Abstract
Explanatory models for the increased prevalence of ill health in Gulf veterans compared to those not deployed to the Gulf War 1990–1991 remain elusive. This article addresses whether multi-symptom reporting in Gulf veterans are types of medically unexplained symptoms and whether the alleged Gulf War Syndrome is best understood as a medically unexplained syndrome. A review of the epidemiological studies, overwhelmingly cross-sectional, describing ill health was conducted including those that used factor analysis to search for underlying or latent clinical constructs. The overwhelming evidence was that symptoms in Gulf veterans were either in keeping with currently defined psychiatric disorders such as depression and anxiety or were medically unexplained. The application of factor analysis methods had varied widely with a risk of over interpretation in some studies and limiting the validity of their findings. We concluded that ill health in Gulf veterans and the alleged Gulf War Syndrome is best understood within the medically unexplained symptoms and syndromes constructs. The cause of increased reporting in Gulf veterans are still not clear and requires further inquiry into the interaction between sociological factors and symptomatic distress.
Keywords: medically unexplained symptoms, medically unexplained syndromes, Gulf War Syndrome, factor analysis, culture, psychiatric disorders
1. Introduction
Shortly after the Persian Gulf War of 1990–1991 it became apparent that a number of veterans were complaining about a wide range of symptoms. The most common symptoms reported were fatigue, headache, sleep disturbance, low mood and memory loss. Many veterans attributed these symptoms to their service in the Gulf and a number of physical exposures were considered as possible causes. It also led to the suggestion that there was a unique or new ‘Gulf War Syndrome’ that had arisen because of the conditions experienced by servicemen and women in the Gulf. However, so-called medically unexplained symptoms, such as fatigue, are also common in the general population and in servicemen who were not deployed to the Gulf War. We suggest that a complex interplay between social processes, culture, politics and neurobiology may help to explain why the controversy around Gulf War Syndrome exists.
2. Rationale for a medically unexplained multi-symptoms model in Gulf veterans
A number of voluntary registers and epidemiological studies (Barrett et al. 2003) and complex statistical methods, such as factor analysis, have failed to unearth a new medical disorder among veterans of the Gulf War (Shapiro et al. 2002). Studies on specific exposures experienced in the Gulf have not substantiated any of the theoretical speculations on the causes of ill health in Gulf veterans (Rook & Zumla 1997; Institute of Medicine 2000). There appears to be an increase in functional psychiatric disorders, such as depression, anxiety and post-traumatic stress disorder, which are themselves symptom-based constructs and do not sufficiently explain all the increased ill health reported by Gulf veterans (Ismail et al. 2002; Barrett et al. 2003; Stimpson et al. 2003) not least because it is well established that increased symptom reporting is associated with an increase in self-reported psychological distress.
Hospitalization rates for serious medical conditions were not increased in US Gulf veterans although there were increases in admission rates for injuries, asthma and diverse symptom diagnoses (Gray et al. 2000; Gray & Kang 2006). In both US and UK studies, mortality rates from all illnesses were lower among Gulf veterans compared to non-Gulf veterans except for a transient increase in mortality from external causes such as motor vehicle accidents (Kang et al. 2002a), consistent with patterns of post-war mortality observed in previous conflicts (Bullmore & Kang 1994). Abnormal outcomes relating to fertility, pregnancy and foetal abnormalities have been inconclusive due to the lack of objectively measured outcomes (Kang et al. 2001; Maconochie et al. 2004). Historical analysis suggests that similar patterns of medically unexplained symptomatic distress were present in previous conflicts (Hyams et al. 1997; Jones et al. 2002; Jones & Wessely 2004a,b). In the absence of any firm evidence, one possible conclusion is that increased symptom reporting in Gulf veterans may be best thought of as medically unexplained symptoms.
3. Medically unexplained symptoms in civilian populations
Medically unexplained symptoms refer to symptoms that are disproportionate to identifiable physical disease and are also sometimes described as functional, in the sense that they are associated with disorders of function in the presence of normal anatomical structure. Nearly one-third of physical symptoms presenting in primary care are either psychiatric or medically unexplained (Kroenke & Price 1993). Chronic fatigue syndrome (CFS) affects around 5–10% of the population and is one of the most commonly reported symptoms in primary care (Kroenke et al. 1988; David et al. 1990; Pawlikowska et al. 1994; Wessely et al. 1997). Other common symptoms in the general population are pain, headache and sleep disturbance (Kroenke et al. 1994; Simon et al. 1996; Gureje et al. 1998). Medically unexplained symptoms are strongly associated with psychiatric morbidity in both cross-sectional (Kroenke et al. 1994; Spitzer et al. 1995; Wessely et al. 1997) and in longitudinal studies (Skapinakis et al. 2004). In the past, there has been a tendency for the medical profession to be somewhat dismissive of medically unexplained symptoms, but they are important and disabling for patients and associated with a poor quality of life (Kroenke et al. 1994; Spitzer et al. 1995; Wessely et al. 1997).
When individuals report several symptoms together in the absence of clinical or epidemiological evidence for a physical cause, they are often termed a medically unexplained syndrome and there are a variety of labels given to these syndromes by the media, pressure groups or the medical community. Most medical specialities have a diagnosis that is used to describe people with a number of symptoms (Wegman et al. 1997).
The three most common medically unexplained syndromes in Western civilian populations are irritable bowel syndrome (IBS), CFS and fibromyalgia. There are a variety of definitions for these syndromes. In IBS, there are symptoms of intermittent abdominal pains, bloating and changes in bowel habit. The prevalence of IBS varies from 5 to 65% depending on the case definition used (Kay et al. 1994). CFS is characterized by disabling fatigue together with muscular pains, joint pains, subjective memory impairment, sore throats, headaches and unrefreshing sleep (Fukuda et al. 1994). The rates for CFS are around 0.5% in primary care but increase with less specific definitions (Wessely et al. 1997; Jason et al. 1999, 2003). Fibromyalgia is defined as a disabling widespread pain and specific tender musculoskeletal points, and it is often associated with fatigue, sleep disturbance and psychological distress. The population prevalence of fibromyalgia is estimated to range from 1 to 4% (Wolfe et al. 1995). Other syndromes that have been described are multiple chemical sensitivity (MCS), sick building syndromes and dental amalgam syndrome. Considerable overlap exists among the symptoms of different syndromes, especially CFS, fibromyalgia and MCS. Syndromes are often defined by the speciality the symptoms present in. Several leading researchers have suggested that these syndromes may well represent different points on a continuum of symptomatic distress or even different manifestations of the same condition (Buchwald & Garrity 1994; Barsky & Borus 1999; Aaron et al. 2000; Black et al. 2000; Nimnuan et al. 2001). There is also evidence from UK general practice that fatigue diagnoses have fallen since 1990 while fibromyalgia diagnoses have risen (Gallagher et al. 2004).
