Abstract
The authors conducted an extensive search for published works concerning healthcare utilization and mortality among Gulf War veterans of the Coalition forces who served during the1990–1991 Gulf War. Reports concerning the health experience of US, UK, Canadian, Saudi and Australian veterans were reviewed. This report summarizes 15 years of observations and research in four categories: Gulf War veteran healthcare registry studies, hospitalization studies, outpatient studies and mortality studies. A total of 149 728 (19.8%) of 756 373 US, UK, Canadian and Australian Gulf War veterans received health registry evaluations revealing a vast number of symptoms and clinical conditions but no suggestion that a new unique illness was associated with service during the Gulf War. Additionally, no Gulf War exposure was uniquely implicated as a cause for post-war morbidity. Numerous large, controlled studies of US Gulf War veterans' hospitalizations, often involving more than a million veterans, have been conducted. They revealed an increased post-war risk for mental health diagnoses, multi-symptom conditions and musculoskeletal disorders. Again, these data failed to demonstrate that Gulf War veterans suffered from a unique Gulf War-related illness. The sparsely available ambulatory care reports documented that respiratory and gastrointestinal complaints were quite common during deployment. Using perhaps the most reliable data, controlled mortality studies have revealed that Gulf War veterans were at increased risk of injuries, especially those due to vehicular accidents. In general, healthcare utilization data are now exhausted. These findings have now been incorporated into preventive measures in support of current military forces. With a few diagnostic exceptions such as amyotrophic lateral sclerosis, mental disorders and cancer, it now seems time to cease examining Gulf War veteran morbidity and to direct future research efforts to preventing illness among current and future military personnel.
Keywords: Persian Gulf Syndrome, Gulf War Syndrome, veterans
1. Introduction
(a) The enigma: studying poorly defined outcomes and exposures
How does one approach epidemiological questions when neither the outcomes in question nor the alleged associated exposures are well-defined? Such was often the challenge for epidemiologists in the mid-1990s when returning veterans of the 1990–1991 Gulf War began complaining of diseases and unexplained symptoms that they attributed to war exposures. Encouraged by news reporting, legislature inquiries and Internet communications (Wheelwright 2001), veterans wondered if their post-war ailments were related to unusual Gulf War exposures. Initially, Gulf War veterans' health concern were very diverse, ranging from the very subjective, such as unusual fatigue or difficulty sleeping, to the more concrete and verifiable such as increased deaths or cancer. The veterans demanded to know whether a large array of unusual war exposures, most of which were very poorly documented, might have been responsible for any excess morbidity or mortality among the nearly one million service men and women who participated in the war. This is a review of how epidemiologists have examined healthcare and mortality data in investigating these questions.
(b) A search for causes through a reductionistic approach
As is recorded in numerous previous reports (Korenyi-Both et al. 1992; Magill et al. 1992; Defense Science Board 1994; Institute of Medicine 1995; Institute of Medicine. Committee to Review the Health Consequences of Service During the Persian Gulf War 1996), the list of possible Gulf War-related illness outcomes and alleged exposures were myriad (table 1). As objective data for many of the disease outcomes and most of the Gulf War-related exposures were not available, epidemiologists often opted to embrace a reductionism approach in studying the veterans. In many of the first epidemiological studies, Gulf War service (serving one or more days in the Gulf War theatre (1991a) during the conflict) was used as a gross exposure variable in examining data that were routinely electronically captured (especially hospitalizations and deaths) and thus thought to be less subject to various biases. It was envisioned that should Gulf War service be found a risk factor for one of these more objective health outcomes, more exposure-specific studies would follow examining such an outcome for causal associations. Hence, reducing the numerous, poorly documented exposures to such a single Gulf War service variable was the strategy embraced in many of the studies of healthcare utilization and mortality we review here. It is important to note that Gulf War service was determined via an administrative process (Gray et al. 1996). Mortality studies have shown the classification to have approximately 5% misclassification error (H. Kang, personal communication 2005).
Table 1.
Potential Gulf War exposures and alleged associated medical outcomes. (Save for where indicated below, quality data were not available to examine these exposures or outcomes.)
| potential Gulf War exposures | alleged associated outcomes |
|---|---|
| anthrax vaccine | amyotrophic lateral sclerosisa |
| antimalarials | birth defectsb |
| biological weapons | cryptic bacteria in urine |
| botulism vaccine | birth defects among children |
| chemically resistant agent paint | cancera |
| chemical weapons exposure at Khamisiyahc | chronic fatigue syndrome |
| ciprofloxacin | increased unexplained other symptom-based illnesses |
| contaminated water | increased deathsb |
| contaminated food | increased miscarriages |
| diesel fuel | Mycoplasma fermentans infections |
| fine sand | multiple chemical sensitivity |
| immune globulin | pain upon sexual intercourse |
| meningococcal vaccine | post-traumatic stress disorder |
| microwaves | unusual rashes |
| oil well firesc | |
| plague vaccine | |
| pesticides or repellants | |
| psychological stressors | |
| pyridostigmine bromide | |
| sand flies | |
| solvents | |
| typhoid vaccine |
Although not initially available, these outcome data were later assembled from multiple data sources.
Data available for study.
Although not initially available, exposure data were later modelled from other extant Gulf War era data sources.
(c) Review methods
This review's objective was to summarize the large body of epidemiological work concerning the healthcare utilization and mortality of Gulf War veterans. The authors used PubMed searches, expert panel reports, Current Contents, Reports to Congress, a topical Gulf War veteran bibliography with 5520 references (Henry & Gray 2001), conference proceedings and personal contacts with knowledgeable investigators to identify published research and ongoing research (as of August 2005) relevant to the review objective.
Research findings are summarized in four areas: Gulf War veteran healthcare registry studies, hospitalization studies, outpatient studies and mortality studies. As an accompanying report reviews reproductive outcomes (Doyle et al. 2006), we have not included them here.
2. Healthcare registry studies
(a) The genesis of Gulf War veteran health registries
As alleged Gulf War associated illnesses reporting was diverse and exposure and outcome data were lacking, first the United States (Joseph & The Comprehensive Clinical Evaluation Program Evaluation Team 1997; Murphy 1999), later the United Kingdom (Coker et al. 1999) and then Canada (Robinson 1995) created health registries for Gulf War veterans. Recently, Australia has similarly conducted comprehensive health evaluations of their veterans but in addition also studied a non-deployed comparison group (Australian Department of Defence et al. 2003).
Health registries provided a means for the collection of both exposure and health outcome data (table 2). In each registry, systematic clinical examinations were conducted and detailed exposure and morbidity questionnaires were administered (Gray et al. 2004). Where illnesses or symptoms were unexplained, veterans were referred to specialists for more comprehensive evaluations. Gulf War veteran health registries provided a means of healthcare delivery for veterans as well as permitted the examination of self-reported exposures for possible association with disease outcomes. While leading scientists helped design and guide the health registries (Institute of Medicine 1997; Institute of Medicine: Committee on the Evaluation of the Department of Defense Comprehensive Clinical Evaluation Program 1997) it is important to note that, with the exception of the Australian effort, they were not designed with controlled research in mind.
Table 2.
Gulf War veteran health registry evaluations. (Data adapted from Gray et al. 2004.)
| registry name | sponsor | start date | number of veterans evaluated | number deployed |
|---|---|---|---|---|
| Persian Gulf Veterans' Health Registry | United States Department of Veterans Affairs | August 1992 | 86 463 | |
| Comprehensive Clinical Evaluation Program | United States Department of Defense | June 1994 | 58 596 | 697 000 |
| Gulf War Medical Assessment Programme | United Kingdom Ministry of Defence | July 1993 | 3000 | 53 000 |
| Canadian Gulf War Registry | Canada Department of National Defence | January 1995 | 213 | 4500 |
| Australian Gulf War Veterans' Health Study | Australian Department of Veterans Affairs | July 2001 | 1456 | 1873 |
Detailed descriptions of health registry methodology have been previously reported (Coker 1996; Graham 1996; Joseph & The Comprehensive Clinical Evaluation Program Evaluation Team 1997; Coker et al. 1999; Murphy et al. 1999; Department of Veterans Affairs 2002; Australian Department of Defence et al. 2003) In brief, veterans were given considerable opportunity to participate and to be clinically evaluated in these registries. Toll-free number appointment access, transportation and priority healthcare access were often provided. During their medical evaluations, veterans were asked to complete questionnaires that captured detailed demographic, health risk behavior, deployment exposures, self-reported symptoms and morbidity data. While initially criticisms were made that the US registries were a waste of government funding (Canavan 1994) in general, their value as potentially hypothesis generating was embraced since they had the potential of uncovering serious pathology in veterans reporting multiple symptoms.
It is important to note that not all veterans who contacted the registries, sought or permitted medical evaluations. As of July 31, 2001, 16 721 (28.8%) of the Department of Defense's (DoD's) 57 953 registry participants had declined clinical evaluations (DoD Health Affairs, CCEP monthly report, July 2001). However, many veterans did seek an evaluation. In fact, as of June 2003 when Gulf War veteran registry programs had essentially ceased or transitioned, 149 728 (19.8%) of 756 373 US, UK, Canadian and Australian Gulf War veterans (table 2) had received clinical examinations under these systematic protocols.
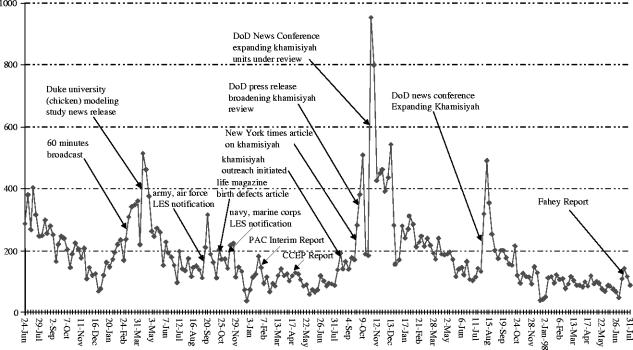
Health registry participation seemed to be temporally associated with news reports or popular literature stories of Gulf War veteran illnesses (figure 1; Department of Veterans Affairs 2002). Certainly some registry participation was in anticipation of disability claims (Wheelwright 2001). However, many participants were quite ill. Smith et al. examined the hospitalization experience of US registry participants and concluded that US Gulf War registry participants were sicker than non-participants, even before the registries were established (Smith et al. 2004b). Overall, US registry participants were more likely to: have served with the Army Reserve or National Guard, to be ≥30 years old and female, to have served near oil well fires and possibly been exposed to munition destruction plumes at Khamisiyah, Iraq in March 1991 and to have served in the Gulf War theatre during armed combat (Gray et al. 1998b; Smith et al. 2002b).
Figure 1.
Weekly number of new toll-free hotline referrals to the US Department of Defense Comprehensive Clinical Evaluation Program (CCEP), (24 June 1994 to 31 July 1998). Adapted from Department of Veterans Affairs (2002). LES, Leave and earning statements; PAC, Presidential Advisory Committee on Gulf War Veterans' Illnesses.
(b) Registry studies and findings
As the healthcare registries collected data regarding the exposures and outcomes in question (table 1), they have been the subject of numerous reports. Registry data have been used in clinical series, cross-sectional studies, case–control studies and cohort studies.
The first peer-reviewed Gulf War veteran registry report was published by Joseph et al. in 1997 as a case series (Joseph & The Comprehensive Clinical Evaluation Program Evaluation Team 1997). The report's summary of the evaluation of the first 20 000 DoD registry participants at 184 medical institutions is consistent with the findings from other US, UK, Canadian and Australian registry participants evaluations (Robinson 1995; Joseph & The Comprehensive Clinical Evaluation Program Evaluation Team 1997; Coker et al. 1999; Murphy 1999; Lee et al. 2001; Department of Veterans Affairs 2002; Smith et al. 2002b; Australian Department of Defence et al. 2003; Lee et al. 2005a). Gulf War veterans frequently self-reported symptoms of fatigue, headache, memory problems, sleep disturbances, skin rash, joint pain, dyspnoea, cough and other non-specific symptoms (table 3). Joseph et al. reported that the many varied diagnoses captured during the evaluations were not unexpected and revealed no evidence for a new deployment-associated syndrome.
Table 3.
