Abstract
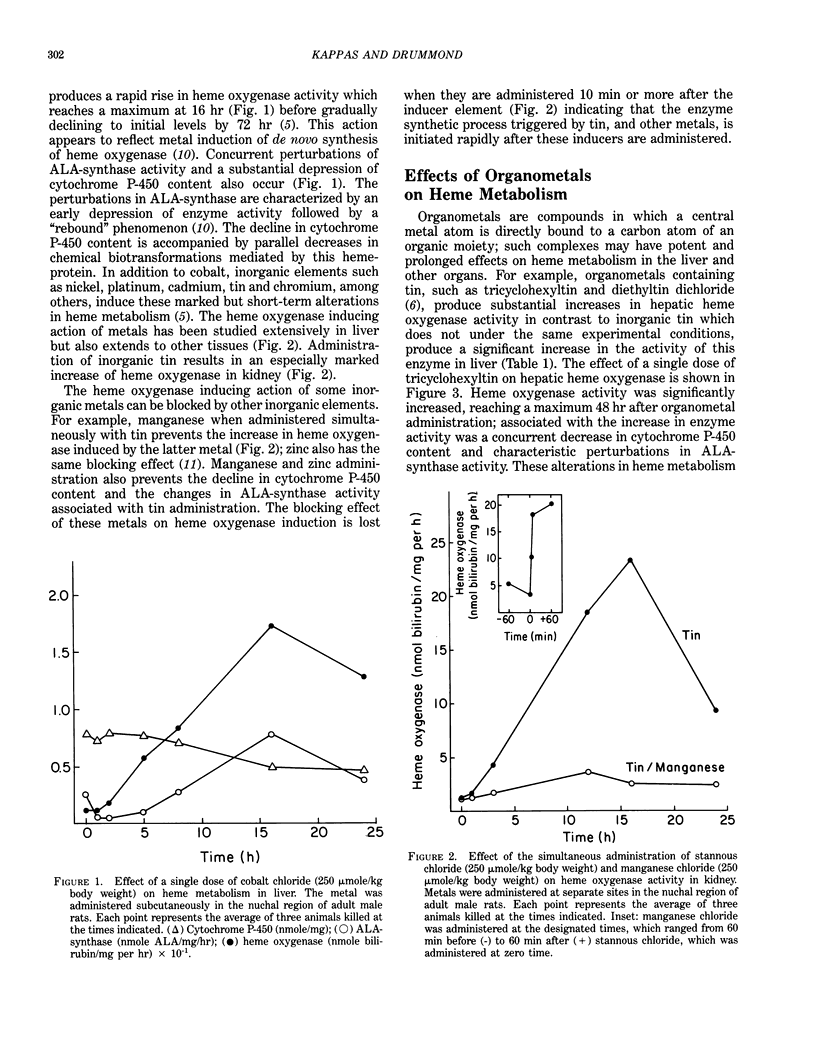
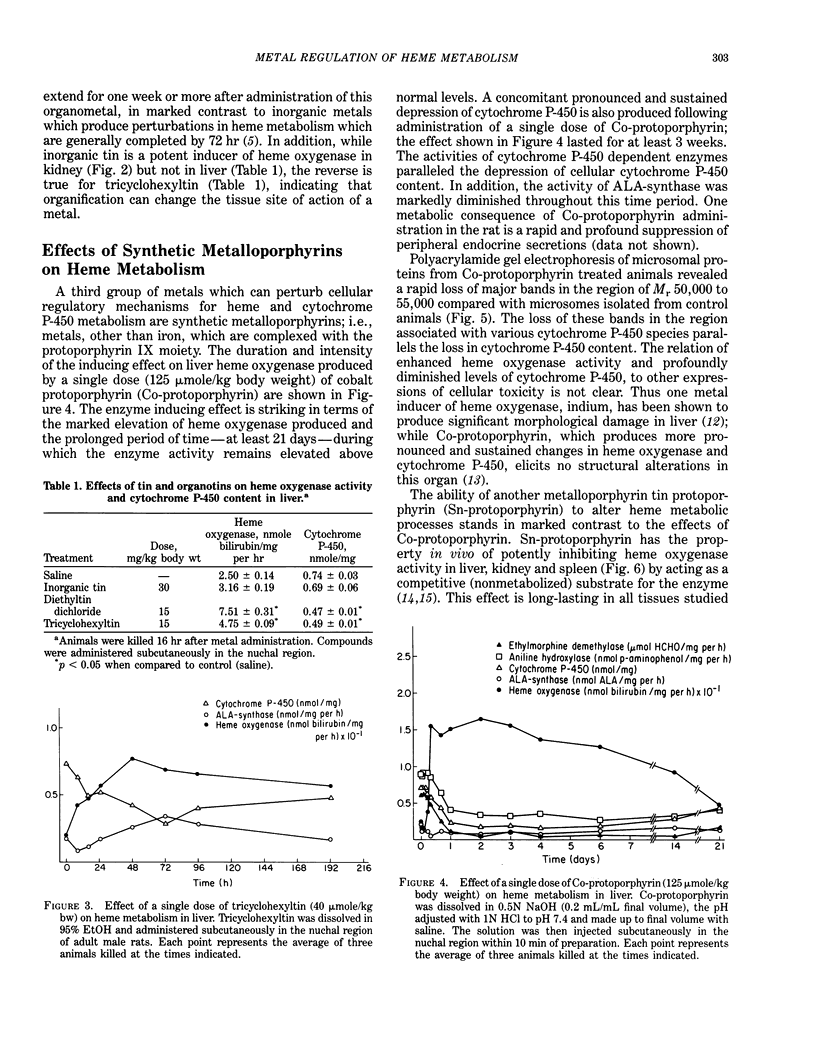
The heme-cytochrome P-450 complexes represent sensitive metabolic systems for examining the biological impact of metals on important cellular functions. Many metals, both in the inorganic form and bound to organic moieties, potently induce heme oxygenase, the rate limiting enzyme of heme degradation. The resulting increase in the rate of heme breakdown is reflected in a marked depression of cellular cytochrome P-450 content and impairment of the oxidative metabolism of natural and foreign chemicals dependent on this hemeprotein. Organometal complexes do not mimic in all their aspects the actions of the inorganic elements which they contain. For example, organotins, in contrast to inorganic tin, produce a prolonged induction response of heme oxygenase in the liver but not in the kidney. Co-protoporphyrin is a much more potent inducer of heme oxygenase in liver than is inorganic cobalt; and Sn-protoporphyrin inhibits heme oxygenase activity nearly completely, whereas inorganic tin is a powerful inducer of the renal enzyme. Contrasting effects on heme metabolism exist as well within the metalloporphyrin species as demonstrated by the effects in vivo of Co-protoporphyrin and Sn-protoporphyrin on heme oxygenase activity; the former induces the enzyme whereas the latter potently inhibits it. In vitro, however, both compounds competitively inhibit heme oxidation activity. These differences, among others which characterize metal actions in vivo and in vitro attest to the importance of pharmacokinetic, adaptive and other host factors in defining the responses of the heme-cytochrome P-450 systems to the impact of metals in the whole animal.
Full text
PDF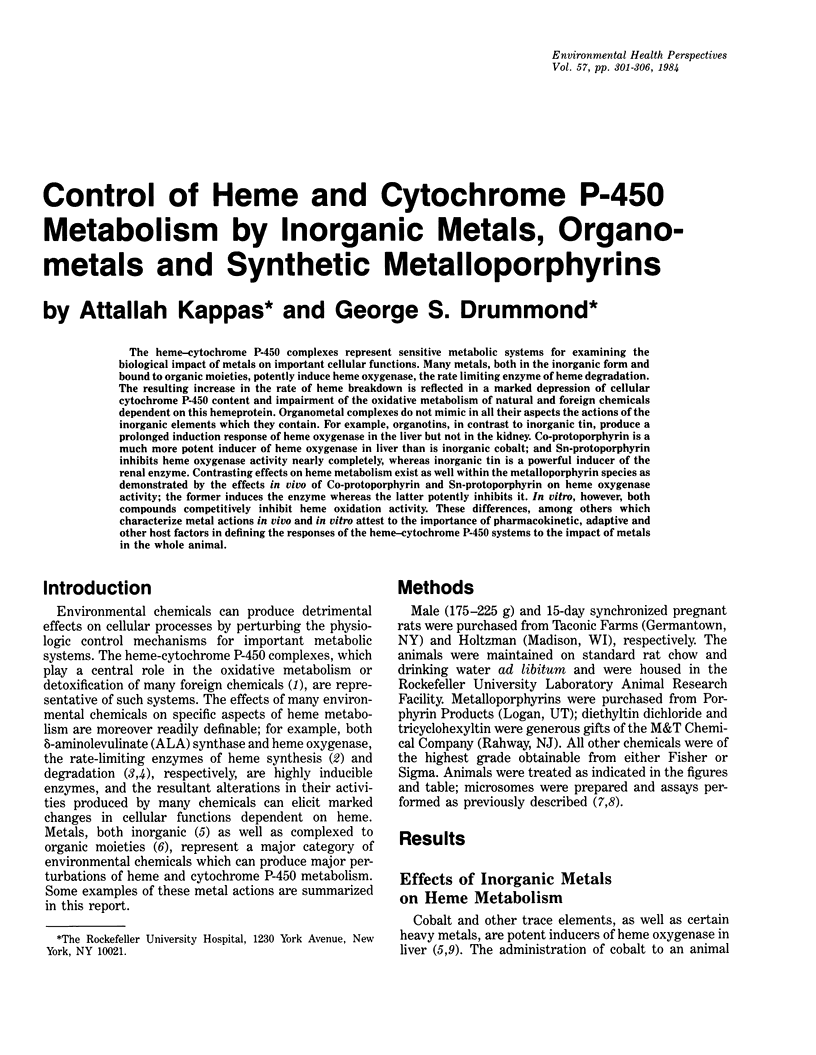
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Conney A. H. Pharmacological implications of microsomal enzyme induction. Pharmacol Rev. 1967 Sep;19(3):317–366. [PubMed] [Google Scholar]
