Abstract
Introduction:
An effective trauma system should offer patients triaged to a trauma center (TC) a survival advantage and cost-effective treatment. Three questions were asked: 1) Does treatment at a TC versus a nontrauma center (NTC) improve survival? 2) Is the system cost-effective? 3) Is access to the system equitable?
Methods:
The 2003 Florida discharge database identified patients with ICD9 codes 800 to 959. Survival risk ratios (SRR) were calculated using1999–2000 data and ICISS were produced for each code. Using 2003 data, mortality rates were calculated for matched patients at TCs and NTCs. Instrumental variables methodology was used to account for differences in mortality risks of patients triaged to TCs versus NTCs. Logistic regression analysis was used to determine differences in mortality. Charge/cost ratios were analyzed to compute the cost care and cost/life saved. Accessibility to a TC within 85 minutes of injury was assessed.
Results:
Treatment at a TC was associated with an 18% reduction in mortality. Mean costs of care in TCs and NTCs were $11,910 and $6019, respectively. Dividing the mean cost difference by the reduction in mortality yields a cost of $34,887/life saved. A total of 42% of patients returned to work within 24 months of injury. Using an expected median of 19 years of employment for a 33-year-old individual and proposed state funding figures for the trauma system, a life saved results in an approximate annual cost to the state of between $100 and $500. Currently, 95% of citizens of the state have access to the trauma system within 85 minutes of injury; however, only 38% of trauma patients are triaged to a TC. Addition of 3 TCs would increase these percentages to 99% and 65%.
Conclusions:
Triage to a Florida TC is associated with a decreased risk of death. Moreover, cost/life year saved is favorable when compared with societal expenditures for other health problems. Improved deployment of TCs is necessary to optimize access. This assessment methodology is a useful model for evaluation of mature trauma systems.
Florida's mature trauma system was evaluated examining access to care, mortality in nontrauma centers versus trauma centers, and whether the system is cost-effective.
The necessary components of an inclusive trauma system were first outlined in the Model Trauma Care Systems Plan published by the U.S. Bureau of Health Resources Development in 1992.1 In an inclusive system, patients with minor to moderate injuries may be treated at nontrauma centers (NTC) with the goal of matching the needs of the patient to the resources of the facility. One of the necessary components of the system is periodic evaluation to assess performance of the system and to determine if modifications are required.2–4 This evaluation may be difficult because of a number of factors. First, accurate data may be difficult to obtain because, while the trauma centers (TC) maintain trauma registries, there are no requirements for nontrauma acute care hospitals to maintain a database of trauma patients.5,6 Second, it may be difficult to demonstrate a survival advantage attributable to treatment at a TC because in a mature trauma system with adequate triage, delivery of seriously injured patients to TCs means that the patients with the largest risk of dying will be clustered in these centers.7 Thus, it would not be unexpected to observe an increased or unchanged mortality risk in TCs in a mature system.8–11 In addition, a “halo effect” may be seen with the maturation of a trauma system. This effect results in improved survival of injured patients regardless of whether they are treated at a TC.12 Shortened EMS response times, improved prehospital medical control, and the performance of airway and resuscitation interventions by emergency medical services personnel have been demonstrated to improve clinical outcomes whether the patient is transported to a TC or a community hospital.13
Finally, the assessment of the cost-effectiveness of a trauma system relies on the return of trauma victims to a productive life. This requires longitudinal follow-up of large groups of patients. This may be difficult to achieve given the limited data sources available. Because of these challenges, few studies have been able to evaluate the effectiveness of mature inclusive trauma systems.
The Florida trauma system was established in 1982 when legislation was passed requiring the Florida Department of Health (DOH) to designate individual TCs based on the American College of Surgeons standards. The Roy E. Campbell Trauma Act, passed in 1990, set up a system of state approved trauma centers. In 1998 the DOH's Bureau of Emergency Medical Services (EMS) provided a report to the legislature entitled “Timely Access to Trauma Care,” which examined the feasibility of establishing a prehospital triage plan to ensure that trauma patients were transported to the closest appropriate TC. This report laid the groundwork for Florida to establish an inclusive trauma system in 1999 when legislation was passed directing the DOH to plan, coordinate, and establish a 5-year plan for a statewide trauma system.
Despite having a long-standing trauma system, Florida has never provided a durable source of funding to support the system. Cost and manpower concerns have resulted in tensions within the trauma system such that over the life of the system the number of trauma centers has declined from a high of 66 TCs in 1987 to 21 TCs in 2004. During 2003 to 2004, 2 additional trauma centers were threatened with closure. One of these centers was 1 of the 6 level I centers for the state and the only center serving a city with a population of nearly 1 million. This crisis was solved, at least temporarily, by a coalition of local government and hospital leaders who were able to arrange funding for support of trauma patient care.
State government support of the Florida trauma system has taken the form of an annual appropriation to each trauma center as well as favorable payment methodologies for trauma centers via the Medicaid insurance system. In May 2004, Governor Bush vetoed the funding bill that would have continued the annual award of grants providing equal amounts of money to each trauma center. In the veto message, the Governor cited the potential inequities of a funding method that awards a set amount to each trauma center regardless of the number of patients served, the absence of a clear plan for the future deployment of trauma system resources, an absence of a clearly articulated plan for consistent local participation in the financial support of the trauma system, and the need to document the effectiveness of the trauma system. Regarding the issue of effectiveness, the Governor stated “Trauma centers save lives, but so do hospitals that are not designated trauma centers. What is the difference derived from adherence to our (trauma system) regulations? If state government is to initiate trauma center unique payments, we must first know we are paying for performance.” The surviving legislation from this bill mandated a study to be funded to ascertain the need for local and state funding for the trauma system, determine the best deployment of the system, and provide outcome data to ensure that the system does confer a survival advantage.
The purpose of this paper is to outline the methodology used to evaluate a mature inclusive trauma system such as the one found in the state of Florida and to answer 3 questions: 1) Does treatment at a TC versus a NTC improve survival? 2) Is the system cost-effective? 3) Is access to the system equitable?