The most common symptoms reported by US registry participants as of September 1999. (Adapted from Department of Veterans Affairs 2002.)
| per cent of veterans with symptoma | |||
|---|---|---|---|
| symptoms | initial VA registry (n=49 079) | revised VA registry (n=21 306) | DoD CCEP (n=32 876) |
| muscle and joint pain | 16.2 | 39.2 | 51.8 |
| fatigue | 21.0 | 24.1 | 46.6 |
| headache | 18.3 | 27.9 | 40.8 |
| memory problems | 14.2 | 24.1 | 36.2 |
| skin rash | 18.5 | 25.3 | 30.0 |
| sleep disturbances | 5.6 | 13.5 | 35.9 |
| diarrhoea | 4.6 | 14.0 | 25.5 |
| shortness of breath | 8.0 | 10.2 | 23.0 |
| abdominal pain | 2.7 | 4.6 | 20.8 |
| no complaint | 12.3 | 8.6 | 6.4 |
The percentage of reported symptoms varied among registries because only three symptoms were captured in the initial VA registry compared to 10 symptoms in the revised VA registry and a 16-item symptom checklist in the CCEP. VA, Department of Veterans Affairs; DoD, Department of Defense; CCEP, Comprehensive Clinical Evaluation Program.
Later researchers observed that the prevalence of self-reported symptoms among US registry participants increased over time (Murphy et al. 1999). Kroenke et al. argued that such latency of symptoms (often up to a year after returning from the Gulf War) and the lack of association with self-reported exposures argued against illness among Gulf War veterans being caused by toxic exposure (Kroenke et al. 1998). Hallman et al. studied symptom patterns among registry participants and concluded that while the prevalence of self-reported symptoms among registry participants was greater, their symptom patterns did not differ from those detected in the general US population (Hallman et al. 2003). While efforts to find clear associations of symptoms or objective pathology with self-reported specific Gulf War exposures have failed, Boyd et al., through a supplemental mail survey of US registry participants, determined that high symptom reporting was closely associated with belief in chemical or biological warfare exposure, war stressors and negative life events after the war (Boyd et al. 2003).
Being more objective than self-reported symptoms, registry diagnoses have often been examined with the hope that they might shed light on the cause of illnesses among Gulf War veterans. It is important to note that many veterans were given no diagnoses after registry evaluations. Considering the two US registries, 34 528 (27%) of the 122 973 registry participants were evaluated without illness (Gray et al. 2004). This reflects the large proportion of participants who had no health complaints but just wanted to participate. A UK registry review reported that 25% of the evaluated were considered well (Lee et al. 2002). Among those given diagnoses, the most common disease classifications were mental disorders, respiratory disorders, skin conditions and musculoskeletal diseases (Gray et al. 1998b, 2004; Department of Veterans Affairs 2002). These diagnoses have been used to study subsets of registry participants for rheumatological diagnoses (Erickson et al. 1998; Escalante & Fischbach 1998; Grady et al. 1998), signs, symptoms and ill-defined conditions (Roy et al. 1998), symptoms consistent with chronic fatigue syndrome (Kipen et al. 1999), reproductive morbidity (Murphy et al. 1997), mental health diagnoses (Ikin et al. 2004; Lee et al. 2005b) and neurological conditions (Newmark & Clayton 1995). While mental health conditions such as post-traumatic stress disorder (PTSD; Ikin et al. 2004) were common (reviewed elsewhere in this volume), like the Joseph et al. report (Joseph & The Comprehensive Clinical Evaluation Program Evaluation Team 1997), these specific studies failed to identify conditions that were unexpected or would explain a new disease entity related to war exposures.
Very similar to the Gulf War veterans who were studied in cross-sectional or cohort studies (Gray et al. 1999a; Kang et al. 2000; Gray et al. 2002b), registry participants reported a high prevalence of Gulf War-related exposures (table 4; Kroenke et al. 1998; Department of Veterans Affairs 2002; Stuart et al. 2002; Boyd et al. 2003; Kelsall et al. 2004). As these exposures were often correlated and the health registries had no comparison groups of non-exposed veterans, it was difficult to use the registry exposure data in evaluating exposures for possible associations with increased symptoms among Gulf War veterans. The self-reported exposures could not be verified and were subject to recall and reporting biases (Joellenbeck et al. 1998). Even so, when an Australian team was commissioned to conduct systematic health evaluations of their Gulf War veterans they added a non-Gulf War exposed group. Using self-reported data they found increased symptom reporting was associated with immunizations, pyridostigmine bromide tablets, anti-biological warfare tablets, pesticides, insect repellants, being in a chemical weapons area and stressful military services experiences (Kelsall et al. 2004).
Table 4.
Self-reported exposure histories of US registry participants as of September 1999. (Adapted from Department of Veterans Affairs 2002. CARC, chemical agent resistant coating; VA, Department of Veterans Affairs; DoD, Department of Defense; NR, not recorded in Comprehensive Clinical Evaluation Program (CCEP).)
| per cent self-reporting exposure | ||
|---|---|---|
| potential exposure during Gulf War | revised VA registry (n=21 306) | DoD CCEP (n=32 876) |
| diesel and other petrochemical fumes | 90.9 | 89.5 |
| passive smoking | 89.1 | 85.4 |
| skin exposure to fuel | 74.8 | NR |
| burning trash/faeces | 77.3 | NR |
| smoke from oil well fires | 75.5 | 70.6 |
| ate food other than provided by military | 70.1 | 66.0 |
| pesticides (creams, sprays) | 68.5 | 67.6 |
| smoke from tent heaters | 70.6 | 70.0 |
| pyridostigmine bromide pills | 69.4 | 78.9 |
| other paints and solvents | 53.7 | 56.0 |
| anthrax vaccination | 53.0 | 49.6 |
| CARC paint | 36.5 | 44.9 |
| microwaves | 32.8 | 28.9 |
| ate or drank contaminated food | 35.3 | 23.5 |
| bathed in water not provided by military | 29.9 | 30.2 |
(c) Value and limitations of registry data
While registry data have often been examined by research teams, registry data are limited in their research value. Registry participants were self-selected. Participation was likely influenced by the news media, the desire for health evaluations and the possibility for compensation. Registry participants did not well represent the population of deployed Gulf War veterans (Gray et al. 1998b; Smith et al. 2002b). In general registry data are without controls so only internal comparisons can be made (eg. the sick vs. those without diagnoses). With these limitations, the research value of the healthcare registry data seems less than that of controlled epidemiological study data we review below. However, registry data were valuable in that they identified Gulf War veterans most likely to seek evaluations and demonstrated that most unexplained illnesses were symptom-based. Registry data were also important for what they failed to do. For instance, although exhaustively examined, registry data failed to implicate a specific Gulf War exposure or group of exposures as aetiologic. They also failed to support the notion that Gulf War veterans were suffering from of a unique group of symptoms or signs, in other words a ‘Gulf War Syndrome’.
3. Hospitalizations studies
US DoD and Department of Veterans Affairs (VA) hospitals in the United States and various fixed foreign settings record admission records in an electronic format. Beginning in October 1988, the US Navy (includes Marine Corps), Army and Air Force adapted a common electronic hospitalization record data structure that permitted hospitalization comparisons across services. The VA has been capturing hospitalization data in an electronic format since 1970. As far as the authors are aware only US and Saudi Arabia's (Gackstetter et al. 2005) servicemen's hospitalizations have been captured in administrative electronic data bases. No similar Gulf War era data are available to study the morbidity of Gulf War veterans from other countries in the 34-country Coalition. While such data bases were designed for administrative purposes and they have limitations (Kuller 1995; Riegodedios et al. 2005), these hospitalization data bases have often proven valuable in epidemiological studies.
(a) War zone hospitalizations
In the Gulf War theatre (1991a) ill US military personnel were evaluated at various field medical facilities, including field hospitals and hospital ships. Some also received treatments at a hospital in Saudi Arabia (Smith et al. 2004a). If their illnesses or injuries required specialized treatment, veterans were evacuated to fixed DoD and VA facilities in Germany and the United States. While administrative electronic records are available from encounters at these fixed facilities, until recently, electronic data were not available for the medical encounters that occurred in the Gulf War theatre in mobile units. Such health records were only captured on paper and due to the rapid nature of the deployment that was not without difficulty (Pohlmann 1991).
After reviewing paper medical records, Wintermeyer and colleagues (Heier et al. 1993; Wintermeyer et al. 1994, 1996) published several descriptive accounts of their field hospital's activity during the periods before and after the fighting. They reported that hospitalization rates fluctuated with the combat activity. They comment that the highest rate of cases occurred during the ground war and Iraqis, not Coalition military personnel, accounted for 82% of admissions during that time.
Recently, the DoD conducted an extensive search for paper records of US military hospitalizations that occurred ‘in-theatre’ during the Gulf War. Record reviewers identified 22 444 in-theatre admissions from 44 Army hospitals, 15 Air Force hospitals and 4 Navy hospitals. They also identified 5563 evacuated admissions to hospitals in Europe (Smith et al. 2004a). Considering the Gulf War period as August 1, 1990 to July 31, 1991, the record reviewers estimated that the 28 000 records accounted for approximately 75% of the total war zone admissions that occurred during the war. These paper records were electronically coded in a fashion similar to that which is used in fixed hospital admissions. To these data, Smith et al. (2004a) added exposure modelling data from oil well fire smoke and munitions destruction at Khamisiyah, Iraq. In their multivariable logistic regression modelling, they found that enlisted personnel who were female, White, Reservists, Army and healthcare workers or supply handlers had the highest odds of in-theatre hospitalization during the war. They saw no increased risk for hospitalization among those exposed to oil well fire smoke or possibly exposed nerve agent plumes at Khamisiyah. The most frequent in-theatre diagnoses were similar to the hospital diagnoses that occurred among Gulf War veterans after the war. The authors also stratified hospitalizations by occupational group and recognized no unusual pattern of diagnoses. Hence, the hospitalization risk factor and diagnoses findings were strikingly similar to those found in studies of post-war hospitalizations that occurred in the United States.
(b) Hospitalizations after the war
Because electronic data were available, a number of large, comprehensive US Gulf War veteran post-war hospitalization analyses have been performed (table 5; Gray et al. 1996, 1999b, 2000; Knoke & Gray 1998; Knoke et al. 1998; Dlugosz et al. 1999; Smith et al. 2000, 2002a, 2003, 2004a,d; Gackstetter et al. 2005). The first controlled study was a comparison of DoD hospitalizations between 547 076 Gulf War veterans and 618 335 non-deployed era veterans during the period August 1991 through September 1993 (Gray et al. 1996). Hospitalizations for three time periods were examined for any cause and diagnoses in 14 broad diagnostic categories. Gulf War veterans were found to have an elevated risk for certain types of hospitalizations, but these increases were likely due to deferred medical care, a post-war baby boom or mental illness previously recognized as war sequelae. A related study of veterans hospitalizations in the VA hospital systems and California hospitals also failed to demonstrate unexpected diagnoses among Gulf War veterans (Gray et al. 2000). These works were accompanied by similar controlled examinations of hospitalizations for a group of 77 diagnoses thought most likely to occur during the emergence of a new unexplained illness (Knoke & Gray 1998), evaluations of risk for the most common cancer among young males (testicular cancer) (Knoke et al. 1998), comprehensive evaluations of mental health diagnoses (Dlugosz et al. 1999), searches for chronic effects of possible sub-clinical exposure to nerve agents during munition destruction (Gray et al. 1999b; Smith et al. 2003), evaluations of risk for fibromyalgia, systemic lupus erythematosus and amyotrophic lateral sclerosis (ALS), (Smith et al. 2000) chronic effects of oil well fire smoke exposure (Smith et al. 2002a), combat-exposure effects among Saudi Gulf War veterans (Gackstetter et al. 2005), evaluations of the hospitalization experience of health registry participants (Smith et al. 2004b) and comparisons of Gulf War veterans with other US veterans who served in other conflicts (Blood & Aboumrad 2001; Smith et al. 2004d).
Table 5.