4. Medically unexplained symptoms in Gulf veterans
There is a large body of evidence that the excess ill health reported by Gulf veterans comprises multi-system and non-specific symptoms not dissimilar to the spectrum of medically unexplained symptoms and syndromes in civilian populations. The term ‘Gulf War Syndrome’ was coined in 1992 following the report of an alleged outbreak of a mystery illness in 79 US Gulf veterans for which no unifying diagnosis could be found (DeFraites et al. 1992). Is there sufficient evidence to support the notion that Gulf War Syndrome is another multi-symptom condition similar to chronic fatigue and fibromyalgia?
Many Gulf veterans believe they have CFS; between 6 and 17% of UK Gulf veterans believed they were suffering from Gulf War Syndrome (Chalder et al. 2001; Simmons et al. 2004). The most common symptoms are related to mood and cognitive functioning. There are over 20 controlled population-based studies that have compared the prevalence of multi-symptoms conditions in both Gulf veterans and non-Gulf veterans.
(a) Individual symptoms
Almost all controlled research studies in which the comparison group has been service personnel who were on active duty at the time of the Gulf War 1990–1991 but not deployed to the Gulf theatre have reported a two- to fourfold increase in individual symptoms in Gulf veterans compared to non-Gulf veterans, regardless of nationality, branch of service and trade, method of measurement (postal versus interview) or duration of symptoms (Barrett et al. 2003). The most common symptoms are headaches, fatigue, sleep disturbance, joint pains and stiffness, mood changes, concentration and memory difficulties. It is important to note that non-Gulf veterans also appear to suffer from the same symptomatic distress but that Gulf veterans report more of the same symptoms. In the Health Survey of UK Military Personnel, which was a cross-sectional postal survey conducted from 1997 to 1998, the rates of almost every symptom was reported 2–3 times more frequently in Gulf veterans compared to Bosnia and Era veterans, respectively (see figure 1; Unwin et al. 1999). The most recent published study is a postal cross-sectional survey to all UK Gulf veterans (n=52 811) and a randomly selected comparison group (n=52 924) (Simmons et al. 2004). This study used free text method of measuring new symptoms to overcome potential reporting biases to standardized symptom scales or categories in previous studies. Of the 42 818 servicemen who responded, 61% of Gulf veterans reported at least one new medical symptom since 1990, compared with 37% of non-Gulf War veterans, with the strongest association for mood swings, memory loss/lack of concentration, night sweats, general fatigue and sexual dysfunction.
Figure 1.
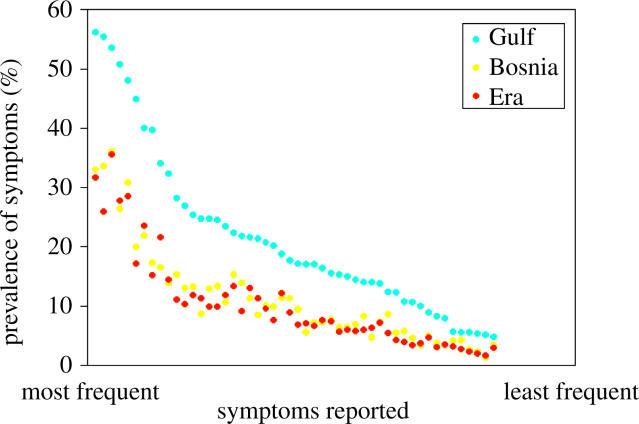
Distribution of 50 symptoms in the Health Survey of UK Military Personnel (Unwin et al. 1999).
Of course, these large-scale surveys did not carry out a medical examination and so it is possible that some of the self-reported symptoms were a reflection of an explainable medical syndrome. However, other studies have demonstrated that the vast majority of these common symptoms are not explainable in the usual medical sense. There are also data from case series of those veterans who have approached the US and UK medical service for veterans (Joseph & the Comprehensive Clinical Evaluation Program Evaluation Team 1997; Kroenke et al. 1998; Roy et al. 1998; Coker et al. 1999; Lee et al. 2001). In these studies, veterans have been medically examined and it has supported the view that the symptoms commonly reported do not have any currently accepted medical explanation.
Epidemiological methods are usually restricted to measuring one or a few risk factors and outcomes and they are not designed to detect underlying patterns, where multiple health indices are being reported and measured as in Gulf veterans. Complex statistical methods, such as factor analysis, have therefore been used to search for latent variables that may then represent the underlying dimensions for the reported symptoms. Factor analysis is mostly used by psychologists to estimate latent variables for psychological characteristics such as intelligence quotient scores and psychometric properties of measurement scales. It relies upon the correlation between several variables and calculates underlying dimensions or factors based upon these correlations. When data are approached using factor analysis, and without a priori theory, there is often controversy surrounding the labelling of the factors. This is a subjective element and so critical appraisal of factor analysis studies requires a careful look at the factor labels provided by the investigators.
The first factor analysis study was carried out by Haley and colleagues who conducted an exploratory factor analysis of 52 symptoms that they measured on 249 Gulf veterans selected from one US Reserve Unit. They reported that six factors accounted for 71% of the variance of the observed variables. The factors were defined as ‘impaired cognition’, ‘confusion–ataxia’, ‘arthro–myo-neuropathy’, ‘phobia–apraxia’, ‘fever–adenopathy’ and ‘weakness–incontinence’. They interpreted their findings as evidence for a discrete cluster of symptoms among Gulf veterans and that this reflected neurological injury. The difficulty with their conclusions was that they chose labels that suggested specific clinical entities and neurological damage. For example, ‘ataxia’, ‘neuropathy’ and ‘apraxia’ would conventionally only be given after a clinical examination. They also did not compare their findings with a non-Gulf control group, which limits any interpretation that this was a new Gulf War Syndrome as it was possible that the same dimensions would have emerged from a similar methodology applied to other veterans not deployed to the Gulf. The impact of Haley and colleagues' publication in a leading medical journal was that it convinced many of those unfamiliar with factor analysis techniques (an overwhelming majority of the military, medical and civilian population) that this provided evidence for a new disorder though this was a step beyond the evidence they provided.
