Abstract
Objective:
To compare laparoscopic versus open gastric bypass procedures with respect to 30-day morbidity and mortality rates, using multi-institutional, prospective, risk-adjusted data.
Summary Background Data:
Laparoscopic Roux-en-Y gastric bypass for weight loss is being performed with increasing frequency, partly driven by consumer demand. However, there are no multi-institutional, risk-adjusted, prospective studies comparing laparoscopic and open gastric bypass outcomes.
Methods:
A multi-institutional, prospective, risk-adjusted cohort study of patients undergoing laparoscopic and open gastric bypass procedures was performed from hospitals (n = 15) involved in the Private Sector Study of the National Surgical Quality Improvement Program (NSQIP). Data points have been extensively validated, are based on standardized definitions, and were collected by nurse reviewers who are audited for accuracy.
Results:
From 2000 to 2003, data from 1356 gastric bypass procedures was collected. The 30-day mortality rate was zero in the laparoscopic group (n = 401), and 0.6% in the open group (n = 955) (P = not significant). The 30-day complication rate was significantly lower in the laparoscopic group as compared with the open group: 7% versus 14.5% (P < 0.0001). Multivariate logistic regression analysis was performed to control for potential confounding variables and showed that patients undergoing an open procedure were more likely to develop a complication, as compared with patients undergoing an laparoscopic procedure (odds ratio = 2.08; 95% confidence interval, 1.33–3.25). Propensity score modeling revealed similar results. A prediction model was derived, and variables that significantly predict higher complication rates after gastric bypass included an open procedure, a high ASA class (III, IV, V), functionally dependent patient, and hypertension as a comorbid illness.
Conclusions:
Multicenter, prospective, risk-adjusted data show that laparoscopic gastric bypass is safer than open gastric bypass, with respect to 30-day complication rate.
Multicenter, prospective, risk-adjusted data collected by the NSQIP (National Surgical Quality Improvement Program) Private Sector Hospitals shows that laparoscopic gastric bypass is safer than open gastric bypass with respect to 30-day complication rates.
Morbid obesity is a major health concern in the United States. The prevalence of obesity (body mass index [BMI] > 30 kg/m2) is currently 30% of the U.S. population, greater than double the prevalence from 20 years ago.1 Diet and exercise rarely lead to long-term weight loss. Medical treatments have also been largely unsuccessful, and many of the pharmacologic agents, including ephedra and fenfluramine, have turned out to be unsafe. In 1991, an NIH Consensus Conference concluded that surgery is the only effective treatment of morbid obesity in patients with a BMI greater than 40 kg/m2 or in patients with weight-related comorbidities and a BMI greater than 35 kg/m2. Since that time, gastric bypass surgery for morbidity obesity has become increasingly popular.
In the United States, open Roux-en-Y gastric bypass has been the most commonly performed procedure for the treatment of morbid obesity. Laparoscopic Roux-en-Y gastric bypass, first described in 1994 by Wittgrove et al,2 is now being performed more frequently, partly driven by consumer demand. Multiple studies have been performed reporting the mortality and complications of each procedure separately. Most of these studies are subject to publication bias, and the results are not generalizable as they are derived from single, high-volume institutions.
Population-based results for obesity surgery have been reported on 16,000 cases gleaned from California discharge abstracts based on ICD-9 codes.3 These results do not differentiate between laparoscopic and open procedures. In-hospital mortality was found to be 0.3%, and rates of life-threatening complications were 10.4%. A recent population-based study in the state of Washington examined discharge abstracts of patients undergoing weight loss surgery.3 Again, laparoscopic and open cases were not differentiated. This statewide, population data revealed a 30-day mortality rate 4 times higher than what was found in single-institution reported results: 1.9% versus <0.5%.4,5 The limitations of administrative data sets do not allow for a comparison of laparoscopic versus open procedures, as shown in 3 recent JAMA articles using the Medicare database, California discharge abstracts, and the Nationwide Inpatient Sample.6–8
A meta-analysis of published data describing complications after laparoscopic gastric bypass, as compared with open gastric bypass, has also been reported.9 Laparoscopic cases had a decreased mortality, wound infection, hernia, and incidental splenectomy rates but a higher frequency of GI tract bleeding, early and late bowel obstruction, and stomal stenosis. Only 3 randomized controlled trials have compared the outcomes from laparoscopic gastric bypass to open gastric bypass procedures.10–12 Although these are single institution studies with a small sample size, they do show that laparoscopic bypasses are safe and cost-effective.
Although surgeons and patients have embraced laparoscopic bariatric procedures, some third-party payors are reluctant to provide coverage. The Blue Cross and Blue Shield Association's Technology Evaluation Center reported that “the evidence is not sufficient to form conclusions about the relative efficacy and morbidity of less invasive approaches to bariatric surgery, specifically laparoscopic gastric bypass.”13
There are currently no multi-institution, prospective, risk-adjusted studies comparing outcomes from laparoscopic and open gastric bypass surgery for morbid obesity. The objective of this study is to provide such information, using data from the private sector hospitals that are involved the National Surgical Quality Improvement Program (NSQIP).