Summary of US Gulf War veteran hospitalization studies. (All were retrospective cohort designs. GWV, Gulf War veterans; NDV, non-deployed veterans of the same era.)
| authors and year | description |
|---|---|
| Gray et al. 1996 | compared DoD hospitalizations among 547 076 GWVs and 618 335 NDVs for 2 years after the war. Unconditional logistic regression modelling was used. GWVs at increased risk for mental health diagnoses. No evidence of unexplained hospitalizations found. |
| Knoke & Gray 1998 | compared DoD hospitalizations among 552 111 GWVs and 1 479 751 NDVs 1 August 1990 through 1 April 1996 for one or more of 77 diagnoses thought by the CDC to best describe an unexplained illnesses. Cox proportional hazards modelling was used. No evidence of unexplained illness detected. |
| Knoke et al. 1998 | examined DoD hospitalizations among 517 223 male GWVs and 1 291 323 male NDVs 1 August 1990 through 31 March 1996 for testicular cancer diagnoses. Cox proportional hazards modelling was used. At 4 years, the cumulative risks for the two groups were not different. |
| Dlugosz et al. 1999 | examined 30 539 initial DoD mental health hospitalizations (2 August 1990–31 July 1991) among 1 805 775 regular active duty personnel for the effects of the Gulf War. Cox proportional hazards modelling was used. GWVs were at increased risk for acute reactions to stress. GWV men who served in ground war combat occupations were at higher risk for alcohol-related disorders. |
| Gray et al. 1999b | examined DoD hospitalizations among 349 291 US Army GWVs from March 1991 to September 1995. Cox proportional hazards modelling was used. Estimates of possible exposure to fumes from nerve agent destruction at Khamisiyah, Iraq (March 1991) were estimated through geographical information system modelling. No suggestion that GWVs were suffering post-war morbidity from sub-clinical nerve agent exposure. |
| Gray et al. 2000 | examined GWVs and NDVs hospital admissions in DoD, VA and California Office of Statewide Health Planning and Development hospital systems (CA) during the years 1991–1994. Proportional morbidity ratios of hospitalization discharge diagnoses were calculated. GWVs experienced proportionally more hospitalizations for fractures and bone and soft-tissue injuries (DoD and CA), various diseases of the respiratory (including asthma) and digestive systems (VA) and diverse symptom diagnoses (VA). |
| Smith et al. 2000 | examined DoD hospitalizations among 551 841 GWVs and 1 478 704 NDVs during 1 October 1988–31 July 1997 for systemic lupus erythematosus, amyotrophic lateral sclerosis or fibromyalgia diagnoses. Cox proportional hazard modelling was used. Study data did not support Gulf War service and disease associations. |
| Blood & Aboumrad 2001 | examined DoD hospitalization rates among 11 894 enlisted US Marine Vietnam veterans with 10 878 GWVs. Age-adjusted hospitalization rates were calculated. GWVs had lower hospitalization rates but a higher proportion of admissions for musculoskeletal disorders. |
| Smith et al. 2002a | examined DoD hospitalizations (1 August 1991–31 July 1999) among 405 142 US GWVs exposed to oil well fire smoke during the war. Exposures to smoke particulate matter were based on meteorologic data, diffusion modelling and troop location data. Cox proportional hazards modelling was used. Study data did not suggest that GWVs were suffering post-war morbidity due to oil well fire smoke exposures. |
| Smith et al. 2003 | the authors used revised nerve agent fume exposure modelling (Khamisiyah, Iraq) to reexamine DoD hospitalizations among 418 072 US GWVs from 10 March 1991 to 31 December 2000. Cox proportional hazards modelling was used. GWVs were found to have an increased risk of cardiac dysrhythmias (risk ratio=1.23, 95% confidence interval (CI)=1.04–1.44). No other chronic disease associations were found. |
| Smith et al. 2004a | the authors examined data from 28 027 US GWV admissions that occurred during 1 August 1990–31 July 1991 in the Gulf War theatre. Unconditional logistic regression modelling was used. Risk factor profiles and most frequent diagnoses were very similar to those recorded in post-war hospitalizations. |
| Smith et al. 2004b | DoD hospitalizations were compared for 69 189 GWV health registry participants and 477 333 non-participants. Registry participants were 1.43 times more likely to have a post-war hospitalization. |
| Gackstetter et al. 2005 | examined the Saudi hospitalization experience of 15 612 Saudi National Guard soldiers during the period 1 January 1999–31 December 1999. 8342 of the soldiers were exposed to combat at Al Khafji during the ground war. Cox proportional hazards modelling was used. Combat-exposed veterans had an increased risk of hospitalization (risk ratio (RR)=1.80, 95% confidence interval (CI)=1.25–2.59) but no unusual patterns of diagnoses. |
| Smith et al. 2004d | examined US DoD hospitalizations for 455 465 GWVs, 249 047 veterans of Southwest Asia after the Gulf War and 44 341 Bosnia veterans after their deployment to 31 December 2000. Cox proportional hazards modelling was used. Compared to GWVs personnel deployed to Southwest Asia were at increased risk for hospitalization (hazard ratio=1.05; 95% confidence interval=1.02–1.08). Bosnia veterans at the least risk. Data did not support unique post-war morbidity among GWVs. |
Considering all hospitalizations, Gulf War veterans have been at increased risk of musculoskeletal disorders, multi-symptom conditions, mental health disorders and injuries (Gray et al. 1996, 2000; Dlugosz et al. 1999). However, these findings have been consistent with the experience of other veteran groups, our understanding of the stressors of war or observations that deployed veterans were more often risk takers (Hobfoll et al. 1991; Dlugosz et al. 1999; Bell et al. 2000, 2001). In some ways, Gulf War veterans have been better off than other veterans groups. Gulf War veterans have had fewer hospitalizations than veterans of the Vietnam War (Blood & Aboumrad 2001) and veterans who deployed to the Gulf war theatre after active hostilities ended (Smith et al. 2004d).
While these hospitalization studies, due to their large size, have had tremendous power to distinguish an usual, even rare Gulf War morbidity effect, they have not done so. There have been some interesting Gulf War-associated findings; however, considering the numerous modelling constructs, these findings could be simply explained by chance alone. One such finding is the slight increase in risk for some Gulf War veterans to be hospitalized with cardiac dysrhythmias (risk ratio (RR)=1.23; Smith et al. 2003). These veterans were possibly exposed to sub-clinical doses of nerve agent munition fumes. While interesting, such a latent chronic effect of a sub-clinical nerve agent exposure would be in contrast to what we understand about this class of chemicals and seems unlikely (Perrotta 1996; Institute of Medicine: Committee on the Evaluation of the Department of Defense Comprehensive Clinical Evaluation Program 1997; Brown 2006).
Recently, Gulf War veterans' hospitalization experiences have been examined in concert with cancer registries. Australian investigators evaluated cancer incidence among Gulf War veterans and non-deployed era veterans (Sim et al. 2003). They linked the personal identifiers from 1833 Gulf War veterans and 2847 non-deployed veterans to the Australian national cancer registry data from 1 January 1991 to 31 December 1998. The authors detected no difference in cancer incidence between the two groups. Macfarlane et al. (2003) studied 51 721 UK Gulf War veterans and 50 755 UK matched era veterans for incident cancers in the UK's National Health Service (NHS) central register. The team found no excess risk of cancer among Gulf War veterans. Levine et al. (2005) linked US cancer registries data from the District of Columbia and New Jersey with the identifiers of 1.4 million Gulf War era veterans. The years 1991–1999 were examined. They found Gulf War veterans to be at increased risk for testicular cancer, citing a crude proportional incidence ratio of 3.05 (95% CI=1.47–6.35). However, this increase is very likely due to ascertainment bias as Gulf War veterans were referred in large numbers to the government hospitals in these regions for health registry evaluations (Gray 2005). Hospitalization data have also been used to examine reproductive and neurologic outcomes. However, as these diagnoses are the subject of accompanying reviews, we will not further discuss their studies here (see Doyle et al. 2006; Rose & Brix 2006).
(c) Value and limitations of hospital data
The hospitalization studies of Gulf War veterans are remarkable for their large size and large number of outcomes. Such data permitted extensive multivariable modelling and granted researches tremendous power to detect small effects. Smith et al.'s (2004b) recent study of hospitalizations among DoD registry participants is a good example. The modelling of 73 218 hospitalizations among 546 522 veterans over nearly a 3 year period afforded the opportunity to examine 14 covariates yielding 34 unique odds ratios in a single model. Hospitalization data are further valuable in that they give researchers an opportunity to examine outcomes over time. Hence, Cox proportional hazards modelling was often used in these studies (table 5).
However, hospitalization data have a number of limitations. They are greatly influenced by the administrative needs that give them origin. Knoke et al. (Knoke & Gray 1998) discovered this in their work. When evaluating a group of non-specific diagnostic codes thought most likely to be used to record hospitalization for unexplained illnesses, they discovered a marked increase in risk among Gulf War veterans. An audit of a sample of hospital paper records revealed the excess was entirely due to administrative hospitalizations in support of the DoD's healthcare registry. Similarly, hospital outcomes can be greatly influenced by nosology. Hospital diagnostic coding is dynamic and the coders frequently receive guidance that over time alters how coders would record hospitalization diagnoses for similar patients. This is particularly true in civilian hospitals, where diagnostic codes are strongly linked to insurance claims.
4. Outpatient studies
Quality outpatient electronic data were only available beginning in 1996 from the US Veteran's Administration (VA; Boyko et al. 2000) and 1999 (DoD) when most of the Gulf War era cohort was no longer eligible for healthcare. Hence, studies of outpatient morbidity have largely been paper record based.
(a) War zone ambulatory care
Medical personnel conducted several surveys of US military personnel serving in the Gulf War theatre before the fighting began. Richards et al. (1993) surveyed 2598 US personnel stationed in Saudi Arabia (September–December 1990), finding that respiratory symptoms were quite common. Participants often complained of cough (43.1%), sore throat (34.4%) and runny noses (15.4%). In a separate survey, Hyams et al. (1991) similarly studied 2022 soldiers serving in Saudi Arabia during late 1990. After only two months of service in theatre, many reported having had diarrhoea (57%) and 20% reported that the diarrhoea kept them from their work. US shipboard personnel also complained of respiratory and diarrhoeal disease symptoms (Paparello et al. 1993). While perhaps not as common a problem as in previous wars (Blood & Aboumrad 2001), Gulf War veterans were markedly affected by infectious diseases (Hyams et al. 1995; Hyams 1999).
Ambulatory care records in the Gulf War theatre are sparse. Most reports are descriptive. Hines summarized 15 401 US outpatient clinical visits that occurred from November 1990 to February 1991 (Hines 1993). Considering all visits for both male and female, orthopaedic problems (30.3%), respiratory complaints (24.9%) and dermatological conditions (13.9%) were most prevalent. In other reviews, injuries and respiratory complaints were most common (Shaw et al. 1991; Wasserman et al. 1997).
Hines (1992) and Murphy et al. (1997) considered US ambulatory visits by women and concluded that women soldiers occasionally need gynaecological care but in general, in-theatre medical care was adequate. However, it was felt that future studies of deployed gender-specific morbidity should be performed.
Before the fighting began, Hyams et al. (1995) conducted surveillance among 40 000 Marines stationed in northeastern Saudi Arabia. They documented waves of gastroenteritis and acute respiratory disease that were associated with the eating of local fruits and vegetables (gastroenteritis) or the sudden mixing of troops (respiratory infections). A military field laboratory established in Saudi Arabia at the beginning of the deployment was very important in understanding these outbreaks (Hyams et al. 1993).
(b) Value and limitations of ambulatory care data
Save for tedious archived medical record reviews (Araneta et al. 1997; Dlugosz et al. 1999), the availability of ambulatory care data for Gulf War veterans is thought to be poor. However, the recent policies of electronically capturing DoD and VA outpatient data holds much promise for future epidemiological study.
5. Mortality studies
If one considers the spectrum of alleged Gulf War-associated morbidity (table 1), perhaps the most objective outcome to study is mortality. Administratively death data are captured by various systems and scrutinized for their causes. While Gulf War veteran mortality studies have been relatively few (table 6) ascertainment of mortality data is thought to be excellent and, compared to other medical outcomes, unequal in veracity.
Table 6.
