In 2003, 194 million people 20 to 79 years of age had diabetes mellitus, almost three-quarters of them living in the developing world. By 2025 this number will have increased by 72%: 333 million cases are predicted, with a doubling of the prevalence in the Middle East, North Africa, South Asia and Sub-Saharan Africa. Almost 1 million people die because of diabetes each year, two-thirds of these in developing countries1 (see Appendix 1, available online at www.cmaj.ca/cgi/content/full/175/7/733/DC1).
This growing problem will have a significant impact on national and individual economies as well as on individual health; however, it has proven difficult to determine just what that impact is. Good data on the direct medical costs of diabetes are not available for most developing countries, although extrapolation from information gathered in developed countries is possible. Worldwide estimates suggest that the annual direct medical costs of diabetes total at least US$129 billion and may be as high as US$241 billion, or 2.5% to 15.0% of global annual health care budgets2 (see Appendix 1, available online at www.cmaj.ca/cgi/content/full/175/7/733/DC1). The indirect costs of diabetes (such as lost productivity) are at least as high and increase as more economically productive people are affected. To lessen the impact, how should governments in developing countries tackle this burgeoning problem?
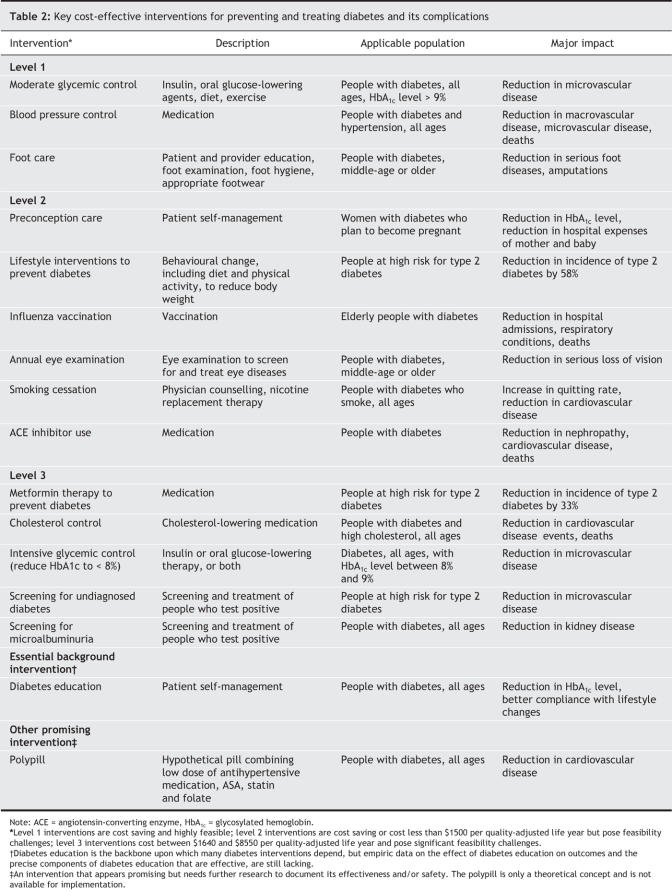
Most interventions to prevent and treat diabetes and its complications have a significant effect on health services utilization. Determining which of these interventions are most cost-effective in developing countries is difficult because of insufficient data. Nonetheless, high-quality efficacy evidence for strategies to prevent diabetes and its complications are available from developed countries and can be used to make useful estimates about the costs and likely benefits of implementing different types of care in developing countries.