The primary aim of the study is to compare laparoscopic versus open gastric bypass procedures with respect to 30-day morbidity and mortality rates. Secondary aims include characterizing morbidity and mortality for surgical treatments of morbid obesity, and identifying independent risk factors that are predictive of complications following these procedures.
METHODS
This study is a multi-institutional, cohort study of patients who underwent Roux-en-Y gastric bypass procedures for morbid obesity. Data were collected prospectively for this study by the hospitals performing gastric bypass procedures (n = 15) that participate in the Patient Safety in Surgery Study of the NSQIP. Studies have shown that the NSQIP techniques can be implemented in the private sector and generate reasonable predictive models.14,15
Data were prospectively collected in a standardized fashion, according to strict definitions of preoperative characteristics, intraoperative information, and postoperative outcomes. Nurse reviewers collected data from computerized and paper patient hospital records, doctor's office records, letters to patients, and telephone interviews with patients. These nurse reviewers are trained in NSQIP techniques and definitions, and are periodically reviewed for quality by national nurse coordinators. The accuracy and reproducibility of the data have been previously demonstrated.16–19
Assembly of Cohort
Roux-en-Y gastric bypass procedures for morbid obesity were determined by the following CPT codes:
43846 Ḡastric restrictive procedure, Roux-en-Y gastric bypass with small bowel reconstruction <100 cm.
43847 Ḡastric restrictive procedure, Roux-en-Y gastric bypass with small bowel reconstruction >100 cm.
43659 Ūnlisted laparoscopic procedures, stomach (Laparoscopic Roux-en-Y gastric bypass).
To assure that the “unlisted laparoscopic procedures” were indeed for the treatment of morbid obesity, the ICD-9 code for morbid obesity (278.01), as well as preoperative BMI, were evaluated. Other procedures (eg, laparoscopic Nissen fundoplication, laparoscopic-assisted esophagectomy) or other diagnoses not consistent with an elective operation for the purpose of weight loss were excluded. Vertical banded gastroplasty, duodenal switch, and other surgical procedures for morbid obesity that have different CPT codes were not included in this analysis.
The preoperative characteristics and intraoperative information were categorized and compared between the 2 groups. Demographic information, comorbid conditions, and preoperative laboratory values were assessed, as well as intraoperative information. χ2 analyses were used for categorical data and t tests for interval data to look for statistically significant differences.
Outcomes were assessed using the NSQIP definitions of complications, as determined and entered into the database prospectively by on-site nurse reviewers.
Analytic Plan and Sample Size
The primary aim of this study was to assess if there is a difference between laparoscopic and open gastric bypasses with respect to mortality and complications.
A χ2 analysis was used to compare 30-day mortality in patients after open gastric bypass as compared with patients status post laparoscopic gastric bypass. A P < 0.05 denoted statistical significance.
Similarly, morbidity, as defined by each of the 23 adverse events from the NSQIP data points, was compared between the laparoscopic and the open techniques for gastric bypass. Again, χ2 analyses were used for nominal data, and t tests for continuous data.
Multivariable regression modeling was used to identify if the type of operation (laparoscopic or open) was an independent risk factor for a poor outcome. Potential independent variables included the 61 preoperative variables such as demographics, comorbid conditions, and preoperative laboratory values, as well as the 15 intraoperative process-of-care variables. Independent variables that are clinically significant and that had a significant relationship with the outcome on univariate analyses were included in the model (with a P < 0.10). A prediction model was then constructed, with stepwise logistic regression model with a significance level for entry and a significance level for selection (SLS) of 0.05. (A backward regression with SLS of 0.05, revealed the same overall model.)
A propensity score analysis was performed to assess for confounding by indication or selection bias, ie, that the type of a procedure that a surgeon chooses for a patient is related to the perceived overall operative risks. A propensity score was developed which determined the probability of being assigned to a particular group based on the observed covariates. Preoperative variables that were found to be statistically different in the laparoscopic and open gastric bypass groups were included in the model to create the propensity score. The propensity score was broken into quintiles, and included as a covariate in the multivariate regression model, to control for possible confounding by indication.
For the prediction model, discrimination was assessed by the c-statistic and calibration assessed by the Hosmer-Lemeshow goodness-of-fit test. Validation was assessed with 10-fold cross-validation and bootstrapping techniques. The Institutional Review Board of the Human Research Committee at the Massachusetts General Hospital approved the study. Statistics were performed using SAS version 8.02, (SAS Institute Inc., Cary, NC).