Descriptions of published Gulf War veteran mortality studies during the post-war period.
| authors and year | study design and country | description |
|---|---|---|
| Kang & Bullman 1996 | Cohort, United States | a study of post-war mortality through 30 September 1993 among 695 516 Gulf veterans and 746 291 non-Gulf War veterans. 1765 deaths among the Gulf and 1729 deaths among non-Gulf veterans were compared and analysed. |
| Macfarlane et al. 2000 | Cohort, United Kingdom | a study of post-war mortality from 1 April 1991 to 31 March 1999 among 53 462 Gulf veterans and an equal number of non-Gulf veterans. 395 deaths among the Gulf and 378 among the era cohort were compared and analysed. |
| Kang & Bullman 2001 | Cohort, United States | further update of the US Gulf veteran mortality study through December 1997. A total of 10 424 deaths in 6.5 year post-war period were analysed by their deployment status. |
| Sim et al. 2003 | Cohort, Australia | a study of post-war mortality from 1 January 1991 to 31 December 2000 among 1833 Gulf veterans and 2848 non-Gulf veterans. 20 deaths among the Gulf and 23 deaths among non-Gulf were studied. |
| Defence Analytical Services Agency 2005 | Cohort, United Kingdom | an extension of Macfarlane et al. study through 30 June 2005. 720 deaths among Gulf and 753 deaths among era veterans were studied. |
(a) Mortality during the war
Two studies of mortality have been conducted regarding deaths during the War. In 1994, Helmkamp summarized the US battle and non-battle fatalities that occurred during the six week combat phase of Operations Desert Shield and Desert Storm, 17 January 1991 to 28 February 1991 (Helmkamp 1994). A total of 219 troops (212 men and 7 women) were killed during the six week period. Of these, 154 (148 men and 6 women) were battlefield casualties and 65 were non-battlefield casualties. Fifty-five of the 65 non-battle deaths resulted from accidental injuries; other causes included six illnesses, two suicides and one homicide. Battle and non-battle casualty rates were one of the lowest experienced by the US in any major conflict in the twentieth century.
Writer et al. studied US active duty Gulf War veterans and a comparison group of veterans who served elsewhere during the war and followed them for a longer period from 1 August 1990 to 31 July 1991 (Writer et al. 1996). During the period from 1 August 1990 to 31 July 1991, a total of 2 590 193 persons served on active duty and 688 702 were deployed to the Persian Gulf. The authors detected no evidence of excess deaths due to rapidly fatal illnesses among Gulf War veterans (standardized mortality ratio, 93.9 (95% CI=63.3–134.2)), while deaths due to all injury (standardized mortality ratio, 117.8 (95% CI=101.2–134.3)) and its subset of unintentional injury (standardized mortality ratio, 154.3 (95% CI=132–177)) were significantly elevated among Gulf veterans. An anticipated high mortality rate from a rapidly fatal illness, had there been a widespread exposure to a chemical or biological warfare agent such as sarin gas or anthrax, was not apparent among Gulf War veterans in this study.
(b) Post-war mortality studies of US, UK and Australian veterans
(i) US Gulf War veterans
Kang & Bullman conducted a cause-specific post-war mortality study of 695 516 Gulf War veterans and 746 291 non-Gulf veterans (Kang & Bullman 1996). Vital status was determined using databases of VA and the Social Security Administration (SSA). A recent study indicated that VA and SSA collectively recorded 96% of all Vietnam era veteran deaths. Causes of death were coded by a qualified nosologist who used the International Classification of Disease (1991b), 9th Revision (ICD-9) without knowing the subject's deployment status. Using Cox proportional-hazards model to adjust for confounders, Gulf veterans had an excess of adjusted overall mortality compared to non-deployed military personnel (RR=1.09; 95% CI=1.01–1.16). This excess was due to external causes of death (RR=1.17; 95% CI=1.08–1.27) rather than disease related deaths. The mortality of Gulf veterans and non-Gulf veterans were then compared separately to that of the US population. The overall mortality of both Gulf and non-Gulf veterans was less than half the expected based on the general population (standard mortality ratio (SMR)=0.44; 95% CI=0.42–0.47 and SMR=0.38; 95% CI=0.36–0.40, respectively). While troops sent to the Persian Gulf before 1 March 1991 would have been subjected to many of the potential risk factors associated with service in the Persian Gulf (pyridostigmine bromide pills, anthrax vaccine, Scud missile attacks, combat stress, etc.), those deployed after that date when the war ended would not have been similarly exposed. Comparing these two groups of Gulf War veterans, there was no difference in cause-specific mortality.
Later, Kang & Bullman further extended the follow-up period through 31 December 1997 for these veteran cohorts, adding an additional 4 years 3 months of observation (Kang & Bullman 2001). Over the entire 6.5 years of the follow-up period, May 1991–December 1997, the risk of deaths due to motor vehicle accidents was still significantly higher among male Gulf veterans than for male non-Gulf veterans. The risk of death due to disease-related causes remained lower or about the level expected among Gulf War veterans in comparison to non-Gulf veterans, males. The deficit from death due to infectious diseases contributed significantly to the lower mortality from disease-related causes. Fifty-seven per cent of deaths due to infectious diseases among Gulf War veterans and 82% of deaths due to infectious diseases among non-Gulf veterans were related to human immunodeficiency virus (HIV) infection (ICD-9, 042).
For Gulf War veterans, the risk of death from motor vehicle accidents has decreased steadily over time, from a rate ratio of 1.32 (95% CI=1.13–1.53) in the first follow-up period to a rate ratio of 1.00 (CI=0.82–1.22) in the last follow-up period. The chi-squared value (χ2=7.53) indicated a significant (p=0.0061, two-sided) decreasing trend in the risk of motor vehicle accident death with increasing time, since the Gulf War among Gulf veterans compared with non-Gulf veterans. Risk of mortality due to disease-related causes among Gulf veterans in comparison with non-Gulf veterans has steadily increased over the last three follow-up periods. In the most recent follow-up period, the risks of mortality from natural causes were almost identical in the two veteran cohorts.
(ii) British Gulf War veterans
Macfarlane et al. (2000) published a post-war mortality study of UK Gulf War veterans. All 53 462 veterans who served in the Gulf at sometime between September 1990 and June 1991 were compared to an equal number of veterans who were in the military on 1 January 1991 but did not serve in the Gulf. Selection was random but stratified to match the Gulf cohort on age (within 5 year age-group), gender, service, fitness for active service and rank.
Study subjects were identified by the UK Ministry of Defence and the ministry provided for each veteran information on age as of 1 January 1991, gender, service branch, rank and date of joining and leaving the military. Vital status was followed from 1 April 1991 to 31 March 1999 using data from the NHS Central Register, the Office for National Statistics (ONS) and provided information on the date and cause of death recorded on the death certificate or the Defence Analytical Services Agency.
A mortality rate for each cause of death was calculated based on the number of deaths and the person-years at risk and subsequently a mortality rate ratio (MRR) with 95% CI for comparison between Gulf War veterans and non-Gulf veterans. As with US Gulf War veterans, mortality from external causes was higher in the UK Gulf War veteran cohort (MRR=1.18; 95% CI=0.98–1.42), while mortality from disease-related causes was lower (MRR=0.87; 95% CI=0.67 to 1.11). The higher mortality rate from external causes was primarily due to a higher number of deaths from motor vehicle accidents, air/space accidents or deaths associated with submersion, suffocation or foreign bodies. There was no excess of deaths in the Gulf War veteran cohort recorded either as suicide or from injury from unknown cause.
Since the original publication of Gulf veteran mortality data through March 1999, several updates have been released by the UK Government including the latest one published by the Defence Analytical Services Agency (DASA) of the UK Ministry of Defence on 14 July 2005 (Defence Analytical Services Agency 2005). The Gulf veteran cohort and the comparison cohort were followed from 1 April 1991 to 30 June 2005. There were 720 deaths among the Gulf veterans and 753 deaths among control veterans. No statistical difference was observed in overall or in any of the cause-specific groups between the Gulf veterans and control veterans. Mortality rates for disease-related causes for both Gulf and control veterans have increased over the period, but the adjusted mortality ratio was 0.86 (95% CI=0.74–1.00), reflecting the natural ageing of the cohorts. The risk of deaths due to transport accidents was still higher among Gulf veterans than controls (RR=1.21; 95% CI=0.96–1.51), although since the year 2000, the rates were slightly higher among control veterans than the Gulf veterans.
(iii) Australian Gulf War veterans
Sim et al. studied whether or not male Australian Defence Force personnel who served in the Gulf War have an excess risk of death compared to non-deployed veterans (Australian Department of Defence et al. 2003). A total of 1833 veterans were identified from the Gulf War Nominal Roll and 2848 non-deployed comparison group veterans were selected and followed from 1 January 1991 to 31 December 2000 for their mortality outcomes. All cause mortality and cancer incidence rate were determined using the data from the National Death Index (NDI) and the National Cancer Statistics Clearing House (NCSCH). Cox regression modelling was used to generate risk ratios (RR). There were 20 deaths among Gulf veterans and 23 among controls resulting in RR=1.4 (95% CI=0.8–2.7). Disease-related death rate was higher in the Gulf veterans than in the controls, RR=2.2 (95% CI=0.8–5.6). A similar rate of death from external causes is observed between the two groups, RR=1.1 (95% CI=0.5–2.9).
(iv) Potential risk factors for the excess deaths from motor vehicle accidents
It seems remarkable that using different techniques and different populations, both US and UK teams found excess deaths due to accidents, especially motor vehicle accidents, among their Gulf War veterans (table 7). Several potential pathways were proposed by Bell et al. to explain the increased risk of such injury mortality following the Gulf War deployment (Bell et al. 2001). First, the increased risk may be a consequence of mental disorders such as depression and PTSD and other psychiatric conditions developed after the war. As many as 12% of Gulf War veterans who participated in a population based survey of 15 000 Gulf War veterans have met the criteria for PTSD (Kang et al. 2003). Second, physical and psychological traumas experienced during the war may result in the post-war adoption of coping behaviours such as heavy drinking that also increased injury risk. The rate of self-reported traumatic injury in the previous three months requiring medical care was higher among a sample of Iowa Gulf War veterans than non-deployed veterans (Odds ratio (OR)=1.26; 95% CI=1.02–1.55), although alcohol involvement in the accident was unknown (Zwerling et al. 2000). Moreover, a survey of 30 000 Gulf War era veterans indicated the proportion of veterans who drank alcoholic beverages was not significantly different between the Gulf veterans and non-Gulf veterans (Kang et al. 2000). Third, greater injury risk may be the indirect consequence of increased experience of ill defined diseases and symptoms reported by many returning veterans (The Iowa Persian Gulf Study Group 1997; Fukuda et al. 1998; Gray et al. 1998b, 1999a; Murphy et al. 1999). Fourth, Gulf War veterans may experience poorer survivability for a given injury event resulting in greater mortality. Finally, the process that selects certain individuals for deployment may lead to a spurious association between Gulf War deployment and injury mortality by preferentially selecting individuals who are risk takers and/or exposed to greater hazards.
Table 7.
Cause-specific mortality among US, UK and Australian veterans of the 1991 Gulf War as compared with non-Gulf War veterans, mortality rate ratios with 95% confidence intervals.
| underlying cause of death | |||||||
|---|---|---|---|---|---|---|---|
| country | study | all causes | all diseases | accidents | motor vehicle accidents | all cancers | amyotrophic lateral sclerosis |
| US veterans | Kang & Bullman, 1996 | 1.09 (1.01–1.16) | 0.88 (0.77–1.02) | 1.31 (1.14–1.49) | 0.83 (0.66–1.05) | — | — |
| Kang & Bullman 2001, male veterans | 0.95 (0.92–0.99) | 0.83 (0.78–0.89) | 1.19 (1.09–1.30) | 0.90 (0.81–1.01) | — | 0.59a (0.21–1.66) | |
| Kang & Bullman 2001, female veterans | 1.16 (0.97–1.38) | 1.02 (0.79–1.33) | 1.63 (1.09–2.45) | 1.11 (0.78–1.57) | — | — | |
| Bullman et al. 2005 | 0.97 (0.91–1.04) | 0.96 (0.86–1.07) | 1.00 (0.86–1.17) | 0.97 (0.82–1.16) | 1.94 (1.12–3.34) | — | |
| UK veterans | Macfarlane et al. 2000 | 1.05 (0.91–1.21) | 0.87 (0.67–1.11) | 1.25 (0.9–1.72) | 1.11 (0.73–1.67) | — | — |
| Defence Analytical Services Agency 2005 | 0.98 (0.88–1.08) | 0.86 (0.74–1.00) | 1.18 (0.92–1.52) | 0.95 (0.76–1.19) | 0.94 (0.50–1.76) | — | |
| Australia | Sim et al. 2003 | 1.4 (0.8–2.7) | 2.2 (0.8–5.6) | — | — | — | — |
Based on the entire Gulf War veterans and a sample of non-Gulf War veterans, adjusted for gender.
