Abstract
The Gram-negative bacterium Francisella tularensis is the causative agent of tularemia. Interest in this zoonotic pathogen has increased due to its classification as a category A agent of bioterrorism, but little is known about the molecular mechanisms underlying its virulence, and especially what secretion systems and virulence factors are present. In this study, we characterized two genes in the F. tularensis genome, tolC and a gene we term ftlC, whose products have high homology with the Escherichia coli TolC protein. TolC functions as the outer membrane channel component for both type I secretion and multidrug efflux systems. We constructed deletion mutations of these genes in the F. tularensis live vaccine strain by allelic replacement. Deletion of either tolC or ftlC caused increased sensitivity to various antibiotics, detergents, and dyes, indicating both genes are involved in the multidrug resistance machinery of F. tularensis. Complementation of the deletion mutations in trans restored drug resistance. Neither tolC nor ftlC was required for replication of the live vaccine strain in murine bone marrow-derived macrophages. However, deletion of tolC, but not ftlC, caused a significant attenuation of virulence in a mouse model of tularemia that could be complemented by addition of tolC in trans. Thus, tolC is a critical virulence factor of F. tularensis in addition to its role in multidrug resistance, which suggests the presence of a functional type I secretion system.
Keywords: multidrug efflux, type I secretion, bacterial pathogenesis
Tularemia is a zoonotic disease caused by the Gram-negative bacterium Francisella tularensis (1, 2). The disease in humans is quite variable and related to the route of infection, which can include arthropod bites (ticks and flies), manipulation of animal carcasses, ingestion of contaminated water or food, and inhalation of aerosolized bacteria. This last route of infection results in pneumonic tularemia, the most severe form of the disease, with a mortality rate of up to 60% if not treated with antibiotics (3). Aerosolized F. tularensis is extremely infectious, with as few as 10 organisms being sufficient to cause disease (3). This high infectivity has led to classification of F. tularensis by the Centers for Disease Control and Prevention as a category A agent of bioterrorism (3–5).
F. tularensis belongs to the γ subgroup of Proteobacteria (6). It is a pleomorphic, nonmotile, facultative intracellular pathogen that is able to survive and replicate inside macrophages and amoebae (7). The Francisella genus contains two main subspecies that cause disease in humans: subspecies tularensis or type A, which is found mainly in North America and is highly virulent; and subspecies holarctica or type B, which is well distributed in Eurasia, found less frequently in North America, and produces a milder form of the disease in humans. The live vaccine strain (LVS), which was developed in the former Soviet Union, belongs to this latter subspecies (3). The LVS is an attenuated strain, but the basis for its attenuation is not known, and its use as a vaccine has been restricted. The LVS retains high virulence in mice and is widely used in laboratory studies due to its relative safety compared to fully virulent strains. There are two additional subspecies of F. tularensis: subspecies novicida, which also has been used extensively in laboratory studies, and subspecies mediasiatica. Both of these subspecies are rarely pathogenic in humans. Although interest in understanding the pathogenesis of F. tularensis has greatly increased after its listing as a category A bioterrorism agent, little is known about the molecular mechanisms underlying its virulence, largely due to an absence of genetic tools. New tools are becoming available, and the study of F. tularensis has been greatly aided by publication of the genome sequence of the highly virulent SchuS4 strain (subspecies tularensis; ref. 8) and the availability of the LVS genome sequence (http://bbrp.llnl.gov/bbrp/html/microbe.html). The known virulence factors of F. tularensis include a capsule that protects the bacteria against serum-mediated lysis (9) and the presence of a duplicated pathogenicity island that encodes genes essential for survival and multiplication inside macrophages (10). F. tularensis produces an unusual LPS that has low toxicity and elicits a low proinflammatory response compared with other bacteria (11, 12). In addition, F. tularensis expresses surface fibers and contains genes coding for a type 4 pilus system (13).
Gram-negative bacteria have a complex cell envelope comprising a cytoplasmic or inner membrane (IM), periplasm, peptidoglycan cell wall, and outer membrane (OM). Gram-negative bacteria have developed sophisticated systems to secrete proteins across this envelope (14); these systems are critical for the secretion of virulence factors and are required for bacterial pathogenesis. However, examination of the F. tularensis genome reveals a surprising lack of secretion systems (8). For example, type III or type IV secretion systems, which can inject virulence factors inside host cells and are commonly found in intracellular Gram-negative pathogens (14), are not present in the F. tularensis genome. To date, except for the capsule, only the type 4 pilus biogenesis system has been described in F. tularensis (13). Given the high infectivity of F. tularensis, additional systems for the expression and secretion of virulence factors are likely to be present. Identification and characterization of these systems will elucidate mechanisms of F. tularensis pathogenesis and will provide targets for the development of novel therapeutic agents.
We report here that the F. tularensis genome encodes two orthologs of the Escherichia coli TolC protein that we term tolC and ftlC. TolC is the prototypical OM channel component used by multidrug efflux pumps and the type I secretion system. The type I secretion system is a three-component system, in which TolC interacts with an IM ATPase and a periplasmic accessory or adaptor protein (15). Type I secretion systems are important for the virulence of a variety of Gram-negative bacteria and are required for the secretion of different toxins, proteases, and lipases (15–17). The prototypical E. coli type I secretion system is required for hemolysin secretion (18). TolC is also involved in multidrug efflux systems that are responsible for resistance to a broad range of detergents, dyes, and antibiotics (19).
We used an allelic replacement method to delete tolC and ftlC in the LVS. Analysis of the deletion mutants revealed that both TolC orthologs in F. tularensis are involved in multidrug efflux. In addition, tolC, but not ftlC, is required for virulence of the LVS in a mouse infection model, although neither gene was required for replication in macrophages. This identifies tolC as an important virulence factor of F. tularensis and suggests that tolC may function as part of a type I secretion system in addition to multidrug efflux.