RESULTS
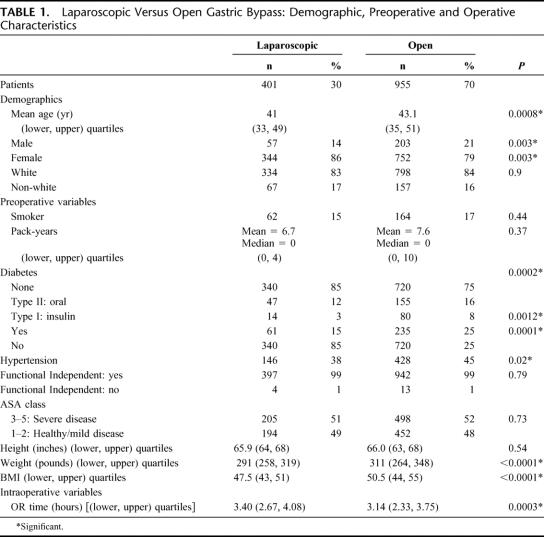
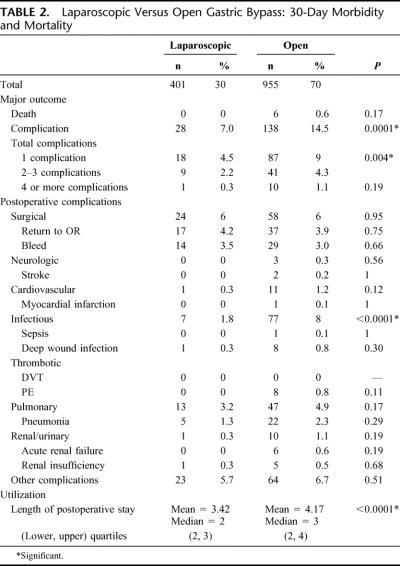
From 2000 to 2003, data from 1356 gastric bypass procedures were collected from the Private Sector Hospitals participating in the NSQIP Patient Safety in Surgery Study (Table 1). Thirty-day mortality rate was zero in the laparoscopic group (n = 401), and 0.6% in the open group (n = 955) [P = 0.17, not significant (Table 2)]. Thirty-day complication rate was 7% in the laparoscopic group and 14.5% in the open group (P < 0.0001). Univariate analysis shows that the open gastric bypass group, compared with the laparoscopic group, had a significantly higher percentage of patients that were older (43.1 versus 41 years), male (21 versus 14%), diabetic (25 versus 15%), hypertensive (45 versus 38%), and who had a higher BMI (50.5 versus 47.5 kg/m2). Compared with the laparoscopic group, the open group had a shorter operative time (3.14 versus 3.40 hours) and a longer length of stay (median of 3 versus 2 days) (Table 1).
TABLE 1. Laparoscopic Versus Open Gastric Bypass: Demographic, Preoperative and Operative Characteristics
TABLE 2. Laparoscopic Versus Open Gastric Bypass: 30-Day Morbidity and Mortality
After multivariable logistic regression to control for potential confounders, patients undergoing an open procedure were more likely to develop a complication, as compared with patients undergoing a laparoscopic procedure (odds ratio [OR], 2.08; 95% confidence interval [CI], 1.33–3.25) (Table 3). Propensity score modeling was done to control for confounding by indication and showed similar results. (Propensity scores were developed by a regression model based on preoperative variables that were significantly different between the laparoscopic and open gastric bypass patients. A separate regression model was then created which included the propensity score, broken up into quintiles, and the overall impact of an open procedure controlling for propensity scores revealed similar results to the original model [OR, 2.05; 95% CI, 1.30–3.24]).
TABLE 3. Multivariable Logistic Regression Prediction Model for a Complication After a Gastric Bypass Operation (Open Versus Laparoscopic): 30-Day Complication Rate
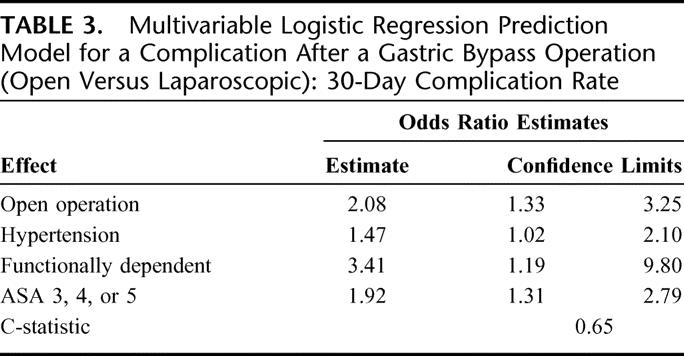
Predictors of a complication included an open procedure (OR, 2.08; 95% CI, 1.33–3.25), a functionally dependent patient (OR, 3.41; 95% CI, 1.19–9.80), a high ASA class (III, IV or V) (OR, 1.92; 95% CI, 1.31–2.79), and hypertension as a comorbid illness (OR, 1.47; 95% CI, 1.02–2.10) (Table 3). The c-statistic of the regression model was 0.65. The Hosmer-Lemeshow test showed excellent calibration, with χ2 of 0.60 and a P value of 0.99. Certain variables that were considered for the model given their significance on univariate analyses (age, BMI, the presence of diabetes, and operative time) did not maintain statistical significance in the final model.
Optimism is a measure used for validation of a predictive model, by assessing how well the predictive model will do in discrimination of a validation data set versus the training set. A model that has been overfit to the training set will have high optimism and not be a good prediction model that is generalizable in that it is predictive in other data sets as well. For the final prediction model presented here, data-derived validation tests were used. Cross validation revealed an optimism of only 0.08 and bootstrapping techniques revealed an optimism of only 0.02.
