Abstract
Objective:
To assess outcome differences between locally burned civilians and military personnel burned in a distant combat zone treated in the same facility.
Summary Background Data:
The United States Army Institute of Surgical Research (USAISR) Burn Center serves as a referral center for civilians and is the sole center for significant burns in military personnel. We made the hypothesis that outcomes for military personnel burned in the current conflict in Iraq and Afghanistan would be poorer because of delays to definitive treatment, other associated injury, and distance of evacuation.
Methods:
We reviewed the civilian and military records of patients treated at the USAISR from the outset of hostilities in Iraq in April 2003 to May 2005. Demographics, injury data, mortality, and clinical outcomes were compared.
Results:
We cared for 751 patients during this time period, 273 of whom were military (36%). Military injuries occurred in a younger population (41 ± 19 vs. 26 ± 7 years for civilian and military respectively, P < 0.0001) with a longer time from injury to burn center arrival (1 ± 5 days vs. 6 ± 5, P < 0.0001), a higher Injury Severity Score (ISS 5 ± 8 vs. 9 ± 11, P < 0.0001), and a higher incidence of inhalation injury (8% vs. 13%, P = 0.024). Total burn size did not differ. Mortality was 7.1% in the civilian and 3.8% in the military group (P = 0.076). When civilians outside the age range of the military cohort were excluded, civilian mortality was 5.0%, which did not differ from the military group (P = 0.57). Total body surface area (TBSA) burned, age ≥40 years, presence of inhalation injury, and ventilator days were found to be important predictors of mortality by stepwise regression, and were used in a final predictive model with the area under receiver operator characteristic curve of 0.97 for both populations considered together. No significant effect of either group was identified during development.
Conclusions:
Mortality does not differ between civilians evacuated locally and military personnel injured in distant austere environments treated at the same center.
The U.S. Army Institute of Surgical Research serves as a referral center for burned civilians and for all burned military personnel including those from the current conflict. We compared outcomes between these populations and found no significant differences despite the higher injury severity scores and an increased incidence of inhalation injury in the military group.
Historically, burns have comprised 8% to 10% of casualties sustained in post World War II conflicts,1–3 and vary based on the predominant type of weapon employed. Wartime injuries, including burns, in the current conflict in southwest Asia, known as Operation Iraqi Freedom (OIF) and Operation Enduring Freedom (OEF), are evaluated and treated within an echelon-based evacuation system, with initial first-aid rendered on site by embedded military medics (level I) who start intravenous resuscitation, control hemorrhage, and immobilize fractures. Injured military personnel are then transported to Forward Surgical Teams (level II), which include a surgeon and anesthetist who provide initial surgical stabilization prior to evacuation to Combat Support Hospitals (level III). The level III facilities contain surgical subspecialists, intensive care unit capability, and other advanced capabilities for further stabilization and treatment. From there, casualties are triaged for evacuation to military hospitals in the continental United States if further care will be required, transiting through Landstuhl Regional Medical Center in Germany (level IV), and finally for burn casualties, to Brooke Army Medical Center in San Antonio, TX, the home of the U.S. Army Institute of Surgical Research (USAISR) Burn Center (level V).
The USAISR serves as the sole referral center for all significantly burned active duty military personnel. The USAISRis notified of casualties by phone from the theater of operations, and depending on severity, can launch a Burn Flight Team of specialized burn care practitioners consisting of a physician, critical care nurse, licensed vocational nurse, respiratory therapist, and a noncommissioned officer to assist with evacuation. Otherwise, injured patients with less severe burns are evacuated using U.S. Air Force Critical Care Air Transport Teams (CCATT). The USAISR Burn Flight Team pioneered the aeromedical transport of seriously ill patients and has been flying missions around the world since 1951.4,5 For the current conflict, severely burned patients are met at Landstuhl Regional Medical Center close to Frankfurt, Germany, where the patient is further stabilized and flown to the burn center in San Antonio, TX. All further care for burned military personnel, including rehabilitation and reconstruction, take place at the USAISR.
The USAISR also functions as the civilian regional burn center in south Texas, serving an area of 80,000 square miles with 6,800,000 people. Patients are brought directly to the USAISR by Emergency Medical Services if burned locally, or if burned outside the immediate metropolitan area, are referred through a centralised referral system for medical emergencies in south Texas. Patients are transported to the USAISR where they receive all of their primary burn care. Patients also receive rehabilitation and reconstruction at the USAISR or are referred to practitioners closer to home if requested by the patient.
Since the USAISR serves as a burn care center for 2 distinct populations, we sought to compare them, with the initial hypothesis that outcomes would be poorer for the active duty military group because of the distance of evacuation, other associated injuries, and extended time to definitive care. We also sought to determine whether clinical outcomes for wartime burns were similar to those sustained in civilians. To address these aims, we compared demographics, burn characteristics, associated injuries, mortality, and clinical outcomes between the 2 populations.
METHODS
The records of all patients treated at the USAISR Burn Center in San Antonio, TX between April 2003 at the beginning of military hostilities in Iraq and May of 2005 were reviewed for patient and injury demographics, including age, gender, height, weight, burn size, anatomic distribution of burn, inhalation injury, and injury severity score. We also assessed clinical outcomes between groups for mortality, hospital length of stay, intensive care unit (ICU) length of stay, ventilator days, discharge disposition, and complications. All data were gathered by a single investigator (D.S.K.) and entered into Excel spreadsheets (Microsoft, Redmond, WA). Approval for the study was given by the Brooke Army Medical Center Institutional Review Board prior to commencement.
Height and weight were measured at admission. Burn size was assessed by completion of a Lund-Browder diagram6 by the attending surgeon at the USAISR, documenting the extent of injury in each body region. Inhalation injury was defined as a history consistent with inhaled toxic fumes and bronchoscopic verification of tracheal and bronchial damage. Injury severity scores (ISS) were calculated from the medical record, and were obtained from the Brooke Army Medical Center level I Trauma Center database. Mortality, hospital length of stay, ICU length of stay, and ventilator days were recorded from the medical notes. Dispositions included discharge to home, transfer to another acute care facility, transfer to a rehabilitation hospital, skilled nursing facility, or nursing home, discharged against medical advice, or death. Gross functional outcomes in survivors were assessed by the USAISR Rehabilitation Team at the time of first follow-up after discharge, and were described as good (previous level of function in activities of daily living), moderate (cares for self but not at the previous level of function and requires occasional assistance), or severe (requires daily care by others).
For civilian patients, resuscitation was begun en route under the direction of USAISR physicians once notified. Department of Defense personnel injured in the current conflict meeting American Burn Association Burn Center admission criteria were brought to the USAISR after receiving immediate care at the site of injury by trained medics and evacuated expeditiously as described above. The USAISR was notified of all significant burns received in the theater of operations, and those who were intubated and/or had burns over 20% of the total body surface area or at the discretion of the verifying flight surgeon are met in Germany by the USAISR Flight Team for treatment and transport to San Antonio by air. If the number of patients requiring transport was more than 4, the team was augmented by CCATT personnel.
Upon arrival at the USAISR, all patients were treated identically with intravenous resuscitation by the modified Brooke formula.7 Abdominal and extremity compartment pressures were measured every 4 hours or more often if indicated, and decompressed if above 25 to 30 mm Hg. Other injuries were identified and stabilized. