Abstract
Context: Recommendations for heat illness prevention provided by sports medicine associations do not always account for sex differences, specific age populations, regional environmental conditions, equipment worn during activity, or the athlete's size or preexisting level of fitness.
Objective: To evaluate the rate of exertional heat illness (EHI) among collegiate football athletes and to monitor environmental conditions during American football practice for a 3-month period.
Design: Epidemiologic study in which we reviewed the occurrence rates of EHI and wet bulb globe temperature readings during a 3-month period of American collegiate football practice sessions.
Setting: Five universities in the southeastern region of the United States.
Patients or Other Participants: Collegiate football players at the 5 universities.
Main Outcome Measure(s): Wet bulb globe temperatures were recorded from August through October 2003, at the beginning, middle, and end of each practice session. The EHIs were identified and recorded, and athlete-exposures (AEs) were calculated.
Results: A total of 139 EHIs and 33 196 AEs were reported (EHI rate = 4.19/1000 AEs). The highest incidence of EHIs was in August (88%, EHI rate = 8.95/1000 AEs) and consisted of 70% heat cramps (6.13/1000 AEs), 23% heat exhaustion (2.06/ 1000 AEs), and 7% heat syncope (0.58/1000 AEs). No cases of heat stroke or hyponatremia were identified. The highest risk of EHI occurred during the first 3 weeks of the study; mean wet bulb globe temperature declined significantly as the study continued ( P < .001). Temperatures in the final 5 weeks of the study were significantly cooler than in the first 5 weeks ( P < .05).
Conclusions: Heat cramps were the most common EHI and occurred most often during the first 3 weeks of practice. Athletic trainers should take all necessary preventive measures to reduce the risk of EHI.
Keywords: heat stress, Heat Stress Index, wet bulb globe temperature, exercise-associated muscle cramps
Stressful environmental conditions can present numerous problems for the athletic participant. Exertional heat illness (EHI) is often associated with physical activity in a hot and humid environment; the incidence of EHI is correlated with the rise in ambient air temperature and humidity. 1 Extreme environmental heat places significant stress on the body's ability to perform while thermoregulatory responses are occurring in various internal organs. 2 These responses include mobilizing nutrients and electrolytes and maintaining an appropriate equilibrium of body fluids and increasing body temperature, pH, and blood pressure. If the organ systems do not respond appropriately, the athlete may develop a serious and potentially catastrophic medical condition.
From 1979 through 1999, the Centers for Disease Control and Prevention reported 8015 deaths among the general population that were attributable to heat-related illnesses as a result of exposure to excessive heat in the United States. 3 Although most of these fatalities were not sport related, the recent and untimely deaths of several professional, collegiate, and high school athletes as a result of heat-related illnesses have generated national attention related to the risk of exertional heat stress illnesses among athletes. Many professional organizations have published position statements 4–12 regarding the appropriate ways to recognize, treat, and prevent these illnesses.
To guard against EHI during athletic events, the American College of Sports Medicine (ACSM) has studied the effects of heat stress and has made specific recommendations (ie, position statements) regarding the participation of individuals in stressful environments. These recommendations consist of guidelines that measure heat stress and define the severity of heat stress by a Wet Bulb Globe Temperature (WBGT) Index. 12 Based on the WBGT at the time of the event, the ACSM also has recommendations regarding the type, duration, and frequency of exercise regimes for a particular day, the frequency of hydration and rest breaks, and whether or not the activity should be moved to a different time of day or canceled altogether. 10
The WBGT Index is the most widely accepted measure of environmental conditions and is used as a monitoring guideline for activities in both athletics and industry. The development of the WBGT equation is well supported by the research performed by Yaglou and Minard 13 and is referenced by many agencies and governing bodies. 3–5, 8, 11, 12, 14–18 The WBGT Index is derived from 3 independent environmental readings: dry bulb temperature (ambient air temperature, dt), wet bulb temperature (humidity, wbt), and black globe temperature (radiant heat, bgt) using the equation below 13:
| WBGT Index = 0.7wbt + 0.2bgt + 0.1dt |
Using the WBGT Index score along with published guidelines allows sports medicine professionals to make decisions regarding the intensity, length, time of day, and required rest periods for exercise sessions in hot and humid environments.