DISCUSSION
For patients undergoing gastric bypass for morbid obesity in the hospitals participating in the private sector of the NSQIP, 30-day mortality in the laparoscopic group (n = 401) was 0%, and in the open group (n = 966) was 0.6% (P = 0.17, not significant). Thirty-day complication rate in the laparoscopic group was 7%, and in the open group was 14.5% (P < 0.0001). Controlling for potential confounding variables, patients undergoing an open procedure were more likely to develop a complication, as compared with patients undergoing a laparoscopic procedure (OR, 2.08; 95% CI, 1.33–3.25). Predictors of a complication after gastric bypass include an open procedure, a functionally dependent patient, a high ASA class (III, IV or V), and hypertension as a comorbid illness.
This is the first multicenter study that suggests that laparoscopic Roux-en-Y gastric bypass may be safer than the open approach, with regards to 30-day complication rate. Previous single-institution randomized, controlled trials also compared complication rates; however, they did not show a statistically significant difference between the groups (Nguyen et al10: major complication rates, laparoscopic 7.6%, open 9.2%, P = 0.78 = not significant; Lujan et al12: early complications, laparoscopy 22.6%, open 29.4%, P = not significant). A meta-analysis comparing the laparoscopic and open gastric bypass showed that the type and frequency of postoperative complications are different, but does not attempt to tabulate overall complication rates.9
A major limitation to this study is that it identifies only morbidity and mortality but does not assess efficacy of the laparoscopic versus open procedures. There are no outcomes measured that reflect long-term weight loss, or reduction of comorbid illnesses. Also, there is no information on other important outcome metrics including return to work or return to normal activity, or the impact on the quality of life.
Although the complications that were tabulated include the major complications from surgical procedures in general, many comorbid conditions and complications specific to bariatric surgery are not included in the NSQIP data. Some of the bariatric specific variables not assessed in the NSQIP data set include preoperative variables like the presence of sleep apnea or use of continuous positive airway pressure, and postoperative events such as anastomotic leaks, stenosis at the anastomotic sites, or events beyond 30 days such as internal or ventral hernias, obstructions etc.
Although the risk adjustment takes into account 61 preoperative and 15 intraoperative variables, it is possible that certain patient characteristics are not accounted for in the risk adjustment model which could lead to differences in morbidity or mortality. Propensity score analysis, however, shows similar results to the multivariable model above, but this also might not include all the potential variables that could lead to confounding by indication.
Another limitation from this study is the relatively small numbers of deaths (0 in the laparoscopic group, and 6 [0.6%] in the open group) (power = 0.146 to detect the difference in mortality, given this number of cases), which made it impossible to do further statistical modeling with death as an outcome. An appropriately powered study (power = 0.8) to determine a statistically significant difference between these mortality rates would require more than 1600 cases in each group.
Generalizability of this study is limited. Although this multi-institution study involves 15 different hospitals, they almost all are large academic health centers and, as such, these findings may not be generalizable to smaller institutions or to the community hospital setting.
A possible limitation is the ability to correctly identify laparoscopic gastric bypasses. Laparoscopic gastric bypass does not have its own CPT code but instead is listed under “Unlisted laparoscopic procedure, stomach.” This is an imprecise term, and it potentially could include partial gastrectomy, laparoscopic gastrostomy tube, or other procedures. The data were cleaned to exclude diagnoses or procedures that would not be consistent with an elective Roux-en-Y operation gastric bypass for weight loss; however, this relies on the accuracy and completeness of the CPT and ICD-9 coding. Another potential limitation is the lack of verification of mortality in the private sector system. Unfortunately, social security number or other identifying information is not included in the private sector database, so that the National Death Index could not be used.
CONCLUSION
Multicenter, prospective, risk-adjusted data collected by the NSQIP Private Sector Hospitals show that laparoscopic gastric bypass is safer than open gastric bypass with respect to 30-day complication rates. Perhaps with the addition of procedure-specific outcomes and 100% capture for certain procedures, the NSQIP data collection system could be the framework behind an even more powerful research, quality assurance, and quality improvement tool to provide prospective, standardized, risk-adjusted multi-institutional data for specific surgical procedures.
ACKNOWLEDGMENTS
The authors thank Daniel E. Singer, MD, for his help with study design, and Professor E. Francis Cook for his assistance and expertise with the statistical modeling.
Discussions
Dr. Walter J. Pories (Greenville, North Carolina): Congratulations, Dr. Hutter, on a beautiful manuscript, and thank you for emphasizing the efficacy and safety of bariatric surgery. It is astonishing to me that we can sit here and hear a report of 401 cases done laparoscopically, in this group with major serious problems, and still have a mortality of zero percent.
NSQIP is a marvelous tool, we have heard several papers before, but I do have some concerns about whether it is a precise enough instrument for bariatric surgery. To make progress in this rapidly moving field, we need current information, not data from 2000 to 2003. We need numbers that are large enough to compare mortality rates of at least two operations. We need national data that are not limited to either 12 or 18 hospitals; I can't quite keep track whether it is 12 or 18 in your abstract. We need procedures that are standardized in a prospective manner to assure reliable comparisons. And we need data that extend to at least 90 days because postoperative bariatric surgical mortality doubles in the early postoperative period.