Several research teams have attempted to replicate Haley's findings and further investigate this possibility. Despite variations in the epidemiological and statistical methods used, every study has detected a latent variable which represents symptoms of mood, cognitive functioning and/or fatigue (Shapiro et al. 2002).
In addition, all but one study of factor analysis, which compares factors in Gulf and non-Gulf veterans, has been unable to identify an underlying pattern of symptom reporting that is unique to Gulf veterans (Fukuda et al. 1998; Ismail et al. 1999; Doebbeling et al. 2000; Knoke et al. 2000; Shapiro et al. 2002). The exception is Kang et al. (2002) who reported that that their second largest factor in Gulf veterans, which they labelled neurological, did not have a parallel factor in the non-Gulf group. They concluded that this may suggest a possible syndrome related to Gulf War deployment.
There are several methods of comparing whether the factors underlying the symptoms measured in Gulf veterans are different from the derived factors in non-Gulf veterans. Most studies reported in table 1 format the factors, the symptoms that load onto them and the size of that factor loading derived from exploratory factor analysis separated by deployment status (Fukuda et al. 1998; Ismail et al. 1999; Doebbeling et al. 2000; Knoke et al. 2000; Shapiro et al. 2002). The limitation of this method is that it does not provide a statistical test of significance. A more valid method is to use confirmatory factor analysis, which is a statistical technique which specifies a factor structure model (identified using exploratory factor analysis) in a sample of Gulf veterans and carries out tests of significance such as goodness-of-fit to test whether the model can be predicted or replicated in non-Gulf veterans. Only one study to date has used confirmatory factor analysis in this way and found that the underlying factor structure of symptoms measured in Gulf veterans fitted reasonably well in the non-Gulf veterans as well.
Table 1.
Summary of studies that have used factor analysis in Gulf veterans.
| study | Haley et al. (1997) | Fukuda et al. (1998) | Ismail et al. (1999) | Bourdette et al. (2001) | Doebbeling et al. (2000) | Knoke et al. (2000) | Shapiro et al. (2002) | Kang et al. (2002b) |
|---|---|---|---|---|---|---|---|---|
| study population | US Seabees (active and ex-service) | US Air Force (active) | UK Military (active and ex-service) | US Military from Oregon or Washington (active and ex-service) | US Military from Iowa (active and ex-service) | US Seabees (active) | US Army/National Guard (active) | US Military (active and ex-service) |
| sample size of Gulf veterans | 249 | 1631a | 3214 | 227 | 3695 | 1459 | 1779 | 10 423 |
| no. of symptoms measured | 52 | 35 | 50 | 35 | 137 | 98 | 19 | 47 |
| percentage of common variance explained by factors reported | 71 | 39.1 | 42.1 | 34.2 | 35 | 80 | 46.7 | 44 |
| labels given to factors by authors | impaired cognition | fatigue | mood–cognition | cognitive/psychological | somatic distress | insecurity | cognitive/psychological | fatigue/ depression |
| confusion–ataxia | mood–cognition | respiratory system | mixed somatic | psychological distress | somatization | dysesthesiab | neurological | |
| arthro–myo-neuropathy | musculoskeletal | peripheral nervous system | musculoskeletal | panic | depression | vestibular dysfunction | musculoskeletal | |
| phobia–apraxia | obsessive–compulsive | gastrointestinal | ||||||
| fever–adenopathy | malaise | pulmonary | ||||||
| weakness–incontinence | upper respiratory |
Included non-Gulf veterans.
In Khamisiyah Gulf veterans only.
There are many other limitations to factor analysis which have been well described by Shapiro et al. (2002). Results from factor analysis are only as valid as the data input, so biases and confounders during the collection of the data will lead to biases in the results. The variations in the results may be related to differences in methodology, such as design, study population, symptoms measured and sample size. There are few rules governing the choice of statistical methods, such as the type of factor analysis, criteria for factor extraction, rotation method, cut-offs of factor loadings for symptom retention and this will lead to differences in results. The differences may be less important than the similarities and labels given to factors may be less informative than a closer look at the symptoms that are included in the factors. For instance, even Haley and colleagues' first factor of impaired cognition had symptoms of mood but they chose to interpret this as evidence of neurological injury.
In a cluster analysis of observed symptoms, no significant differences were found in the symptoms groupings between Gulf, Bosnia and non-deployed Era servicemen (Everitt et al. 2002). Factor analysis of symptoms presenting in primary care has found dimensions of symptoms relating to mood, cognition, fatigue and musculoskeletal symptomatology (Simon et al. 1996). The comorbidity of mood disorders and self-reported physical symptoms is well known and universally reported (Kroenke & Price 1993). Symptomatic distress is a common and universal phenomenon regardless of exposure to conflict or military/civilian status. Nevertheless, Gulf War veterans do report more symptomatic distress than veterans who were not deployed to the Gulf.
(b) Chronic fatigue and chronic fatigue syndrome
The Iowa Persian Gulf study was the first to report a population-based cross-sectional survey of health status in a large sample of Gulf and non-Gulf veterans resident in Iowa (The Iowa Persian Gulf Study Group 1997). Using a self-report telephone survey of 3696 respondents, there was a threefold increase in the prevalence of symptoms of chronic fatigue in regular Gulf veterans (1.0%) compared to non-Gulf veterans (0.2%) and in reservists compared to regular personnel (2.9 versus 1.1%). Goss Gilroy Inc. (1998) carried out a self-report postal survey of all Canadian Gulf veterans and a sample of non-Gulf veterans (n=6552 respondents) and reported a fivefold increase in CFS in Gulf veterans. The Health Survey of UK Military Personnel was unique in comparing Gulf veterans with two control groups, those deployed to Bosnia 1992–1997 (in order to control for the stress of deployments) and those not deployed to either (Era veterans). They reported a two- to threefold increase in fatigue in Gulf servicemen (2.1%) compared to both Bosnia (0.7%) and Era (1.8%) servicemen (Unwin et al. 1999; Reid et al. 2001). Even higher increase prevalence in fatigue was reported in UK Gulf servicewomen (Unwin et al. 2002). Steele et al. conducted a population-based telephone survey and reported an 11-fold increase in rates of CFS derived from self-report symptom measures in 1548 Gulf veterans (7.1%) and 482 non-Gulf veterans (0.7%) resident in Kansas (Steele 2000). Gray et al. (2002) conducted a nationwide postal survey of 18 945 Seabees construction workers on active duty during the Gulf War 1990–1991; Gulf Seabees veterans (5.2%) were nearly seven times more likely to self-report physician-diagnosed CFS than non-Gulf Seabees (0.7%).