MATERIALS AND METHODS
Overview
This is a population-based study. Because the state of Florida does not require NTCs to maintain trauma registries, data were obtained from the Florida Agency for Health Care Administration (AHCA), which maintains a database on admissions to all Florida hospitals. This database includes information on the patients’ age, sex, race, up to 9 ICD-9 codes and procedures, and the discharge status of the patient. The AHCA data sets from 2001 to 2003 were queried to identify all patients with ICD-9 codes of 800 to 959. From this group of patients the following diagnoses were excluded: 1) elderly patients with femoral neck fractures resulting from a fall (age >65 ICD-9 code 820.xx), 2) patients with a single injury that had no potential for mortality, 3) admissions not classified as an emergency, 4) patients with diagnoses relating to the insertion of foreign objects into body orifices, 5) patients admitted for complications occurring from a previous trauma, 6) patients admitted as a transfer from another acute care hospital, 7) patients discharged to another acute care hospital and patients discharged to hospice care or a nursing home, and 8) patients with a length of stay less than 24 hours who had no intensive care unit charges. The study group consisted of patients with the following injuries: 1) patients with fractures of the skull, neck, trunk, intracranial injury, and spinal cord injuries (ICD-9 codes 800–809, 850–854, 952), 2) other fractures (810–819, 821–829), 3) internal injury of the thorax, abdomen, or pelvis (860–869), 4) injury of blood vessels (900–904), and 5) burns (940–949). These patients were defined as “true trauma” patients for the purposes of the study.
The International Classification Injury Severity Scores (ICISS) methodology was used to estimate the severity of injury and the risk of mortality for patients admitted to Florida hospitals.14–16 Survival risk ratios (SRRs) for specific injuries were calculated from the AHCA database for the 3 years prior to the study (1998–2000). ICISS for patients with multiple injuries were calculated as the product of the individual SRRs.
Mortality
The ACHA data set for the 3-year period 2001 to 2003 was used to identify “true trauma patients” as defined above. The data was examined for structural breaks using the Chow test in a linear specification model (P < 0.01).17 This test indicated that the elderly population (age >65 years) was systematically different from the rest of the trauma population as they have a higher risk of comorbid disease and a disproportionally higher mortality than younger patients. In addition, only 3.8% of elderly trauma patients with an ICISS <0.75 were treated at NTCs compared with 21.8% treated in TCs. Because the overall number of elderly patients with severe injuries treated at NTCs was small, it was not possible to perform a meaningful statistical analysis of this patient population. For these reasons, the elderly were excluded from the mortality analysis.
Comparisons of mortality between TCs and NTCs may be further complicated because once a trauma system is established, a selection bias may exist whereby the more severely injured patients are preferentially transported to a TC. To the extent that selection bias is present the TC population will be systematically different from the NTC population. This bias must be controlled to compensate for measurement error inherent to variables used to approximate injury severity. The endogenous variable in the analysis is defined as dichotomous, with values of one or zero for, respectively, nonsurviving or surviving patients. A logistic estimator is used to determine the odds of mortality:
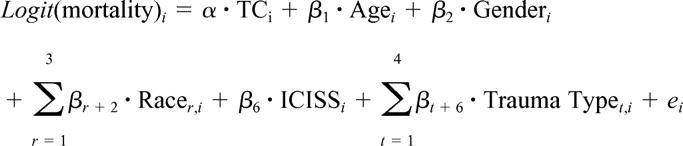 |
In the specification, the subscripts i, r, and t indicate, respectively, the individual patient, the ethnicity of that patient, and the type of trauma that resulted in hospitalization.
Since it is not possible in practice to randomize trauma patients to treatment at a TC or a NTC, as in a conventional clinical trial, special care must be applied to constructing the statistical analysis using the logistic estimator. A well-established method to deal with the selection bias is known as instrumental variables: in this case the observed admission to a TC is replaced by an “instrument” that is correlated with the selection (treatment at a TC) but is not independently related to the odds of mortality. This has the effect of creating an analysis with case matched controls.18–21
Instruments must pass 2 tests: theoretical and statistical. The elements that make up the instrument were chosen on theoretical grounds based on 3 factors. The first is geographic residence location, which is itself independent from the expected mortality but is highly correlated to the probability of transport to a DTC. Thus, the first element of the instrument is based on the relative distance of the individual's residence to the nearest TC. Similarly, the time of an injury is itself independent of the risk of mortality. This assumption forms the basis of the second instrument which is dichotomous with a value of one if the injury took place during a weekend. The probability of transport to a NTC decreases during weekends as staffing levels at those facilities are not as assured during those times. The third instrument is the overall number of injuries. The literature suggests that the number of injuries is itself an extremely poor predictor of mortality. This last instrument is not as theoretically “clean” as the previous but was demonstrated not to enter the equation directly.
In statistical terms, the instruments must 1) be as strongly correlated as possible to the probability of treatment at a DTC, and 2) they must be independent of the probability of mortality. The first criterion is easily tested by the joint significance of the instruments. The second is tested using a χ2 statistic that tells whether any of the instruments should have been included in the primary equation. If they should have been in the primary equation, they cannot be considered independent of mortality. The instruments included in the first stage model include distance, weekend injuries, and the number of injuries. The distance variable contains 6 intervals indicating whether the center of the patient's zip code was within 10, 20, 30, 40, and 50 miles from a TC. The estimated coefficients associated with the instruments in the first stage equation were: distance −0.004 (P < 0.0001), weekend injuries 0.057 (P = 0.08), and the number of injuries 0.03 (P < 0.001). The F-statistic for overall significance of the first stage regression was 185 (P < 0.001). These tests indicate that the instruments are not invalid.
The introduction of instruments tends to produce underestimated standard errors. True standard errors are obtained using the bootstrapping method. Bias-corrected standard errors for the estimates were derived using bootstrapping with 1000 repetitions. Convergence took place at approximately 500 repetitions. All P values reported were derived using this method.
Cost
Cost-to-charge ratios were derived from the AHCA hospital financial characteristics dataset for the year 2002, the last year for which cost data were available. The ratios were calculated for each individual hospital based on the institution's reported total direct costs associated with inpatient care and the total charges levied to patients. Because capital costs and expenses for nondirect patient care activities, for example, finance and other operations, are not included, the cost estimates tend to be biased downward. Moreover, the cost ratio estimates apply to all hospitalizations including nontrauma cases, which tend to be less costly, therefore causing further downward bias in the estimates. For these reasons, the cost estimates used in this paper should be interpreted as lower bounds. A separate estimate of the fixed cost of operating a TC was obtained from the “Medicare Cost Reports” of 18 of the 21 TCs. These figures include the costs of uncompensated care as well as “preparedness costs” for such things as maintaining operating rooms, radiology suites, emergency departments, and personnel staffing including physicians, 24 hours a day 7 days a week.
