/jvi.73.2.1146-1155.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shinya K., Hatta M., Yamada S., Takada A., Watanabe S., Halfmann P., Horimoto T., Neumann G., Kim J. H., Lim W., et al. J. Virol. 2005;79:9926–9932. doi: 10.1128/JVI.79.15.9926-9932.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gambaryan A., Tuzikov A., Pazynina G., Bovin N., Balish A., Klimov A. Virology. 2006;344:432–438. doi: 10.1016/j.virol.2005.08.035. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization Emerg. Infect. Dis. 2005;11:1515–1521. [Google Scholar]
- 15.Bridges C. B., Kuehnert M. J., Hall C. B. Clin. Infect. Dis. 2003;37:1094–1101. doi: 10.1086/378292. [DOI] [PubMed] [Google Scholar]
- 16.Schulman J. L., Kilbourne E. D. Nature. 1962;195:1129–1130. doi: 10.1038/1951129a0. [DOI] [PubMed] [Google Scholar]
- 17.Herlocher M. L., Elias S., Truscon R., Harrison S., Mindell D., Simon C., Monto A. S. J. Infect. Dis. 2001;184:542–546. doi: 10.1086/322801. [DOI] [PubMed] [Google Scholar]
- 18.Herlocher M. L., Carr J., Ives J., Elias S., Truscon R., Roberts N., Monto A. S. Antiviral Res. 2002;54:99–111. doi: 10.1016/s0166-3542(01)00214-5. [DOI] [PubMed] [Google Scholar]
- 19.Herlocher M. L., Truscon R., Elias S., Yen H. L., Roberts N. A., Ohmit S. E., Monto A. S. J. Infect. Dis. 2004;190:1627–1630. doi: 10.1086/424572. [DOI] [PubMed] [Google Scholar]
- 20.Baum L. G., Paulson J. C. Acta Histochem. Suppl. 1990;40:35–38. [PubMed] [Google Scholar]
- 21.Matrosovich M. N., Matrosovich T. Y., Gray T., Roberts N. A., Klenk H. D. Proc. Natl. Acad. Sci. USA. 2004;101:4620–4624. doi: 10.1073/pnas.0308001101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leigh M. W., Connor R. J., Kelm S., Baum L. G., Paulson J. C. Vaccine. 1995;13:1468–1473. doi: 10.1016/0264-410x(95)00004-k. [DOI] [PubMed] [Google Scholar]
- 23.Shinya K., Ebina M., Yamada S., Ono M., Kasai N., Kawaoka Y. Nature. 2006;440:435–436. doi: 10.1038/440435a. [DOI] [PubMed] [Google Scholar]
- 24.van Riel D., Munster V. J., de Wit E., Rimmelzwaan G. F., Fouchier R. A., Osterhaus A. D., Kuiken T. Science. 2006;312:399. doi: 10.1126/science.1125548. [DOI] [PubMed] [Google Scholar]
- 25.Andrewes C. H., Glover R. E. Br. J. Exp. Pathol. 1941;22:91–97. [Google Scholar]
- 26.Stevens J., Blixt O., Tumpey T. M., Taubenberger J. K., Paulson J. C., Wilson I. A. Science. 2006;312:404–410. doi: 10.1126/science.1124513. [DOI] [PubMed] [Google Scholar]
- 27.Scholtissek C., Stech J., Krauss S., Webster R. G. J. Virol. 2002;76:1781–1786. doi: 10.1128/JVI.76.4.1781-1786.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yen H. L., Herlocher L. M., Hoffmann E., Matrosovich M. N., Monto A. S., Webster R. G., Govorkova E. A. Antimicrob. Agents Chemother. 2005;49:4075–4084. doi: 10.1128/AAC.49.10.4075-4084.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maines T. R., Lu X. H., Erb S. M., Edwards L., Guarner J., Greer P. W., Nguyen D. C., Szretter K. J., Chen L. M., Thawatsupha P., et al. J. Virol. 2005;79:11788–11800. doi: 10.1128/JVI.79.18.11788-11800.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Falcon A. M., Marion R. M., Zurcher T., Gomez P., Portela A., Nieto A., Ortin J. J. Virol. 2004;78:3880–3888. doi: 10.1128/JVI.78.8.3880-3888.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fodor E., Devenish L., Engelhardt O. G., Palese P., Brownlee G. G., Garcia-Sastre A. J. Virol. 1999;73:9679–9682. doi: 10.1128/jvi.73.11.9679-9682.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li Z., Chen H., Jiao P., Deng G., Tian G., Li Y., Hoffmann E., Webster R. G., Matsuoka Y., Yu K. J. Virol. 2005;79:12058–12064. doi: 10.1128/JVI.79.18.12058-12064.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Subbarao K., Chen H., Swayne D., Mingay L., Fodor E., Brownlee G., Xu X., Lu X., Katz J., Cox N., et al. Virology. 2003;305:192–200. doi: 10.1006/viro.2002.1742. [DOI] [PubMed] [Google Scholar]
- 34.Reed L. J., Muench H. Am. J. Hyg. 1938;27:493–497. [Google Scholar]
- 35.Stephenson I., Wood J. M., Nicholson K. G., Charlett A., Zambon M. C. Virus Res. 2004;103:91–95. doi: 10.1016/j.virusres.2004.02.019. [DOI] [PubMed] [Google Scholar]