Recently, Kang and colleagues estimated in their US nationwide sample of 30 000 military personnel the rates of CFS using a self-administered questionnaire on the eight symptoms for diagnosing CFS based on the Centers of Disease Control and Prevention's 1994 definition (Fukuda et al. 1994), as well as questions about onset and severity (Kang et al. 2003). They found that the prevalence of a CFS-like illness in Gulf veterans was 5.6% compared to 1.2% in non-Gulf veterans. They also found that there was a linear dose–response association between CFS and combat but only at mild to moderate levels of stress. Kelsall et al.'s (2004) study of the entire cohort of 1871 Australians who served in the Gulf War 1990–1991 found that the symptom of fatigue was 1.6 more likely to be reported than in a random sample of 2924 non-Gulf veterans.
There have been fewer case–comparison studies that have conducted objective medical assessment or clinical interviews to validate the self-reported medically unexplained syndromes. In the Danish study, clinical examination of peacekeeping Gulf veterans (n=686) revealed increased rates of medically unexplained symptoms compared to age- and gender-matched controls (n=231) (Ishoy et al. 1999). In a population-based sample of active duty Seabees who had (n=527) and had not been (n=970) deployed to the Gulf War 1990–1991, no respondent met the symptom criteria for CFS. A clinical examination and a range of non-specific markers of chronic disease were used to exclude significant physical causes of symptomatic distress. Gulf veterans had slightly lower hand grip strength and ferritin levels, but the values were well within the normal range (Gray et al. 1999). One of the limitations of this study is a potential healthy worker bias in that active duty personnel are more likely to be healthy and less likely to be suffering from conditions such as CFS, which require substantial functional impairment as one of its criteria. The rates of CFS were not significantly greater in the random sub-sample of Gulf veterans from the Devens cohort (n=180) compared to a group who had been deployed to Germany (n=46) (Proctor et al. 2001), but this was small study. A recent study examined the health status of a population-based random sample of US Gulf (n=1966) and non-Gulf veterans (n=2883) 10 years after the Gulf War 1990–1991. Standardized clinical evaluations were conducted to assess 12 medical conditions in Veterans Affairs (VA) medical centres across the US. The authors found that physical health was similar in the Gulf (n=1061) and non-Gulf deployed (n=1128) veterans but Gulf veterans had a higher prevalence of CFS (1.6 versus 0.1%), skin conditions (34.6 versus 26.8%) and dyspepsia (9.1 versus 6.0%) (Eisen et al. 2005).
In summary, the overwhelming conclusion from the self-reported studies suggest that Gulf veterans are reporting CFS and related symptoms at least 2–3 times more frequently than non-Gulf veterans.
(c) Fibromyalgia
There have been fewer studies examining the relative rates of fibromyalgia in Gulf War veterans compared to those not deployed to the Gulf. In the Iowa Persian Gulf study, Gulf veterans reported a significantly higher prevalence of symptoms of fibromyalgia (19.2 versus 9.6%; The Iowa Persian Gulf Study Group 1997). In other US military population, fibromyalgia was reported 3.7 times more frequently in Kansas Gulf veterans compared to non-Gulf veterans (Steele 2000). A similar relative increase in fibromyalgia in Gulf veterans has also been reported in Canadian Gulf veterans (Goss Gilroy Inc. 1998). In the recent VA study, the prevalence of fibromyalgia after clinical evaluation was 2% Gulf veterans compared to 1.2% in non-Gulf veterans (Eisen et al. 2005).
(d) Other medically unexplained syndromes
Some Gulf veterans have suggested that their symptoms are in keeping with MCS because they were exposed to, inter alia, oil, gas fumes and pesticides. MCS is characterized by the reporting of a wide variety of symptoms, in the absence of accompanying physical signs or biomedical test abnormalities, attributed by its proponents to chemical exposure or increased sensitivity. Fukuda et al. (1998) found a significant 2.5 increased rate of symptoms of chemical sensitivity lasting more than six months in Gulf veterans currently in active service Air Force veterans compared to non-Gulf deployed. Reid et al. (2001) in the UK Health Survey of Military Personnel found a self-reported prevalence of MCS of 1.3% in Gulf veterans compared to 0.3 and 0.2% in Bosnia and Era veterans, respectively. In a similar secondary analysis of the Iowa Persian Gulf study, Black et al. (2000) found that Gulf veterans reported a significantly higher prevalence of MCS symptoms than non-Gulf veterans (5.4 versus 2.6%). Gulf War Seabees reported a fourfold increase in self-report of MCS compared to Seabees deployed elsewhere (Gray et al. 2002). To date, only the Seabees population-based study has studied IBS, although all the controlled studies have measured gastrointestinal symptoms and found them to be increased in Gulf veterans. In the Seabees study, Gulf veterans were 3.5 times more likely to report IBS than in non-Gulf veterans (Gray et al. 2002).
5. An explanatory model for Gulf War Syndrome or Gulf related ill health?
The overwhelming evidence suggests that ill health in Gulf veterans has many properties in common with medically unexplained syndromes in civilian populations. Based on current evidence, it is likely that the alleged Gulf War Syndrome is a concept that overlaps with constructs such as CFS and fibromyalgia. Medically unexplained syndromes do not fit neatly into any classification scheme or medical aetiological model, but it is likely that their genesis is influenced by a complex interplay of neurobiological, social, cultural and political forces (Jones & Wessely 2004a,b).
Medically unexplained symptoms are by their definition currently unexplained by current medical and neurobiological models. They are often diagnoses of exclusion, in which an absence of positive physical signs and diagnostic tests indicates that the symptoms are unexplained. Of course, we hope that medical knowledge and understanding will continue to grow. It is possible that psychological, hormonal and other influences can lead to physical symptoms through a variety of neurobiological influences that are as yet not described.
How can medically unexplainable symptomatic distress acquire a label with presumed diagnosis such as the term Gulf War Syndrome? Wegman et al. (1997) in their landmark theoretical paper described how a syndrome acquires a status. They defined five processes that individually or in varying combination can lead to the identification of a new syndrome:
The clinical features have to be sufficiently distinct from recognized conditions.
The limits of the case definition have to be within a certain range to exclude common aetiologies and to avoid being too narrow.