To make estimates for developing countries, we updated an earlier comprehensive review3 of cost-effectiveness studies to 2003 (see Appendix 2, available online at www.cmaj.ca/cgi/content/full/175/7/733/DC1). We then estimated the cost-effectiveness ratio (CER) of diabetes interventions for the 6 developing regions, assuming that the effectiveness of these interventions (in quality-adjusted life years [QALYs]) was the same as for developed countries but that their costs were different (Table 1). CERs for developing regions were calculated by multiplying the CER for the developed countries by the ratio of costs in the developing region to costs in the developed countries. We estimated the costs of diabetes care in the 6 developing regions using the framework of Mulligan and associates,4 which calls for the development of a relative cost index for health care services across regions and the availability of information about costs for one region. We estimated the relative cost index using data from Mulligan and associates, assuming that the cost of diabetes care in the United States (where most studies were conducted) was 8.6 times the cost for the Latin America and the Caribbean region.5 The costs of diabetes care in the other 5 developing regions were calculated by multiplying the cost of care in the Latin America region by the relative cost index. A more complete description of the methods is available in the relevant chapter of the online publication Disease control priorities in developing countries.5
Table 1
Having established cost-effectiveness data for the 6 developing regions, we then assessed which interventions should have priority on the basis of their CERs and feasibility of implementation (Box 1). Feasibility was judged from 4 aspects: difficulty of reaching the intended population, technical complexity, capital intensity and cultural acceptability. Level 1 interventions are both cost saving and feasible, although a short-term increase in intervention costs may be a barrier to their implementation (Table 1 and Table 2). Level 2 interventions are cost saving but moderately feasible (e.g., it may be difficult to reach all women needing preconception care) or cost less than US$1500 per QALY (e.g., angiotensin-converting enzyme [ACE] inhibitors) but are fully or moderately feasible. They represent good value for money but may present some challenges in terms of feasibility. Some interventions are more cost-effective according to patients' age (e.g., screening and treatment for diabetic retinopathy in older people) or are more sensitive to drug prices (e.g., use of ACE inhibitors). Lowering drug prices is a key factor for the success of some drug therapies in developing countries. Smoking cessation appears to be the least cost-effective of the level 2 interventions but its cost-effectiveness is probably underestimated, as our calculations took into account only the projected reduction in risk of cardiovascular disease. Adding the health benefits associated with preventing cancer and pulmonary diseases might improve the cost-effectiveness of smoking cessation.
Box 1.
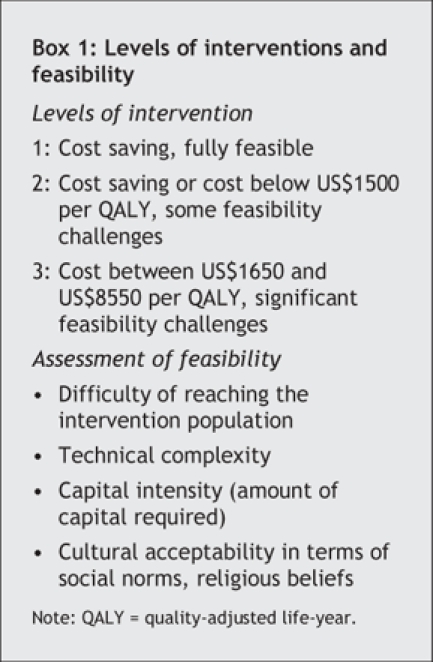
Table 2
Compared with level 1 and 2 interventions, level 3 interventions are less feasible and may not always be justifiable — in the short-term — for all people in developing countries, given limited health care resources. The cost-effectiveness of metformin therapy for preventing type 2 diabetes among people at high risk (e.g., those with prediabetes) and of cholesterol control for people with total cholesterol above 200 mg/dL would improve if drug costs could be lowered (i.e., if generic versions of the drug could be made available).
We also considered the cost-effectiveness of diabetes education, community-based prevention and improvement of quality care. Evaluating the effectiveness of health education is challenging because of the difficulty of separating the effect of education from that of other interventions. A review of literature published in the United States suggests that education about self-management of diabetes may be cost-effective3 and also that diabetes self-management training reduces medical costs in developing countries in the short-term.2 Because the costs of education programs are generally low, this may be a cost-effective strategy. Training patients to better manage their diabetes is also feasible because of its low technical complexity, low capital requirements and cultural acceptability. Diabetes education should be a high-priority intervention for all developing regions.
Data on community-or population-based prevention strategies are sparse, and implementation priorities are unclear. Available studies on preventing type 2 diabetes have used clinic-based approaches targeting high-risk groups, and researchers generally agree that type 2 diabetes can be prevented or its onset delayed. However, the implementation of these results in practice is fraught with unanswered questions: Who would benefit from diabetes prevention? How can those who might benefit be identified? What are the costs, and what is the cost-effectiveness for diabetes prevention at a population level? How should results be extrapolated from developed countries to developing countries, where priorities and approaches may be different?
The quality of diabetes care remains suboptimal worldwide, regardless of a country's level of development, health care system or population.6 Small, single-site studies have identified several promising interventions to improve quality of care at the patient, provider and system levels.7 A systematic review8 has also found that interventions such as regular contact and tracking of patients on computerized tracking systems and the use of nurses to educate patients and facilitate treatment adherence improves care, yet data on the cost-effectiveness of these approaches are sparse.
