Abstract
One candidate cause of Gulf War illness is vaccination against infectious diseases including medical counter-measures against biological weapons. One influential theory has suggested that such mass-vaccination caused a shift in immune response to a Type 2 cytokine pattern (Th2), which it was suggested was accompanied by a chronic fatigue syndrome-like illness. This article critically appraises this theory. We start by examining epidemiological evidence, which indicates that single vaccines are unlikely to be a substantial cause of Gulf War illness, but that there was a modest relationship with multiple vaccines, which was strongest in those vaccinated while deployed to the Gulf. These relationships may be affected by recall bias. We conclude by examining the results of immunological studies carried out in veterans or in a relevant setting in vitro. The balance of evidence from immunological studies on veterans returning from the War, including those developing multi-symptom illness, is that the immune response has not become polarized towards Th2. In summary, the epidemiological evidence for a multiple vaccine effect on Gulf War-related illness remains a potentially important aetiological lead, but mechanistic studies available at this stage do not identify any immunological basis for it.
Keywords: vaccination, Gulf War illness, anthrax vaccine, dendritic cells, T lymphocytes, cytokines
1. Introduction
Modern military medicine has made considerable strides in controlling infectious diseases, which have in many deployments caused more deaths than have direct combat injuries. The Gulf War was a success story for preventive medicine, in that casualties from infectious diseases were low. This was probably due in part to vaccination against common diseases, and the use of insecticides and insect repellents, all of which have since been suggested as potential causes of Gulf War illness. If the multi-symptom illnesses seen in Gulf War veterans are caused by a single or small number of agents, it is necessary to identify hazards to which many veterans would have been exposed. Some hazards which have attracted considerable interest as potential causes such as depleted uranium are—from an epidemiological perspective—inherently unlikely to be a major cause of illness, as too few personnel could have been exposed to cause the health effect observed (Hotopf & Wessely 2005). This is one reason why medical counter measures (MCM) against nuclear, biological and chemical attack which theoretically were available to all deployed personnel are an important potential cause.
While receiving multiple vaccines has frequently been cited among the lay media as a cause of Gulf War illness, a speculative article published in The Lancet by Graham Rook & Alimuddin Zumla provided scientific support for the hypothesis (Rook & Zumla 1997). Rook & Zumla suggested that Gulf War illness shared many features with chronic fatigue syndrome (CFS). They further suggested that CFS in civilians is associated with an underlying shift in the immune response from a Th1 to Th2 pattern. They then postulated that mass vaccination was the most likely cause of this shift in Gulf War illness and could account for the CFS-like multi-symptom illness. They pointed out that vaccination in Gulf War veterans had a number of features likely to cause this pattern: first, personnel received multiple vaccines in a short space of time; second, in UK personnel at least, pertussis vaccine was used as an adjuvant in order to enhance the immune response to anthrax and plague vaccines; third, vaccination often took place in stressful circumstances, namely during the deployment.
This article aims to determine (i) whether there is evidence from epidemiological studies to suggest a link between vaccination and multi-symptom illness; (ii) whether there is any evidence for the type of shift in cytokine profile proposed by Rook & Zumla and to characterize any other differences in immune parameters between Gulf veterans and controls; and (iii) whether any relationship between vaccines and multi-symptom illness can be explained by such observed immune changes.
2. The vaccination programme
In 1990–1991, the threat that Saddam Hussein would use his biological warfare capabilities against Coalition forces was taken seriously. This meant that military personnel were given a range of different vaccines. MCM against biological weapons in UK personnel consisted of vaccines to anthrax, plague and pertussis as an adjuvant (Ministry of Defence 2000). No previous deployment had involved such mass vaccination against biological warfare agents. Canadian personnel received a similar combination to the UK forces. For the US forces, pertussis was not used, a different variety of anthrax was used and personnel received botulinum toxoid vaccine (Department of Defense 2000).
As well as receiving vaccines against potential biological warfare attack, numerous additional routine vaccines were provided. For US personnel these included boosters of tetanus, diphtheria and oral polio vaccines; and other measures recommended for the region including meningococcal, typhoid and yellow fever vaccines, and immune globulin against hepatitis A (Department of Defense 2000). Similarly, the UK forces were routinely provided boosters for tetanus, diphtheria (if required) and oral polio, plus typhoid, yellow fever, cholera, hepatitis A and B (if indicated), meningococcal meningitis A and B. This, with a total of three anthrax, two pertussis and two plague vaccines, would bring the total number of potential vaccines received over a six-month period to 20 (Ministry of Defence 2000).
3. Epidemiological evidence
(a) Individual vaccines
The first study to report on the relationship between vaccines and illness in Gulf War veterans was from King's College London (Unwin et al. 1999). This was a large cross-sectional study which compared a variety of health outcomes between Gulf War veterans and two comparison groups, military personnel at the time of the Gulf (Era) and veterans of United Nations' Bosnian peace-keeping duties deployed in 1992–1996. The first problem identified by the authors was that relatively few veterans (30%) had any record of their vaccine exposure, making it difficult to determine whether the reported exposure was accurate. We performed brief telephone interviews to determine whether individuals who reported still having records had used them to complete their questionnaires and found the majority (80%) had. Perhaps surprisingly, the pattern of vaccine uptake between those with and those without records was broadly similar and the prevalence of vaccine uptake in the study by and large accorded with figures subsequently reported by the UK Ministry of Defence (Ministry of Defence 2000).