Results
F. tularensis Has Two Genes with High Homology to TolC.
Using blast analysis of the F. tularensis SchuS4 genome (8, 20), we identified two ORFs sharing significant homology with the E. coli TolC protein (NP_755652; Fig. 1A). TolC is the prototypical OM channel component of both type I protein secretion and multidrug efflux systems (15, 17). One F. tularensis ortholog was already annotated as tolC (FTT1724) in the SchuS4 genome. For the second ortholog, which is annotated as a hypothetical gene (FTT1095), we propose the name ftlC, for Francisella tolC.blast analysis of the LVS genome (http://bbrp.llnl.gov/bbrp/html/microbe.html) revealed that it also contains both tolC and ftlC, and that both genes are intact. In addition, we amplified both genes from F. tularensis subspecies novicida strain U112 by PCR. Sequencing of the PCR products revealed that both genes are intact in U112 as well (GenBank accession nos. DQ394299 for tolC and DQ394298 for ftlC).
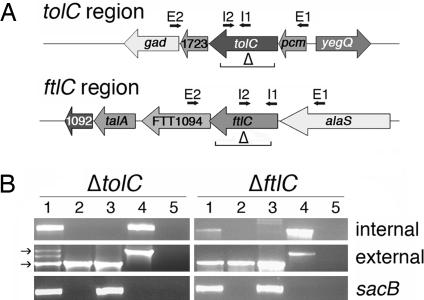
Fig. 1.
Construction and validation of the DTH1 and DTB3 mutants. (A) Chromosomal regions encoding tolC and ftlC. The genes and predicted functions in the tolC locus are: gad, glutamate decarboxylase; FTT1723, 4′-phosphopantetheinyl transferase; pcm, protein l-isoaspartate O-methyltransferase; yegQ, protease. tolC may be in an operon together with pcm and FTT1723, with a possible promoter located upstream of pcm. The genes and predicted functions in the ftlC locus are: FTT1092, hypothetical protein; talA, transaldolase; FTT1094, cytosol aminopeptidase; alaS, alanyl tRNA synthetase. ftlC likely forms an operon together with FTT1094 and possibly alaS. The regions deleted in tolC and ftlC are indicated, as are the locations of the internal (I1 and I2) and external (E1 and E2) primers used for PCR. (B) Genotypic validation of strains DTH1 (ΔtolC) and DTB3 (ΔftlC). PCR was performed by using primers internal or external to the targeted gene (as shown in A) or to sacB. Lanes: 1, intermediate strain; 2, final deletion strain (DTH1 or DTB3); 3, suicide vector (pPVTAH1 or pPVTBH3); 4, LVS; 5, water control. The arrows on the left indicate the expected positions of the intact and truncated versions of the targeted gene.
F. tularensis tolC and ftlC code for proteins of 509 and 460 amino acids, respectively, compared to 506 amino acids for E. coli TolC. F. tularensis TolC has 20% identity and 32% similarity (identical plus similar residues) with E. coli TolC. FtlC has 18% identity and 30% similarity with E. coli TolC. F. tularensis TolC and FtlC share 23% identity and 38% similarity with each other, and both proteins are highly conserved among the three Francisella subspecies (Fig. 4, which is published as supporting information on the PNAS web site). Both F. tularensis proteins contain predicted leader sequences, with the cleavage site for TolC located between residues 19 and 20 (ALA↓NE) and for FtlC between residues 23 and 24 (SIA↓NP). TolC and FtlC are predicted to localize to the OM, and both contain duplicate domains belonging to the OM efflux protein family (pfam02321; ref. 21). These domains are hallmarks of TolC proteins and form part of the TolC domain (COG1538; ref. 22). The ftlC gene has an unusual initial codon (TTG), which suggests that the expression of this protein is low. The tolC gene is surrounded by two ORFs that encode transferases and could be part of an operon together with these two genes (Fig. 1A). A predicted promoter is located upstream of the pcm gene. The ftlC gene is surrounded by alaS and ORF FTT1094, which encodes an aminopeptidase (Fig. 1A). The initial codon for FTT1094 is within ftlC and is likely part of an operon together with ftlC and possibly alaS.
Construction of LVS Mutants Deleted for tolC or ftlC.
Tools for the genetic manipulation of F. tularensis have only recently become available (23–28). We used the allelic replacement method of Golovliov et al. (23) to construct deletion mutations of tolC and ftlC in the LVS. To obtain the deletion mutants, the medium composition and other parameters of the protocol were optimized, as described in detail in Supporting Text, which is published as supporting information on the PNAS web site. Proper construction of strains DTH1 (ΔtolC) and DTB3 (ΔftlC) was validated both phenotypically and genotypically. Intermediate strains obtained after the first recombination event, which contain the crg and sacB genes from the suicide vector integrated into the chromosome (Fig. 5, which is published as supporting information on the PNAS web site), were resistant to chloramphenicol and sensitive to sucrose compared with the parental LVS (Fig. 6, which is published as supporting information on the PNAS web site). In contrast, the final deletion strains, obtained after the second recombination event, were sensitive to chloramphenicol and resistant to sucrose (Fig. 6). PCR products could be amplified from the intermediate strains by using primer pairs both internal and external to tolC or ftlC (Fig. 1B). The expected simultaneous presence of the intact and truncated target gene (Fig. 5) was detected in the tolC intermediate strain (Fig. 1B Left, lane 1). However, only the amplicon corresponding to the truncated gene was detected in the ftlC intermediate strain (Fig. 1B Right, lane 1). We believe this was due to preferential amplification of the smaller PCR product from the truncated gene. Note that in both intermediate strains, integration of the suicide plasmid was verified by amplification of the sacB gene (Fig. 1B, lane 1). In contrast to the intermediate strains, only the external primers generated products with the final deletion strains (Fig. 1B, lane 2). The amplicons were smaller in size compared to the parental LVS (Fig. 1B, lane 4), as expected for deletion of the genes. In addition, sacB was no longer detected in the final deletion strains (Fig. 1B, lane 2), confirming loss of the vector genes during the second recombination event. We also verified that all intermediate and final strains were F. tularensis and not contaminants by using PCR to detect the F. tularensis pilT gene (ref. 13; data not shown).