Future diabetes care in developing countries could be better targeted with the support of well-aimed research. Community-based studies of primary prevention, using lifestyle interventions and/or safer and cheaper drugs to prevent diabetes (when lifestyle interventions are either unfeasible or have failed), are needed. We also need to know the long-term effects of diabetes prevention on cardiovascular and other outcomes and to find more effective and cheaper ways to prevent the major complications of diabetes. Research into noninvasive methods for monitoring blood glucose, effective screening for prediabetes, diabetes and early diabetes complications, and the impact of diabetes education on health outcomes and risk factor control is required.
Epidemiologic and economic data could also support control efforts. Scant data are available on the future burden of diabetes and its complications in developing countries. Data on trends in and effects of diabetes risk factors — obesity, birth weight, physical inactivity, television viewing, dietary factors, socioeconomic factors and the effects of urbanization, industrialization, globalization and stress — are also sparse. More data are needed on the economics of diabetes, its impact on quality of life and the cost-effectiveness of various interventions in the context of developing countries.
Finally, greater emphasis on translational research will support this process, for example, the development of computer models for forecasting burden of disease and research aimed at understanding the trade-offs and best mix of resource allocation for diabetes and chronic disease care needed in developing countries. Well-targeted basic research could lead to better prevention and treatment strategies, such as understanding the role of prenatal influences and gene-environment interactions on diabetes development.
Interventions to reduce the morbidity and mortality associated with diabetes are available and effective, and most, if not all, are feasible to implement in developing countries. It is now up to governments to use these data to address the challenges of a growing diabetes problem.
K.M. Venkat Narayan Hubert Department of Global Health The Rollins School of Public Health Emory University Ping Zhang Desmond Williams Michael Engelgau Giuseppina Imperatore Division of Diabetes Translation National Center for Chronic Disease Prevention and Health Promotion US Centers for Disease Control and Prevention Atlanta, Ga. Alka Kanaya Division of General Internal Medicine University of California San Francisco, Calif. Ambady Ramachandran Diabetes Research Centre Chennai, India
Supplementary Material
Footnotes
The opinions expressed are those of the authors and do not necessarily represent the views of the US Centers for Disease Control and Prevention.
Competing interests: None declared.
REFERENCES
- 1.World Health Organization. Global burden of disease for the year 2001 by World Bank region, for use in disease control priorities in developing countries. 2nd ed. Geneva: World Health Organization; 2002.
- 2.Diabetes atlas. 2nd ed. Brussels: International Diabetes Federation; 2003.
- 3.Klonoff DC, Schwartz DM. An economic analysis of interventions for diabetes. Diabetes Care 2000;23:390-404. [DOI] [PubMed]
- 4.Mulligan J, Fox-Rushby JA, Adam T, et al. Unit costs of health care inputs in low and middle income regions. DCPP Working Paper no. 9. Bethesda (MD): Disease Control Priorities Project; 2003. Available: www.dcp2.org/file/24/wp9.pdf#search=%22Unit%20Costs%20of%20Health%20Care%20Inputs%20in%20Low%20and%20Middle%20Income%20Regions.%20DCPP%20Working%20Paper%20No.%209%22 (accessed 2006 Aug 17).
- 5.Narayan KMV, Zhang P, Kanaya AM, et al. Diabetes: the pandemic and potential solutions. In: Jamison DT, Breman JG, Measham AR, et al, editors. Disease control priorities in developing countries [online publication]. 2nd ed. Geneva: International Bank for Reconstruction and Development/ World Bank; 2006. Available: www.dcp2.org/pubs/DCP/30 (accessed 2006 Aug 24). [PubMed]
- 6.Engelgau MM, Narayan KM, Saaddine JB, et al. Addressing the burden of diabetes in the 21st century: better care and primary prevention. J Am Soc Nephrol 2003;14(Suppl 2):S88-91. [DOI] [PubMed]
- 7.Narayan KM, Benjamin E, Gregg EW, et al. Diabetes translation research: where are we and where do we want to be? Ann Intern Med 2004;140:958-63. [DOI] [PubMed]
- 8.Renders CM, Valk GD, Griffin SJ, et al. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care 2001;24:1821-33. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.