Abstract
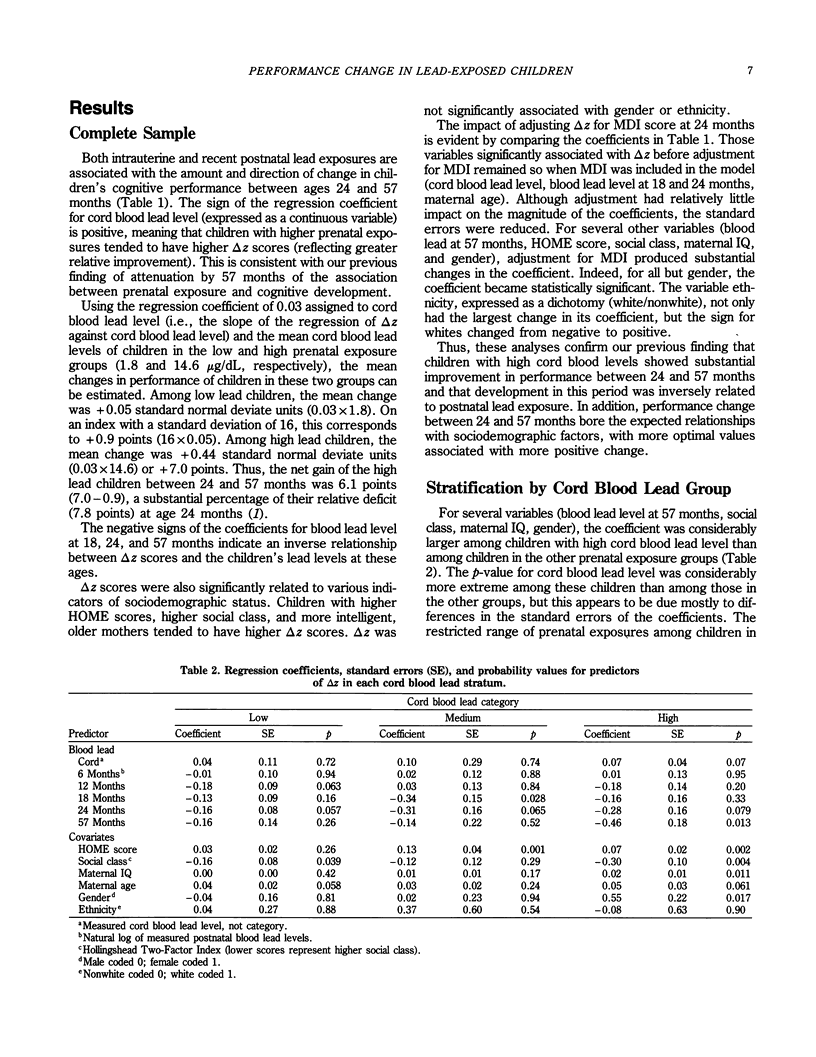
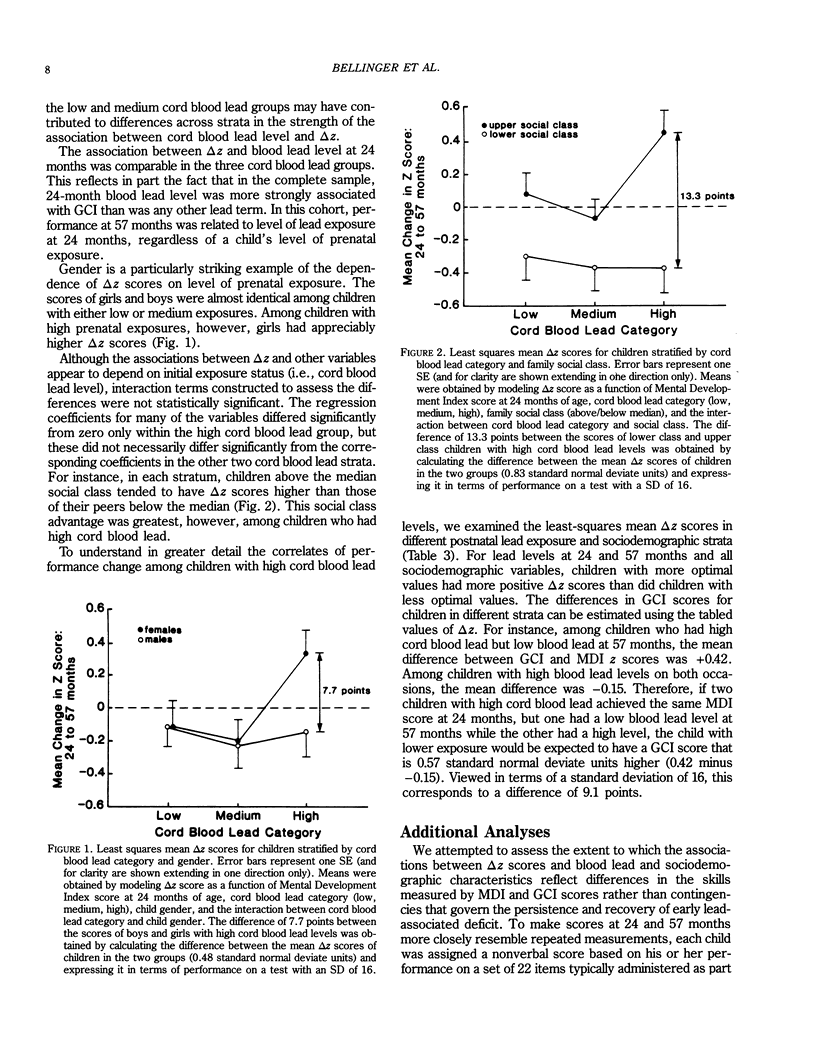
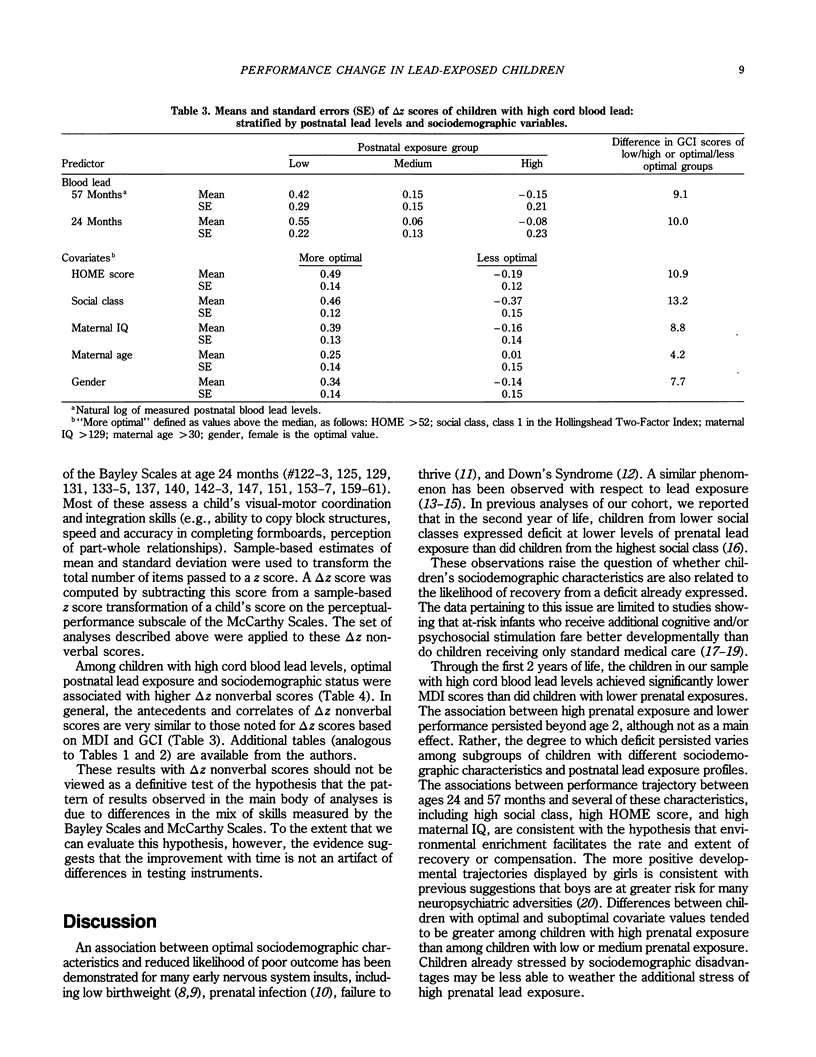
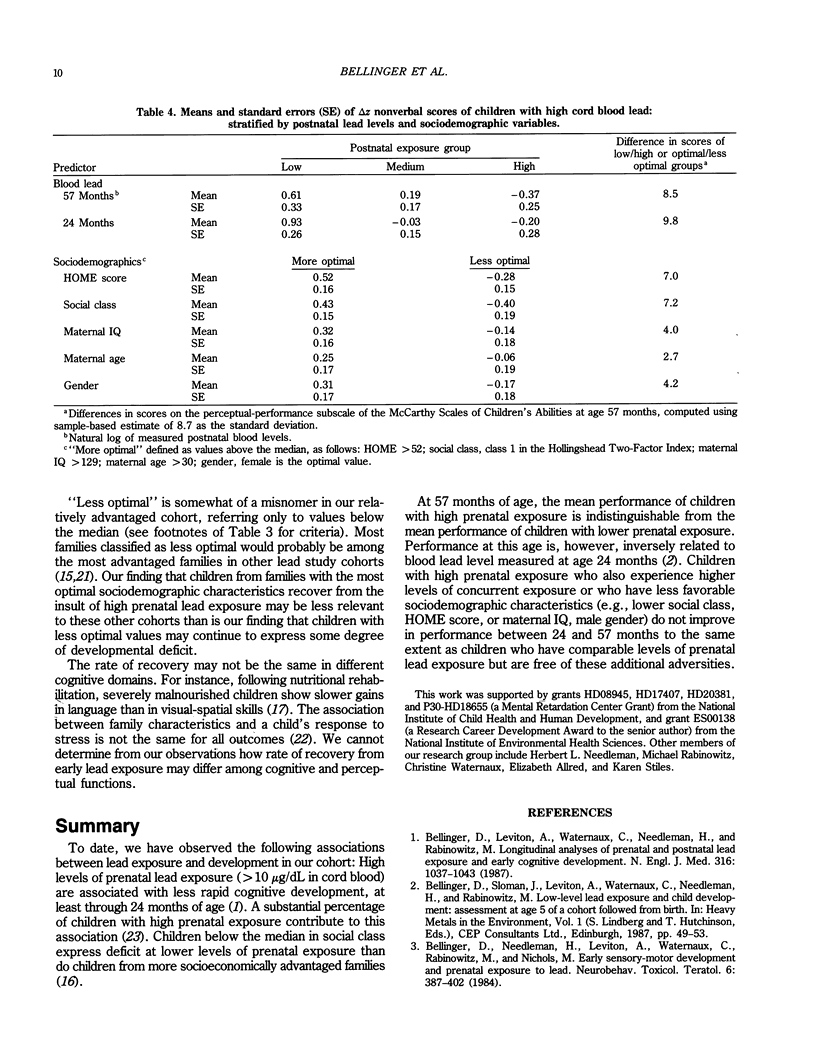
Up to 2 years of age, children with umbilical cord blood lead levels of 10 to 25 micrograms/dL achieve significantly lower scores on tests of cognitive development than do children with lower prenatal exposures. By age 5 years, however, they appear to have recovered from, or at least compensated for, this early insult. Change in performance between 24 and 57 months of age was examined in relation to level of postnatal lead exposure and various sociodemographic factors. Among children with high prenatal lead exposure, greater recovery of function was associated with lower blood level at 57 months, higher socioeconomic status, higher Home Observation for Measurement of the Environment scores, higher maternal IQ, and female gender. The difference between the scores at 57 months of children with optimal and less optimal values on these variables generally exceed 1/2 standard deviation. Higher prenatal lead exposure is associated with an increased risk of early cognitive deficit. Furthermore, the risk that a deficit will persist through the preschool years is increased among children with high prenatal exposure and either high postnatal exposure or less optimal sociodemographic characteristics.