The American Society for Bariatric Surgery, faced with the same challenges, therefore organized a consortium of centers of excellence, a group of hospitals and surgeons spread throughout the nation, academic and private, who agreed to meet rigorous requirements, standardize their procedures, and report outcomes verified by site inspection. The process is not managed by the ASBS but rather an independent nonprofit entity that focuses only on bariatric surgery.
This slide shows the results from the previous 12 months, ie, 2004 to 2005, in the 106 centers that include operations on 33,117 patients. The 30-day mortality in these centers is 0.11%, and the 90-day mortality is 0.3%. Remarkably, these outcomes are about the same as those for cholecystectomies in the United States and done in a much sicker population.
The consortium is still a work in progress, but we believe that we can do even better as we use these data for continuous quality improvement. Come and join us, colleagues dedicated to improving the surgical care for the morbidly obese are very welcome.
Dr. Matthew M. Hutter (Boston, Massachusetts): Dr. Pories, thank you very much for your comments. I applaud the efforts of the ASBS and the SRC in the work that they have done in leading these efforts in quality improvement.
The American College of Surgeons has also developed a program, the Bariatric Surgery Center Network to evaluate and to accredit hospitals to perform weight loss surgery. The limitations of the current NSQIP data points that you point out, have all been corrected with the new ACS Bariatric Surgery data collection program. All cases will be captured, using standardized, bariatric specific data points for risk adjustment and outcome assessment. Audited nurse reviewers will collect the data, and data collection will continue well beyond thirty days.
The fact that the ASBS and the American College of Surgeons are working in parallel at this point, I think, is a shame. We all need to work together. The overall goal here is to provide quality improvement and safety for the morbidly obese patient undergoing weight loss surgery. Data collection seems to be the key, and it would be great if the College and the ASBS could work together on this.
Dr. B. Todd Heniford (Charlotte, North Carolina): It is always a pleasure reading studies where the information was prospectively gathered by uninvolved third parties and was evaluated by experts in public health as well as surgery. I do have several questions.
First, in looking at NSQIP, we have had this problem ourselves in trying to compare open and laparoscopic procedures. How were the procedures that were converted from laparoscopy to open handled? Was that a reason that perhaps there was a lower incidence of complications in the laparoscopic group, where the people who are evaluating the charts put them in the open group instead of the intention to treat in the laparoscopic group?
Secondly, is there any way to tell if those patients in the open group with complications were performed by surgeons in institutions who do mostly laparoscopic surgery? Also vice versa? Those surgeons who do mostly open in their institution and they had fewer laparoscopic cases, did they have more complications?
Thirdly, the study included 1356 patients and 12 hospitals over 3 years. And if you look at that, it is about 37 patients per year per institution. As I understand it, this is a sample of that institution, so about 25% of the patients are included. So that would be about 150 patients per institution total that underwent a gastric bypass either open or laparoscopic. And in looking at that, could you break it down to the institutions that had higher versus lower volumes? And then also in open versus laparoscopic, higher and lower volumes, and incidence of complications? Is it an institution that had 400 cases versus 50 cases, did they do better?
Lastly, did insurance status or type of insurance impact complication rates? Private insurance versus government insurance versus the uninsured?
Dr. Matthew M. Hutter (Boston, Massachusetts): Your first question was about how were laparoscopic procedures that were converted to open procedures handled. The NSQIP database is limited by its reliance on CPT codes and it depends on how each hospital codes the procedure for this situation. I attempted to see how different institutions handled this issue, and found that some tended to code it as a laparoscopic procedure, if the majority of the case was done laparoscopically, (partially because the CPT code for a laparoscopic procedure is reimbursed higher). Others would code this as an open procedure. This is a potential limitation. I am not sure to what degree this will affect the results. It depends upon the conversion rate. At our institution where there is a conversion rate of approximately 2%, if you were to extrapolate that to the 400 cases here, that would mean eight cases that could be shifting from one group to another. It is an issue and it is a limitation, and thanks for pointing that out.
The second question was about the results from certain surgeons who perform mostly open procedures and then dabble in laparoscopy or other surgeons who do mostly laparoscopic procedures and then dabble in open procedures. The data that we have are by institution and not by surgeon, so we are not able to evaluate that surgeon-to-surgeon variance, just the hospital variation.
The third question, addressed whether a volume-outcome relationship was evident from this data. Analyses were done to look for a volume-outcome relationship, by breaking the hospitals into quartiles ranging from low to high volume institutions. Multivariate regression modeling using this volume variable did not show a statistically significant volume-outcome relationship with respect to complications or mortality. I did not present that data in my talk.
Your last question, I believe, was whether results, when stratified by insurance status, showed any differences. The type of insurance is not captured by this data set. However, I think this is a very important question, especially in light of the recent CMS proposal. A week ago CMS—the center of Medicare and Medicaid Services—came out with a memorandum proposing non-coverage for bariatric surgery for patients over 65. This was based partially on results reported by Dave Flum at the American College of Surgeons meeting in October, and published in JAMA, which looked at weight loss surgery in the Medicare population. The NSQIP does not have information about the insurance status, but I was able to break results down by age. Contrary to Dave Flum's study, our study did not find a significant difference in death or complication rates in patients over 65. Thank you Todd for your questions and comments.