Access
Access to care was estimated by obtaining each county's population, growth statistics, and area in square miles from the 2004 Florida Statistical abstract. The number of advanced life support (ALS) vehicles, emergency medical technicians (EMT) and paramedics per county was obtained from the DOH. This information was used to calculate each county's ALS vehicles, EMTs, and paramedics per 1000/population and per 100 square miles. Air medical services were identified through EMS air licenses on file at the DOH, and through the Association of Air Medical Services Directory and the Atlas and Database of Air Medical Services. Trauma volumes, population, and prehospital resources were analyzed by Domestic Security Task Force (DSTF) regions. This analysis was used to identify areas of population that lacked access to the trauma system and to make recommendations about the placement of additional trauma centers. Data for access to care was obtained from the AHCA data set for the year 2003 only.
RESULTS
Trauma Demographics and Access to Care
In the year 2003, Florida had 20 TCs and 221 NTC hospitals. TCs consisted of 6 level I centers and 14 level II centers. Florida does not designate level III centers. All level I trauma centers were also pediatric trauma centers. A level I center was added at the University of Florida, Shands Hospital, Gainesville in 2004. This hospital was not included in the mortality analysis. On average, TC hospitals were larger in overall bed size averaging 590 hospital beds in contrast to 210 beds at NTC hospitals. Thirteen of Florida's 67 counties had a trauma center, and 6 counties had more than one TC. In 2003, TCs, on average, served 10 counties and level I centers served 22 counties. The geographic distribution of TCs and the number of trauma patients served per county are illustrated in Figure 1.
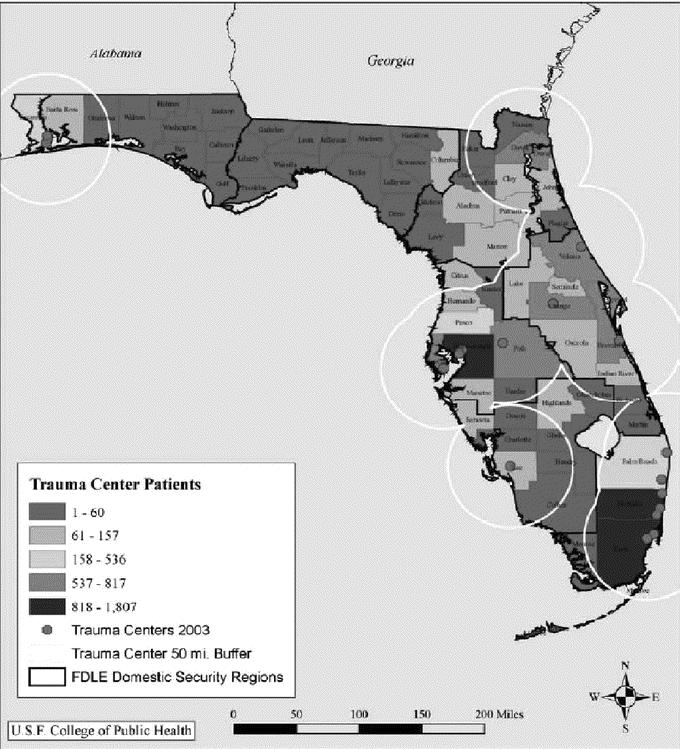
FIGURE 1. Distribution of trauma center patients by county of residence, 2003.
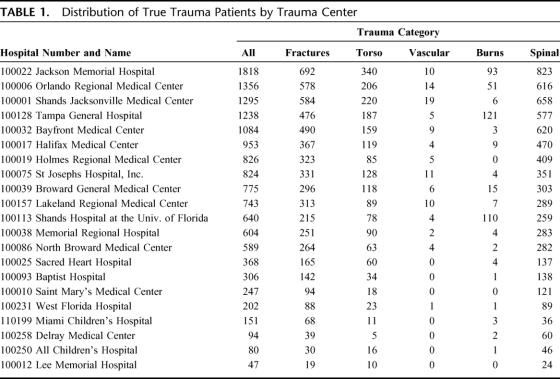
During calendar year 2003, 2,422,655 discharges took place from Florida hospitals. State designated TCs provided care for 22% (n = 533,720) of all patients, trauma and nontrauma. There were 37,842 “true trauma” patients, as defined in the materials and methods section, treated at Florida hospitals in 2003. State designated TCs treated 38.3% (14,240) of these patients. Table 1 illustrates the distribution of trauma cases among the 21 designated trauma centers. This analysis underestimates the actual number of “true trauma” patients treated at TCs because of problems associated with the coding of patients in the AHCA data set. Two TCs (Lee Memorial and All Children's Hospital) recorded approximately 1800 and 600 trauma patients respectively in their trauma registries for the year 2003 but were listed as treating only 127 patients total in the AHCA database. The effects of miscoding on the proportion of patients treated in TCs versus NTCs are unknown because the NTC do not keep trauma registries with which the AHCA data can be compared.
TABLE 1. Distribution of True Trauma Patients by Trauma Center
Finally, the age distribution of trauma patients treated at TCs and NTCs is different. The TC population reflects the traditional bell-shaped curve peaking for the ages 21 and 45 years (Fig. 2). The NTC population is skewed toward elderly patients with less severe injuries as demonstrated by the fact that 96.2% of elderly patients treated at NTCs had a survival probability between 0.75 and 1 compared with 78.2% at TCs.
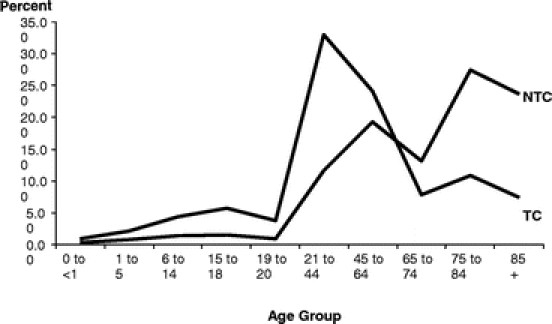
FIGURE 2. Age distribution of all trauma discharges.
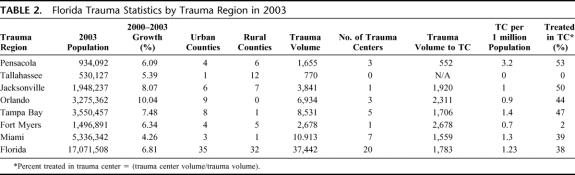
Florida's Domestic Security Strategy was developed as a comprehensive approach to address and limit potential vulnerabilities related to acts of terrorism and natural disasters. These efforts are organized around 7 DSTF regions. In July 2004, the state created trauma regions that are coterminous with these DSTF regions. Demographic data regarding Florida's 7 DTSF regions including their corresponding populations, number of TCs per region, and TCs per million population are listed in Table 2.