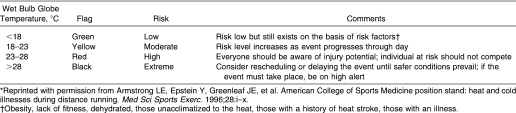
Since 1975, ACSM has published 3 position statements addressing the prevention of heat illnesses as it applies to distance running. 10, 12, 19 The original statement was updated in 1987 to include thermal injuries affecting not only distance runners but also the general population. 10 In 1996, the ACSM again updated the position statement by addressing exercise in extreme environmental conditions for both the recreational jogging community and elite distance runners, as seen in Table 1. 12 This guideline includes a WBGT Index Risk Chart that delineates temperature ranges and descriptive terminology for potential environmental heat stress.
Table 1. American College of Sports Medicine Wet Bulb Globe Temperature Index Risk Chart 5,12* .
The ACSM Risk Chart recommendations were derived for the general community, recreational joggers, and elite distance runners. These recommendations are to be applied to all geographic areas of the United States and do not take into account sex differences, specific age populations, environmental conditions unique to the different regions of the country, equipment worn during activity, or the size or preexisting level of conditioning or fitness of the athlete. 10 Our purpose was to evaluate the WBGT and the incidence of EHI during American football practice sessions at 5 National Collegiate Athletic Association Division I Southeastern universities from August through October 2003.
METHODS
A total of 5 southeastern US Division I varsity football programs participated in this study. Data were collected from August through October 2003, during which time environmental readings, the number of athlete participants, and the number of EHIs occurring during football practice were recorded. A certified athletic trainer at each institution was responsible for all equipment setup, data collection, and information transmission to the researchers. Each athletic trainer was given a detailed instruction manual that included equipment setup instructions, definitions of EHIs, and reporting forms. Environmental conditions were monitored only for days on which football practice was held.
Definition of Illness
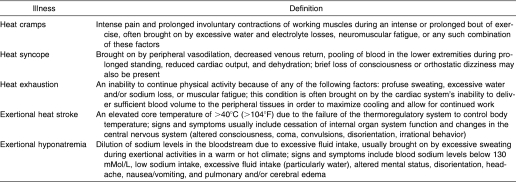
Exertional heat illness cases were defined using the National Athletic Trainers' Association position statement on EHIs 5 and were assessed by the medical and athletic training staff at each institution. We provided descriptions of the clinical signs and symptoms of EHIs for consistency of evaluation and assessment of these injuries (Table 2).
Table 2. Exertional Heat Illness Definitions 5 .
Instrumentation
Each participating athletic trainer was given a WBGT-103F Heat Stroke Checker (KEM Kyoto Electronics Manufacturing Co, Ltd, Tokyo, Japan). The Heat Stroke Checker is a portable, handheld environmental monitor, which records ambient air temperature, relative humidity, and globe temperature and calculates the WBGT. All environmental conditions were monitored and recorded at the beginning, middle, and end of each practice session; if multiple practices were held on a single day, the athletic trainer was asked to record data during both sessions. For collecting data, the Heat Stroke Checker was positioned in a sunny location, as near to the center of the practice field as possible, at the appropriate recording time. The reliability of each Heat Stroke Checker unit was evaluated using a Tenney Environmental Chamber (Lunaire Environmental, Williamsport, PA). We found strong correlations between the Heat Stroke Checker units and the environmental chamber as well as among the 5 units when recording WBGT (interclass r = 0.9930, intraclass r = 0.9993).
Data Analysis
Athletic trainers at all 5 schools submitted complete data on the number of EHIs. However, because of equipment difficulties, athletic trainers at only 4 schools submitted complete WBGT data. Mean WBGT was calculated for each practice based on the data reported by each institution. The number of EHIs and athlete-exposures (AEs) were summed from all reporting institutions, and the rates of EHIs were computed by dividing the total number of injuries by the total number of AEs. All EHI incidence rates are reported by 1000 AEs. This illness rate was calculated for each participating school and for each month the data were collected. The incidence of EHI for each ACSM Index Risk level (see Table 1) was based on the mean practice WBGT.