Dr. Bruce D. Schirmer (Charlottesville, Virginia): I have a few questions for Dr. Hutter and a few comments.
This seems like a carefully selected group of patients. Half have an ASA rate of less than 3, the DPT rate for over 1300 patients is zero, and the wound infection rate for the open group is under 1%. The average weight of the lap group is under 300 pounds and the open group just over 300. While we have seen the early experiences of many institutions with carefully selected patient populations for laparoscopic and perhaps even open bariatric surgery, how many of these institutions have a long track record in doing bariatric surgery?
Second is a sequel question, and with apologies to the Carpenters, but where have all the cases gone? This study includes 17 hospitals for 4 years and only 401 lap bypasses were reported, yielding an average of less than 7 cases per hospital per year. For the open cases, it would be about 15 per hospital. Do you feel this group is, with this sampling, projecting an accurate picture of the outcome?
Now, my comment. We have this excellent paper demonstrating a zero and 0.6% mortality in open and lab bypasses. We have Dr. Flum's recent JAMA paper describing a 2% mortality in Medicare patients. Who do we believe? I think the answer is they are both correct and believable. It depends on who walks through your clinic door, whom you choose to operate on, whether you would be willing to do the high-risk patients, and whether you can and should based on your outcomes.
We recently submitted an abstract from our own institutional data, which confirmed a significant advantage of a laparoscopic approach in terms of overall complications and especially wound complications and incisional hernias. The differences are dramatic. Anybody who does lap cholecystectomy knows that for the obese patient the benefits over open surgery are more pronounced than for thin patients. The same is true for appendectomy, and it is becoming apparent the same is true for bariatric surgery.
So you have done wonderfully well, documented your outcomes, scientifically showing that the laparoscopic approach to bariatric surgery is better. Will it make a difference for our patients? Will we have some scientific panels or other insurance company's equivalent group still find that there are not enough data to substantiate the performance of laparoscopic bariatric surgery? Unfortunately, the answer may depend more on how the company's earnings have been doing or whether they have to contain costs than on the data.
Tort reform is recognized by our profession as the current largest problem we all face, because it ultimately leads to denial of access to care. But that denial of access to care pales in comparison to the 99% of people who are eligible for but do not receive the potential benefits of bariatric surgery annually. We may do the best science in the world and report the greatest surgical outcomes, but until the stranglehold of the insurance companies to access of care is broken, that may all go for naught for some of our patients.
Dr. Matthew M. Hutter (Boston, Massachusetts): Dr. Schirmer, your first question was about patient selection, and about how long the institutions in this study had been doing bariatric surgery. The hospitals in the Patient Safety in Surgery study of the NSQIP are mostly tertiary care, academic institutions, though it does include some private hospitals. The data is hospital specific, but I was blinded as to which specific institutions were which. I therefore cannot speak for the cumulative weight loss surgery experience at each specific institution, except for the data in this study.
As for patient selection, I agree with your analysis of the data that this seems to be a carefully selected patient population. And I am happy about that. That is the way it should be, I think. Data collection here started in 2000, which is relatively early in the weight loss surgery experience for some institutions, especially the laparoscopic experience. They should have been starting with cases that are less challenging, and then they can broaden their selection criteria as they gain more experience. Perhaps it is partially due to patient selection that we are seeing the excellent results we see here. I am in no way saying we should deny surgery to the high-risk patient who might just benefit the most from it. These high-risk operations should be performed by the right people in the right setting. It is exactly this kind of selection that is key for patient safety, and which has been advocated by several different groups, including the Betsy Lehman Center Report from the Massachusetts Department of Public Health, the ASBS and their Centers of Excellence program, and the American College of Surgeons.
Where have all the cases gone? I think that is a good question as well. I think the key point, as demonstrated in the first graph that I showed, is that there has been an exponential rise in the number of cases being done. The data set that I was looking at was early in this ascent. Though the numbers are not what they could be, they do provide the power to make the statistically significant findings that I just showed. In the last year and a half, there have been an additional 2,000 bariatric surgery cases collected by the NSQIP. And this is only a sample of the cases that are being done. If we increase data collection to 100% of cases done, include bariatric specific data points, and continue to collect data after 30 days, then this is going to be very powerful information. This is exactly what the ACS Bariatric Surgery Center Network and the ASBS Centers of Excellence programs are planning to do. From these future data sets, we will be able to draw much more powerful conclusions, including robust risk adjustment and meaningful outcome analyses to help determine which institutions should be operating on which patients.
Dr. Patrick O'Leary (New Orleans, Louisiana): I am in awe of your presentation and of the data that you presented. Tim Fabian this morning talked about “pearls among swine,” but anytime you have an opportunity to review a paper that has to depend on a “goodness test” or a “bootstrap analysis” and then use “optimism” as a measure of validation, I know that you are presenting solid data. I just don't know that I understand the words.