The condition has be observed and replicated by other researchers.
Adequate demonstration of a unique cause and effect association could be sufficient that the effect should be recognized.
Socio-cultural, economic and political pressures to accept or reject a condition may be operating.
In the case of ill health in Gulf veterans, this review and other chapters show that none of the first four criteria for identifying a new syndrome have been met. However, the role of social, economic and political forces may have played an important role in the genesis of a new disorder.
Every society has explanatory models of illness (Kleinman 1988), which are notions that help to explain episode of sickness and its treatment and employed by the patient, the public and the medical profession. Lay or non-professional explanatory models tend to be more idiosyncratic, changeable and heavily influenced by cultural and personal factors. The growth of alternative medicines has legitimized the idea that ‘Western’ medicine has a limited range of expertise and a narrow view in regard to unconventional or new treatments not produced by large pharmaceutical companies. Sufferers with symptomatic distress, in the face of no convincing medical explanation, tend to conduct their own ‘search for meaning’ and can attribute their illness to a variety of possible and plausible causes including viruses, immune system dysfunction, diet, chemicals or even buildings (Wessely et al. 1999).
Medically unexplained syndromes have overlapping symptoms, but the label and attributed cause(s) can be very different (Stewart 1990). Some of the CFS voluntary organizations believe that CFS is caused by an infection from an unknown agent that will one day be discovered. For Gulf veterans, the possibility that depleted uranium, oil smoke, pesticides, vaccinations, chemical weapons and biological weapons might lead to illness have been suggested as possible causes. The fear is worsened by the nature of modern warfare where chemical and biological weapons constitute psychological warfare as much as physical assaults (Holloway et al. 1997).
Most individuals respond to symptoms they experience as distressing by asking members of their own social network, usually before seeking advice from the medical profession, but they are also often looking to the media and internet. Gulf veterans in distress may turn to fellow Gulf veterans and to veterans and patient groups, charities, internet literature and chat rooms in addition to multiple second medical opinions that on occasions may reinforce explanations without widespread medical acceptance. Those who were most likely to report ill health were from the lower ranks (Ismail et al. 2000). Almost all illnesses are more common in the less privileged in society but the military tradition of secrecy and authoritarianism may have led to the development of blame and conspiracy theories, particularly in those with less status within that system.
The Centers for Disease Control, one of the most influential health organizations in the world, described the first cases of ill health in Gulf veterans as an ‘outbreak of unexplained illness’. Some early publications (Haley & Kurt 1997) since criticized on methodological grounds were published in influential journals and promoted the case for a new syndrome. Subsequent debate within the medical community has continued to lead to confusion in Gulf veterans and can reinforce suspicion of the ‘establishment’ opinion. Even though most medical opinion has not supported most of the biological explanations for Gulf War Syndrome, the communication of medical opinions has often led the public to believe that there is much more controversy amongst medical experts. The media plays a crucial role in disseminating information. Topics that are controversial or political, such as Gulf War Syndrome, are more likely to be newsworthy and the media tends to present simplified and polarized points of view, justified by their desire to remain impartial. News, in its widest meaning of information and opinion dissemination, can in the minds of sufferers legitimize their symptoms and become part of an individual's repertoire of beliefs (Wessely et al. 1998).
6. Conclusion
There is now a growing consensus that veterans of the Gulf War 1990–1991 are experiencing many more multi-symptom conditions than comparable servicemen and women who were not deployed to the Gulf theatre. There is no convincing evidence for a new Gulf War Syndrome and it appears that similar syndromes have occurred after previous conflicts. However, there is still no satisfactory explanation for the increased rate of multi-symptom conditions in Gulf War veterans. The syndromes seen in Gulf War veterans are probably best considered as similar to the medically unexplained syndromes found in civilian populations.
Why has the Gulf War 1990–1991 led to this controversy? It is possible the change was more in the response of the veterans to these symptoms rather than in the presence of the symptoms themselves. There has been a tendency for the medical profession to be rather dismissive of medically unexplained symptoms. Perhaps veterans of previous wars have tended to accept their doctors' reassurance more readily than our current generation. Medically unexplained symptoms are important, distressing and disabling—even if the medical profession has no satisfactory explanation for them. The veterans have made it clear that dismissing or discounting these medically unexplained symptoms is no longer an option for the medical profession.
Footnotes
One contribution of 17 to a Theme Issue ‘The health of Gulf War veterans’.
References
- Aaron L, Burke M, Buchwald D. Overlapping conditions among patients with chronic fatigue syndrome, fibromyalgia and temperomandibular disorder. Arch. Intern. Med. 2000;160:221–227. doi: 10.1001/archinte.160.2.221. doi:10.1001/archinte.160.2.221 [DOI] [PubMed] [Google Scholar]