RESULTS
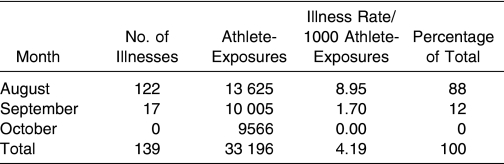
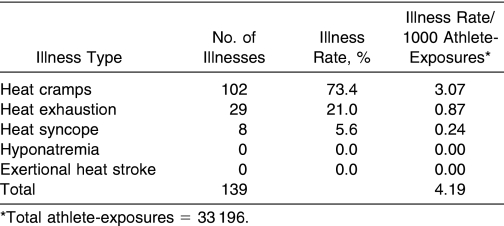
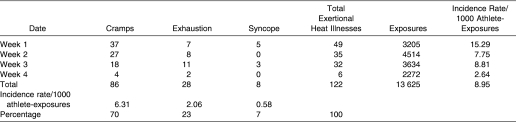
Athletic trainers at participating institutions reported a total of 139 EHIs during the 3-month period. The overall illness rate was greatest in August, with a sharp decline in the following months. The EHIs accounted for 88% of all illnesses in August and 12% in September; no EHIs were reported in October (Table 3). Heat cramps were the most frequently recorded illness, followed by heat exhaustion and then heat syncope (Table 4). We received no data from any school indicating an occurrence of heat stroke or hyponatremia in the 3-month period.
Table 3. Total Exertional Heat Illnesses by Month.
Table 4. Total Exertional Heat Illnesses by Type.
An evaluation of reported August EHIs shows that heat cramps had the highest overall illness rate, with lower illness rates found for heat exhaustion and heat syncope (Table 5). Of all reported cases in August, 70% (86/122) were heat cramps, 23% (28/122) were heat exhaustion, and 7% (8/122) were heat syncope. The greatest risk of EHI to athletes occurred during the first 3 weeks of practice: 84% (116/139) of all reported EHIs and 95% (116/122) of all August EHIs occurred during this time frame.
Table 5. August Exertional Heat Injuries.
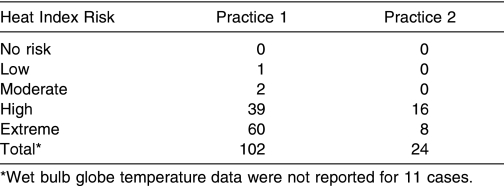
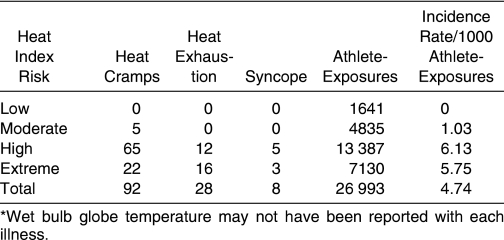
Wet Bulb Globe Temperature Indexes and Risk Relationship
Mean WBGT during practice for August was 28.98° ± 4.67°C for practice session 1 and 27.14° ± 2.70°C for practice session 2. Mean WBGT for each practice session was categorized by risk as outlined in the ACSM WBGT Risk Index Scale (Table 6). A total of 54.4% (68/125) of all August practices were conducted in the extreme range based on the ACSM scale. The numbers and types of EHI categorized by the ACSM risk index levels based on WBGT are presented in Table 7.
Table 6. Practices in Each Category of the American College of Sports Medicine Risk Index 12 .
Table 7. Exertional Heat Illnesses by American College of Sports Medicine Risk Index*.
DISCUSSION
Five Division I universities participated in this study, with 4 providing complete environmental and EHI data over a 90-day period in 2003. The data indicate that most EHIs occurred during the first 3 weeks of August, with heat cramps exhibiting the greatest illness rate. Heat exhaustion and heat syncope were also noted but at much lower rates. No cases of hyponatremia or heat stroke were reported. The vast majority of WBGT Index readings during all August practice sessions were in the extreme-risk or high-risk category based on the ACSM Risk Index.