My concern is if this sample of hospitals, in fact, represents what is happening in America. It is probably, as Bruce Schirmer has suggested, that this evaluation may be outdated. If I were to opine, the number of laparoscopic bariatric procedures done today it is probably 4:1 over the open procedures. Your data showed laparoscopic procedures to be only one fourth of the cases done. The incidence of diabetes in your series is lower than I think I see in my patients. I am also a little concerned about the data that you showed are at variance to the Washington state data that David Flum has produced.
At the beginning, you stated that the hospitals that you evaluated were in the private sector, but in the latter part of your manuscript you described most of the patients were from large academic health sciences centers. I wonder: what is the demographics of the hospital set for those 15 hospitals that actually responded? Do they reflect the current American surgical experience? Or, in fact, are they just a subset?
Dr. Matthew M. Hutter (Boston, Massachusetts): Dr. O'Leary, thank you for your kind comments. As for your question, about whether this data reflects the current American surgical experience, I think the short answer is “no”. These are mostly academic hospitals. Yes, they are in the private sector, but I was distinguishing the private sector from the VA hospitals, and was not referring to private practice. The 18 hospitals that I am talking about are academic centers with high volumes of all different kinds of surgical procedures. There are four different community hospitals that have been included in the Patient Safety in Surgery Study of the NSQIP, but these hospitals were added in the more recent years, so their data is, for the most part, not reflected here. The results therefore are not entirely generalizable. Nonetheless, these multi-institutional findings are much more generalizable than the single institution studies which make up the majority of the published literature. The quality of this data, collected by trained, audited nurse-reviewers armed with standardized data definitions, is much more powerful than the quality of the data collected by administrative data sets.
To your question about the percentage of laparoscopic cases, yes, I showed that 30% of the cases were done laparoscopically and 70% open. More recent data shows that those percentages have been reversed. When I looked at the NSQIP data for gastric bypasses for the most recent 9 months, I found that 77% were done by the laparoscopic approach, and the remaining 23% were done open.
And that brings up the question: “Why the change from laparoscopic to open?” This change has not been driven by data reported in the literature that laparoscopic or open is better than the other, because there is no such data in the literature. Is this reversal in the laparoscopic and open ratios because of the media attention of the laparoscopic gastric bypass—because it was printed on the cover of People magazine that Al Roker, and other celebrities, had their procedures done laparoscopically? Is that how we are going to determine how our operations are done—by the media and by consumer demand? Hopefully not. Hopefully we will put some science behind it. And that was the attempt here.
Dr. John M. Kellum (Richmond, Virginia): At our single institution, we have performed over 3800 gastric bypasses, including more than 1000 laparoscopic gastric bypasses. I would agree with Dr. O'Leary's experience that in the last 4 years over 80% to 90% of our operations have been laparoscopic. My one concern is that a raw complication rate is of limited value. For example, a trocar site abscess would have equal weighting with an anastomotic leak.
We, too, have found that laparoscopic gastric bypass is associated with a lower incidence of marginal ulcer, a lower wound infection rate, and a dramatically lower incisional hernia rate. On the other hand, the more important, or arguably the most important, and life-threatening complication was anastomotic leak. We actually found that leaks were more common in the laparoscopic group, although any individual patient having a leak was less likely to die of a leak if he had had a laparoscopic gastric bypass. Another serious complication, small bowel obstruction, was more common in the laparoscopic group.
My one question is, did you stratify your complication results for specific complications to give weighting to the morbidity of each of these complications?
Dr. Matthew M. Hutter (Boston, Massachusetts): As far as assessing the complications themselves, that is something we could not address with this data set.
A wound infection is counted equally on this overall aggregated complication rate as an anastomotic leak. One of the other issues is that anastomotic leak, as well as other bariatric surgery specific preoperative comorbidities and postoperative outcomes, are not included in the NSQIP data. These are definite limitations to this study. The bariatric specific data set that has been developed for the ACS-NSQIP Bariatric Surgery Center Network addresses all these issues and will provide much more meaningful data in the future.
Dr. Kellum, I also congratulate you on your 3,800 cases that you have done so far. I hope that you have a robust data collection system, and that going forward you join with either the ASBS or the American College of Surgeons data collection systems—or wouldn't it be even better if these were one and the same data collection systems—so that the power of the information from your surgical volume can be harnessed in order to get some valuable information about weight loss surgery, that will allow us to make this surgery safer and more effective for our patients.
Dr. Joseph B. Cofer (Chattanooga, Tennessee): I rise to ask a question that has nothing to do with laparoscopic bypass surgery but has to do with the process. As an institution that is currently in the process of getting into NSQIP ānd proud to be there, I might add, I think it is a wonderful experiment Ī just wanted to ask you about the process.
Your abstract, I believe, mentions 12 institutions. I thought I saw 15 in your presentation. I think Dr. Schirmer mentioned 16. There were six authors. And it is presented under the aegis of the Massachusetts General Hospital.
My question is: who owns the NSQIP data? As we go forward into this experiment, what is the process maybe you can't answer this what is the process whereby an investigator gets permission to go into the NSQIP database and get the data and present it from, I assume, at least eight other hospitals who weren't on your slide. Can you explain that process to me?