TolC and FtlC Are Part of the Multidrug Resistance Machinery of F. tularensis.
TolC serves as the OM channel component for multidrug efflux pumps that provide resistance to a variety of antibiotics, detergents, dyes, and other harmful compounds (15, 19). In fact, TolC mutants of E. coli exhibit increased sensitivity to these substances (29). We tested strains DTH1 (ΔtolC) and DTB3 (ΔftlC) for sensitivity to a variety of agents by using a disk diffusion assay. As shown in Table 1, both deletion mutants had increased sensitivity to a number of different antibiotics, detergents, and dyes compared to the parental LVS. Thus, both tolC and ftlC participate in multidrug resistance in F. tularensis. The drug-sensitivity profiles for strains DTH1 and DTB3 were similar, suggesting either that TolC and FtlC participate in the same multidrug efflux pathway or that independent efflux systems are present that recognize similar substrates. Deletion of tolC or ftlC did not increase sensitivity to all drugs tested; therefore, the drug resistance phenotype was not due to a nonspecific effect on the bacteria or a defect in OM integrity due to loss of TolC or FtlC. This conclusion is supported by the fact that no increased sensitivity to vancomycin, which is unable to penetrate the intact OM of Gram-negative bacteria (30), was detected in the mutant strains (Table 1). Furthermore, the OM protein profiles of DTH1 and DTB3 were similar to the profile of the parental LVS, and no differences in the LPS profiles of the strains were observed (data not shown). Finally, the DTH1 and DTB3 deletion strains exhibited no growth defects on solid or in liquid media (data not shown).
Table 1.
Drug sensitivity of the LVS, ΔtolC, and ΔftlC mutants and complemented strains
| Drug class | Name | Micrograms per disk | LVS | DTH1 | DTB3 | DTH1/pGPTA | DTB3/pGPTB |
|---|---|---|---|---|---|---|---|
| Penicillins | Ampicillin | 10 | 6 ± 0* | 6 ± 0 | 6 ± 0 | ND† | ND |
| Aminoglycosides | Streptomycin | 10 | 20 ± 1 | 25 ± 1 | 23 ± 1 | 23 ± 1 | 21 ± 1 |
| Gentamicin | 10 | 27 ± 1 | 32 ± 1 | 31 ± 1 | 29 ± 1 | 29 ± 1 | |
| Kanamycin | 5 | 18 ± 1 | 22 ± 1 | 20 ± 0 | ND | ND | |
| Tetracyclines | Tetracycline | 5 | 29 ± 1 | 33 ± 2 | 34 ± 1 | 29 ± 2 | 29 ± 2 |
| Macrolides | Erythromycin | 15 | 6 ± 0 | 6 ± 0 | 6 ± 0 | ND | ND |
| Quinolones | Nalidixic acid | 30 | 25 ± 1 | 30 ± 3 | 27 ± 1 | 26 ± 3 | 27 ± 1 |
| Others | Polymyxin B | 100 | 6 ± 0 | 6 ± 0 | 6 ± 0 | ND | ND |
| Chloramphenicol | 5 | 20 ± 1 | 24 ± 1 | 26 ± 1 | 21 ± 1 | 22 ± 1 | |
| Vancomycin | 20 | 6 ± 0 | 6 ± 0 | 6 ± 0 | 6 ± 0 | 6 ± 0 | |
| Novobiocin | 30 | 18 ± 1 | 21 ± 1 | 22 ± 1 | 16 ± 1 | 17 ± 1 | |
| Detergents | SDS | 750 | 9 ± 1 | 13 ± 1 | 13 ± 1 | 10 ± 1 | 9 ± 1 |
| Deoxycholate | 100 | 6 ± 0 | 10 ± 1 | 10 ± 0 | 6 ± 0 | 6 ± 0 | |
| Dyes | Acriflavin | 25 | 18 ± 1 | 19 ± 1 | 19 ± 1 | 19 ± 0 | 19 ± 0 |
| Ethidium bromide | 5 | 6 ± 0 | 18 ± 1 | 17 ± 1 | 6 ± 0 | 6 ± 0 |
*Average diameter of the zone of inhibition (including filter disk) in millimeters ± standard deviation. The diameter of the filter disk is 6 mm.
†ND, not determined. The plasmids used in the complemented strains confer resistance to ampicillin and kanamycin (26).
Vectors for stable gene expression in F. tularensis have only recently become available (26, 31). We cloned the tolC and ftlC genes from the LVS by PCR and placed them under control of the constitutive groE promoter in the F. tularensis expression vector pFNLTP6-gro-gfp (26). The resulting plasmids, pGPTA (tolC) and pGPTB (ftlC), were used to complement the deletion strains DTH1 and DTB3, respectively. As shown in Table 1, expression of tolC or ftlC in trans restored drug sensitivity of the mutants back to levels matching the parental LVS. This observation confirms that the multidrug sensitivity of the deletion strains was due to loss of tolC or ftlC and was not caused by a secondary effect.
Deletion of tolC Attenuates Virulence of the LVS in Mice.
We next examined the roles of tolC and ftlC in virulence by using a mouse model of tularemia. Groups of five mice were inoculated intradermally with the LVS, DTH1 (ΔtolC), or DTB3 (ΔftlC), and the mice were monitored for survival for 15 days. In the experiment shown in Fig. 2A, mice inoculated with 107 cfu of the LVS or strain DTB3 began succumbing to the infection 2 and 3 days after inoculation, and all mice died by day 5. In comparison, strain DTH1 was highly attenuated, with only one mouse dying on day 5 (Fig. 2A). Similarly, none of the mice inoculated with 106 cfu of strain DTH1 succumbed to infection (Fig. 2B), whereas four or three mice inoculated with the LVS or DTB3, respectively, died by day 6. In total, 91% of mice inoculated with 107 or 106 cfu of the LVS died compared to only 17% of mice inoculated with strain DTH1 (Table 2, which is published as supporting information on the PNAS web site). Thus, tolC is critical for virulence of the LVS in mice by the intradermal route. In contrast, ftlC does not appear to play an important role in virulence, because strain DTB3 behaved similarly to the LVS (Fig. 2 and Table 2).