When a multi-symptom health outcome approximating to the Centers for Disease Control (CDC) definition of Gulf War illness was used as the outcome, no clear pattern of association with individual routine vaccines was found (Unwin et al. 1999). There were small (maximum odds ratio (OR) 1.3) and marginally statistically significant associations between some of the routine vaccines and illness among individuals without vaccine records, but none of these associations were present in those with vaccine records, indicating a possible reporting bias. For biological warfare vaccines, the pattern was slightly different. There was a modest association between illness and anthrax (OR 1.4) and pertussis vaccines (OR 1.3), but not for plague. These findings did not suggest a single vaccine could have been responsible for illness in the Gulf veterans, and the effect sizes reported were smaller than those seen for any other individual exposures reported, apart from ‘eating local food’. A similar modest relationship (OR 1.5) between anthrax vaccine and multi-symptom illness was shown in one US study (Wolfe et al. 2002).
These studies on individual vaccines relied on self-report. Another study used data from the US National Health Survey of Gulf War Era Veterans and Their Families (Mahan et al. 2003), in which 11 441 Gulf War veterans participated. Those who reported having received anthrax vaccination were more likely to have experienced most of the outcomes assessed, including a range of physical symptoms, functional impairment and so on. However, for a small subset of participants, Department of Defense records were available, which indicated the participant had definitely had the anthrax vaccine. When those with documented vaccination were compared with those with no (self-reported) vaccine, the strength of most associations fell, although several remained statistically significant. Finally, there was evidence suggestive of reporting bias when the group who had documented exposure to the vaccine were assessed in isolation. Of these, approximately 10% answered ‘no’ when asked about exposure to anthrax vaccine. This group who had mis-recorded their vaccine exposure were considerably healthier than those who had recorded it accurately. What the study was unable to demonstrate, because there was no documented evidence of people who did not receive the vaccine, was whether the converse effect operated—i.e. whether illness status influenced self-reported exposure in those known not to have received anthrax vaccination.
Hence from the available information on individual vaccinations, it seems unlikely that this is a major influence on illness in Gulf War veterans. The effect sizes are generally small, and even if concerns about reporting bias were ignored, the population attributable risk percentage of anthrax vaccination, assuming 70% were exposed to at least one vaccine, would be 9% based on our original data. This means that if the relationship were genuine, anthrax vaccination could account for no more than 9% of all cases of multi-symptom illness in Gulf War veterans. Given our concerns regarding the possible biased nature of the association, the real estimate is likely to be smaller.
(b) Multiple vaccines
The Rook & Zumla hypothesis does not suggest that vaccines in isolation would cause difficulties. Instead what counted was the total number of reported vaccines. Using the King's data, we were able to show a modest difference, larger than that for individual vaccines. Individuals in the Gulf cohort who had retained their vaccine records and fell into the highest quartile of vaccine exposure (more than 6) were more likely to report multiple symptoms (OR 1.8; Unwin et al. 1999). Further evidence was provided by a comparison of Gulf and Bosnia veterans (see figure 1). Because Bosnia veterans had received vaccines, it was possible to determine whether there was a difference in the effect of multiple vaccines in the two cohorts, and we did indeed find this, with Bosnia veterans having a weaker association with multiple vaccines (OR 1.2), and a statistically significant interaction term (p=0.03) between deployment and vaccines and their effect on our outcome (Unwin et al. 1999). Although a potentially important finding, the effect size was still relatively modest, and close to those reported for nearly all associations between hazards and CDC multiple symptoms.
Figure 1.
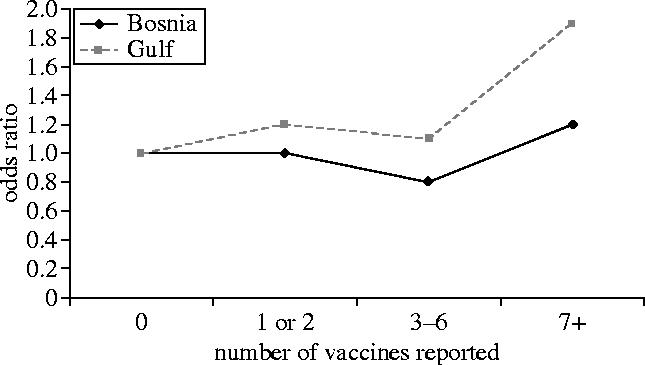
Relationship between total number of vaccines reported and multi-symptom illness, according to place of deployment. Data from Unwin et al. (1999).