TABLE 2. Florida Trauma Statistics by Trauma Region in 2003
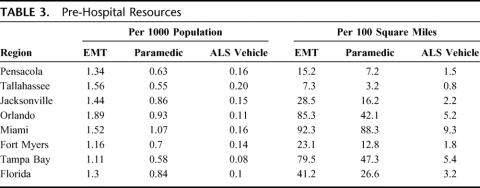
Prehospital resources are listed by DSTF region in Table 3. Areas with less than average resources are listed in bold print. In 2003, the ratio of paramedics to population in Florida was 1 to 1163 in urban counties and 1 to 1293 for rural counties. Air transport was available to approximately 80% of the population. Figure 1 demonstrates areas within a 50-mile buffer of a trauma center. Assuming an average speed of 45 mph, a 15-minute scene time, and a 5-minute dispatch time the majority of the population had access to TCs within 85 minutes. When areas served by air transport using a 75 mile buffer zone are added, 95.7% of the population of the state is within 85 minutes of aTC.
TABLE 3. Pre-Hospital Resources
Mortality
The AHCA database for the years 2001 to 2003 was used to compare mortality between TCs and NTCs. There were 415,709 admissions to Florida hospitals with an ICD-9 code of 800–959. Patients with admission diagnoses related to foreign objects in body orifices, complications of previous injuries, or the late effects of injuries were excluded. All cases with a single injury associated with an ICISS of 1.0 were also excluded. The latter exclusion criterion had the effect of excluding the majority of pediatric patients as these patients tended to have single injuries that were not associated with mortality.
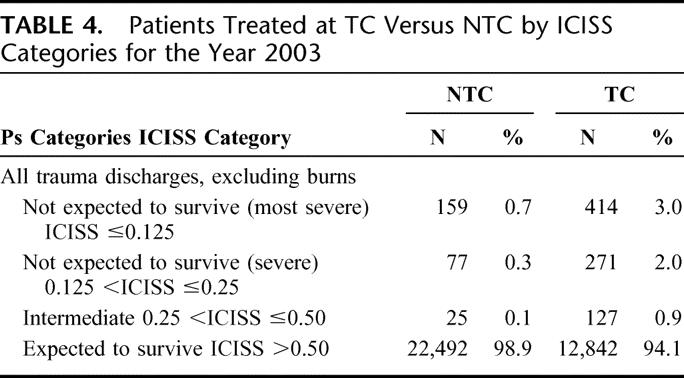
After these exclusions, 105,527 patients with an ICISS scores ≤0.99 remained for the 3-year period; an average of 35,176 “true trauma” patients per year. Analysis of the distribution of patients for the year 2003 indicate that as expected in a mature trauma system the most severely injured patients are preferential directed to the trauma system (Table 4).
TABLE 4. Patients Treated at TC Versus NTC by ICISS Categories for the Year 2003
The AHCA database allows for the classification of admissions as elective, urgent or emergent. As the primary interest was in the outcome of patients with injuries associated with a significant risk of mortality who would have required trauma team activation at a TC, patients whose admission was not classified as emergent were excluded. This criterion resulted in the majority of exclusions to the 105,527 “true trauma” patients treated over the years 2001 to 2003. Patients discharged to another short term hospital, admitted as a transfer from another short term hospital, or discharged to a hospice or nursing home were excluded because of the inability to control for the initial care that the patient received prior to transfer or discharge and because the survival status of patients discharged to other acute or long-term care facilities could not be determined. Finally, patients with a length of stay less than 24 hours and no ICU charges were excluded to prevent bias from patients who were moribund on arrival to the emergency room. Patients excluded for the latter reasons comprised about 3% of the “true trauma” patient exclusions. The final data set consisted of 21,854 patients of whom 98.3% were admitted through hospital emergency rooms.
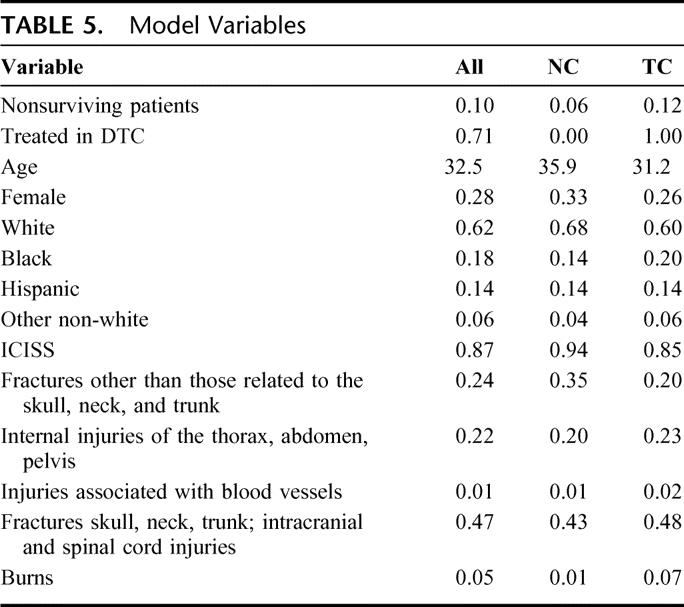
Table 5 contains the means and proportions of the model variables for all observations for patients treated at either TCs or NTCs. Nonsurviving patients make up 10% of the sample. The majority of patients in the sample (71%) were treated in TCs. The average age of patients in the sample is 33 years and the majority (72%) are male. The average ICISS score was 0.87.
TABLE 5. Model Variables
A 2-stage instrumental variables technique was used to adjust for the systematic bias introduced by the preferential transport of more severely injured patients to TCs. In the second stage of the analysis the variable TC* in the logistic estimator was replaced by the fitted instrument. (Table 6).