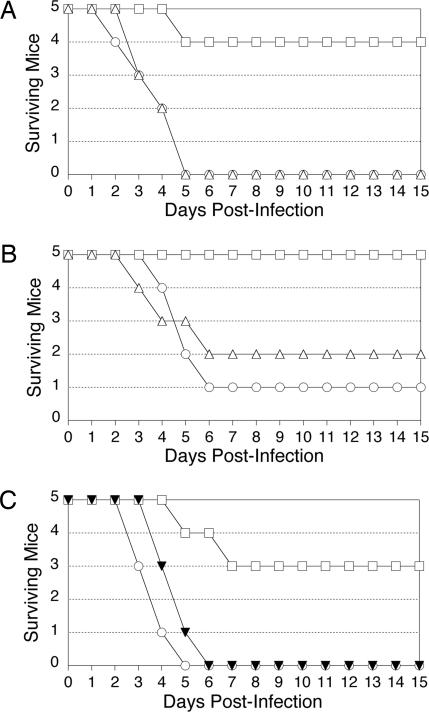
Fig. 2.
Mouse infection experiments. In all experiments, groups of five mice were inoculated intradermally and monitored for survival for 15 days. (A) Infection with 107 cfu of the parental LVS, DTH1 (ΔtolC), or DTB3 (ΔftlC). (B) Infection with 106 cfu of the LVS, DTH1, or DTB3. (C) Infection with 107 cfu of the LVS, DTH1, or DTH1/pGPTA (tolC). Symbols: circles, LVS; triangles, DTB3; squares, DTH1; and black triangles, DTH1/pGPTA.
To confirm the role of tolC in virulence, we conducted mouse experiments as described above, comparing the LVS, strain DTH1, and DTH1 complemented with plasmid pGPTA (tolC). As shown in Fig. 2C and Table 2, expression of tolC in trans restored the virulence of DTH1 when mice were inoculated with 107 cfu. This confirms that the virulence defect of strain DTH1 was specifically due to loss of tolC. However, complementation of the tolC deletion was partial, because no mice inoculated with 106 cfu DTH1/pGPTA succumbed to infection (Table 2). This was likely due to use of the heterologous groE promoter to drive expression of tolC from plasmid pGPTA. Nonetheless, our results clearly demonstrate that tolC is an important virulence determinant of the LVS.
tolC and ftlC Are Not Required for Replication of the LVS in Macrophages.
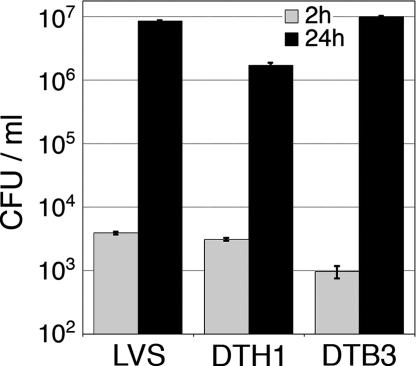
F. tularensis is capable of surviving and replicating inside macrophages (32, 33). This ability is critical for virulence, because mutants of F. tularensis defective for replication in macrophages are attenuated in the mouse infection model (7, 10, 23). To determine whether the attenuation of the DTH1 strain was due to an inability to replicate in macrophages, we examined the growth of DTH1, DTB3, and the LVS in murine bone marrow-derived macrophages (muBMDM). Macrophages were infected with the bacteria at a multiplicity of infection of 50 and inspected at 2 and 24 h after infection for bacterial replication by indirect immunofluorescence microscopy and determination of viable intracellular bacteria. At 2 h after infection, association of the parental LVS and mutant strains with the muBMDM was similar, with infection rates of ≈40% and viable bacterial counts of 103 cfu per milliliter (Fig. 3 and Fig. 7, which is published as supporting information on the PNAS web site). At 24 h after infection, significant increases in intracellular bacteria were observed for macrophages infected with all strains, giving viable bacterial counts of 106-107 cfu per milliliter (Figs. 3 and 7). Thus, tolC and ftlC are not required for replication of the LVS in macrophages. However, strain DTH1 (ΔtolC) consistently showed a slight replication defect compared to the parental LVS or DTB3 (ΔftlC), yielding 5-fold lower cfu at 24 h after infection (Figs. 3 and 7). This observation suggests that tolC, but not ftlC, is required for optimal growth in macrophages. The slight replication defect of strain DTH1 in muBMDM could be complemented by addition of plasmid pGPTA (tolC; data not shown). Because the DTH1 and DTB3 mutant strains exhibited increased sensitivity to gentamicin compared to the wild-type LVS (Table 1), we conducted the macrophage infection experiments without adding gentamicin to kill extracellular bacteria. However, experiments performed with addition of gentamicin gave identical results (data not shown).
Fig. 3.
Macrophage infection experiments. muBMDM were infected with the parental LVS, DTH1 (ΔtolC), or DTB3 (ΔftlC) at a multiplicity of infection of 50. The macrophages were lysed at 2 and 24 h after infection and plated to determine viable intracellular bacteria (cfu per milliliter). Error bars indicate standard deviations of triplicate samples. Strain DTH1 consistently showed a slight replication defect at 24 h compared to the wild-type LVS (P < 0.01; unpaired analysis of variance and Tukey–Kramer multiple comparison post-test).