Comparison of our data with those collected previously gives a variety of results. During the 1996 US Olympic Trials in Atlanta, GA, and the 1996 Atlanta Olympic Games, Martin 20, 21 monitored weather conditions and the number of heat-related medical encounters. A heat-related medical encounter was defined as 1 of 3 heat illnesses: heat exhaustion (including dehydration, electrolyte imbalance, dizziness, weakness, fatigue), heat cramps (painful muscle spasms), or heat syncope (fainting). Hyponatremia and heat stroke were not considered. The EHI risk rates for the Olympic Trials and the Olympics were 2.84/1000 AEs and 2.93/1000 AEs, respectively. Medical encounters related to EHIs were most common among athletes competing in long-distance running events and race-walking events, in which these illnesses collectively accounted for 30.6% (19/62) at the Olympic Trials and 52.9% (62/117) of the total EHIs at the Olympic Games. Temperature averaged 24.5°C for the 13 men's and women's long-distance running or walking events of the Olympic Trials and 22.7°C for the 1996 Olympics Games, correlating with the moderate- to high-risk categories on the ACSM Risk Index. The average Heat Stress Index value for all the track and field competitions during the Olympic Trials was 28.8°C, which correlates with the extreme-risk ACSM Risk Index category. Despite similar environmental conditions, the higher overall EHI rate seen in our study, as compared with these, may be associated with the size of the athletes or the protective equipment they wore.
The protective equipment worn by football players decreases the ability of the body to cool itself. 22 Kulka and Kenney 22 presented data from 8 recreational athletes with maximal oxygen consumption rates (V̇ o 2max) and body mass indexes similar to those of professional football players. The participants walked on a treadmill at a speed eliciting 35% of V̇ o 2max while temperature and humidity were systematically increased and core body temperature was recorded. The test was performed multiple times while the participants wore increasing amounts of protective clothing (shorts only, practice uniform, and a full football uniform). The participants were better able to maintain core body temperature when they were wearing less protective equipment. The consistent exercise protocol used by these investigators, however, may have influenced their findings. Fowkes Godek et al 23 reported that cross-country runners performing continuous exercise showed a steady increase in core temperature. Football athletes performing intermittent exercise associated with practices were able to dissipate some body heat during the rest periods.
The National Collegiate Athletic Association Injury Surveillance System compiled EHI data regarding injuries in football during the 2003–2004 sport season. 24 In its ongoing study, EHIs are defined as “time-loss” illnesses, thereby excluding all incidents not requiring the athlete to miss practice time. As a result, it does not seem likely that heat cramps would be included as a time-loss illness, and only heat exhaustion and heat stroke were reported. During the 2003–2004 season, illness rates of 0.18/1000 AEs and 0.01/1000 AEs for heat exhaustion and heat stroke, respectively, were reported. Although the illness rate for heat exhaustion is considerably lower than that seen in our data, it was based on 265 841 AEs as a representation of all US Division I football programs during the reporting year, whereas our data were based on 33 196 AEs. The total of 265 841 AEs represents 12.4% of the total AEs reported to the Association, which could reflect a potential underreporting by Division I institutions to the Injury Surveillance System during the same reporting period.
Although our study involved a significant number of AEs when compared with other injury databases, our cohort is still relatively small and localized to the southeastern United States. Future projects including greater numbers of AEs from other regions would be beneficial. Furthermore, previous authors 15, 21 did not consider heat cramps as part of their reported EHIs because they are often regarded as minor illnesses. The inclusion of heat cramps in our study dramatically increased the illness rate during the reporting period. In addition, the epidemiologic design of this project places certain constraints on data interpretation. Internal validity is reduced because we could not control for factors such as athlete conditioning, acclimatization status, hydration, food consumption, or rest. We also recognize that some athletes may have incurred more than 1 EHI during the study, but the rate of repeat occurrences was not recorded. The inability to control for some factors, however, reflects what commonly occurs in the clinical practice, making for high external validity.