In an effort to evaluate the possible reasons for the excess deaths due to moving vehicle accidents (MVA), Kang et al. analysed data from 549 Gulf War veterans and 398 non-Gulf veterans who died from motor vehicle accidents (ICD-9, E810–E825; Kang et al. 1997). Gulf and non-Gulf veterans were compared on numerous host and external factors including age, race, gender, marital status, driver status (driver versus passenger), vehicle type, speed, alcohol and drug measures, seat belt use, nature of collision (fixed object versus moving vehicle). Data for the evaluation were obtained from the mortality study and the fatal accident reporting system (FARS). Of the 947 veterans identified as having died from MVA, 92% were on the FARS. Those who were not on FARS were veterans who died overseas. Gulf veterans who died from MVA accidents less often used seat belts, wore motorcycle helmets or made crash-avoidance manoeuvres; more often were speeding, alcohol involved, had single vehicle crash, collisions with fixed objects, rollovers, ejections and previous driving under the influence convictions. More Gulf veterans died at the scene of the accident or within one hour of medical attention. This descriptive pattern lends support to speculation that Gulf veterans being the survivors of war would perceive the degree of risk in any given situation differently from other non-war veterans and they may therefore engage in more risk-taking behaviour. Something similar has been observed in veterans of World War II, Korea and Vietnam.
(v) Cancer mortality
There has been concern about a possible link between service in the Gulf and an increased risk of cancer, particularly among those who were exposed to depleted uranium, oil well fire smoke and other petrochemical products. Mortality studies of Australia, US and UK veterans found no significant increase in the risk of death from cancer.
A cause-specific mortality study of US Gulf War veterans to date has not suggested excess deaths due to cancer in aggregate or any specific type of cancer (Kang & Bullman 1996; Kang & Bullman 2001). While over the 7 year follow-up period, from 1991 to 1997, the risk of death due to disease related causes among US Gulf War veterans in comparison to non-Gulf veterans has steadily increased, there was no significant excess of overall cancer deaths or deaths from cancer at any specific site. A similar finding was reported for UK Gulf War veterans whose vital status was followed through March 1999 (Macfarlane et al. 2000). In a more recent follow-up of the same UK veterans through June 2005, 144 deaths due to cancer were reported, while 164 deaths were reported among the era controls resulting in adjusted MRR of 0.95 (95% CI=0.76–1.19). No site-specific cancer was found to be associated with the Gulf War deployment status. Among the Australian Gulf War veterans, five deaths due to cancer were observed, while four cancer deaths were recorded among the controls. No relative mortality risk was calculated due to these small numbers.
The mortality study results were supported by a UK cancer incidence study. Among the UK Gulf veterans, there was no overall increase in incidence of cancer and neither was the incidence higher among those veterans who reported specific exposures during their deployment such as multiple vaccinations, personal use of pesticides/insecticides and depleted uranium (Macfarlane et al. 2003). In Australian Gulf veterans, the cancer incidence rate was higher than the comparison group (RR=1.5; 95% CI=0.6–3.9), but this was not statistically significant (Australian Department of Defence et al. 2003). There were too few cancers of any one type to evaluate for individual cancer type: 9 among Gulf and 10 in comparison group. There was no comparable cancer incidence study in US Gulf War veterans.
(vi) Potential nerve agent exposure and brain cancer
Bullman et al. compared the cause-specific mortality of 100 487 who were potentially exposed to nerve agent plumes from Khamisiyah with that of 224 980 unexposed US Army Gulf War veterans (Bullman et al. 2005) using a revised model of plume exposure. Vital status follow-up for each veteran began on the date the veteran left the Gulf Theatre alive and ended on the earlier of either the veteran's date of death or 31 December 2000. The risks of most disease-related mortality were similar for exposed and unexposed veterans for over 60 comparisons. However, exposed veterans had an increased risk of brain cancer deaths (RR=1.94; 95% CI=1.12–3.34). The risk was greater among those who were exposed two or more days than those who were exposed only 1 day when each group was compared separately to all unexposed veterans (RR=3.26; 95% CI=1.33–7.96 and RR=1.72; 95% CI=0.95–3.10, respectively). In addition, the results were analysed for three separate follow-up periods. The highest risk was observed during the last third observation period, 1 August 1997–31 December 2000 with a rate ratio of 3.03 (95% CI=1.34–6.82). However, caution is needed in interpreting these findings. Until quite recently there has been little evidence suggesting that sub-acute exposure to nerve agents could cause any adverse health effects (Fulco et al. 2003). However, recent animal studies reported alterations in the brain that could lead to memory loss, cognitive dysfunction and sarin induced immunosuppression (Henderson et al. 2001, 2002; Kalra et al. 2002). There is no evidence in animal studies that sarin is carcinogenic (Fulco et al. 2003). Moreover, there was little evidence that veterans possibly exposed the nerve agent plumes experienced unusual post-war hospitalization or cancer mortality when the exposure status was based on the previous DoD 1997 model (Gray et al. 1999b; Smith et al. 2003). In view of these and other animal study findings, further follow-up of this cohort should be undertaken in the future.
(vii) Amyotrophic lateral sclerosis
Two recent studies reported that US Gulf War veterans may be at increased risk for ALS, known as motor neuron disease in the United Kingdom (Haley 2003; Horner et al. 2003). An association of Gulf War service and ALS was first suggested when ALS cases began to occur in young servicemen at an age when it is not common (Karsarskis et al. 1999). ALS is a progressively fatal neurological disease characterized by a progressive loss of motor control. The peak age at onset of ALS is between 55 and 75 years old and is found more often among men than women. Haley et al. compared the number of ALS cases diagnosed between 1991 and 1998 among Gulf War veterans 45 years of age or younger with the expected number (Haley 2003). The expected number was calculated from the age distribution of the Gulf War veteran population and age-specific incidence rates of ALS estimated from the vital statistics of the general population. This study reported that over the 8 years of follow-up, 20 ALS cases were confirmed in approximately 690 000 Gulf War veterans and 17 were diagnosed before age 45 years. The study found that the incidence of ALS cases among Gulf War veterans exceeded the expectation (Poisson trend test, p=0.05) and suggested a war-related environmental trigger. A second overlapping study also reported an excess of ALS among Gulf War veterans (Horner et al. 2003). This study attempted to identify all ALS cases occurring among all Gulf War veterans who served at least one month during the Gulf War. Comparing those deployed to the Gulf theatre to those who were not deployed to the Gulf theatre, the study reported an almost twofold excess of ALS cases among those deployed (RR=1.92; 95% CI=1.29–2.84).
Although the studies were conducted with care, there still is the concern that a limitation in the study methodology could have biased the results. A differential ascertainment of ALS cases by Gulf War deployment status of veterans could have increased or decreased the risk of ALS associated with the Gulf War. A future mortality study of these cohorts should shed light on this health issue. ALS is almost always fatal and median survival time from diagnosis is an estimated 1.5–3 years. Therefore, the ALS mortality is a good surrogate for incidence. While the diagnosis of ALS may be difficult early in the disease course, the validity of the ALS diagnosis reported in death certificates is considered accurate.
A mortality study of US Gulf War veterans whose vital status was followed through 1997 did not find a rise in ALS mortality among the Gulf veterans in comparison to non-Gulf veterans (RR=0.59; 95% CI=0.21–1.66; Kang & Bullman 2001). Unless the ALS mortality risk associated with Gulf War deployment is an order of magnitude greater among the deployed, it is unlikely that either a study of UK veterans or a study of Australian veterans could provide a definite answer to this question because of its very rare annual mortality rate, especially among the age groups of Gulf War veterans (less than 0.5 per 100 000 in those aged 30–40 years).
(c) Value and limitations of mortality data
A study of mortality experience in US Gulf War veterans is considerably less problematic than a study of their morbidity. The sources used for vital status in the Australian, British and US studies should ensure fairly complete vital status ascertainment for both Gulf and non-Gulf veterans. In the first US mortality study, it was determined that vital status was ascertained at an estimated rate of 89 per cent (95% CI=83–97) with no significant differences between Gulf War and non-Gulf War veterans (Kang & Bullman 1996). Cause of death was obtained for equally high percentages for each veteran cohort, 93.7% of Gulf veterans and 93.4% of non-Gulf veterans. For a more complete ascertainment of vital status of veterans, one could use the NDI maintained by the National Center for Health Statistics, but cost likely outweighs the gain.
Another strength of the VA mortality study was substantial statistical power to detect small to moderate increased risks of cause-specific mortality. Sampling errors should also be reduced as all Gulf War veterans were used as the study group and almost half of all veterans who did not go to the Persian Gulf were used as a comparison group (Kang & Bullman 1998).
A potential limitation of the US study is that some of the non-Gulf veterans may not have been as healthy as those who were sent to the Persian Gulf as indicated by the excess deaths from HIV infection among non-Gulf veterans. Non-Gulf veterans may have included individuals who were recovering from surgery or had ailments serious enough to preclude them from being deployed but not serious enough to require their dismissal from the military. To evaluate the magnitude of this potential selection bias, Kang & Bullman compared the mortality of a group of 106 840 non-Gulf Reservists and National Guard veterans who were activated and deployed to locations other than the Persian Gulf to that of 115 478 Reserve and National Guard members who were not deployed at all (Kang & Bullman 1998). Again using the Cox proportional hazards models, there was no difference in either overall mortality or cause-specific mortality between the two groups, although the adjusted rate ratio for infectious and parasitic disease (ICD, 001–139) was 0.43 (95% CI=0.11–1.62). If there had been a significant selection bias, then those deployed would have had a significantly lower risk of cause-specific mortality than those who were not deployed. Gray et al. also reported, on the basis of history of pre-war hospitalization rates among Gulf and non-Gulf veterans, that the effect of the possible selection bias was transient and largely resolved by the conclusion of the war (Gray et al. 1998a). They concluded that military personnel, in general, are healthy and without serious chronic conditions. If they develop a chronic disease that causes a sustained reduction in their ability to perform their military duties, they are eventually separated from military service. The effect of this potential selection bias would be very limited and could not have accounted for the findings. It should be noted, however, that in the UK study this potential selection bias is not an issue since the two cohorts were matched on fitness for active service.
Another potential limitation is the reliance on death certificates rather than medical records for cause of death data. While death certificates are reliable sources for vital status ascertainment, their accuracy in recording cause of death may be variable (Engel et al. 1980; Percy et al. 1981). However, the agreement between medical records and death certificates has been reported to be good for external causes of death (1987; Boehmer et al. 2004). One additional limitation is the lack of data on non-military service related characteristics/behaviours, e.g. excessive alcohol consumption and smoking that could be risk factors for adverse health outcomes. However, such factors should be present in similar proportions in both Gulf War and non-Gulf veterans, as both joined the military prior to the Gulf War and in almost all instances deployment to the Persian Gulf area was not voluntary. A population-based survey may capture prevalent cases; however, a very large sample size (over 100 000) is necessary due to relative rarity of disease among Gulf War era veterans of generally middle age men and women. In a population based health survey of 15 000 Gulf War veterans completed in 1995/1996, only 0.7% of veterans reported having a cancer other than a skin cancer, while 0.6% of non-Gulf War veterans reported having a similar condition (Kang et al. 2000). There are several other cross-sectional surveys of US and UK Gulf War veterans and none of these studies has reported a significant increase in cancer prevalence or hospitalization rate for cancer among Gulf War veterans (Gray et al. 2000; Cherry et al. 2001). Mortality surveillance is more efficient and less expensive than incidence surveillance and is a reasonable approximation of incidence for diseases that are known to have a short survival time since diagnosis. Five year survival is just 6% for liver cancers and 13% for lung cancers (Ries et al. 1996).