- Barrett D, Gray G, Doebbeling B, Clauw D, Reeves W. Prevalence of symptoms and symptom-based conditions among Gulf War veterans: current status of research findings. Epidemiol. Rev. 2003;24:218–227. doi: 10.1093/epirev/mxf003. doi:10.1093/epirev/mxf003 [DOI] [PubMed] [Google Scholar]
- Barsky A, Borus J. Functional somatic syndromes. Ann. Intern. Med. 1999;130:910–921. doi: 10.7326/0003-4819-130-11-199906010-00016. [DOI] [PubMed] [Google Scholar]
- Black D.W, Doebbeling B.N, Voelker M.D, Clarke W.R, Woolson R.F, Barrett D.H, Schwartz D.A. Multiple chemical sensitivity syndrome: symptom prevalence and risk factors in a military population. Arch. Intern. Med. 2000;160:1169–1176. doi: 10.1001/archinte.160.8.1169. doi:10.1001/archinte.160.8.1169 [DOI] [PubMed] [Google Scholar]
- Bourdette D.N, McCauley L.A, Barkhuizen A, Johnston W, Wynn M, Joos S.K, Storzbach D, Shuell T, Sticker D. Symptom factor analysis, clinical findings, and functional status in a population-based case control study of Gulf War unexplained illness. J. Occup. Environ. Med. 2001;43:1026–1040. doi: 10.1097/00043764-200112000-00005. [DOI] [PubMed] [Google Scholar]
- Buchwald D, Garrity D. Comparison of patients with chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivities. Arch. Intern. Med. 1994;154:2049–2053. doi:10.1001/archinte.154.18.2049 [PubMed] [Google Scholar]
- Bullmore T, Kang H. Posttraumatic stress disorder and the risk of traumatic deaths among Vietnam veterans. J. Nerv. Ment. Disord. 1994;182:604–610. doi: 10.1097/00005053-199411000-00002. [DOI] [PubMed] [Google Scholar]
- Chalder T, Hotopf M, Unwin C, Hull L, Ismail K, David A, Wessely S. Prevalence of Gulf war veterans who believe they have Gulf war syndrome: questionnaire study. Br. Med. J. 2001;323:473–476. doi: 10.1136/bmj.323.7311.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker W, Bhatt B, Blatchley N, Graham J. Clinical findings for the first 1000 Gulf War veterans in the Ministry of Defence's medical assessment programme. Br. Med. J. 1999;318:290–294. doi: 10.1136/bmj.318.7179.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David A, Pelosi A, McDonald E, Stephens D, Ledger D, Rathbone R, Mann A. Tired, weak, or in need of rest: fatigue among general practice attenders. Br. Med. J. 1990;301:1199–1202. doi: 10.1136/bmj.301.6762.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeFraites R, Wanat E, Norwood A, Williams S, Cowan D, Callahan T. Epidemiology Consultant Service, Division of Preventative Medicine, Walter Reed Army Institute of Research; Washington, DC: 1992. Investigation of a suspected outbreak of an unknown disease among veterans of operation Desert Storm/Shield. 123rd Army Reserve Command, Fort Benjamin Harrison, Indiana. [Google Scholar]
- Doebbeling B.N, Clarke W.R, Watson D, Torner J.C, Woolson R.F, Voelker M.D, Barrett D.H, Schwartz D.A. Is there a Persian Gulf War Syndrome? Evidence from a large population-based survey of veterans and nondeployed controls. Am. J. Med. 2000;108:695–704. doi: 10.1016/s0002-9343(00)00405-8. doi:10.1016/S0002-9343(00)00405-8 [DOI] [PubMed] [Google Scholar]
- Eisen S, et al. Gulf war veterans' health: medical evaluation of a US Cohort. Ann. Intern. Med. 2005;142:881–890. doi: 10.7326/0003-4819-142-11-200506070-00005. [DOI] [PubMed] [Google Scholar]
- Everitt B, Ismail K, David A, Wessely S. Searching for a Gulf War Syndrome using cluster analysis. Psychol. Med. 2002;32:1371–1378. doi: 10.1017/s0033291702006311. doi:10.1017/S0033291702006311 [DOI] [PubMed] [Google Scholar]
- Fukuda K, Straus S.E, Hickie I, Sharpe M.C, Dobbins J.G, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann. Intern. Med. 1994;121:953–959. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- Fukuda K, et al. Chronic multi-symptom illness affecting Air Force veterans of the Gulf War. J. Am. Med. Assoc. 1998;280:981–988. doi: 10.1001/jama.280.11.981. doi:10.1001/jama.280.11.981 [DOI] [PubMed] [Google Scholar]
- Gallagher A, Thomas J, Hamilton W, White P. Incidence of fatigue symptoms and diagnoses presenting in UK primary care from 1990 to 2001. J. R. Soc. Med. 2004;97:571–575. doi: 10.1258/jrsm.97.12.571. doi:10.1258/jrsm.97.12.571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goss Gilory Inc. Health study of Canadian Forces personnel involved in the 1991 conflict in the Persian Gulf. Goss Gilory Inc; Ottawa, Ontario: 1998. [Google Scholar]
- Gray G.C, Kang H.K. Health utilization and mortality among veterans of the Gulf War. Phil. Trans. R. Soc. B. 2006;361:553–569. doi: 10.1098/rstb.2006.1816. doi:10.1098/rstb.2006.1816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray G, Kaiser K, Hawksworth A, Hall F, Barrett-Connor E. Increased postwar symptoms and psychological morbidity among US Navy Gulf War veterans. Am. J. Trop. Med. Hyg. 1999;60:758–766. doi: 10.4269/ajtmh.1999.60.758. [DOI] [PubMed] [Google Scholar]
- Gray G, Smith T, Kang H, Knoke J. Are Gulf veterans suffering from war-related illnesses? Federal and civilian hospitalizations examined, June 1991 to December 1994. Am. J. Epidemiol. 2000;151:63–67. doi: 10.1093/oxfordjournals.aje.a010123. [DOI] [PubMed] [Google Scholar]
- Gray G, Reed R, Kaiser K, Smith T, Gastanaga V. Self reported symptoms and medical conditions among 11,868 Gulf War-Era veterans. The Seabee Health Study. Am. J. Epidemiol. 2002;155:1033–1044. doi: 10.1093/aje/155.11.1033. doi:10.1093/aje/155.11.1033 [DOI] [PubMed] [Google Scholar]
- Gureje O, Von Korff M, Simon G.E, Gater R. Persistent pain and well being: a World Health Organization study in primary care. J. Am. Med. Assoc. 1998;280:147–151. doi: 10.1001/jama.280.2.147. doi:10.1001/jama.280.2.147 [DOI] [PubMed] [Google Scholar]
- Haley R, Kurt T. Self-reported exposure to neurotoxic chemical combinations in the Gulf war. A cross sectional epidemiologic study. J. Am. Med. Assoc. 1997;277:231–237. doi:10.1001/jama.277.3.231 [PubMed] [Google Scholar]