Discussion
We show here that F. tularensis contains two genes, tolC and ftlC, encoding proteins homologous to E. coli TolC, which is the prototypical OM channel component involved in multidrug resistance and type I secretion. Both tolC and ftlC are highly conserved among the three subspecies of F. tularensis studied and free of disabling mutations, indicating the genes play important roles in the biology of this pathogen. We found that both F. tularensis orthologs, similar to E. coli TolC, participate in multidrug resistance. Furthermore, mouse infection experiments demonstrated that tolC is a significant virulence determinant of F. tularensis.
Tools for the genetic manipulation of F. tularensis have only recently become available; only a few techniques have been described for the generation and complementation of mutants in the LVS (23, 25–28, 31). We deleted the tolC and ftlC genes in the LVS by using an allelic exchange protocol (23). A number of parameters of the protocol were optimized to obtain the mutants successfully, and detailed procedures for construction and complementation of the mutant strains are provided in Supporting Text. This optimized protocol also was used to generate a mutation of the sodB gene in the LVS (34). The ΔtolC and ΔftlC LVS strains were sensitive to a variety of antibiotics, detergents, and dyes, indicating that TolC and FtlC form part of the multidrug resistance machinery of F. tularensis. The absence of the OM channel component prevents the bacteria from pumping such drugs to the external environment, leading to the accumulation of the drugs and producing greater sensitivity. The drug sensitivity of the ΔtolC and ΔftlC LVS mutants was restored back to wild-type levels upon complementation with the deleted genes in trans. It is important to note that gene complementation in F. tularensis has been done rarely and not always with a successful outcome (10, 35).
In addition to increased drug sensitivity, we found that the ΔtolC LVS mutant was highly attenuated for virulence in mice when inoculated by the intradermal route. Moreover, this attenuation was reversed when the gene was reintroduced in trans, indicating the virulence defect was due specifically to the deletion of tolC. Complementation of the ΔtolC mutation was partial, because virulence was restored for the 107 but not the 106 inoculum (Table 2). This partial complementation may be explained by constitutive and likely excessive expression of tolC from the heterologous groE promoter (26), as compared to its natural promoter. Previously characterized F. tularensis mutants attenuated for virulence in mice were also severely defective for replication in macrophages (7, 10, 23). In contrast, our ΔtolC mutant exhibited only a slight growth defect in murine macrophages. Although it is possible that this defect is amplified within the host and could account for the virulence attenuation of the ΔtolC strain, this result argues for a function of TolC in F. tularensis pathogenesis separate from growth in macrophages.
Only the ΔtolC mutant had a virulence defect in mice, despite the fact that both ΔtolC and ΔftlC showed equivalent increases in drug susceptibility. TolC and FtlC may participate in distinct multidrug efflux systems, with overlapping but different substrate profiles. Thus, the ΔtolC mutant may not be able to pump out a harmful agent encountered in vivo, whereas the ΔftlC mutant retains this ability (16). A second and more exciting possibility is that tolC participates in a type I secretion system in addition to its role in multidrug efflux, whereas ftlC participates only in drug efflux. If this is the case, TolC may be involved in the secretion of a toxin or other factor important for the pathogenesis of F. tularensis. Until now, no toxins have been described in F. tularensis (8), other than the presence of a potential hemolysin in F. tularensis subspecies novicida and Francisella philomiragia (36). This potential hemolysin appears to be absent in F. tularensis subspecies tularensis and holarctica. A F. tularensis virulence factor could also be secreted by a TolC-containing multidrug efflux system, because evidence from Pseudomonas aeruginosa suggests that multidrug efflux systems can secrete virulence determinants in addition to pumping out harmful compounds (37).
The presence of more than one TolC homolog and multiple multidrug efflux systems is common in Gram-negative bacteria (15, 16). In addition to the TolC OM efflux protein, multidrug efflux and type I secretion systems require a periplasmic adaptor protein and an IM energy-providing protein (15, 19). The F. tularensis genome contains a number of genes that could provide these additional components for multidrug efflux or protein secretion in conjunction with TolC and/or FtlC (8, 38). The IM component of type I secretion and some multidrug efflux pathways is an ATP-binding cassette (ABC) transporter. The genome of SchuS4 encodes 15 potential ABC transporters, five to seven of which may be involved in efflux or secretion (38). For multidrug efflux systems, the IM component is more commonly a proton antiporter belonging to either the resistance-nodulation division (RND) or major facilitator superfamily (MFS; ref. 15). ORF FTT0105 of the SchuS4 genome is homologous to the RND exporter AcrB, and ORF FTT1257 is homologous to the MFS exporter EmrB. The Acr and Emr systems work together with TolC in other bacteria to pump out a broad range of antibiotics and harmful compounds (15, 19).
In summary, we have described the presence of two genes, tolC and ftlC, that belong to the multidrug resistance machinery of F. tularensis. Significantly, we identified tolC as a new virulence factor of F. tularensis, which could participate in a type I secretion system for the export of a toxin or other virulence determinant critical for the pathogenesis of F. tularensis. These findings open new avenues for understanding the molecular basis underlying the high virulence of F. tularensis and provide new targets for the development of therapeutic agents. In addition, the virulence attenuation of the F. tularensis ΔtolC mutant holds promise for the construction of a defined attenuated vaccine strain.
Materials and Methods
Strains and Plasmids.
The strains and plasmids used in this study are described in Table 3, which is published as supporting information on the PNAS web site. F. tularensis strains were incubated at 37°C with 5% CO2 in different media as follows. The LVS was grown on Mueller–Hinton II chocolate agar plates (MHC) or in Mueller–Hinton broth (MHB), as described (12, 13). F. tularensis subspecies novicida U112 was grown in tryptic soy media supplemented with 0.1% cysteine (7). E. coli strains were grown on Luria agar plates or in LB supplemented with 10 μg/ml chloramphenicol, 100 μg/ml ampicillin, or 50 μg/ml of kanamycin, as appropriate.