Full text
PDF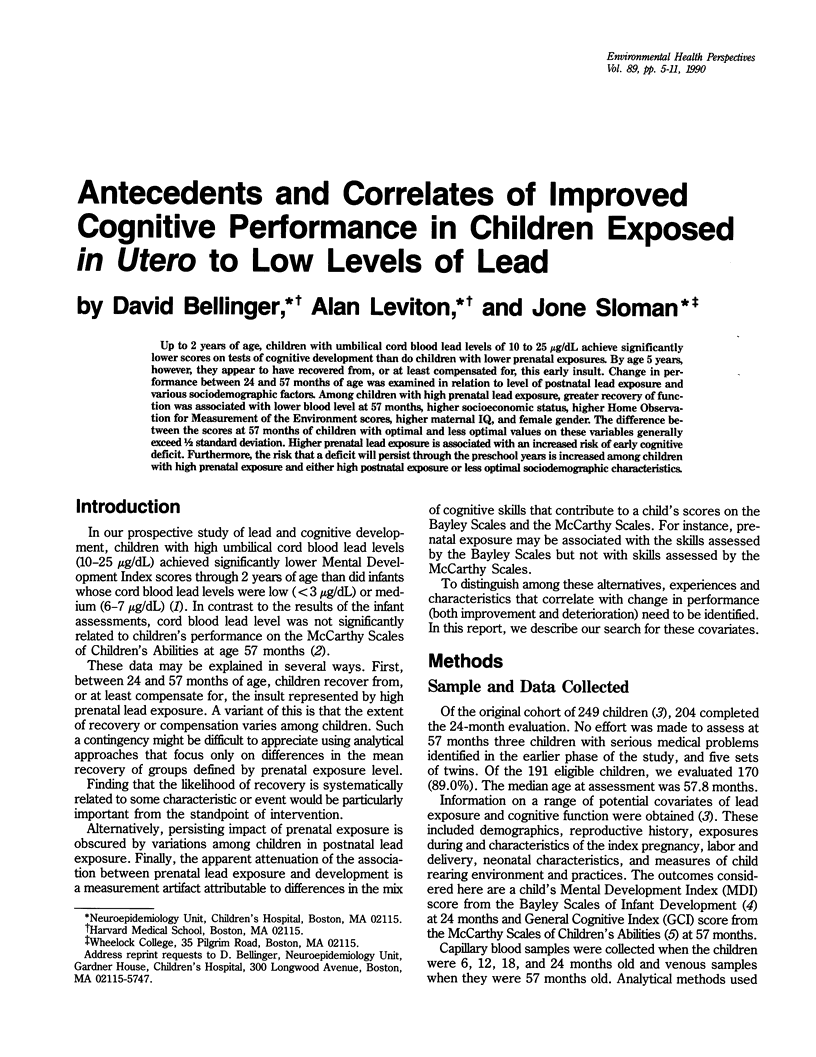

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bellinger D. C., Needleman H. L., Leviton A., Waternaux C., Rabinowitz M. B., Nichols M. L. Early sensory-motor development and prenatal exposure to lead. Neurobehav Toxicol Teratol. 1984 Sep-Oct;6(5):387–402. [PubMed] [Google Scholar]
- Bellinger D., Leviton A., Waternaux C., Needleman H., Rabinowitz M. Longitudinal analyses of prenatal and postnatal lead exposure and early cognitive development. N Engl J Med. 1987 Apr 23;316(17):1037–1043. doi: 10.1056/NEJM198704233161701. [DOI] [PubMed] [Google Scholar]
- Bellinger D., Leviton A., Waternaux C., Needleman H., Rabinowitz M. Low-level lead exposure, social class, and infant development. Neurotoxicol Teratol. 1988 Nov-Dec;10(6):497–503. doi: 10.1016/0892-0362(88)90084-0. [DOI] [PubMed] [Google Scholar]
- Dietrich K. N., Krafft K. M., Bornschein R. L., Hammond P. B., Berger O., Succop P. A., Bier M. Low-level fetal lead exposure effect on neurobehavioral development in early infancy. Pediatrics. 1987 Nov;80(5):721–730. [PubMed] [Google Scholar]
- Ernhart C. B., Morrow-Tlucak M., Marler M. R., Wolf A. W. Low level lead exposure in the prenatal and early preschool periods: early preschool development. Neurotoxicol Teratol. 1987 May-Jun;9(3):259–270. doi: 10.1016/0892-0362(87)90011-0. [DOI] [PubMed] [Google Scholar]
- Grantham-McGregor S., Schofield W., Powell C. Development of severely malnourished children who received psychosocial stimulation: six-year follow-up. Pediatrics. 1987 Feb;79(2):247–254. [PubMed] [Google Scholar]
- Hanshaw J. B., Scheiner A. P., Moxley A. W., Gaev L., Abel V., Scheiner B. School failure and deafness after "silent" congenital cytomegalovirus infection. N Engl J Med. 1976 Aug 26;295(9):468–470. doi: 10.1056/NEJM197608262950902. [DOI] [PubMed] [Google Scholar]