- Holloway H, Norwood A, Fullerton C, Engel C, Ursano R. The threat of biological weapons: prophylaxis and mitigation of psychological and social consequences. J. Am. Med. Assoc. 1997;278:425–427. doi:10.1001/jama.278.5.425 [PubMed] [Google Scholar]
- Hyams K, Wignall S, Roswell R. War syndromes and their evaluation: from the US civil war to the Persian Gulf War. Ann. Intern. Med. 1997;125:398–405. doi: 10.7326/0003-4819-125-5-199609010-00007. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . Gulf War and health: vol. 1. Depleted uranium, pyridostigmine bromide, sarin, and vaccines. National Academy Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- Ishoy T, Suadicani P, Guldager B, Appleyard M, Hein H, Gyntelberg F. State of health after deployment in the Persian Gulf. Dan. Med. Bull. 1999;46:416–427. [PubMed] [Google Scholar]
- Ismail K, Everitt B, Blatchley N, Hull L, Unwin C, David A, Wessely D. Is there a Gulf War Syndrome? Lancet. 1999;353:179–182. doi: 10.1016/S0140-6736(98)11339-9. doi:10.1016/S0140-6736(98)11339-9 [DOI] [PubMed] [Google Scholar]
- Ismail K, Blatchley N, Hotopf M, Hull L, Palmer I, Unwin C, David A, Wessely S. Occupational risk factors for ill health in UK Gulf veterans. J. Epidemiol. Community Health. 2000;54:834–838. doi: 10.1136/jech.54.11.834. doi:10.1136/jech.54.11.834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ismail K, et al. The mental health of UK Gulf War veterans: phase 2 of a two-phase cohort study. Br. Med. J. 2002;325:576–579. doi: 10.1136/bmj.325.7364.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason L.A, Richman J.A, Rademaker A.W, Jordan K.M, Plioplys A.V, Taylor R.R, McCready W, Huang C.F, Plioplys S. A community based study of chronic fatigue syndrome. Arch. Intern. Med. 1999;159:2129–2137. doi: 10.1001/archinte.159.18.2129. doi:10.1001/archinte.159.18.2129 [DOI] [PubMed] [Google Scholar]
- Jason L, Helgerson J, Torres-Harding S, Carrico A, Taylor R. Variability in diagnostic criteria for chronic fatigue syndrome may result in substantial differences in patterns of symptoms and disability. Eval. Health Prof. 2003;26:3–22. doi: 10.1177/0163278702250071. doi:10.1177/0163278702250071 [DOI] [PubMed] [Google Scholar]
- Jones E, Wessely S. Hearts, guts and minds: somatisation in the military from 1900. J. Psychosom. Res. 2004a;56:425–429. doi: 10.1016/S0022-3999(03)00626-3. doi:10.1016/S0022-3999(03)00626-3 [DOI] [PubMed] [Google Scholar]
- Jones E, Wessely S. War syndromes: the impact of culture on medically unexplained syndromes. Med. Hist. 2004b;49:55–78. doi: 10.1017/s0025727300008280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones E, Hodgins-Vermaas R, McCartney H, Everitt B, Beech C, Poynter D, Palmer I, Hyams K, Wessely S. Post-combat syndromes from the Boer War to the Gulf War: a cluster analysis of their nature and attribution. Br. Med. J. 2002;324:1–7. doi: 10.1136/bmj.324.7333.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph S, the Comprehensive Clinical Evaluation Program Evaluation Team A comprehensive clinical evaluation of 20 000 Persian Gulf War veterans. Mil. Med. 1997;162:149–155. [PubMed] [Google Scholar]
- Kang H, Magee C, Mahan C, Lee K, Murphy F, Jackson L, Matanoski G. Pregnancy outcomes among US Gulf War veterans: a population based survey of 30,000 veterans. Ann. Epidemiol. 2001;11:504–511. doi: 10.1016/s1047-2797(01)00245-9. doi:10.1016/S1047-2797(01)00245-9 [DOI] [PubMed] [Google Scholar]
- Kang H, Bullman T, Macfarlane G, Gray G. Mortality among US and UK veterans of the Persian Gulf War: a review. Occup. Environ. Med. 2002a;59:794–799. doi: 10.1136/oem.59.12.794. doi:10.1136/oem.59.12.794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang H, Mahan C, Lee K, Murphy F, Simmens S, Young H, Levine P.H. Evidence for a deployment-related Gulf War Syndrome by factor analysis. Arch. Environ. Health. 2002b;57:61–68. doi: 10.1080/00039890209602918. [DOI] [PubMed] [Google Scholar]
- Kang H, Natelson B, Mahan C, Lee K, Murphy P. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am. J. Epidemiol. 2003;157:141–148. doi: 10.1093/aje/kwf187. doi:10.1093/aje/kwf187 [DOI] [PubMed] [Google Scholar]
- Kay L, Jorgensen T, Jensen K. The epidemiology of irritable bowel syndrome in a random population: prevalence, incidence, natural history and risk factors. J. Intern. Med. 1994;236:23–30. doi: 10.1111/j.1365-2796.1994.tb01115.x. [DOI] [PubMed] [Google Scholar]
- Kelsall H.L, Sim M.R, Forbes A.B, Glass D.C, McKenzie D.P, Ikin J.F, Abramson M.J, Blizzard L, Ittak P. Symptoms and medical conditions in Australian veterans of the 1991 Gulf War: relation to immunisations and other Gulf War exposures. Occup. Environ. Med. 2004;61:1006–1013. doi: 10.1136/oem.2003.009258. doi:10.1136/oem.2003.009258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman A. University of California Press; Berkeley, CA: 1988. Patients and healers in the context of culture: an exploration of the borderland between anthropology, medicine, and psychiatry. [Google Scholar]
- Knoke J, Smith T, Gray G, Kaiser K, Hawksworth A. Factor analysis of self reported symptoms: does it identify a Gulf War Syndrome? Am. J. Epidemiol. 2000;152:379–388. doi: 10.1093/aje/152.4.379. doi:10.1093/aje/152.4.379 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Price R. Symptoms in the community: prevalence, classification and psychiatric comorbidity. Arch. Intern. Med. 1993;153:2474–2480. doi:10.1001/archinte.153.21.2474 [PubMed] [Google Scholar]
- Kroenke K, Wood D, Mangelsdorff A, Meier N, Powell J. Chronic fatigue in primary care. Prevalence, patient characteristics, and outcome. J. Am. Med. Assoc. 1988;260:929–934. doi:10.1001/jama.260.7.929 [PubMed] [Google Scholar]
- Kroenke K, Spitzer R, Williams J. Physical symptoms in primary care: predictors of psychiatric disorders and functional impairment. Arch. Fam. Med. 1994;3:774–779. doi: 10.1001/archfami.3.9.774. doi:10.1001/archfami.3.9.774 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Koslowe P, Roy M. Symptoms in 18,495 Persian Gulf war veterans. Latency of onset and lack of association with self-reported exposures. J. Occup. Environ. Med. 1998;40:520–528. doi: 10.1097/00043764-199806000-00004. doi:10.1097/00043764-199806000-00004 [DOI] [PubMed] [Google Scholar]