TABLE 6. Logistic Probability Regression Results
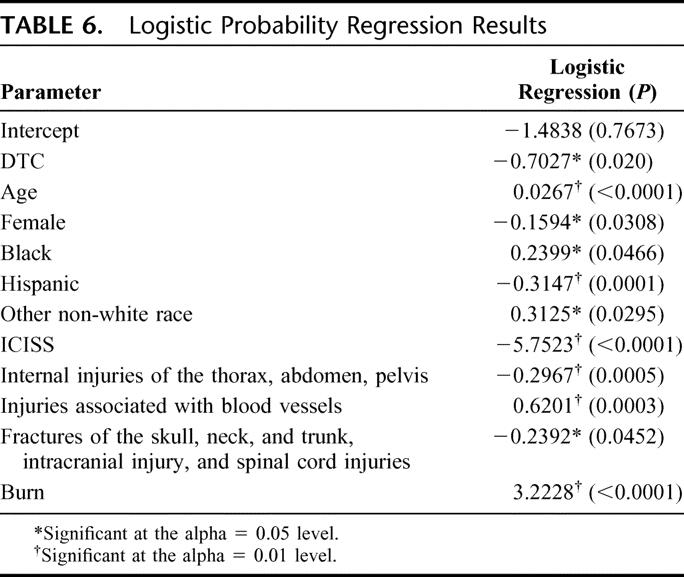
The focus of this paper is on the influence of TCs; therefore, the following provides only a brief summary of the findings related to the remaining factors. According to expectations, age has a highly significant and direct impact on the probability of mortality. Holding all other variables fixed, women face a lower risk of mortality. The severity of the injury, measured by the ICISS variable has the largest impact on the probability of mortality, both in terms of absolute magnitude and statistical significance. Vascular and, especially burn patients have a substantially higher risk of mortality as compared with general fractures.
The estimated coefficient associated with the trauma center variable (−0.7027) indicates a significantly lower risk of mortality for trauma victims treated in a TC after controlling for the confounding influence of age, gender, race, ICISS, injury type, and selection bias. Using the transformation
 |
the probability of mortality is estimated to be 0.185 and 0.364 for patients treated in a TC and a NTC, respectively. In this equation, the βs are the estimated parameters (Table 5) and the x's are the mean values of the explanatory variables (Table 6). The difference (0.178), or 17.8%, represents the decrease in the probability of mortality for trauma victims who receive treatment in a TC.
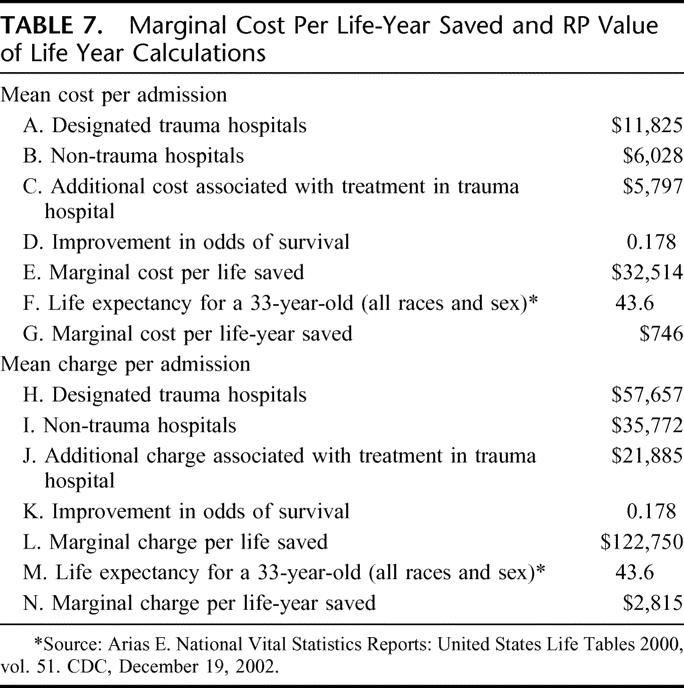
Cost Per Life-Year Saved
Table 7 lists both costs to the hospital and charges to the patient. The cost data may be interpreted as the lower bound and charges as the upper bound estimate of the expense of caring for a trauma patient. In both estimates, care at a TC is more expensive than at a NTC. Row C shows the marginal or added cost of caring for the average trauma victim at a TC compared with a NTC. Dividing by the marginal probability of death yields the marginal cost per life saved listed in row E. According to the CDC's National Vital Statistics Report of 2002, the expected remaining years of survival for a 33-year-old individual (the mean age of the patients in the sample) for all races and all sexes is approximately 43.6 years (row F). Dividing the marginal cost per life saved by the life expectancy yields the marginal cost per life-year saved. The marginal cost per life-year saved is $746 and the charge per life-year saved is $2815.
TABLE 7. Marginal Cost Per Life-Year Saved and RP Value of Life Year Calculations
Fixed Costs
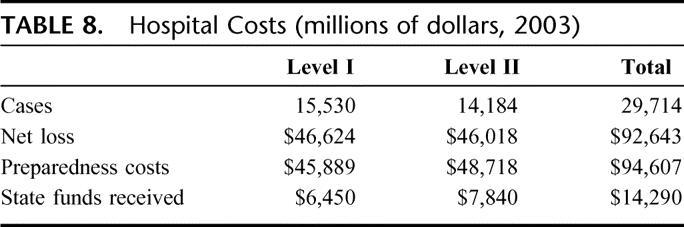
Indirect or fixed costs associated with being a TC were estimated from the Medicare cost.
Reports submitted by 18 of the 21 trauma centers for the year 2003. Net losses include cost for uncompensated care as well as preparedness costs minus funds received from the state (Table 8). The overall net loss for 18 TCs for the year 2003 was $92,607,000.
TABLE 8. Hospital Costs (millions of dollars, 2003)
DISCUSSION
In 2004, we received a mandate from the state of Florida to conduct a comprehensive assessment of its trauma system. This study concentrates on 3 aspects of that assessment: 1) evaluation of the system comparing outcomes of patients at TCs versus NTCs, 2) costs of the system, and 3) access to care.
Florida established an inclusive trauma system in 1998. Evaluation of Florida's trauma system is difficult because NTCs are not required to maintain a trauma registry. For this reason, we elected to use the AHCA data set, which contains ICD-9 codes for all patients admitted to acute care hospitals in the state of Florida. However, as in other population-based studies, there were a number of limitations associated with the use of this data set.6,8,22,23 First, there was a problem with miscoding. It was not possible to determine the degree of these coding errors for NTCs as no other data sources were available. However, when compared with the trauma registries at 2 TCs approximately 2200 patients listed in their registries for the year 2003 were not coded as “true trauma” patients in the AHCA database. This problem with miscoding did not affect any of the other 18 TCs.