Subsequent reports have, to some extent, replicated these findings. Cherry et al. (2001) used a similar sampling frame to the King's study to identify 7971 British service personnel who had deployed to the Gulf. Reassuringly, a similar proportion of veterans had retained vaccination records and the pattern of the total number of vaccines recorded was similar to that shown in our study. The main outcome was the total severity of symptoms reported and a clear dose–response relationship was shown with incrementally higher symptom scores for those who reported more vaccines, an effect which was similar for those with and without vaccine records. A major Australian study of 1456 Gulf War veterans (Kelsall et al. 2004) has also shown an effect of multiple vaccines and total symptom scores, with those reporting no vaccines having a mean symptom score of 13.3 and those reporting 10 or more vaccines having a mean symptom score of 18.3.
If there was an association between multiple vaccines and illness was this worsened by receiving the vaccines at a time of stress, i.e. during deployment? This was a further claim made by Rook & Zumla. Only the King's study has attempted to answer this (Hotopf et al. 2000). There was a strong dose–response effect between multiple vaccines and illness, but this was limited to those who reported receiving the multiple vaccines while deployed in theatre (see figure 2). Here now were powerful effect sizes with an OR of 5.0 in the top quintile of personnel who were deployed. However, further analyses indicated that there was no statistically significant difference in the overall effect of vaccines before and during deployment, indicating that although the relationship looked compelling, it would be wrong to assume that no association existed between multiple vaccines received before deployment and illness (Hotopf 2000). Essentially, the study lacked statistical power to determine whether the effect of multiple vaccines was isolated to those who received them on deployment, and despite being an a priori hypothesis which was apparently supported by the data, we are cautious regarding its meaning and like many other intriguing findings, it requires replication.
Figure 2.
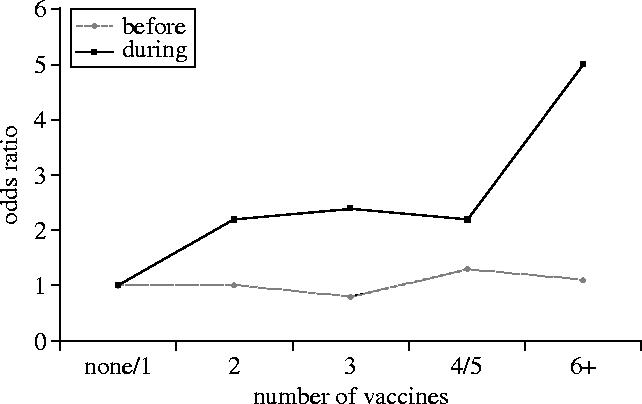
Relationship between total vaccines received before or during deployment and multi-symptom illness in Gulf War 14 veterans. Data from Hotopf et al. (2000).
(c) Exposures and recall bias
The primary problem with all such research on vaccines pertains to recall of exposure. We have demonstrated elsewhere that recall of exposures is not constant, indeed Gulf veterans when presented with the same list of exposures on two separate occasions had only modest test–retest reliability (Wessely et al. 2003). Further, changes in exposure status were not independent of changes in health status: individuals whose health improved had an accompanying reduction in total exposures recalled and vice versa. Thus, recall bias exists. While it is possible that limiting analyses to individuals who had vaccine records to some extent protected against this, there is no guarantee that recall bias has not operated. For example, personnel who are currently well may have put less energy into reading their vaccine record and thus report fewer vaccines than those who remain deeply concerned about their health (Mahan et al. 2003). Thus, one of the key research and practical conclusions of this epidemiological review is the need for robust systems to record vaccination and other exposure data before, during and after military deployments.
4. Immunological studies
(a) Exploring the Th1/Th2 hypothesis I: theoretical considerations
Before examining the evidence for Th2 skewing in Gulf War-related illness, it is worth considering the origin and rational basis of the Th1/Th2 hypothesis. CD4 helper T cells were originally described as becoming polarized towards different cytokine profiles in murine studies, leading to the delineation of Th1 and Th2 subsets, the characteristics of which are shown in table 1 (Angello et al. 2003; Gor et al. 2003; Kapsenberg 2003; Kalinski & Moser 2005). Subsequent confirmation that these subsets could be defined in man (Romagnani 1997) led to an intense period of experimentation, during which there was a particular focus on defining the immunopathological bases of a variety of human conditions as being Th1 or Th2. The Th1/Th2 classification of disease is particularly strong in relation to allergic diseases that have a clearly demonstrable component of IgE-mediated, immediate (Type I) hypersensitivity (Singh et al. 1999) with associated Th2 cell bias. In contrast, autoimmune diseases in which there is a strong tissue destructive element to the pathogenesis (e.g. Type 1 diabetes mellitus) are characterized by Th1 autoreactive T cells (Arif et al. 2004). However, for many human diseases, the Th-picture is complex and there is rarely such clear polarity of the immune response.
Table 1.