- Lee H, Gabriel R, Bale A, Bolton P, Blatchley N. Clinical findings of the second 1000 UK Gulf War veterans who attended the Ministry of Defence's Medical Assessment Programme. J. R. Army Med. Corps. 2001;147:153–160. doi: 10.1136/jramc-147-02-08. [DOI] [PubMed] [Google Scholar]
- Maconochie N, Doyle P, Carson C. Infertility among male UK veterans of the 1990-1 Gulf war: reproductive cohort study. Br. Med. J. 2004;329:196–201. doi: 10.1136/bmj.38163.620972.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nimnuan C, Rabe-Hesketh S, Wessely S, Hotopf M. How many functional somatic syndromes? J. Psychosom. Res. 2001;51:549–557. doi: 10.1016/s0022-3999(01)00224-0. doi:10.1016/S0022-3999(01)00224-0 [DOI] [PubMed] [Google Scholar]
- Pawlikowska T, Chalder T, Hirsch S, Wallace P, Wright D, Wessely S. Population based study of fatigue and psychological distress. Br. Med. J. 1994;308:763–766. doi: 10.1136/bmj.308.6931.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor S, Heaton K, White R, Wolfe J. Chemical sensitivity and chronic fatigue in Gulf War veterans: a brief report. J. Occup. Environ. Med. 2001;43:259–264. doi: 10.1097/00043764-200103000-00014. [DOI] [PubMed] [Google Scholar]
- Reid S, Hotopf M, Hull L, Ismail K, Unwin C, Wessely S. Multiple chemical sensitivity and chronic fatigue syndrome in British Gulf War veterans. Am. J. Epidemiol. 2001;153:604–609. doi: 10.1093/aje/153.6.604. doi:10.1093/aje/153.6.604 [DOI] [PubMed] [Google Scholar]
- Rook G, Zumla A. Gulf war syndrome: is it due to a systemic shift in cytokine balance towards a Th2 profile? Lancet. 1997;349:1831–1833. doi: 10.1016/S0140-6736(97)01164-1. doi:10.1016/S0140-6736(97)01164-1 [DOI] [PubMed] [Google Scholar]
- Roy M, Koslowe P, Kroenke K, Magruder C. Signs, symptoms, and ill defined conditions in Persian Gulf War veterans: findings from the Comprehensive Clinical Evaluation Program. Psychosom. Med. 1998;60:663–668. doi: 10.1097/00006842-199811000-00001. [DOI] [PubMed] [Google Scholar]
- Shapiro S, Lasarev M, McCauley L. Factor analysis of Gulf War illness: what does it add to our understanding of possible health effects of deployment. Am. J. Epidemiol. 2002;156:578–585. doi: 10.1093/aje/kwf087. doi:10.1093/aje/kwf087 [DOI] [PubMed] [Google Scholar]
- Simmons R, Maconochie N, Doyle P. Self-reported ill health in male UK Gulf War veterans: a retrospective cohort study. BMC Public Health. 2004;4:27. doi: 10.1186/1471-2458-4-27. doi:10.1186/1471-2458-4-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon G, Gater R, Kisely S, Piccinelli M. Somatic symptoms of distress: an international primary care study. Psychosom. Med. 1996;58:481–488. doi: 10.1097/00006842-199609000-00010. [DOI] [PubMed] [Google Scholar]
- Skapinakis P, Lewis G, Mavreas V. Temporal relations between unexplained fatigue and depression: longitudinal data from an international study in primary care. Psychosom. Med. 2004;66:330–335. doi: 10.1097/01.psy.0000124757.10167.b1. doi:10.1097/01.psy.0000124757.10167.b1 [DOI] [PubMed] [Google Scholar]
- Spitzer R.L, Kroenke K, Linzer M, Hahn S.R, Williams J.B, deGruy F.V, III, Brody D, Davies M. Health-related quality of life in primary care patients with mental disorders. Results from the PRIME-MD 1000 Study. J. Am. Med. Assoc. 1995;274:1511–1517. doi:10.1001/jama.274.19.1511 [PubMed] [Google Scholar]
- Steele L. Prevalence and patterns of Gulf War illness in Kansas veterans: association of symptoms with characteristics of person, place, and time of military service. Am. J. Epidemiol. 2000;152:992–1002. doi: 10.1093/aje/152.10.992. doi:10.1093/aje/152.10.992 [DOI] [PubMed] [Google Scholar]
- Stewart D. The changing face of somatisation. Psychosomatics. 1990;31:153–158. doi: 10.1016/S0033-3182(90)72188-3. [DOI] [PubMed] [Google Scholar]
- Stimpson N, Thomas H, Weightman A, Dunstan F, Lewis G. Psychiatric disorder in veterans of the Persian Gulf War of 1991: systematic review. Br. J. Psychiatry. 2003;182:391–403. doi:10.1192/bjp.182.5.391 [PubMed] [Google Scholar]
- The Iowa Persian Gulf Study Group Self-reported illnesses and health status among Gulf War veterans. A population based study. J. Am. Med. Assoc. 1997;277:238–245. doi:10.1001/jama.277.3.238 [PubMed] [Google Scholar]
- Unwin C, et al. Health of UK servicemen who served in the Persian Gulf War. Lancet. 1999;353:169–178. doi: 10.1016/S0140-6736(98)11338-7. doi:10.1016/S0140-6736(98)11338-7 [DOI] [PubMed] [Google Scholar]
- Unwin C, Hotopf M, Hull L, Ismail K, David A, Wessely S. Women in the Persian Gulf: lack of gender differences in long-term health effects of Service in United Kingdom Armed Forces in the 1991 Persian Gulf War. Mil. Med. 2002;167:406–413. [PubMed] [Google Scholar]
- Wegman D, Woods N, Bailar J. Invited commentary: how would we know a Gulf War Syndrome if we saw one? Am. J. Epidemiol. 1997;146:704–711. doi: 10.1093/oxfordjournals.aje.a009344. [DOI] [PubMed] [Google Scholar]
- Wessely S, Chalder T, Hirsch S, Wright D. The prevalence and morbidity of chronic fatigue and chronic fatigue syndrome: a prospective primary care study. Am. J. Public Health. 1997;87:1449–1455. doi: 10.2105/ajph.87.9.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wessely S, Hotopf M, Sharpe M. Oxford University Press; Oxford: 1998. Chronic fatigue and its syndromes. [Google Scholar]
- Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: one or many? Lancet. 1999;354:936–939. doi: 10.1016/S0140-6736(98)08320-2. doi:10.1016/S0140-6736(98)08320-2 [DOI] [PubMed] [Google Scholar]
- Wolfe F, Ross K, Anderson J, Russell I.J, Hebert L. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38:19–28. doi: 10.1002/art.1780380104. [DOI] [PubMed] [Google Scholar]