In the mortality analysis, the intent was to study patients, at significant risk who would have required trauma team activation if treated at a trauma center. These patients represented about 20% of the patients with trauma ICD-9 codes as defined in the materials and methods section. Ninety-eight percent of these patients were admitted through the emergency room. Transfers were excluded from the analysis either because the effect of transfer on mortality from one acute care hospital to another could not be determined or because the patients’ final outcome could not be ascertained. However, transfers made up less than 3% of the patients and when a second logistic regression was performed including transfers there was no change in the study findings.
Based on the AHCA data it was determined that TC populations tended to be younger and more severely injured then NTC populations. The elderly with minor to moderate injuries tended to be concentrated in NTCs. Statistical analysis using the Chow test demonstrated that the elderly population (age >64 years) was structurally different from the younger trauma patient population. For this reason, elderly patients were not included in the mortality analysis. However, we did analyze mortality for the elderly trauma patients in a separate study (unpublished data). Overall mortality in the elderly at TCs versus NTCs was higher (8.6% vs. 3.8%). However, as with younger patients, the more severely injured patients tended to be concentrated in the TCs. The small number of elderly patients with severe injuries treated at NTCs did not allow for meaningful statistical analysis by ICISS quartile.
In Florida's mature trauma system, patients triaged to TCs are systematically different from NTCs. This bias in triage was corrected by a statistical technique (instrumental variables) that has the effect of creating a case-matching methodology.18–21 Using this methodology, a 17.8% improvement in survival was demonstrated associated with treatment at a TC versus a NTC for similarly injured patients. This is similar to the 15% to 20% improvement in survival associated with organized trauma care that Mullins et al found in their review of population-based studies.6
The cost of treatment at a TC was higher than at an NTC. The additional cost for treatment in a TC was between $5797 (cost) and $21,875 (charges). The marginal cost per life saved was between $32,514 and $122,750. This translates into a cost per life-year saved between $746 to $2815 using the mean age of this trauma population as 33 years and a mean life expectancy of 77 years. This compares favorably with the cost of treating other major healthcare problems. Examples of costs per life-year saved for widely accepted medical interventions include renal dialysis (approximately $50,000), implantable cardioverter-defibrillators ($30,000), breast cancer treatment ($22,000), coronary artery bypass ($26,000), and coronary artery angioplasty ($11,000).24–26 From a productivity standpoint, assuming that 42% of patients return to work within 2 years of injury and work for 19 years the cost per work/year gained is between $1708 and $5800. Currently, the median Florida yearly income is $30,446.27 Thus, for each trauma patient returned to work there is a 5- to 15-fold return of the investment.
In the state of Florida, as in other trauma systems, costs associated with maintaining TCs have been one of the major threats to the system. Using Medicare cost reports, it was estimated that for the 18 centers reporting financial data the net loss for the year 2003 was about $92 millions. This has had the effect of reducing the number of TCs over time and of discouraging additional hospitals from applying for trauma designation. The end result has been gaps in access to care in some areas of the state. At the time that data were collected for this study, Florida had no durable state funding for trauma care. Since this report was written, legislation has been passed that designates money collected for red light traffic violations and for fines collected, in which the driver is deemed at fault for traffic crashes that result in death or serious bodily injury, to be set aside for distribution to TCs. This legislation is expected to generate $10 to $30 million to be distributed among the 21 TCs based on a formula that takes into account the number of trauma patients treated, the severity of injury, and the presence of local funding for trauma care. This funding remains well below the estimated deficit of $92 million.
The state of Florida in the year 2003 had 20 TCs or about 1.23 TCs per million population. This is slightly higher than the 1.06 TCs per million population estimated by Mackenzie et al who did not include pediatric TCs in their analysis.28 TCs per million population based on DSTF regions ranged from 0 in the Tallahassee region (no TCs for a population of 530,127) to 3.2 in Pensacola (3 level II centers for a population of 934,092). This compares with a range of 0.19 to 7.8 level I and II TCs per million population reported per state by Mackenzie et al.28
Prehospital resources varied by region based in part on rural-urban mix. Counties with TCs tended to have fewer ALS vehicles per 1000 population, possibly reflecting shorter transport times and the presence of helicopter programs with ALS capabilities. Regions with less than average resources per 100 square miles tended to have more rural than urban counties.
National standards for triage rates to TCs in inclusive trauma systems have not been established. Nathens et al, in an assessment of trauma care in the United States, found that 56% of all trauma patients and about one third of severely injured patients were treated in NTCs.29 In Florida, 38% of eligible trauma patients were treated in TCs in the year 2003. With the addition of a level I TC at the University of Florida, this triage rate has risen to over 50%. Addition of 2 trauma centers in underserved areas in Bay County and Tallahassee would increase the triage rate to 59%. Secondary priorities are to add level II trauma centers in the Jacksonville and Orlando regions, which are currently served by level I centers with large trauma populations to bring the triage rate to TCs to 65%. Finally, the state of Florida does not have a limit on the number of TCs that may be designated. As TC performance has been linked to volume, it has been suggested that no more than one or 2 TCs are necessary per million population.28,30 In addition to improving performance, limiting the number of trauma centers decreases the duplication of expensive resources. This did not appear to be an issue for the Florida trauma system, except in the Pensacola area where there are 3 level II TCs with volumes ranging from 202 to 368 patients.
Branas estimated that, as of January 2005, 84% of Americans had access to a level I or II center within 60 minutes and that 69% had access within 45 minutes.31 Their analysis of Florida indicated that 78% and 94% of the population had access to a TC within 45 and 60 minutes, respectively. Our analysis, using a longer evacuation time of 85 minutes by ground or air, indicated that 95.7% of the population had access to a TC. This would be increased to 99.7% if TCs were added in Bay County and Tallahassee as previously discussed. Reassessment of the trauma system after these changes would be necessary to determine if the addition of TCs to further decease transport times would be cost-effective in an inclusive trauma system. Based on these assessments, prehospital transport times in Florida are better than the national average as would be expected in a mature trauma system and may have improved survival at both TCs and NTCs.
CONCLUSION
Patients admitted to TCs compared with NTCs tended to be younger and more severely injured based on ICISS. After adjustment for this systematic triage bias, there was an approximately 18% improvement in survival associated with treatment at a TC. This resulted in a marginal cost per life year saved of $746 to $2815. This cost compares favorably with other major public health expenditures. In this population-based analysis of a mature trauma system, access to TCs was better than the national average but could be improved further by the addition of TCs in underserved areas. Periodic assessment of trauma systems is necessary to assure that the system does confer a survival advantage and that it is cost-effective.
Discussions
Dr. Stephen M. Cohn (San Antonio, Texas): Trauma systems exist in approximately two thirds of states in the United States. They have been demonstrated to reduce the risk of death attributable to vehicular crashes by about 10%.