- Drummond G. S., Kappas A. An experimental model of postnatal jaundice in the suckling rat. Suppression of induced hyperbilirubinemia by Sn-protoporphyrin. J Clin Invest. 1984 Jul;74(1):142–149. doi: 10.1172/JCI111394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond G. S., Kappas A. Chemoprevention of neonatal jaundice: potency of tin-protoporphyrin in an animal model. Science. 1982 Sep 24;217(4566):1250–1252. doi: 10.1126/science.6896768. [DOI] [PubMed] [Google Scholar]
- Drummond G. S., Kappas A. Manganese and zinc blockade of enzyme induction: studies with microsomal heme oxygenase. Proc Natl Acad Sci U S A. 1979 Oct;76(10):5331–5335. doi: 10.1073/pnas.76.10.5331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond G. S., Kappas A. Prevention of neonatal hyperbilirubinemia by tin protoporphyrin IX, a potent competitive inhibitor of heme oxidation. Proc Natl Acad Sci U S A. 1981 Oct;78(10):6466–6470. doi: 10.1073/pnas.78.10.6466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond G. S., Kappas A. Suppression of hyperbilirubinemia in the rat neonate by chromium-protoporphyrin. Interactions of metalloporphyrins with microsomal heme oxygenase of human spleen. J Exp Med. 1982 Dec 1;156(6):1878–1883. doi: 10.1084/jem.156.6.1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond G. S., Kappas A. The cytochrome P-450-depleted animal: an experimental model for in vivo studies in chemical biology. Proc Natl Acad Sci U S A. 1982 Apr;79(7):2384–2388. doi: 10.1073/pnas.79.7.2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler B. A., Kardish R. M., Woods J. S. Alteration of hepatic microsomal structure and function by indium chloride. Ultrastructural, morphometric, and biochemical studies. Lab Invest. 1983 Apr;48(4):471–478. [PubMed] [Google Scholar]
- GRANICK S., URATA G. Increase in activity of alpha-aminolevulinic acid synthetase in liver mitochondria induced by feeding of 3,5-dicarbethoxy-1,4-dihydrocollidine. J Biol Chem. 1963 Feb;238:821–827. [PubMed] [Google Scholar]
- Kappas A., Drummond G. S., Simionatto C. S., Anderson K. E. Control of heme oxygenase and plasma levels of bilirubin by a synthetic heme analogue, tin-protoporphyrin. Hepatology. 1984 Mar-Apr;4(2):336–341. doi: 10.1002/hep.1840040227. [DOI] [PubMed] [Google Scholar]