Properties of Th1 and Th2 cells. (STAT1, 4, 6, signal transducer and activator of transcription 1, 4, 6; T-bet, Th1-specific T box transcription factor; GATA3, GATA binding protein 3; c-Maf, proto-oncogene c-maf, musculoaponeurotic fibrosarcoma oncogene homologue, maf is a family of genes encoding bZIP transcription factors; NFAT, nuclear factor of activated T cell; TSLP, thymic stromal lymphopoietin.)
| property | Th1 | Th2 |
|---|---|---|
| cytokine production | interleukin-2 (IL-2) | IL-4, IL-6 |
| interferon-γ (IFN-γ) | IL-5, IL-9 | |
| lymphotoxin-β | IL-13 | |
| IL-10 | ||
| associated immunoglobulin class | IgG2a in mice, IgG2 in man | IgG1, IgE |
| transcription factors | STAT4, T-bet, STAT1 | STAT6, GATA3, c-Maf, NFAT |
| effector properties | inflammatory cellular responses | humoral immunity (especially IgE-mediated) and inhibition of Th1 responses |
| provoking tissue factors | IFN-γ, α, β, IL12p70, TNFβ, IL-18, IL-27, IL-23 | IL-4, IL-5, IL-9, IL-13, IL-25, TSLP, cAMP up regulators (PGE2, histamine) |
| provoking factors in vivo | intracellular pathogens (bacteria, viruses) | extracellular pathogens: parasites (helminths), bacteria, fungi |
| disease associations | tissue destructive organ-specific autoimmunity (e.g. Type 1 diabetes, multiple sclerosis, posterior uveitis) | allergy, autoantibody-associated autoimmune disease (e.g. systemic lupus erythematosus) |
It is against this background that the Th1/Th2 hypothesis of Gulf War-related illness was proposed by Rook & Zumla (1997). The central tenets of the hypothesis are shown in table 2 and deserve some scrutiny 8 years later. The first critical observation of the proposal is the similar constellation of symptoms reported by Gulf War veterans and patients with CFS (Ismail & Lewis 2006), itself asserted to be a syndrome associated with Th2 skewing in view of increased allergic events and reduced Th1-like activity. In reality, the putative association between CFS and allergy is controversial. Nonetheless, in a study designed to directly examine the balance of Th1 and Th2 cells in the peripheral blood of CFS patients, we observed a significant increase in Th2 effector memory cells over normal values (Skowera et al. 2004), and other studies similarly support a Th2 bias in this condition (Hanson et al. 2001). However, Th2 effector memory cell numbers were not associated with clinical status in CFS patients in our study, nor with total or allergen-specific IgE levels or self-reported allergy, leading us to conclude that Th2 skewing might not reflect a primary pathogenetic process. More importantly, we subsequently applied the identical technology in our laboratory to the study of Th cells in Gulf War veterans (see below).
Table 2.
The main tenets of the Th1/Th2, ‘Rook & Zumla’ hypothesis for Gulf War-related illness. (CFS, chronic fatigue syndrome.)
| observation | explanation | comments |
|---|---|---|
| Gulf War-related illness is CFS-like and therefore a Th2 disease | symptoms similar in the two conditions; CFS is a Th2 disease | there is support for CFS being characterized by a Th2 bias; but no evidence that CFS symptoms and Th2 skewing are related |
| Th2-biasing factors | ||
| pertussis adjuvant | pertussis infection and the whole cell vaccine are Th1 inducers; but the acellular vaccine component of pertussis used as adjuvant biases to Th2 | pertussis whole cell adjuvant was used for UK, but not US veterans; yet multi-symptom illness is similar and similarly prevalent in both; no evidence that pertussis skewed the anthrax response to Th2 (Skowera et al. in press) |
| large antigen load in multiple vaccines | studies show that high-titre vaccines may skew to Th2 response | studies are open to interpretation and relate to single, rather than multiple, antigens; more recent studies show that high antigen dose more likely to skew responses towards Th1 and low concentrations of the same antigen can drive the responses towards Th2 (Hosken et al. 1995; Itoh & Germain 1997) |
| high circulating glucocorticoids (GCs) during deployment | in vitro studies show potent effects of GCs in skewing to Th2 | ‘stress’ effects on immune function in vitro or in vivo are complex and do not follow a simple Th1/Th2 pattern (Glaser & Kielcolt-Glaser 2005) |
Having put forward this associative foundation for the hypothesis, a mechanistic basis for the immunological events was sought. The second and third elements of the proposal related to MCMs, the first of which was a potential role for the pertussis vaccine, administered as an adjuvant to boost the generation of anthrax immunity. The acellular pertussis vaccine is known from studies performed in vitro to induce Th2 skewing (Mu & Sewell 1993), although there is little or no human in vivo data to support this. It should also be noted that pertussis use was a feature of the preparation of UK troops but not other nations, and that pertussis whole cell vaccine was used, which is known to be a potent Th1-polarizing agent (Skowera et al. in press). A testable prediction in relation to pertussis is that if it is a potent Th2-biasing adjuvant, then the response to the co-administered antigens (in this case anthrax) should likewise be Th2 biased. We therefore examined the T helper cell recall response to anthrax in the blood of UK Gulf War veterans whose vaccination records confirm receipt of both anthrax vaccine and pertussis adjuvant. The results show no evidence of Th2 bias, rather a mixed Th1/Th2 pattern of responsiveness similar to that seen against other vaccines such as tetanus toxoid (Skowera et al. in press). There was a potent Th1 cell response detectable, as well as the presence of numerous IL-13 secreting Th2 cells, but IL-4 secreting Th2 cells were rare. In light of this, it would seem highly paradoxical for pertussis to prove capable of inducing a ‘global’ skewing of the immune response to Th2 sufficient to cause multi-symptom disease, without, at the same time, achieving a similar Th2 effect on the immune response to a co-administered vaccine.