In this study, the authors found that the great majority of Floridians have rapid access to state designated trauma centers and that survival in these centers is better than at non-trauma centers, when controlling for contributing factors such as severity of injury and age.
Unfortunately, less than 40% of the injured were actually taken to trauma centers. The care of patients at trauma centers is more costly than at non-trauma centers. The estimated additional $2800 charge incurred per year life saved appears justified when compared to the costs of common interventions such as $26,000 for coronary bypass surgery per year of life saved.
I have got a few questions for the authors.
First, how confident are the authors that the database is accurate and how do you plan to improve the reliability of your data? For example, a level 1 trauma center, Lee Memorial Hospital, reported in your paper over 1800 trauma admissions in their trauma registry, but the ACHA database found only 47 trauma patients that were included in your analysis.
Second, most patients with severe injuries, those with less than a 75% predicted likelihood of survival by the International Classification Injury Severity Scores, were managed at designated trauma centers. In these severely injured patients, did they do better if they were managed at trauma centers? Also, what was the impact of trauma center care on patients with specific injuries that we are most concerned about, for example, severe brain injuries?
Third, if in fact the state of Florida decides to adequately finance verified trauma centers, who will control the number and site of these centers? In reviewing your data, there are some areas of Florida, such as Broward County, where there are quite a number of trauma centers with low patient volumes. Considering the limited funds available to support trauma care, should Florida limit the location of trauma centers to those specific facilities necessary to provide adequate access to optimal quality trauma care for the populace?
Finally, if the state financially supports trauma centers and they were located appropriately to optimize patient access, how would the authors ensure that the injured were actually taken to these hospitals?
I would like to thank the Association for the privilege of discussing this interesting paper, and commend the authors on completing this major investigation.
Dr. Rodney M. Durham (Tampa, Florida): As in any population-based study, it is only as good as the data you get. Non-trauma centers in the state of Florida do not keep trauma registries, so the only way that we could compare mortality between non-trauma centers and trauma centers was to use the ACHA database.
You correctly identified, as we did in the paper, that Lee Memorial had 1800 patients in their registry. About 50% of these patients were trauma alerts, which were the real population that we wanted to study. So that was about 900 patients that they had there. I think that 900 patients out of 21,584 patients didn't make a major difference. I will point out that none of the other 18 trauma centers had this problem in classification of their ACHA database. Most of that occurred because Lee Memorial failed to designate these patients as emergency admissions.
The comparison of the more severely injured patients’ mortality we did not look at. It was difficult to compare because of the differences in patient population served in trauma centers and non-trauma centers. The non-trauma centers tended to admit elderly patients with minor injuries, whereas the trauma centers tended to admit the more severely injured younger patients, so it was difficult to get major groups of patients in the non-trauma centers to perform a valid statistical analysis.
The same was also true for head injuries. These trauma centers tend to be large regional resources, and point of fact, most of the non-trauma centers don't have neurosurgical capabilities available. So it is very common that, head-injured patients are transferred immediately to a trauma center.
Who decides where the trauma centers are put? At the current time, the state does. Now, as you are aware, one of the West criteria is: does the state have the capability of limiting the number of trauma centers that are present? At the current time, the state of Florida does not limit the number of trauma centers present. This has not been a problem for the majority of the state because of the costs associated with trauma centers.
It has been a problem in the Pensacola area where for political reasons there are 3 level IIs for a population of about 1 million. Again, because of political reasons, we have not addressed that. In addition, if you look at the Pensacola Domestic Security Task Force Region, there is an area in Bay County, that doesn't have any trauma centers, and is far enough away from Pensacola that they were really one of the underserved areas that you looked at in the panhandle. That is one of the things that Dr. Lottenberg, who is here and is the trauma director for the state of Florida, will have to address at some point.
I think Florida actually has a fairly strong trauma system. Ensuring that the most severely injured patients are taken to trauma centers has not been a problem at the present because the non-trauma centers don't want anything to do with them. If it at some there actually becomes financial advantage to keeping these patients, then I think possibly the state would have to step in and look at where these patients are being treated.
Dr. Norman E. McSwain, Jr. (New Orleans, Louisiana): Once again, the outstanding group of trauma surgeons from Florida has given us a lot of data, and it has added to the care of the trauma patient nationwide by looking at their program.
I have a concern, however, that a lot of patients seemingly were carried to non-trauma centers which were trauma patients. And that would mean that the EMS personnel are undertriaging the patients and not carrying them directly to the trauma center or you don't have a good protocol for appropriately delivering the patient to the trauma center, or there may be some political reasons for this to occur. Could you address your pre-hospital assessment of patients and how you determine who goes to what hospital?
Dr. Rodney M. Durham (Tampa, Florida): We have some of the same concerns. If you look at Nathan's paper looking at access to trauma centers published in 2002, he actually stated that about 56% of trauma patients across the country are treated in non-trauma centers.
When we looked at our data and one of the reasons for doing this study was to look at access to trauma centers there were particular gaps in the panhandle, and at the time the study was started there was a gap in the middle of the state. Since that time, a level 1 trauma center has come online at the University of Florida in Gainesville, and currently our data indicate that about 50% of trauma patients are treated in trauma centers with the addition of this trauma center.
We have fairly standard triage criteria for transport to a trauma center. The problem has not been with the triage criteria; it has been the location of the trauma centers in the state. We have recommended an additional increase to 60% trauma center in Tallahassee which is well above the national average.
Dr. Steven M. Steinberg (Columbus, Ohio): I do have one question, and it has to do with the cost and charge data that you presented. Why did you compare the cost data from the trauma centers and the non-trauma centers? You made the point that the trauma centers are caring for a more severely injured patient population than the non-trauma centers. It only stands to reason that the cost per patient is going to be higher. I am afraid you might bias the politicians against the trauma centers a little bit if that data are looked at too superficially.
Dr. Rodney M. Durham (Tampa, Florida): I would agree with you. Unfortunately, the government had already figured out that the cost was more expensive in trauma centers than non-trauma centers. And we were trying to show them that indeed we were treating more severely injured patients and that it only costs about $746 per life-year saved to treat these patients at a trauma center versus a non-trauma center.
In addition, if you look at cost per life saved the cost was about $245 more at a trauma center versus a non-trauma center. And as mentioned earlier, this compares favorably with the cost data for other major health care, public health problems, like dialysis and coronary artery bypass.