Construction of the F. tularensis deletion mutants and complementation plasmids is described in detail in Supporting Text. Briefly, we used an allelic exchange protocol (23) to generate the LVS deletion mutants (Fig. 5). Regions upstream and downstream of tolC and ftlC (Fig. 1A) were PCR-amplified and ligated together into the pPV suicide vector (23), kindly provided by Anders Sjöstedt (Umeå University, Umeå, Sweden), which contains markers conferring chloramphenicol resistance and sucrose sensitivity. E. coli S17-1 was used to conjugate the suicide plasmids into the LVS, and chloramphenicol-resistant sucrose-sensitive colonies were screened by PCR to verify integration of the suicide plasmid into the target gene. Colonies were then grown on medium containing sucrose to select for the second recombination event and elimination of the vector sequences (Fig. 5). These colonies were again screened by PCR to verify deletion of the target gene and elimination of the vector. The final LVS ΔtolC and ΔftlC strains were named DTH1 and DTB3, respectively. Plasmids pGPTA and pGPTB, expressing tolC and ftlC, respectively, were constructed by PCR, amplifying the genes from the LVS and cloning them into vector pFNLTP6-gro-gfp (26), which was kindly provided by Thomas Zahrt (Medical College of Wisconsin, Milwaukee, WI). This placed the genes under the control of the F. tularensis groE promoter. The plasmids were transformed into DTH1 and DTB3 by electroporation (Supporting Text).
Identification and Analysis of Francisella TolC Orthologs.
F. tularensis tolC orthologs were identified by BLAST (20) by using the E. coli TolC protein sequence (NP_755652). BLAST analysis was performed against the genomes of F. tularensis SchuS4 (8) and F. tularensis LVS (http://bbrp.llnl.gov/bbrp/bin/f.tularensis_blast). The tolC and ftlC genes in F. novicida (strain U112) were amplified by PCR by using the primers listed in Table 4, which is published as supporting information on the PNAS web site. The amplicons were purified by using the Qiagen (Valencia, CA) Gel Purification kit and sequenced by using the BigDye terminator V3.1 cycle sequencing kit (Applied Biosystems, Foster City, CA). The sequences of TolC and FtlC from the three F. tularensis subspecies were aligned with E. coli TolC by using ClustalW (39) and the MacVector software program (Oxford Molecular, Madison, WI). The presence of conserved domains in the TolC homologs was investigated by using National Center for Biotechnology Information Structure (www.ncbi.nlm.nih.gov/Structure; ref. 40), the presence of a leader sequence was determined by using SignalP3 (www.cbs.dtu.dk/services/SignalP; ref. 41), and the cellular localization of the proteins was determined by using PsortB (www.psort.org/psortb; ref. 42). The locations of promoters and operons were investigated by using the FGENESB and BPROM programs available from Softberry (Mt. Kisco, NY).
Multidrug Sensitivity Assay.
F. tularensis strains were grown on MHC and then suspended into MHB. The bacteria were spread with a cotton swab onto MHC (supplemented with 1 μg/ml kanamycin for complemented strains) to obtain a bacterial lawn. Sterile disks (Becton Dickinson, San Jose, CA) soaked with different drugs, as indicated in Table 1, were placed on the plates. After 3 days, the growth inhibition halos around the disks were measured as the diameter of the zone of inhibition including the diameter of the disk (6 mm). The experiments were repeated at least three times for each drug and strain.
OM Preparations and LPS Profiles.
Strains were grown in 50 ml of MHB overnight at 37°C, with 5% CO2 and shaking at 100 rpm. Bacteria were harvested by centrifugation (7,500 × g, 5 min, 4°C), resuspended into 0.1 ml of 20 mM Tris·HCl, pH 8, containing Complete Protease Inhibitor mixture (Roche, Indianapolis, IN), and lysed by sonication. The lysate was centrifuged at 7,500 × g to pellet unbroken cells, and sarkosyl (sodium-N-laurylsarcosinate) was added to the supernatant fraction to 0.5% final concentration. The mixture was incubated for 5 min at 25°C to solubilize the IM, and the OM was pelleted by ultracentrifugation (100,000 × g, 1 h, 4°C). The pellet was resuspended into 50 μl of 20 mM Tris·HCl (pH 8), mixed with an equal volume of 2× SDS sample buffer, and incubated for 10 min at 95°C before separation by SDS/PAGE and staining with Coomassie blue.
For detection of LPS, 10 μl of OM, prepared as described above, was separated by SDS/PAGE, transferred to a poly(vinylidene difluoride) membrane (Osmonic, Gloucester, MA), and blotted with a murine monoclonal antibody to the LPS of the LVS strain (Abcam, Cambridge, MA).
Mouse Infection Experiments.
Groups of five 6- to 8-week-old C3H/HeN mice were infected intradermally with LVS, DTH1, DTB3, or DTH1/pGPTA. The bacteria were grown in MHB overnight to an OD600 of 0.2 and diluted in MHB to inoculate 107, 106, or 105 microorganisms per mouse. The animals were monitored for 15 days. All studies with mice were approved by the Institutional Animal Care and Use Committee of Stony Brook University.
Macrophage Infection Experiments.