The second counter-measure invoked as Th2 biasing was the shear excess of immunological stimuli represented by the multiplicity of vaccines, administered within a relatively short time frame. The putative mechanisms through which excess antigen load might lead to Th2 biasing are not immediately obvious, and in the original description of the hypothesis, the supporting citations related to excessive stimulus with a single vaccine rather than multiple vaccines (Bretscher et al. 1992; Hernandez-Pando & Rook 1994; Aaby 1995). The immunological arbiter of Th polarization is the dendritic cell (DC), which acquires stimuli such as vaccines through pinocytosis, digests them proteolytically and then presents them as short fragments to naive T cells, along with requisite Th-polarizing signals (cytokines, surface molecules), which are generated as a result of the integration of numerous signals relating to the ‘nature’ of the antigen (Reis e Sousa 2001). Chemical and other manipulations of DCs are known to be able to shape the polarizing signals and lead to skewing, but there is no evidence to date that DCs are altered in the presence of multiple vaccine agents. We have attempted to test this hypothesis in vitro, using human DCs exposed to multiple vaccines including anthrax, plague and whole cell pertussis. Our finding is that DCs summate the signals available into a final, integrated effector response (Skowera et al. in press). For example, in the presence of three vaccines, of which one is a strong Th1-biasing stimulus, DCs become potent producers of Th1-skewing cytokines and promote Th1 polarization. We could find no evidence that additional stimuli inhibited or subverted the DC response. In summary, the epidemiological evidence for a multiple vaccine effect on Gulf War-related illness remains a potentially important aetiological lead, but mechanistic studies available at this stage do not identify any immunological basis for it. Prospective, case-controlled human studies are in progress to assess the immunological outcome of different vaccination regimes reflecting high and low antigen loads, and their outcome should be able to settle this important debate. These studies may also be capable of casting light on the final platform of the Th2 hypothesis, namely the role of stress hormones in Th skewing, for which compelling data exist from studies in vitro (Ramirez et al. 1996), but for which studies on intact animals are hard to design and interpret.
In summary, it is a matter of debate whether the Th1/Th2 hypothesis, as originally written, stands up to careful scrutiny. Nonetheless, it is testable, and focused several post-conflict studies onto the immune system.
(b) Exploring the Th1/Th2 hypothesis II: experimental considerations
The combination of an explicit immunological hypothesis and a possible role for vaccines in Gulf War-related illness spawned numerous immunological studies, the majority of which had either in vitro design, addressing the effects of putative aetiological agents on the function of cell lines, or studied the immune responses of experimental animals. These studies will not be discussed further; rather this section will focus on those studies examining immune function in Gulf War veterans. Of these, there have been relatively few (table 3; Soetekouw et al. 1999; Zhang et al. 1999; Brimacombe et al. 2002; Everson et al. 2002; Skowera et al. 2002; Vojdani & Thrasher 2005). Clearly, there are important considerations in relation to these studies, not least the performance of peripheral blood analyses several years after the end of the conflict. On the other hand, some studies were designed to include veterans who still had symptoms at the time of testing (Soetekouw et al. 1999; Zhang et al. 1999; Brimacombe et al. 2002; Everson et al. 2002; Skowera et al. 2002), and some included veterans who had been symptomatic but had then shown some recovery, enabling the inter-relation of immune parameters and illness to be explored (Skowera et al. 2002).
Table 3.
Immunological studies on Gulf War or similar veterans.
| study | study design | Th1/Th2 hypothesis tested | immunological analysis | results support Th2 hypothesis? | comments |
|---|---|---|---|---|---|
| Zhang et al. (1999) | cross-sectional; veteransa and non-veterans fulfilling case definition of CFS | yes | mRNA levels of cytokine genes | no | resting PBLs used rather than purified or stimulated CD4 cells |
| Soetekouw et al. (1999) | cross-sectional; UNTAC soldiers with multi-symptom illness | yes | direct quantification of cytokine-secreting CD4 cells | no | |
| Brimacombe et al. (2002) | cross-sectional; veterans and non-veterans fulfilling case definition of CFS or healthy veterans | yes | mRNA levels of cytokine genes | yes | no conventional group-to-group comparisons; IL-6 invoked as a ‘Th2’ cytokine |
| Everson et al. (2002) | cross-sectional; ill and well veterans | yes | cytokines secreted after stimulation of PBLs | no | |
| Skowera et al. (2002) | cross-sectional; veterans of Gulf and Bosnia conflicts; ill and well veterans | yes | direct quantification of cytokine-secreting CD4 cells | no | resting, activated, CD4 and CD8 cells studied |
| Vojdani & Thrasher (2005) | cross-sectional; veterans and control subjects | no | multiple analyses, including tests of cell-mediated and antibody responses | n/a | no compelling evidence of Th1/Th2 imbalance |
Veterans are from the 1990–91 Gulf War unless otherwise stated. PBLs, peripheral blood lymphocytes; CFS, chronic fatigue syndrome; UNTAC, United Nations Transitional Authority for Cambodia.