In this era of pay for performance, the government is demanding this type of data before authorizing public funding of trauma systems.
Footnotes
Reprints: Rodney Durham, MD, Regional Trauma Center, Tampa General Hospital, P.O. Box 1289, Suite G417, Tampa, FL 33601. E-mail: rdurham@hsc.usf.edu.
REFERENCES
- 1.U.S. Department of Health and Human Services: Public Health Service Health Resources and Services Administration. Model Trauma Care System Plan. Washington, DC: U.S. Department of Health and Human Services, 1992. [Google Scholar]
- 2.Hoff W, Schwab C. Trauma system development in North America. Clin Orthop. 2004;422:17–22. [DOI] [PubMed] [Google Scholar]
- 3.Bazzoli G, Madura K, Cooper G, et al. Progress in development of trauma systems in the United States: results of a national survey. JAMA. 1995;273:395–401. [PubMed] [Google Scholar]
- 4.West J, Williams M, Trunkey D, et al. Trauma systems: current status-future challenges. JAMA. 1988;259:3597–3600. [DOI] [PubMed] [Google Scholar]
- 5.Chiara O, Cimbanassi S. Organized trauma care: does volume matter and do trauma centers save lives? Curr Opin Crit Care. 2003;9:510–514. [DOI] [PubMed] [Google Scholar]
- 6.Mullins R, Mann N, Hedges J, et al. Population-based research assessing the effectiveness of trauma systems. J Trauma. 1999;47(suppl):59–66. [DOI] [PubMed] [Google Scholar]
- 7.Flint L, Orban B, Durham R, et al. A comprehensive assessment of the Florida trauma system. Accessed on October 27, 2005.
- 8.Clark D, Anderson K, Hahn D. Evaluating an inclusive trauma system using linked population-based data. J Trauma. 2004;57:501–509. [DOI] [PubMed] [Google Scholar]
- 9.Reilly J, Chin B, Berkowitz J. Use of a statewide administrative database in assessing a regional trauma system: the New York City experience. J Am Coll Surg. 2004;198:509–518. [DOI] [PubMed] [Google Scholar]
- 10.Clark D. Trauma system evaluation using the fatality analysis reporting system. J Trauma. 2003;54:1199–1204. [DOI] [PubMed] [Google Scholar]
- 11.Rogers F, Osler T, Shackford S, et al. Population-based study of hospital trauma care in a rural state without a formal trauma system. J Trauma. 2001;50:409–414. [DOI] [PubMed] [Google Scholar]
- 12.Barquist E, Pizzutiello M, Tian L, et al. Effect of trauma system maturation on mortality rates in patients with blunt injuries in the Finger Lakes region of New York State. J Trauma. 2000;49:63–70. [DOI] [PubMed] [Google Scholar]
- 13.Melton SM, McGwin G, Abernathy J, et al. Motor vehicle crash-related mortality is associated with prehospital and hospital-based resource availability. J Trauma. 2002;54:273–279. [DOI] [PubMed] [Google Scholar]
- 14.Meredith W, Evans G, Kilgo P, et al. A comparison of the abilities of nine scoring algorithms in predicting mortality. J Trauma. 2002;53:621–629. [DOI] [PubMed] [Google Scholar]
- 15.Osler T, Rutledge R, Deis J, et al. ICISS: an international classification of disease-9 based injury severity score. J Trauma. 1996;41:380–388. [DOI] [PubMed] [Google Scholar]
- 16.Rutledge R, Osler T. The ICD-9-based illness severity score: a new model that outperforms both DRG and APR-DRG as predictors of survival and resource utilization. J Trauma. 1998;45:791–799. [DOI] [PubMed] [Google Scholar]
- 17.Chow G. Tests of equality between sets of coefficients in two linear regressions. Econometrica. 1960;28:591–605. [Google Scholar]
- 18.Goldman D, Bhattacharya J, McCaffrey D, et al. Effect of insurance on mortality in an HIV positive population in care. J Am Statist Assoc. 2001;96:883–894. [Google Scholar]
- 19.McClellan M, McNeil B, Newhouse J. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. JAMA. 1994;272:859–866. [PubMed] [Google Scholar]
- 20.McConnell K, Newgard G, Mullins R, et al. Mortality benefit of transfer to level I versus level II trauma centers for head-injured patients. Health Serv Res. 2005;40:435–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ressler R, Melissa S, Waters R, et al. Welfare payments and the spread of HIV in the United States. Contemp Econ Policy. 2005;23:40–49. [Google Scholar]
- 22.Mann N, MacKenzie E, Teitelbaum S, et al. Trauma system structure and viability in the current healthcare environment: a state-by-state assessment. J Trauma. 2005;58:136–147. [DOI] [PubMed] [Google Scholar]
- 23.Mann N, Mullins R, MacKenzie E, et al. Systematic review of published evidence regarding trauma system effectiveness. J Trauma. 1999;47(suppl):25–33. [DOI] [PubMed] [Google Scholar]
- 24.Bozic K, Rosenberg A, Huckman. R, et al. Economic evaluation in orthopedics. J Bone Joint Surg Am. 2003;85:129–142. [DOI] [PubMed] [Google Scholar]
- 25.Jauhar S, Slotwiner D. The economics of ICDs. N Engl J Med. 2004;351:2542–2544. [DOI] [PubMed] [Google Scholar]
- 26.Tengs T, Adams M, Pliskin J, et al. Five hundred life saving interventions and their cost-effectiveness. Risk Anal. 1995;15:369–390. [DOI] [PubMed] [Google Scholar]
- 27.U.S. Bureau of Economic Analysis. Survey of Current Business. U.S. Bureau of Economic Analysis, 2004. [Google Scholar]
- 28.Mackenzie E, Hoyt D, Sacra J. National inventory of hospital trauma centers. JAMA. 2003;89:1566–1567. [DOI] [PubMed] [Google Scholar]
- 29.Nathens A, Jurkovich G, MacKenzie E, et al. A resource-based assessment of trauma care in the United States. J Trauma. 2004;56:173–178. [DOI] [PubMed] [Google Scholar]
- 30.Nathens A, Jurkovich G, Rivara F, et al. Effectiveness of state trauma systems in reducing injury related mortality: a national evaluation. J Trauma. 2000;48:25–31. [DOI] [PubMed] [Google Scholar]
- 31.Branas C, MacKenzie E, Williams J, et al. Access to trauma centers in the United States. JAMA. 2005;293:2626–2633. [DOI] [PubMed] [Google Scholar]