We sought to track the rate of EHI and the associated WBGT at 5 Division I football programs located within the southeastern United States during the late summer and early autumn of 2003. The multisite epidemiologic nature of this research leads to certain limitations. Most importantly, we relied on the correct usage and interpretation of the EHI definitions we provided to the institutional medical staff. The primary data collector at each site was an athletic trainer; however, each EHI was not confirmed by a physician. In addition, we assumed that each athlete suffering from an EHI was able to identify it as such and report it to the medical staff on hand. Finally, our study design did not require the athletic trainer to measure core body temperature or serum sodium levels at the time of illness. Thus, cases of hyponatremia or exertional heat stroke may have occurred and not been recorded.
CONCLUSIONS
Based on the data collected, our results indicate that most reported EHIs occurred during the first 3 weeks of practice in August, with a dramatic decline in illness rates after this time. This finding coincides with the beginning of football practice and 2-a-day practices; it appears that once 2-a-day practices conclude, the rate of EHI goes down. The WBGT readings during practice sessions in August were consistently in the high-risk or extreme-risk category of the ACSM Risk Index for the entire month. No cases of hyponatremia or heat stroke were reported during the study. The majority of the reported EHIs were heat cramps, which are most often associated with a lack of acclimatization or conditioning. 25 Although we did not measure the acclimatization status of the football athletes in this study, this factor may have contributed to the high number of EHIs in the early weeks of the study.
To decrease the number of heat-related illnesses, the National Collegiate Athletic Association recently instituted a mandatory 5-day acclimatization period. Some research indicates, however, that a longer acclimatization period may be needed. Several authors 16, 26–28 have proposed that an athlete requires approximately 10 to 14 days to fully acclimatize to environmental conditions and that the specific WBGT may not play a significant role in the incidence rate of heat cramps. 16, 27–29 Increasing the mandatory acclimatization period in hot environments may reduce the incidence of EHIs.
Acknowledgments
We thank the certified athletic trainers from the 5 universities that participated in this project, which was funded by the National Athletic Trainers' Association College and University Athletic Trainers' Committee.
REFERENCES
- Armstrong LE. Classification, nomenclature, and incidence of the exertional heat illnesses. In: Exertional Heat Illnesses. Champaign, IL: Human Kinetics; 2003:17–28 .
- Moran DS. Potential applications of heat and cold stress indices to sporting events. Sports Med. 2001;31:909–917. doi: 10.2165/00007256-200131130-00002. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Extreme Heat. Atlanta, GA: Centers for Disease Control and Prevention; 2003.
- Department of Navy, Bureau of Medicine and Surgery. Preventive Medicine for Ground Forces: Section V. Prevention of Heat Injuries. Wet Bulb Globe Temperature (WBGT) Index. Manual of Naval Preventive Medicine. Available at: http://www.vnh.org/PreventiveMedicine/Chapter9/9.36.html. Accessed May 29, 2003 .
- Binkley HM, Beckett J, Casa DJ, Kleiner DM, Plummer PE. National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train. 2002;37:329–343. [PMC free article] [PubMed] [Google Scholar]
- Bar-Or O, Cantrill S, Kenney WL. Inter-Association Task Force on exertional heat illnesses consensus statement. NATA News. June 2003. pp. 24–29. et al.
- Casa DJ, Armstrong LE, Hillman SK. National Athletic Trainers' Association position statement: fluid replacement for athletes. J Athl Train. 2000;35:212–224. et al. [PMC free article] [PubMed] [Google Scholar]
- Committee on Sports Medicine and Fitness. Climatic heat stress and the exercising child and adolescent. American Academy of Pediatrics. Pediatrics. 2000;106:158–159. (1 pt 1) [PubMed] [Google Scholar]
- Hughson R. Canadian Association of Sports Sciences position paper on protection from exertional heat injuries. Can J Appl Sport Sci. 1981;6:99–100. [PubMed] [Google Scholar]
- American College of Sports Medicine. American College of Sports Medicine position stand on the prevention of thermal injuries during distance running. Med Sci Sports Exerc. 1987;19:529–533. [PubMed] [Google Scholar]
- Almquist J. Virginia High School League Heat Guidelines. Fairfax, VA: Fairfax County Public Schools; 2003.