Of the six studies on veterans, five were able or designed to test the Th2 hypothesis. Of these, four resulted in a negative conclusion, while one concludes the existence of a Th2 factor that exerts its functional status via changes in cognitive abilities (Brimacombe et al. 2002). The latter study involves the analysis of clusters of clinical and immunological characteristics that predict CFS caseness for Gulf War veterans. In the absence of any reporting of the raw data for the Type 2 cytokine cluster, this study remains open to interpretation. In contrast are the four studies using direct approaches to the assessment of Th2 cell activation in Gulf War-related illness. These include detection of Th2 cytokine expression in the form of mRNA, secreted protein and intracellular expression. While the former analyses are unable to specify the cellular source, examination of intracellular cytokine expression is a powerful means of directly enumerating Th1 and Th2 cells, and has been widely used in the definition of cellular responses in patients with Th1-biasing viruses. Indeed, as discussed previously, this technique was, in our hands, able to detect Th2 skewing in CFS patients (Skowera et al. 2004), while the identical approach was unable to find Th1/Th2 disturbance in UK veterans with Gulf War-related illness. Thus, the outcome of these studies is a negative one in terms of relating Th2 skewing to Gulf War service or Gulf War-related illness.
We have recently taken a further step in the analysis of Th1/Th2 balance in Gulf War veterans (Allen et al. in press). We reasoned that, according to the Rook & Zumla hypothesis, the immune response to neo-antigens, co-administered with multiple other vaccines and pertussis, should be Th2 biased. Troops deployed in the Gulf War were indeed exposed to neo-antigens, in the form of the anthrax and plague vaccines. In our study, we show that recall T cell immunity to anthrax has equal balance of Th1 and Th2-type responses, while plague immunity is polarized towards Th1. This study argues strongly against the Th2 hypothesis of Gulf War-related illness.
5. Conclusions
Our results suggest that although there may be epidemiological evidence for an association between multiple vaccines and multi-symptom illness, this is relatively weak, and subject to recall bias. The balance of immunological studies that have directly addressed Th2 bias of the immune response as an explanation for Gulf War-related illness appears to favour rejection of the hypothesis. We conclude that multiple vaccination, or the perception of it, could have favoured illness as an outcome of the post-deployment era, but that this has little to do with any putative effects on the immune system.
Acknowledgments
Work by the authors discussed in this article was supported by the UK Medical Research Council and US Department of Defense.
Footnotes
One contribution of 17 to a Theme Issue ‘The health of Gulf War veterans’.
References
- Aaby P. Assumptions and contradictions in measles and measles immunization research: is measles good for something? Soc. Sci. Med. 1995;41:673–686. doi: 10.1016/0277-9536(95)00038-9. doi:10.1016/0277-9536(95)00038-9 [DOI] [PubMed] [Google Scholar]
- Allen J.S, Skowera A, Rubin G.J, Wessely S.C, Peakman M. Long lasting T cell responses to biological warfare vaccines in human vaccines. Clin. Infect. Dis. In press doi: 10.1086/504806. [DOI] [PubMed] [Google Scholar]
- Angello D, Lankford C.S, Bream J, Morinobu A, Gadina M, O'Shea J.J, Frucht D.M. Cytokines and transcription factors that regulate T helper cell differentiation: new players and new insights. J. Clin. Immunol. 2003;23:147–161. doi: 10.1023/a:1023381027062. [DOI] [PubMed] [Google Scholar]
- Arif S, Tree T.I, Astill T.P, Tremble J.M, Bishop A.J, Dayan C.M, Roep B.O, Peakman M. Autoreactive T cell responses show proinflammatory polarization in diabetes but a regulatory phenotype in health. J. Clin. Invest. 2004;113:451–463. doi: 10.1172/JCI19585. doi:10.1172/JCI200419585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bretscher P.A, Wei A.G, Menon J.N, Bielefeldt-Ohmann H. Establishment of stable, cell-mediated immunity that makes ‘susceptible’ mice resistant to Leishmania major. Science. 1992;257:539–542. doi: 10.1126/science.1636090. [DOI] [PubMed] [Google Scholar]