muBMDM were obtained as described (43), resuspended in bone marrow medium [BMM; DMEM (Invitrogen, Carlsbad, CA) containing 2 mM l-glutamine, 1 mM sodium pyruvate, 20% heat-inactivated FBS (HyClone, Logan, UT), and 30% medium previously conditioned by L929 cells], and seeded on coverslips in 24-well plates at a concentration of 1.5 × 105 cells per well. The conditioned medium was obtained by plating 2 × 105 L929 cells in 75-cm2 culture flasks in Minimum Essential Medium (Invitrogen) containing 2 mM l-glutamine, 1 mM sodium pyruvate, 1 mM nonessential amino acids (Invitrogen), and 10% FBS and collecting the medium after 10 days. The muBMDM were used for experiments the next day. For each experiment, F. tularensis strains were streaked from frozen stocks to MHC, and a single colony was grown in MHB to late-log phase (16–18 h) at 37°C with shaking at 100 rpm in a 5% CO2 atmosphere. Aliquots of the bacterial cultures were centrifuged, resuspended in BMM, and added at a multiplicity of infection of 50 to the muBMDM. Bacterial concentrations were initially estimated by the OD600 of the suspension culture, and actual numbers of viable bacteria were determined by cfu counts on MHC. Plates were centrifuged for 3.5 min at 200 × g to facilitate contact between the macrophages and bacteria. After 2 h of coculture at 37°C, the muBMDM were washed extensively, and a set of wells was fixed for microscopy as described below. To measure viable intracellular bacteria, samples were lysed with water at 4°C for 10 min, and serial dilutions were plated to determine cfu. The remaining wells were incubated for a total of 24 h in BMM before determination of cfu or fixing for microscopy. In some experiments, after the 2-h washing step, cells were incubated with 5 μg/ml gentamicin for 1 h to kill any remaining extracellular bacteria. Cells were fixed with 2.5% p-formaldehyde for 30 min, washed with PBS, and permeabilized with 0.5% Triton X-100 in PBS. Cells were blocked with 3% BSA in PBS and stained with a 1:100 dilution of rabbit antiserum to F. tularensis followed by a goat fluorescein-conjugated anti-rabbit antibody (both from BD Biosciences, Lincoln Park, NJ).
Supplementary Material
Acknowledgments
We are grateful to Vitaly Pavlov (State Research Center for Applied Microbiology, Obolensk, Russia) for much helpful advice and consultation in establishing the allelic replacement technique for construction of the LVS deletion mutants. We thank Patricio Mena and Gloria Monsalve (Stony Brook University) for assistance with the mouse experiments and Karl Klose (University of Texas, San Antonio, TX) for providing F. tularensis subspecies novicida strain U112, Anders Sjöstedt (Umeå University, Umeå, Sweden) for providing plasmid pPV, and Thomas Zahrt (Medical College of Wisconsin, Milwaakee, WI) for providing plasmid pFNLTP6-gro-gfp. Preliminary LVS sequence data were obtained from the Biology and Biotechnology Research Program Sequencing Group at Lawrence Livermore National Laboratory (http://bbrp.llnl.gov/bbrp/html/microbe.html). This work was supported by National Institutes of Health Grant AI055621.
Abbreviations
- IM
inner membrane
- LVS
live vaccine strain
- MHB
Mueller–Hinton broth
- MHC
Mueller–Hinton chocolate agar plates
- muBMDM
murine bone marrow-derived macrophages
- OM
outer membrane.
Footnotes
Conflict of interest statement: No conflicts declared.
This paper was submitted directly (Track II) to the PNAS office.
References
- 1.McCoy G. W., Chapin C. W. J. Infect. Dis. 1912;10:61–72. [Google Scholar]
- 2.Petersen J. M., Schriefer M. E. Vet. Res. 2005;36:455–467. doi: 10.1051/vetres:2005006. [DOI] [PubMed] [Google Scholar]
- 3.Dennis D. T., Inglesby T. V., Henderson D. A., Bartlett J. G., Ascher M. S., Eitzen E., Fine A. D., Friedlander A. M., Hauer J., Layton M., et al. J. Am. Med. Assoc. 2001;285:2763–2773. doi: 10.1001/jama.285.21.2763. [DOI] [PubMed] [Google Scholar]
- 4.Feldman K. A., Stiles-Enos D., Julian K., Matyas B. T., Telford S. R., III, Chu M. C., Petersen L. R., Hayes E. B. Emerg. Infect. Dis. 2003;9:350–354. doi: 10.3201/eid0903.020462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rotz L. D., Khan A. L., Lillibridge S. R., Ostroff S. M., Hughes J. M. Emerg. Infect. Dis. 2002;8:225–230. doi: 10.3201/eid0802.010164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sjöstedt A. In: The Proteobacteria, Part B, Bergey’s Manual of Systematic Bacteriology. Brenner K., Staley G., editors. New York: Springer; 2005. pp. 200–210. [Google Scholar]
- 7.Lauriano C. M., Barker J. R., Yoon S. S., Nano F. E., Arulanandam B. P., Hassett D. J., Klose K. E. Proc. Natl. Acad. Sci. USA. 2004;101:4246–4249. doi: 10.1073/pnas.0307690101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Larsson P., Oyston P. C., Chain P., Chu M. C., Duffield M., Fuxelius H. H., Garcia E., Halltorp G., Johansson D., Isherwood K. E., et al. Nat. Genet. 2005;37:153–159. doi: 10.1038/ng1499. [DOI] [PubMed] [Google Scholar]
- 9.Sandström G., Lofgren S., Tärnvik A. Infect. Immun. 1988;56:1194–1202. doi: 10.1128/iai.56.5.1194-1202.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nano F. E., Zhang N., Cowley S. C., Klose K. E., Cheung K. K., Roberts M. J., Ludu J. S., Letendre G. W., Meierovics A. I., Stephens G., et al. J. Bacteriol. 2004;186:6430–6436. doi: 10.1128/JB.186.19.6430-6436.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sandström G., Sjöstedt A., Johansson T., Kuoppa K., Williams J. C. FEMS Microbiol. Immunol. 1992;5:201–210. doi: 10.1111/j.1574-6968.1992.tb05902.x. [DOI] [PubMed] [Google Scholar]