- Armstrong LE, Epstein Y, Greenleaf JE. American College of Sports Medicine position stand: heat and cold illnesses during distance running. Med Sci Sports Exerc. 1996;28:i–x. et al. [PubMed] [Google Scholar]
- Yaglou CP, Minard D. Control of heat casualties at military training centers. Arch Indust Health. 1957;16:302–305. [PubMed] [Google Scholar]
- Frank A, Belokopytov M, Shapiro Y, Epstein Y. The cumulative heat strain index: a novel approach to assess the physiological strain induced by exercise-heat stress. Eur J Appl Physiol. 2001;84:527–532. doi: 10.1007/s004210000368. [DOI] [PubMed] [Google Scholar]
- Kark JA, Burr PQ, Wenger CB, Gastaldo E, Gardner JW. Exertional heat illness in Marine Corps recruit training. Aviat Space Environ Med. 1996;67:354–360. [PubMed] [Google Scholar]
- Maresh CM, VanHeest JL. Recommendations for athletes and weekend warriors. In: Armstrong LE, ed. Exertional Heat Illnesses. Champaign, IL: Human Kinetics; 2003:197–205 .
- The National Association for Sport and Physical Education. The Coaches' Code of Conduct: National Standards for Athletic Coaches. Reston, VA: American Alliance for Health, Physical Education, Recreation and Dance; 2001.
- Unruh N, Unruh S, Scantling E. Heat can kill: guidelines to prevent heat illness in athletic and physical education. J Phys Educ Rec Dance. 2002;73:36–38. [Google Scholar]
- American College of Sports Medicine. Position stand on: prevention of heat injury during distance running. Med Sci Sports Exerc. 1975;7:vii–ix. doi: 10.1249/00005768-198410000-00017. [DOI] [PubMed] [Google Scholar]
- Martin DE. Climatic heat stress and athletic performance. Track Coach. Spring 1997. pp. 4425–4452.
- Martin DE. Measurement of climatic heat stress at outdoor venues for endurance events at the Atlanta Olympic Games, 1996. Sports Med Train Rehabil. 1999;8:321–346. [Google Scholar]
- Kulka TJ, Kenney WL. Heat balance limits in football uniforms: how different uniform ensembles alter the equation. Physician Sportsmed. 2002;30(7):29–35. doi: 10.3810/psm.2002.07.377. [DOI] [PubMed] [Google Scholar]
- Godek S Fowkes, Godek JJ, Bartolozzi AR. Thermal responses in football and cross-country athletes during their respective practices in a hot environment. J Athl Train. 2004;39:235–240. [PMC free article] [PubMed] [Google Scholar]
- National Collegiate Athletic Association (NCAA). NCAA Football Injury Surveillance System for Academic Year 2003–2004, Division I. Available at: http://www.ncaa.org. Accessed February 6, 2005 .
- Armstrong LE, Casa DJ. Predisposing factors for exertional heat illnesses. In: Armstrong LE, ed. Exertional Heat Illnesses. Champaign, IL: Human Kinetics; 2003:151–167 .
- Gardner JW, Kark JA. Clinical diagnosis, management, and surveillance of exertional heat illness. In: Panolf KB, Burr RE, eds. Medical Aspects of Harsh Environments. Vol 1. Falls Church, VA: Office of the Surgeon General, United States Army Medical Department; 2003:231–279 .
- Sawka MN. Physical exercise in hot climates: physiology, performance, and biomedical issues. In: Wenger CB, Burr RE, eds. Medical Aspects of Harsh Environments. Vol 2. Falls Church, VA: Office of the Surgeon General, United States Army Medical Department; 2002:87–133 .
- Wenger CB. Human adaptation to hot environments. In: Pandolf KB, Burr RD, eds. Medical Aspects of Harsh Environments. Vol 1. Falls Church, VA: Office of the Surgeon General, United States Army Medical Department; 2003:51–86 .
- Casa DJ, Roberts WO. Considerations for the medical staff: preventing, identifying, and treating exertional heat illnesses. In: Armstrong LE, ed. Exertional Heat Illnesses. Champaign, IL: Human Kinetics; 2003:169–195 .