- Brimacombe M, Zhang Q, Lange G, Natelson B.H. Immunological variables mediate cognitive dysfunction in Gulf War veterans but not civilians with chronic fatigue syndrome. Neuroimmunomodulation. 2002;10:93–100. doi: 10.1159/000065185. doi:10.1159/000065185 [DOI] [PubMed] [Google Scholar]
- Cherry N, Creed F, Silman A, Dunn G, Baxter D, Smedley J, Taylor S, MacFarlane G.J. Health and exposures of United Kingdom Gulf War veterans. Part II: the relation of health to exposure. Occup. Environ. Med. 2001;58:299–306. doi: 10.1136/oem.58.5.299. doi:10.1136/oem.58.5.299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Defense . Department of Defense; Washington, DC: 2000. Information paper: vaccine use during the Gulf War. [Google Scholar]
- Everson M.P, Shi K, Aldridge P, Bartolucci A.A, Blackburn W.D. Immunological responses are not abnormal in symptomatic Gulf War veterans. Ann. N. Y. Acad. Sci. 2002;966:327–342. doi: 10.1111/j.1749-6632.2002.tb04233.x. [DOI] [PubMed] [Google Scholar]
- Glaser R, Kielcolt-Glaser J.K. Stress-induced immune dysfunction: implications for health. Nat. Rev. Immunol. 2005;5:243–251. doi: 10.1038/nri1571. doi:10.1038/nri1571 [DOI] [PubMed] [Google Scholar]
- Gor D.O, Rose N.R, Greenspan N.S. TH1–TH2: a Procrustean paradigm. Nat. Immunol. 2003;4:503–505. doi: 10.1038/ni0603-503. doi:10.1038/ni0603-503 [DOI] [PubMed] [Google Scholar]
- Hanson S.J, Gause W, Natelson B. Detection of immunologically significant factors for chronic fatigue syndrome using neural-network classifiers. Clin. Diagn. Lab. Immunol. 2001;8:658–662. doi: 10.1128/CDLI.8.3.658-662.2001. doi:10.1128/CDLI.8.3.658-662.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez-Pando R, Rook G.A.W. The role of TNF-alpha in T-cell-mediated inflammation depends on the Th1/Th2 cytokine balance. Immunology. 1994;82:591–595. [PMC free article] [PubMed] [Google Scholar]
- Hosken N.A, Shibuya K, Heath A.W, Murphy K.M, O'Garra A. The effect of antigen dose on CD4+ T helper cell phenotype development in a T cell receptor-alpha beta-transgenic model. J. Exp. Med. 1995;182:1579–1584. doi: 10.1084/jem.182.5.1579. doi:10.1084/jem.182.5.1579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotopf M. Reanalysis of Gulf War vaccination data does not contradict findings. Br. Med. J. 2000;321:761. [PMC free article] [PubMed] [Google Scholar]
- Hotopf M, Wessely S. Epidemiology and the fog of war: lessons from the 1990–1991 Gulf War. Int. J. Epidemiol. 2005;34:791–780. doi: 10.1093/ije/dyi102. doi:10.1093/ije/dyi102 [DOI] [PubMed] [Google Scholar]
- Hotopf M, David A, Hull L, Ismail K, Unwin C, Wessely S. Role of vaccinations as risk factors for ill health in veterans of the Gulf War: cross sectional study. Br. Med. J. 2000;320:1363–1367. doi: 10.1136/bmj.320.7246.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ismail K, Lewis G. Multi-symptom illnesses, unexplained illness and Gulf War Syndrome. Phil. Trans. R. Soc. B. 2006;361:543–551. doi: 10.1098/rstb.2006.1815. doi:10.1098/rstb.2006.1815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itoh Y, Germain R.N. Single cell analysis reveals regulated hierarchical T cell antigen receptor signaling thresholds and intraclonal heterogeneity for individual cytokine responses of CD4+ T cells. J. Exp. Med. 1997;186:757–766. doi: 10.1084/jem.186.5.757. doi:10.1084/jem.186.5.757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalinski P, Moser M. Consensual immunity: success-driven development of T-helper-1 and T-helper-2 responses. Nat. Rev. Immunol. 2005;5:251–260. doi: 10.1038/nri1569. doi:10.1038/nri1569 [DOI] [PubMed] [Google Scholar]
- Kapsenberg M.L. Dendritic-cell control of pathogen-driven T-cell polarization. Nat. Rev. Immunol. 2003;3:984–993. doi: 10.1038/nri1246. doi:10.1038/nri1246 [DOI] [PubMed] [Google Scholar]