- 12.Forestal C. A., Benach J. L., Carbonara C., Italo J. K., Lisinski T. J., Furie M. B. J. Immunol. 2003;171:2563–2570. doi: 10.4049/jimmunol.171.5.2563. [DOI] [PubMed] [Google Scholar]
- 13.Gil H., Benach J. L., Thanassi D. G. Infect. Immun. 2004;72:3042–3047. doi: 10.1128/IAI.72.5.3042-3047.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kostakioti M., Newman C. L., Thanassi D. G., Stathopoulos C. J. Bacteriol. 2005;187:4306–4314. doi: 10.1128/JB.187.13.4306-4314.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koronakis V., Eswaran J., Hughes C. Annu. Rev. Biochem. 2004;73:467–489. doi: 10.1146/annurev.biochem.73.011303.074104. [DOI] [PubMed] [Google Scholar]
- 16.Nishino K., Latifi T., Groisman E. A. Mol. Microbiol. 2006;59:126–141. doi: 10.1111/j.1365-2958.2005.04940.x. [DOI] [PubMed] [Google Scholar]
- 17.Delepelaire P. Biochim. Biophys. Acta. 2004;1694:149–161. doi: 10.1016/j.bbamcr.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 18.Wandersman C., Delepelaire P. Proc. Natl. Acad. Sci. USA. 1990;87:4776–4780. doi: 10.1073/pnas.87.12.4776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nikaido H. J. Bacteriol. 1996;178:5853–5859. doi: 10.1128/jb.178.20.5853-5859.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Altschul S. F., Gish W., Miller W., Myers E. W., Lipman D. J. J. Mol. Biol. 1990;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 21.Bateman A., Coin L., Durbin R., Finn R. D., Hollich V., Griffiths-Jones S., Khanna A., Marshall M., Moxon S., Sonnhammer E. L. L., et al. Nucleic Acids Res. 2004;32:D138–D141. doi: 10.1093/nar/gkh121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tatusov R. L., Galperin M. Y., Natale D. A., Koonin E. V. Nucleic Acids Res. 2000;28:33–36. doi: 10.1093/nar/28.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Golovliov I., Sjöstedt A., Mokrievich A., Pavlov V. FEMS Microbiol. Lett. 2003;222:273–280. doi: 10.1016/S0378-1097(03)00313-6. [DOI] [PubMed] [Google Scholar]
- 24.Twine S., Bystrom M., Chen W., Forsman M., Golovliov I., Johansson A., Kelly J., Lindgren H., Svensson K., Zingmark C., et al. Infect. Immun. 2005;73:8345–8352. doi: 10.1128/IAI.73.12.8345-8352.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maier T. M., Pechous R., Casey M., Zahrt T. C., Frank D. W. Appl. Environ. Microbiol. 2006;72:1878–1885. doi: 10.1128/AEM.72.3.1878-1885.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maier T. M., Havig A., Casey M., Nano F. E., Frank D. W., Zahrt T. C. Appl. Environ. Microbiol. 2004;70:7511–7519. doi: 10.1128/AEM.70.12.7511-7519.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lauriano C. M., Barker J. R., Nano F. E., Arulanandam B. P., Klose K. E. FEMS Microbiol. Lett. 2003;229:195–202. doi: 10.1016/S0378-1097(03)00820-6. [DOI] [PubMed] [Google Scholar]
- 28.Kawula T. H., Hall J. D., Fuller J. R., Craven R. R. Appl. Environ. Microbiol. 2004;70:6901–6904. doi: 10.1128/AEM.70.11.6901-6904.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Whitney E. N. Genetics. 1971;67:39–53. doi: 10.1093/genetics/67.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vaara M., Nurminen M. Antimicrob. Agents Chemother. 1999;43:1459–1462. doi: 10.1128/aac.43.6.1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuoppa K., Forsberg A., Norqvist A. FEMS Microbiol. Lett. 2001;205:77–81. doi: 10.1111/j.1574-6968.2001.tb10928.x. [DOI] [PubMed] [Google Scholar]
- 32.Golovliov I., Baranov V., Krocova Z., Kovarova H., Sjöstedt A. Infect. Immun. 2003;71:5940–5950. doi: 10.1128/IAI.71.10.5940-5950.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bolger C. E., Forestal C. A., Italo J. K., Benach J. L., Furie M. B. J. Leukocyte Biol. 2005;77:893–897. doi: 10.1189/jlb.1104637. [DOI] [PubMed] [Google Scholar]
- 34.Bakshi C. S., Malik M., Regan K., Melendez J. A., Metzger D. W., Pavlov V. M., Sellati T. J. J. Bacteriol. 2006;188 doi: 10.1128/JB.00266-06. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lai X. H., Golovliov I., Sjöstedt A. Microb. Pathog. 2004;37:225–230. doi: 10.1016/j.micpath.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 36.Lai X. H., Wang S. Y., Edebro H., Sjöstedt A. FEMS Microbiol. Lett. 2003;224:91–95. doi: 10.1016/S0378-1097(03)00431-2. [DOI] [PubMed] [Google Scholar]
- 37.Hirakata Y., Srikumar R., Poole K., Gotoh N., Suematsu T., Kohno S., Kamihira S., Hancock R. E. W., Speert D. P. J. Exp. Med. 2002;196:109–118. doi: 10.1084/jem.20020005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Atkins H. S., Dassa E., Walker N. J., Griffin K. F., Harland D. N., Taylor R. R., Duffield M. L., Titball R. W. Res. Microbiol. 2006;157:593–604. doi: 10.1016/j.resmic.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 39.Thompson J. D., Higgins D. G., Gibson T. J. Nucleic Acids Res. 1994;22:4673–4680. doi: 10.1093/nar/22.22.4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marchler-Bauer A., Bryant S. H. Nucleic Acids Res. 2004;32:327–331. doi: 10.1093/nar/gkh454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bendtsen J. D., Nielsen H., von Heijne G., Brunak S. J. Mol. Biol. 2004;340:783–795. doi: 10.1016/j.jmb.2004.05.028. [DOI] [PubMed] [Google Scholar]
- 42.Gardy J. L., Laird M. R., Chen F., Rey S., Walsh C. J., Ester M. Bioinformatics. 2005;21:617–623. doi: 10.1093/bioinformatics/bti057. [DOI] [PubMed] [Google Scholar]
- 43.Celada A., Gray P. W., Rinderknecht E., Schreiber R. D. J. Exp. Med. 1984;160:55–74. doi: 10.1084/jem.160.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.