6. Discussion
It seems remarkable that 15 years after the war there has been so much invested in evaluating the health of Gulf War veterans. There have been numerous expert panels assembled, many research projects commissioned, a small army of government investigators assembled, dozens of public hearings, extensive health registries established and many resultant reports. The sheer volume of published works is daunting. A PubMed search on 28 August 2005 using the keywords ‘Gulf War’ yielded 1102 citations in the medical literature and this search misses the many news stories, the expert panel reports, the legislative actions and the volumes of written material available on the Internet. In all it has been estimated that the US government alone has expended more than a billion dollars (Gray et al. 2004) in evaluating Gulf War veteran illnesses. This investment is unprecedented.
In several of the Coalition countries, this investment and the Gulf War experience has significantly influenced the collection of exposure and medical outcome data during military deployments (Hyams et al. 2002; Trump et al. 2002). For example, the US has commissioned extensive pre- and post-deployment evaluations of veterans, increased environmental samplings during deployment and given us an understanding that the health consequences of serving in combat arena can be long, profound and the cause of both mental and somatic illness. It has influenced the commissioning of the largest prospective cohort studies ever attempted, a study of more than 100 000 military personnel over 21 years (Gray et al. 2002a; Ryan et al. 2002; Smith et al. 2004c) and a study of 20 000 UK military service personnel, half of whom deployed to the 2003 invasion of Iraq. In short, comprehensive efforts are now made to aggressively prevent disease and to monitor veterans' exposures and health from their service entry to well beyond their separation from service. This reflects a major shift in thinking. Examinations of Gulf War veterans' healthcare utilization and mortality data have greatly influenced this paradigm shift.
7. Conclusions
Since returning home, Gulf War veterans have consistently reported a wide variety of health problems. As recorded in the health registries and in controlled epidemiological studies reviewed elsewhere in this volume, these health problems have caused considerable disabilities. However, in general the problems have not manifested in unusual causes of hospitalizations or mortality that might indicate a new Gulf War-specific condition. Instead, the comprehensive and very valuable studies of Gulf War veterans' healthcare utilization and mortality have provided direction towards improving the health of future military personnel who are asked to go in harms way. From these studies, we recognized that we can expect future veterans to be at increased risk for mental health disorders, multi-symptom conditions, accident-related injuries and musculoskeletal disorders.
While a number of diagnoses (e.g. cardiac dysrhythmias, ALS, mental disorders and cancer mortality) merit continued monitoring among Gulf War veterans in case more convincing latent deployment effects are detected, it now seems time to consider ceasing other Gulf War veteran research. Health registries have closed and the ones that remain open are greatly reduced in activity. Available healthcare utilization data have been thoroughly examined. Because Gulf War veterans have experienced many confounding exposures since the War and because many have left the service, it becomes increasingly difficult to conduct epidemiological studies for aetiology of ‘Gulf War illness’. It seems prudent now to direct veteran research efforts, especially that involving aetiology, towards improving the health of those who are now serving in Iraq and Afghanistan.
Acknowledgments
The authors thank the many collaborators who made the authors' study of Gulf War veterans possible. Specifically, we recognize the much appreciated contributions of Gary Gackstetter, Kenneth Hyams, Tim Bullman, Gary Macfalane Rick Riddle, Roger Gibson, Myrna Gray, Jim Knoke, Tyler Smith, Besa Smith, Megan Ryan, Steve Wignall, John Graham and Mike Dove.
Footnotes
One contribution of 17 to a Theme Issue ‘The health of Gulf War veterans’.
References
- Araneta M.R, Moore C.A, Olney R.S, Edmonds L.D, Karcher J.A, McDonough C, Hiliopoulos K.M, Schlangen K.M, Gray G. Goldenhar syndrome among infants born in military hospitals to Gulf War veterans. Teratology. 1997;56:244–251. doi: 10.1002/(SICI)1096-9926(199710)56:4<244::AID-TERA3>3.0.CO;2-Z. doi:10.1002/(SICI)1096-9926(199710)56:4<244::AID-TERA3>3.0.CO;2-Z [DOI] [PubMed] [Google Scholar]
- Australian Department of Defence, Australian Department of Veterans' Affairs, Monash University, Department of Epidemiology and Preventive Medicine & Health Services Australia. Commonwealth of Australia; Canberra, Australia: 2003. Australian Gulf War veterans' health study 2003. [Google Scholar]
- Bell N.S, Amoroso P.J, Williams J.O, Yore M.M, Engel C.C, Jr, Senier L, DeMattos A.C, Wegman D.H. Demographic, physical, and mental health factors associated with deployment of U.S. Army soldiers to the Persian Gulf. Mil. Med. 2000;165:762–772. [PMC free article] [PubMed] [Google Scholar]
- Bell N.S, Amoroso P.J, Wegman D.H, Senier L. Proposed explanations for excess injury among veterans of the Persian Gulf War and a call for greater attention from policymakers and researchers. Inj. Prev. 2001;7:4–9. doi: 10.1136/ip.7.1.4. doi:10.1136/ip.7.1.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blood C.G, Aboumrad T.L. A comparison of postdeployment hospitalization incidence between active duty Vietnam and Persian Gulf War Veterans. Mil. Med. 2001;166:648–655. [PubMed] [Google Scholar]
- Boehmer T.K, Flanders W.D, McGeehin M.A, Boyle C, Barrett D.H. Postservice mortality in Vietnam veterans: 30-year follow-up. Arch. Intern. Med. 2004;164:1908–1916. doi: 10.1001/archinte.164.17.1908. doi:10.1001/archinte.164.17.1908 [DOI] [PubMed] [Google Scholar]
- Boyd K.C, Hallman W.K, Wartenberg D, Fiedler N, Brewer N.T, Kipen H.M. Reported exposures, stressors, and life events among Gulf War Registry veterans. J. Occup. Environ. Med. 2003;45:1247–1256. doi: 10.1097/01.jom.0000099980.38936.09. [DOI] [PubMed] [Google Scholar]
- Boyko E.J, Koepsell T.D, Gaziano J.M, Horner R.D, Feussner J.R. US Department of Veterans Affairs medical care system as a resource to epidemiologists. Am. J. Epidemiol. 2000;151:307–314. doi: 10.1093/oxfordjournals.aje.a010207. [DOI] [PubMed] [Google Scholar]
- Brown M. Toxicological assessments of Gulf War veterans. Phil. Trans. R. Soc. B. 2006;361:649–679. doi: 10.1098/rstb.2006.1825. doi:10.1098/rstb.2006.1825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullman T.A, Mahan C.M, Kang H.K, Page W.F. Mortality in US Army Gulf War veterans exposed to 1991 Khamisiyah chemical munitions destruction. Am. J. Public Health. 2005;95:1382–1388. doi: 10.2105/AJPH.2004.045799. doi:10.2105/AJPH.2004.045799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canavan K. US Medicine. 1994. Gulf illness studies seen wasting funds. p. 1 and 49. [Google Scholar]
- Centers for Disease Control Vietnam Experience Study. Postservice mortality among Vietnam veterans. J. Am. Med. Assoc. 1987;257:790–795. [PubMed] [Google Scholar]
- Cherry N, Creed F, Silman A, Dunn G, Baxter D, Smedley J, Taylor S, Macfarlane G.J. Health and exposures of United Kingdom Gulf war veterans. Part I: the pattern and extent of ill health. Occup. Environ. Med. 2001;58:291–298. doi: 10.1136/oem.58.5.291. doi:10.1136/oem.58.5.291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker W. A review of Gulf War illness. J. R. Navy Med. Serv. 1996;82:141–146. [PubMed] [Google Scholar]
- Coker W.J, Bhatt B.M, Blatchley N.F, Graham J.T. Clinical findings for the first 1000 Gulf war veterans in the Ministry of Defence's medical assessment programme. Br. Med. J. 1999;318:290–294. doi: 10.1136/bmj.318.7179.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Defence Analytical Services Agency. Defence Analytical Services Agency; London, UK: 2005. 1990/1991 Gulf conflict—UK Gulf veterans mortality data: causes of death. [Google Scholar]
- Defense Science Board. Office of the Under Secretary of Defense for Acquisition and Technology; Washington, DC: 1994. Final Report: Defense Science Board Task Force on Persian Gulf War health effects. [Google Scholar]
- Department of Veterans Affairs, Veterans Health Administration and Department of Defense, Office of the Assistant Secretary of Defense, Health Affairs. Department of Veterans Affairs, Veterans Health Administration and the Department of Defense, Office of the Assistant of the Secretary of Defense, Health Affairs; Washington, DC: 2002. Combined analysis of the VA and DoD Gulf War clinical registries: a study of clinical findings from systematic medical examinations of 100,000 U.S. Gulf War veterans. pp. 1–109. [Google Scholar]
- Dlugosz L.J, Hocter W.J, Kaiser K.S, Knoke J.D, Heller J.M, Hamid N.A, Reed R.J, Kendler K.S, Gray G.C. Risk factors for mental disorder hospitalization after the Persian Gulf War: U.S. Armed Forces, June 1, 1991–September 30, 1993. J. Clin. Epidemiol. 1999;52:1267–1278. doi: 10.1016/s0895-4356(99)00131-6. doi:10.1016/S0895-4356(99)00131-6 [DOI] [PubMed] [Google Scholar]
- Doyle P, Maconochie N, Ryan M. Reproductive health of Gulf War veterans. Phil. Trans. R. Soc. B. 2006;361:571–584. doi: 10.1098/rstb.2006.1817. doi:10.1098/rstb.2006.1817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel L.W, Strauchen J.A, Chiazze L, Jr, Heid M. Accuracy of death certification in an autopsied population with specific attention to malignant neoplasms and vascular diseases. Am. J. Epidemiol. 1980;111:99–112. doi: 10.1093/oxfordjournals.aje.a112879. [DOI] [PubMed] [Google Scholar]
- Erickson A.R, Enzenauer R.J, Bray V.J, West S.G. Musculoskeletal complaints in Persian Gulf War veterans. J. Clin. Rheumatol. 1998;4:181–185. doi: 10.1097/00124743-199808000-00005. doi:10.1097/00124743-199808000-00002 [DOI] [PubMed] [Google Scholar]
- Escalante A, Fischbach M. Musculoskeletal manifestations, pain, and quality of life in Persian Gulf War veterans referred for rheumatologic evaluation. J. Rheumatol. 1998;25:2228–2235. [PubMed] [Google Scholar]
- 1991a Executive Order 12744. Designation of Arabian Peninsula areas, airspace and adjacent waters as a combat zone. Fed. Regist 56, 2663.