- Kelsall H.L, Sim M.R, Forbes A.B, Glass D.C, McKenzie D.P, Ikin J.F, Abramson M.J, Blizzard L, Ittak P. Symptoms and medical conditions in Australian veterans of the 1991 Gulf War: relation to immunisations and other Gulf War exposures. Occup. Environ. Med. 2004;12:1006–1013. doi: 10.1136/oem.2003.009258. doi:10.1136/oem.2003.009258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahan C.M, Kang H.K, Dalager N.A, Heller J.M. Anthrax vaccination and self-reported symptoms, functional status, and medical conditions in the National Health Survey of Gulf War Era Veterans and Their Families. Ann. Epidemiol. 2003;13:1–8. doi: 10.1016/S1047-2797(03)00124-8. doi:10.1016/S1047-2797(02)00423-4 [DOI] [PubMed] [Google Scholar]
- Ministry of Defence . Ministry of Defence; London: 2000. Implementation of the immunisation programme against biological warfare agents for UK forces during the Gulf Conflict 1990/1991. [Google Scholar]
- Mu H.H, Sewell W.A. Enhancement of interleukin-4 production by pertussis toxin. Infect. Immun. 1993;61:2834–2840. doi: 10.1128/iai.61.7.2834-2840.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez F, Fowell D.J, Puklavec M, Simmonds S, Mason D. Glucocorticoids promote a TH2 cytokine response by CD4+ T cells in vitro. J. Immunol. 1996;156:2406–2412. [PubMed] [Google Scholar]
- Reis e Sousa C. Dendritic cells as sensors of infection. Immunity. 2001;14:495–498. doi: 10.1016/s1074-7613(01)00136-4. doi:10.1016/S1074-7613(01)00136-4 [DOI] [PubMed] [Google Scholar]
- Romagnani S. The Th1/Th2 paradigm. Immunol. Today. 1997;18:263–266. doi: 10.1016/s0167-5699(97)80019-9. doi:10.1016/S0167-5699(97)80019-9 [DOI] [PubMed] [Google Scholar]
- Rook G.A.W, Zumla A. Gulf War syndrome: is it due to a systemic shift in cytokine balance towards a Th2 profile? Lancet. 1997;39:1831–1833. doi: 10.1016/S0140-6736(97)01164-1. [DOI] [PubMed] [Google Scholar]
- Singh V.K, Mehrotra S, Agarwal S.S. The paradigm of Th1 and Th2 cytokines: its relevance to autoimmunity and allergy. Immunol. Res. 1999;20:147–161. doi: 10.1007/BF02786470. [DOI] [PubMed] [Google Scholar]
- Skowera A, et al. Cellular immune activation in Gulf War veterans. J. Clin. Immunol. 2002;24:66–73. doi: 10.1023/B:JOCI.0000018065.64685.82. doi:10.1023/B:JOCI.0000018065.64685.82 [DOI] [PubMed] [Google Scholar]
- Skowera A, Cleare A, Blair D, Bevis L, Wessely S, Peakman M. High levels of type 2 cytokine-producing cells in chronic fatigue syndrome. Clin. Exp. Immunol. 2004;135:294–302. doi: 10.1111/j.1365-2249.2004.02354.x. doi:10.1111/j.1365-2249.2004.02354.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skowera A, de Jong E.C, Schuitemaker J.H, Allen J.S, Wessely S, Griffiths G.S, Kapsenberg M.L, Peakman M. Analysis of anthrax and plague bio-warfare vaccine interactions with human monocyte-derived dendritic cells. J. Immunol. 2006;175:7235–7243. doi: 10.4049/jimmunol.175.11.7235. [DOI] [PubMed] [Google Scholar]
- Soetekouw P.M, de Vries M, Preijers F.W, Van Crevel R, Bleijenberg G, van der Meer J.W. Persistent symptoms in former UNTAC soldiers are not associated with shifted cytokine balance. Eur. J. Clin. Invest. 1999;29:960–963. doi: 10.1046/j.1365-2362.1999.00545.x. doi:10.1046/j.1365-2362.1999.00545.x [DOI] [PubMed] [Google Scholar]
- Unwin C, et al. Health of UK servicemen who served in the Persian Gulf War. Lancet. 1999;353:169–178. doi: 10.1016/S0140-6736(98)11338-7. doi:10.1016/S0140-6736(98)11338-7 [DOI] [PubMed] [Google Scholar]
- Vojdani A, Thrasher J.D. Cellular and humoral immune abnormalities in Gulf War veterans. Environ. Health Perspect. 2005;112:840–846. doi: 10.1289/ehp.6881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wessely S, Unwin C, Hotopf M, Hull L, Ismail K, Nicolaou V, David A. Stability of recall of military hazards over time: Evidence from the Persian Gulf War of 1991. Br. J. Psychiatry. 2003;183:314–322. doi: 10.1192/bjp.183.4.314. doi:10.1192/bjp.183.4.314 [DOI] [PubMed] [Google Scholar]
- Wolfe J, Proctor S.P, Erickson D.J, Hu H. Risk factors for multisymptom illness in US Army veterans of the Gulf War. J. Occup. Environ. Med. 2002;44:271–281. doi: 10.1097/00043764-200203000-00015. [DOI] [PubMed] [Google Scholar]
- Zhang Q, et al. Changes in immune parameters seen in Gulf War veterans but not in civilians with chronic fatigue syndrome. Clin. Diagn. Lab. Immunol. 1999;6:6–13. doi: 10.1128/cdli.6.1.6-13.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]