- Maines M. D., Kappas A. Cobalt induction of hepatic heme oxygenase; with evidence that cytochrome P-450 is not essential for this enzyme activity. Proc Natl Acad Sci U S A. 1974 Nov;71(11):4293–4297. doi: 10.1073/pnas.71.11.4293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maines M. D., Kappas A. Cobalt stimulation of heme degradation in the liver. Dissociation of microsomal oxidation of heme from cytochrome P-450. J Biol Chem. 1975 Jun 10;250(11):4171–4177. [PubMed] [Google Scholar]
- Maines M. D., Kappas A. Metals as regulators of heme metabolism. Science. 1977 Dec 23;198(4323):1215–1221. doi: 10.1126/science.337492. [DOI] [PubMed] [Google Scholar]
- Maines M. D., Kappas A. Study of the developmental pattern of heme catabolism in liver and the effects of cobalt on cytochrome P-450 and the rate of heme oxidation during the neonatal period. J Exp Med. 1975 Jun 1;141(6):1400–1410. doi: 10.1084/jem.141.6.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maines M. D. Zinc . protoporphyrin is a selective inhibitor of heme oxygenase activity in the neonatal rat. Biochim Biophys Acta. 1981 Mar 18;673(3):339–350. doi: 10.1016/0304-4165(81)90465-7. [DOI] [PubMed] [Google Scholar]
- Rosenberg D. W., Drummond G. S., Kappas A. The influence of organometals on heme metabolism. In vivo and in vitro studies with organotins. Mol Pharmacol. 1982 Jan;21(1):150–158. [PubMed] [Google Scholar]
- Sassa S., Drummond G. S., Bernstein S. E., Kappas A. Tin-protoporphyrin suppression of hyperbilirubinemia in mutant mice with severe hemolytic anemia. Blood. 1983 May;61(5):1011–1013. [PubMed] [Google Scholar]
- Tenhunen R., Marver H. S., Schmid R. Microsomal heme oxygenase. Characterization of the enzyme. J Biol Chem. 1969 Dec 10;244(23):6388–6394. [PubMed] [Google Scholar]
- Tenhunen R., Marver H. S., Schmid R. The enzymatic conversion of heme to bilirubin by microsomal heme oxygenase. Proc Natl Acad Sci U S A. 1968 Oct;61(2):748–755. doi: 10.1073/pnas.61.2.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshinaga T., Sassa S., Kappas A. Purification and properties of bovine spleen heme oxygenase. Amino acid composition and sites of action of inhibitors of heme oxidation. J Biol Chem. 1982 Jul 10;257(13):7778–7785. [PubMed] [Google Scholar]