- Fukuda K, et al. Chronic multisymptom illness affecting Air Force veterans of the Gulf War. J. Am. Med. Assoc. 1998;280:981–988. doi: 10.1001/jama.280.11.981. doi:10.1001/jama.280.11.981 [DOI] [PubMed] [Google Scholar]
- Fulco C, Liverman C, Sox H. Gulf War and health. vol. 1. National Academy Press; Washington, DC: 2003. Depleted uranium, pyridostigmine bromide, sarin, vaccines. [PubMed] [Google Scholar]
- Gackstetter G.D, et al. Assessing the potential health impact of the 1991 Gulf War on Saudi Arabian National Guard soldiers. Int. J. Epidemiol. 2005;34:801–808. doi: 10.1093/ije/dyi008. doi:10.1093/ije/dyi008 [DOI] [PubMed] [Google Scholar]
- Grady E.P, Carpenter M.T, Koenig C.D, Older S.A, Battafarano D.F. Rheumatic findings in Gulf War veterans. Arch. Intern. Med. 1998;158:367–371. doi: 10.1001/archinte.158.4.367. doi:10.1001/archinte.158.4.367 [DOI] [PubMed] [Google Scholar]
- Graham J.T. Investigating Gulf veterans' health concerns. J. R. Navy Med. Serv. 1996;82:113–116. [PubMed] [Google Scholar]
- Gray G.C. Increased evidence of testicular cancer among veterans of the 1991 Gulf War. Mil. Med. 2005;170:394. [PubMed] [Google Scholar]
- Gray G.C, Coate B.D, Anderson C.M, Kang H.K, Berg S.W, Wignall F.S, Knoke J.D, Barrett-Connor E. The postwar hospitalisation experience of U.S. veterans of the Persian Gulf War. N. Engl. J. Med. 1996;335:1505–1513. doi: 10.1056/NEJM199611143352007. doi:10.1056/NEJM199611143352007 [DOI] [PubMed] [Google Scholar]
- Gray G, Knoke J, Berg S, Wignall F, Barrett-Connor E. Counterpoint: responding to suppositions and misunderstandings. Am. J. Epidemiol. 1998a;148:328–333. doi: 10.1093/oxfordjournals.aje.a009648. [DOI] [PubMed] [Google Scholar]
- Gray G.C, Hawksworth A.W, Smith T.C, Kang H.K, Knoke J.D, Gackstetter G.D. Gulf War veterans' health registries. Who is most likely to seek evaluation? Am. J. Epidemiol. 1998b;148:343–349. doi: 10.1093/oxfordjournals.aje.a009651. [DOI] [PubMed] [Google Scholar]
- Gray G.C, Kaiser K.S, Hawksworth A.W, Hall F.W, Barrett-Connor E. Increased postwar symptoms and psychological morbidity among U.S. Navy Gulf War veterans. Am. J. Trop. Med. Hyg. 1999a;60:758–766. doi: 10.4269/ajtmh.1999.60.758. [DOI] [PubMed] [Google Scholar]
- Gray G.C, Smith T.C, Knoke J.D, Heller J.M. The postwar hospitalization experience of Gulf War veterans possibly exposed to chemical munitions destruction at Khamisiyah, Iraq. Am. J. Epidemiol. 1999b;150:532–540. doi: 10.1093/oxfordjournals.aje.a010043. [DOI] [PubMed] [Google Scholar]
- Gray G.C, Smith T.C, Kang H.K, Knoke J.D. Are Gulf War veterans suffering war-related illnesses? Federal and civilian hospitalizations examined, June 1991 to December 1994. Am. J. Epidemiol. 2000;151:63–71. doi: 10.1093/oxfordjournals.aje.a010123. [DOI] [PubMed] [Google Scholar]
- Gray G.C, Chesbrough K.B, Ryan M.A, Amoroso P, Boyko E.J, Gackstetter G.D, Hooper T.I, Riddle J.R. The millennium Cohort Study: a 21-year prospective cohort study of 140,000 military personnel. Mil. Med. 2002a;167:483–488. [PubMed] [Google Scholar]
- Gray G.C, Reed R.J, Kaiser K.S, Smith T.C, Gastanaga V.M. Self-reported symptoms and medical conditions among 11,868 Gulf War-era veterans: the Seabee Health Study. Am. J. Epidemiol. 2002b;155:1033–1044. doi: 10.1093/aje/155.11.1033. doi:10.1093/aje/155.11.1033 [DOI] [PubMed] [Google Scholar]
- Gray G.C, Gackstetter G.D, Kang H.K, Graham J.T, Scott K.C. After more than 10 years of Gulf War veteran medical evaluations, what have we learned? Am. J. Prev. Med. 2004;26:443–452. doi: 10.1016/j.amepre.2004.02.006. doi:10.1016/j.amepre.2004.02.006 [DOI] [PubMed] [Google Scholar]
- Haley R.W. Excess incidence of ALS in young Gulf War veterans. Neurology. 2003;61:750–756. doi: 10.1212/wnl.61.6.750. [DOI] [PubMed] [Google Scholar]
- Hallman W.K, Kipen H.M, Diefenbach M, Boyd K, Kang H, Leventhal H, Wartenberg D. Symptom patterns among Gulf War registry veterans. Am. J. Public Health. 2003;93:624–630. doi: 10.2105/ajph.93.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heier S.J, Enzenauer R.W, Wintermeyer S.F, Delaney M, LaPiana F.P. Ocular injuries and diseases at a combat support hospital in support of Operations Desert Shield and Desert Storm. Arch. Ophthalmol. 1993;111:795–798. doi: 10.1001/archopht.1993.01090060083028. [DOI] [PubMed] [Google Scholar]
- Helmkamp J.C. United States military casualty comparisons during the Persian Gulf War. J. Occup. Med. 1994;36:609–615. [PubMed] [Google Scholar]
- Henderson R.F, et al. Response of F344 rats to inhalation of subclinical levels of sarin: exploring potential causes of Gulf War illness. Toxicol. Ind. Health. 2001;17:294–297. doi: 10.1191/0748233701th105oa. doi:10.1191/0748233701th105oa [DOI] [PubMed] [Google Scholar]
- Henderson R.F, et al. Response of rats to low levels of sarin. Toxicol. Appl. Pharmacol. 2002;184:67–76. doi:10.1016/S0041-008X(02)99495-0 [PubMed] [Google Scholar]
- Henry L, Gray G. Naval Health Research Center; San Diego, CA: 2001. Topical bibliography of published works regarding the health of veterans of the Persian Gulf War. [Google Scholar]
- Hines J.F. Ambulatory health care needs of women deployed with a heavy armor division during the Persian Gulf War. Mil. Med. 1992;157:219–221. [PubMed] [Google Scholar]
- Hines J.F. A comparison of clinical diagnoses among male and female soldiers deployed during the Persian Gulf War. Mil. Med. 1993;158:99–101. [PubMed] [Google Scholar]
- Hobfoll S, et al. War-related stress: addressing the stress of war and other traumatic events. Am. Psychol. 1991;46:848–855. doi: 10.1037//0003-066x.46.8.848. doi:10.1037/0003-066X.46.8.848 [DOI] [PubMed] [Google Scholar]
- Horner R.D, et al. Occurrence of amyotrophic lateral sclerosis among Gulf War veterans. Neurology. 2003;61:742–749. doi: 10.1212/01.wnl.0000069922.32557.ca. [DOI] [PubMed] [Google Scholar]
- Hyams K. Gulf War syndrome: potential role of infectious diseases. Curr. Opin. Infect. Dis. 1999;12:439–443. doi: 10.1097/00001432-199910000-00005. [DOI] [PubMed] [Google Scholar]
- Hyams K.C, et al. Diarrheal disease during Operation Desert Shield. N. Engl. J. Med. 1991;325:1423–1428. doi: 10.1056/NEJM199111143252006. [DOI] [PubMed] [Google Scholar]
- Hyams K.C, Bourgeois A.L, Escamilla J, Burans J, Woody J.N. The Navy forward laboratory during Operations Desert Shield/Desert Storm. Mil. Med. 1993;158:729–732. [PubMed] [Google Scholar]
- Hyams K.C, Hanson K, Wignall F.S, Escamilla J, Oldfiled E.C. The impact of infectious diseases on the health of U.S. troops deployed to the Persian Gulf during operations Desert Shield and Desert Storm. Clin. Infect. Dis. 1995;20:1497–1504. doi: 10.1093/clinids/20.6.1497. [DOI] [PubMed] [Google Scholar]
- Hyams K.C, Riddle J, Trump D.H, Wallace M.R. Protecting the Health of United States Military Forces in Afghanistan: applying lessons learned since the Gulf War. Clin. Infect. Dis. 2002;34:S208–S214. doi: 10.1086/340705. [DOI] [PubMed] [Google Scholar]
- Ikin J.F, et al. War-related psychological stressors and risk of psychological disorders in Australian veterans of the 1991 Gulf War. Br. J. Psychiatry. 2004;185:116–126. doi: 10.1192/bjp.185.2.116. doi:10.1192/bjp.185.2.116 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. National Academy Press; Washington, DC: 1995. Health consequences of service during the Persian Gulf War: initial findings and recommendations for immediate action. [PubMed] [Google Scholar]
- Institute of Medicine. Committee to Review the Health Consequences of Service During the Persian Gulf War. National Academy Press; Washington, DC: 1996. Health consequences of service during the Persian Gulf War: recommendations for research and information systems. [PubMed] [Google Scholar]
- Institute of Medicine. National Academy Press; Washington, DC: 1997. Adequacy of the comprehensive clinical evaluation program: a focused assessment. [PubMed] [Google Scholar]
- Institute of Medicine: Committee on the Evaluation of the Department of Defense Comprehensive Clinical Evaluation Program. National Academy Press; Washington, DC: 1997. Adequacy of the Comprehensive Clinical Evaluation Program: nerve agents. [Google Scholar]
- Joellenbeck L.M, Landrigan P.J, Larson E.L. Gulf War veterans' illnesses: a case study in causal inference. Environ. Res. 1998;79:71–81. doi: 10.1006/enrs.1998.3873. doi:10.1006/enrs.1998.3873 [DOI] [PubMed] [Google Scholar]
- Joseph S, The Comprehensive Clinical Evaluation Program Evaluation Team A comprehensive clinical evaluation of 20,000 Persian Gulf War veterans. Mil. Med. 1997;162:149–155. [PubMed] [Google Scholar]
- Kalra R, Singh S, Razani-Boroujerdi S, Langley R, Blackwell W, Henderson R, Sopori M. Subclinical doses of the nerve gas sarin impair T cell responses through the autonomic nervous system. Toxicol. Appl. Pharmacol. 2002;184:82–87. doi:10.1016/S0041-008X(02)99497-4 [PubMed] [Google Scholar]
- Kang H, Bullman T. Mortality among US veterans of the Persian Gulf War. N. Engl. J. Med. 1996;355:1498–1504. doi: 10.1056/NEJM199611143352006. doi:10.1056/NEJM199611143352006 [DOI] [PubMed] [Google Scholar]
- Kang H.K, Bullman T. Counterpoint: negligible “healthy-warrior effect” on Gulf War veterans' mortality. Am. J. Epidemiol. 1998;148:324–325. doi: 10.1093/oxfordjournals.aje.a009646. [discussion 334–338.] [DOI] [PubMed] [Google Scholar]
- Kang H.K, Bullman T.A. Mortality among US veterans of the Persian Gulf War: 7-year follow-up. Am. J. Epidemiol. 2001;154:399–405. doi: 10.1093/aje/154.5.399. doi:10.1093/aje/154.5.399 [DOI] [PubMed] [Google Scholar]
- Kang, H., Magee, C. & Bullman, T. 1997 Analysis of potential risk factors for the excess accidental deaths among Persian Gulf veterans. In 125th American Public Health Association Meeting, Indiana, IN.