Dr. Matthew M. Hutter (Boston, Massachusetts): Your question about who owns the NSQIP data is a very good question. The way it has worked for the NSQIP Patient Safety in Surgery Study, which was done through an AHRQ grant, was that a publication committee was set up to help determine the appropriate dissemination and evaluation of the data. For each NSQIP institution, there is a surgeon investigator, and each surgeon investigator is able to request specific aggregated, national, de-identified data sets that include results from all participating institutions. An investigator gets IRB approval from their institution, then sends in a two page proposal to the publication committee, who will then consider this and all other requests equally. Based on the merit of the proposal, and the ability to do the proper analysis, they will then divvy out the data.
So the data definitely are available to any of the investigators from any of the hospitals that enroll in the NSQIP. Actually, right now, most of this information is still not analyzed, presented, or published. The fact that there are 60,000–75,000 cases for which data has been collected, and we are hearing very few results from this so far, is a problem. This is very high quality, multi-institutional data, and it has a lot to offer to surgical knowledge. More and more hospitals are signing up for the NSQIP through the ACS, and investigators at these hospitals need to know that the national data sets are available to them.
Footnotes
Reprints: Matthew Murray Hutter, MD, MPH, Massachusetts General Hospital, Department of Surgery, Division of General and Gastrointestinal Surgery, 15 Parkman Street, Wang ACC 335, Boston, MA 02114. E-mail: mhutter@partners.org.
REFERENCES
- 1.Hedley AA, Ogden CL, Johnson CL, et al. Prevalence of overweight and obesity among US children, adolescents and adults, 1999–2002. JAMA. 2004;291:2847–2850. [DOI] [PubMed] [Google Scholar]
- 2.Wittgrove AC, Clark GW, Tremblay LJ. Laparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases. Obes Surg. 1994;4:353–357. [DOI] [PubMed] [Google Scholar]
- 3.Liu JH, Zingmond D, Etzioni DA, et al. Characterizing the performance and outcomes of obesity surgery in California. Am Surgeon. 2003;69:823–828. [PubMed] [Google Scholar]
- 4.Flum DR, Dellinger EP. Impact of gastric bypass surgery on survival: a population-based analysis. J Am Coll Surg. 2004;199:543–551. [DOI] [PubMed] [Google Scholar]
- 5.Buchwald H, Avidor Y, Braunwlad E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–1737. [DOI] [PubMed] [Google Scholar]
- 6.Flum DR, Salem L, Elrod JB, et al. Early mortality among Medicare beneficiaries undergoing bariatric surgical procedures. JAMA. 2005;294:1903–1908. [DOI] [PubMed] [Google Scholar]
- 7.Zingmond DS, McGory ML, Ko CY. Hospitalization before and after gastric bypass surgery. JAMA. 2005;294:1918–1924. [DOI] [PubMed] [Google Scholar]
- 8.Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA. 2005;294:1909–1917. [DOI] [PubMed] [Google Scholar]
- 9.Podnos YD, Jimenez JC, Wilson SE, et al. Complications after laparoscopic gastric bypass: a review of 3464 cases. Arch Surg. 2003;138:957–961. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen NT, Goldman C, Rosenquist J, et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg. 2001;234:279–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Westling A, Gustavson S. Laparoscopic vs. open Roux-en-Y gastric bypass: a prospective, randomized trial. Obes Surg. 2001;11:284–292. [DOI] [PubMed] [Google Scholar]
- 12.Lujan JA, Frutis MD, Hernandez Q, et al. Laparoscopic versus open gastric bypass in the treatment of morbid obesity: a randomized prospective study. Ann Surg. 2004;239:433–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blue Cross and Blue Shield Association. Technology Evaluation Center, vol. 18, no. 10. September 2003. [Updated vol. 20, no. 5, August 2005].
- 14.Fink AS, Campbell DA, Mentzer RM, et al. The National Surgical Quality Improvement Program in non-veterans administration hospitals: initial demonstration of feasibility. Ann Surg. 2002;236:344–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henderson WG, Mosca C, Denwood R, et al. Patient Safety in Surgery Study: Statistical Progress Report. Chicago, March 25–26, 2003.
- 16.Khuri SF, Daley J, Henderson W, et al. The National Veterans Administration Surgical Risk Study: risk adjustment for the comparative assessment of the quality of surgical care. J Am Coll Surg. 1995;180:519–531. [PubMed] [Google Scholar]
- 17.Khuri SF, Daley J, Henderson W, et al. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk adjusted, and peer-controlled program for the measurement and enhancement for the quality of surgical care. Ann Surg. 1998;228:491–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khuri SF, Daley J, Henderson W, et al. Risk adjustment of the postoperative mortality rate for the comparative assessment of the quality of surgical care: results of the National Veterans Affairs Surgical Risk Study. J Am Coll Surg. 1997;185:325–338. [PubMed] [Google Scholar]
- 19.Daley J, Khuri SF, Henderson W, et al. Risk adjustment of the postoperative morbidity rate for the comparative assessment of the quality of surgical care: results of the National Veterans Affairs Surgical Risk Study. J Am Coll Surg. 1997;185:339–352. [PubMed] [Google Scholar]