- Harvey P. G., Hamlin M. W., Kumar R., Delves H. T. Blood lead, behaviour and intelligence test performance in preschool children. Sci Total Environ. 1984 Dec;40:45–60. doi: 10.1016/0048-9697(84)90341-3. [DOI] [PubMed] [Google Scholar]
- Masten A. S., Garmezy N., Tellegen A., Pellegrini D. S., Larkin K., Larsen A. Competence and stress in school children: the moderating effects of individual and family qualities. J Child Psychol Psychiatry. 1988 Nov;29(6):745–764. doi: 10.1111/j.1469-7610.1988.tb00751.x. [DOI] [PubMed] [Google Scholar]
- Rabinowitz M. B., Needleman H. L. Temporal trends in the lead concentrations of umbilical cord blood. Science. 1982 Jun 25;216(4553):1429–1431. doi: 10.1126/science.7089532. [DOI] [PubMed] [Google Scholar]
- Rabinowitz M., Leviton A., Needleman H. Variability of blood lead concentrations during infancy. Arch Environ Health. 1984 Mar-Apr;39(2):74–77. doi: 10.1080/00039896.1984.10545838. [DOI] [PubMed] [Google Scholar]
- Rauh V. A., Achenbach T. M., Nurcombe B., Howell C. T., Teti D. M. Minimizing adverse effects of low birthweight: four-year results of an early intervention program. Child Dev. 1988 Jun;59(3):544–553. [PubMed] [Google Scholar]
- Shoham-Yakubovich I., Barell V. Maternal education as a modifier of the association between low birthweight and infant mortality. Int J Epidemiol. 1988 Jun;17(2):370–377. doi: 10.1093/ije/17.2.370. [DOI] [PubMed] [Google Scholar]
- Singer L. T., Fagan J. F., 3rd Cognitive development in the failure-to-thrive infant: a three-year longitudinal study. J Pediatr Psychol. 1984 Sep;9(3):363–383. doi: 10.1093/jpepsy/9.3.363. [DOI] [PubMed] [Google Scholar]
- Slater M. A., Naqvi M., Andrew L., Haynes K. Neurodevelopment of monitored versus nonmonitored very low birth weight infants: the importance of family influences. J Dev Behav Pediatr. 1987 Oct;8(5):278–285. [PubMed] [Google Scholar]
- Winneke G., Kraemer U. Neuropsychological effects of lead in children: interactions with social background variables. Neuropsychobiology. 1984;11(3):195–202. doi: 10.1159/000118077. [DOI] [PubMed] [Google Scholar]