- Kang H.K, Mahan C.M, Lee K.Y, Magee C.A, Murphy F.M. Illnesses among United States veterans of the Gulf War: a population-based survey of 30,000 veterans. J. Occup. Environ. Med. 2000;42:491–501. doi: 10.1097/00043764-200005000-00006. [DOI] [PubMed] [Google Scholar]
- Kang H.K, Natelson B.H, Mahan C.M, Lee K.Y, Murphy F.M. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am. J. Epidemiol. 2003;157:141–148. doi: 10.1093/aje/kwf187. doi:10.1093/aje/kwf187 [DOI] [PubMed] [Google Scholar]
- Karsarskis E, Brooks B, Ross M. Office of Under Secretary for Health, Department of Veterans Affairs; Washington, DC: 1999. Persian Gulf veterans with amyotrophic lateral sclerosis (ALS): report of a review panel. [Google Scholar]
- Kelsall H.L, Sim M.R, Forbes A.B, Glass D.C, McKenzie D.P, Ikin J.F, Abramson M.J, Blizzard L, Ittak P. Symptoms and medical conditions in Australian veterans of the 1991 Gulf War: relation to immunisations and other Gulf War exposures. Occup. Environ. Med. 2004;61:1006–1013. doi: 10.1136/oem.2003.009258. doi:10.1136/oem.2003.009258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kipen H.M, Hallman W, Kang H, Fiedler N, Natelson B.H. Prevalence of chronic fatigue and chemical sensitivities in Gulf Registry veterans. Arch. Environ. Health. 1999;54:313–318. doi: 10.1080/00039899909602493. [DOI] [PubMed] [Google Scholar]
- Knoke J.D, Gray G.C. Hospitalizations for unexplained illnesses among U.S. veterans of the Persian Gulf War. Emerg. Infect. Dis. 1998;4:211–219. doi: 10.3201/eid0402.980208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knoke J.D, Gray G.C, Garland F.C. Testicular cancer and Persian Gulf War service. Epidemiology. 1998;9:648–653. doi:10.1097/00001648-199811000-00011 [PubMed] [Google Scholar]
- Korenyi-Both A.L, Molnar A.C, Korenyi-Both A.L, Fidelus-Gort R.F. Al Eskan disease: Desert Storm pneumonitis. Mil. Med. 1992;157:452–462. [PubMed] [Google Scholar]
- Kroenke K, Koslowe P, Roy M. Symptoms in 18,495 Persian Gulf War veterans. J. Occup. Environ. Med. 1998;40:520–528. doi: 10.1097/00043764-199806000-00004. doi:10.1097/00043764-199806000-00004 [DOI] [PubMed] [Google Scholar]
- Kuller L. The use of existing databases in morbidity and mortality studies. Am. J. Public Health. 1995;85:1198–1200. doi: 10.2105/ajph.85.9.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H.A, Gabriel R, Bale A.J, Bolton P, Blatchley N.F. Clinical findings of the second 1000 UK Gulf War veterans who attended the Ministry of Defence's Medical Assessment Programme. J. R. Army Med. Corps. 2001;147:153–160. doi: 10.1136/jramc-147-02-08. [DOI] [PubMed] [Google Scholar]
- Lee H.A, Gabriel R, Bolton J.P, Bale A.J, Jackson M. Health status and clinical diagnoses of 3000 UK Gulf War veterans. J. R. Soc. Med. 2002;95:491–497. doi: 10.1258/jrsm.95.10.491. doi:10.1258/jrsm.95.10.491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H.A, Bale A.J, Gabriel R. Results of investigations on Gulf War veterans. Clin. Med. 2005a;5:166–172. doi: 10.7861/clinmedicine.5-2-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H.A, Gabriel R, Bale A.J. Clinical outcomes of Gulf veterans' medical assessment programme referrals to specialised centers for Gulf veterans with post-traumatic stress disorder. Mil. Med. 2005b;170:400–405. doi: 10.7205/milmed.170.5.400. [DOI] [PubMed] [Google Scholar]
- Levine P.H, Young H.A, Simmens S.J, Rentz D, Kofie V.E, Mahan C.M, Kang H.K. Is testicular cancer related to Gulf War deployment? Evidence from a pilot population-based study of Gulf War era veterans and cancer registries. Mil. Med. 2005;170:149–153. [PubMed] [Google Scholar]
- Macfarlane G.J, Thomas E, Cherry N. Mortality among UK Gulf War veterans. Lancet. 2000;356:17–21. doi: 10.1016/S0140-6736(00)02428-4. doi:10.1016/S0140-6736(00)02428-4 [DOI] [PubMed] [Google Scholar]
- Macfarlane G.J, Biggs A.M, Maconochie N, Hotopf M, Doyle P, Lunt M. Incidence of cancer among UK Gulf war veterans: cohort study. Br. Med. J. 2003;327:1373. doi: 10.1136/bmj.327.7428.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill A, Gasser R.J, Oster C, Grogl M, Sun W. Viscerotropic leishmaniasis in persons returning from Operation Desert Storm 1990–1991. Arch. Dermatol. 1992;128:1033–1034. [Google Scholar]
- Murphy F.M. Gulf war syndrome. Br. Med. J. 1999;318:274–275. doi: 10.1136/bmj.318.7179.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy F, Browne D, Mather S, Scheele H, Hyams K.C. Women in the Persian Gulf War: health care implications for active duty troops and veterans. Mil. Med. 1997;162:656–660. [PubMed] [Google Scholar]
- Murphy F.M, Kang H, Dalager N.A, Lee K.Y, Allen R.E, Mather S.H, Kizer K.W. The health status of Gulf War veterans: lessons learned from the Department of Veterans Affairs Health Registry. Mil. Med. 1999;164:327–331. [PubMed] [Google Scholar]
- Newmark J, Clayton W.L.I. Persian Gulf illnesses: preliminary neurological impressions. Mil. Med. 1995;160:505–507. [PubMed] [Google Scholar]
- Paparello S.F, Garst P, Bourgeois A.L, Hyams K.C. Diarrheal and respiratory disease aboard the hospital ship, USNS-Mercy T-AH 19, during Operation Desert Shield. Mil. Med. 1993;158:392–395. doi: 10.21236/ada268438. [DOI] [PubMed] [Google Scholar]
- Percy C, Stanek E, III, Gloeckler L. Accuracy of cancer death certificates and its effect on cancer mortality statistics. Am. J. Public Health. 1981;71:242–250. doi: 10.2105/ajph.71.3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrotta D.M. A review conducted by the Environmental Committee of the Armed Forces Epidemiological Board. Armed Forces Epidemiological Board; Falls Church, VA: 1996. Long-term health effects associated with sub-clinical exposures to GB and mustard. [Google Scholar]
- Pohlmann G.P. War and medicine in the desert. A report of the 13th Evacuation Hospital in Saudi Arabia. Wis. Med. J. 1991;90:511–516. [PubMed] [Google Scholar]
- Richards A.L, Hyams K.C, Watts D.M, Rozmajzl P.J, Woody J.N, Merrell B.R. Respiratory disease among military personnel in Saudi Arabia during Operation Desert Shield. Am. J. Public Health. 1993;83:1326–1329. doi: 10.2105/ajph.83.9.1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riegodedios A.J, Ajene A, Malakooti M.A, Gaydos J.C, MacIntosh V.H, Bohnker B.K. Comparing diagnostic coding and laboratory results. Emerg. Infect. Dis. 2005;11:1151–1153. doi: 10.3201/eid1107.041058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ries L, Hankey B, Harras A, Devesa S. In: Cancer incidence, mortality, and patient survival in the United States. Cancer epidemiology and prevention. Schottenfeld D, Fraumeni J.F, editors. Oxford University Press; New York, NY: 1996. p. xxi. [Google Scholar]
- Robinson A. Veterans worry that unexplained medical problems a legacy of service during Gulf War. CMAJ. 1995;152:944–947. [PMC free article] [PubMed] [Google Scholar]
- Rose M.R, Brix K.A. Neurological disorders in Gulf War veterans. Phil. Trans. R. Soc. B. 2006;361:605–618. doi: 10.1098/rstb.2006.1820. doi:10.1098/rstb.2006.1820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy M, Koslowe P, Kroenke K, Magruder C. Signs, symptoms, and ill-defined conditions in Persian Gulf War veterans: findings from the Comprehensive Clinical Evaluation Program. Psychosom. Med. 1998;60:663–668. doi: 10.1097/00006842-199811000-00001. [DOI] [PubMed] [Google Scholar]
- Ryan M.A, Amoroso P, Boyko E.J, Gackstetter G.D, Gary G.C, Hooper T.I, Riddle J.R. The millennium cohort study. Mil. Med. 2002;167:ii. [PubMed] [Google Scholar]
- Shaw E, Hermansen L, Pugh W, White M. Naval Health Research Center; San Diego, CA: 1991. Disease and non-battle injuries among Navy and Marine Corps personnel during operation Desert Shield/Desert Storm. [Google Scholar]
- Sim, M. et al 2003 Australian Gulf War Veterans Health Study. Available online at: http://www.dva.gov.au/media/publicat/2003/gulfwarhs/
- Smith T.C, Gray G.C, Knoke J.D. Is systemic lupus erythematosus, amyotrophic lateral sclerosis, or fibromyalgia associated with Persian Gulf War service? An examination of Department of Defense hospitalisation data. Am. J. Epidemiol. 2000;151:1053–1059. doi: 10.1093/oxfordjournals.aje.a010147. [DOI] [PubMed] [Google Scholar]
- Smith T.C, Heller J.M, Hooper T.I, Gackstetter G.D, Gray G.C. Are Gulf War veterans experiencing illness due to exposure to smoke from Kuwaiti oil well fires? Examination of Department of Defense hospitalization data. Am. J. Epidemiol. 2002a;155:908–917. doi: 10.1093/aje/155.10.908. doi:10.1093/aje/155.10.908 [DOI] [PubMed] [Google Scholar]
- Smith T.C, Smith B, Ryan M.A, Gray G.C, Hooper T.I, Heller J.M, Dalager N.A, Kang H.K, Gackstetter G.D. Ten years and 100,000 participants later: occupational and other factors influencing participation in US Gulf War health registries. J. Occup. Environ. Med. 2002b;44:758–768. doi: 10.1097/00043764-200208000-00011. [DOI] [PubMed] [Google Scholar]
- Smith T.C, Gray G.C, Weir J.C, Heller J.M, Ryan M.A. Gulf War veterans and Iraqi nerve agents at Khamisiyah: postwar hospitalization data revisited. Am. J. Epidemiol. 2003;158:457–467. doi: 10.1093/aje/kwg178. doi:10.1093/aje/kwg178 [DOI] [PubMed] [Google Scholar]
- Smith T.C, Corbeil T.E, Ryan M.A, Heller J.M, Gray G.C. In-theatre hospitalisations of US and allied personnel during the 1991 Gulf War. Am. J. Epidemiol. 2004a;159:1064–1076. doi: 10.1093/aje/kwh152. doi:10.1093/aje/kwh152 [DOI] [PubMed] [Google Scholar]
- Smith T.C, et al. The postwar hospitalization experience of Gulf War veterans participating in U.S. health registries. J. Occup. Environ. Med. 2004b;46:386–397. doi: 10.1097/01.jom.0000121126.49292.69. [DOI] [PubMed] [Google Scholar]
- Smith T.C, Smith B, Corbeil T.E, Riddle J.R, Ryan M.A. Self-reported mental health among US military personnel prior and subsequent to the terrorist attacks of September 11, 2001. J. Occup. Environ. Med. 2004c;46:775–782. doi: 10.1097/01.jom.0000135545.51183.ad. [DOI] [PubMed] [Google Scholar]
- Smith, B., Smith, T., Ryan, M. & Gray, G. 2004d A comparison of the post-deployment hospitalization experience of US military personnel following service in the 1991 Gulf War, Southwest Asia after the Gulf War, and Bosnia. Technical report no. 04-25. San Diego: Naval Health Research Center.
- Stuart J.A, Murray K.M, Ursano R.J, Wright K.M. The Department of Defense's Persian Gulf War registry year 2000: an examination of veterans' health status. Mil. Med. 2002;167:121–128. [PubMed] [Google Scholar]
- 1991bThe International Classification of Diseases, 9th Revision, Clinical Modification 3rd edn. Washington, DC: US Department of Health and Human Services.
- The Iowa Persian Gulf Study Group. Self-reported illness and health status among Persian Gulf War veterans: a population-based study. J. Am. Med. Assoc. 1997;277:238–245. doi:10.1001/jama.277.3.238 [PubMed] [Google Scholar]
- Trump D.H, Mazzuchi J.F, Riddle J, Hyams K.C, Balough B. Force health protection: 10 years of lessons learned by the Department of Defense. Mil. Med. 2002;167:179–185. [PubMed] [Google Scholar]
- Wasserman G.M, Martin B.L, Hyams K.C, Merrill B.R, Oaks H.G, McAdoo H.A. A survey of outpatient visits in a United States Army Forward Unit during Operation Desert Shield. Mil. Med. 1997;162:374–379. [PubMed] [Google Scholar]
- Wheelwright J. W.W. Norton & Company; New York, NY: 2001. The irritable heart: the medical mystery of the Gulf War. [Google Scholar]
- Wintermeyer S.F, Pina J.S, Cremins J.E, Heier J.S. The inpatient experience of a US Army combat support hospital in the Persian Gulf during non-combat and combat periods. Mil. Med. 1994;159:746–751. [PubMed] [Google Scholar]
- Wintermeyer S.F, Cremins J.E, Pina J.S, Heier J.S. Medical care of Iraqis at a forwardly deployed US Army hospital during Operation Desert Storm. Mil. Med. 1996;161:294–297. [PubMed] [Google Scholar]
- Writer J.V, DeFraites R.F, Brundage J.F. Comparative mortality among US military personnel in the Persian Gulf region and worldwide during Operations Desert Shield and Desert Storm. J. Am. Med. Assoc. 1996;275:118–121. doi:10.1001/jama.275.2.118 [PubMed] [Google Scholar]
- Zwerling C, Torner J.C, Clarke W.R, Voelker M.D, Doebbeling B.N, Barrett D.H, Merchant J.A, Woolson R.F, Schwartz D.A. Self-reported postwar injuries among Gulf War veterans. Public Health Rep. 2000;115:346–349. doi: 10.1093/phr/115.4.346. doi:10.1093/phr/115.4.346 [DOI] [PMC free article] [PubMed] [Google Scholar]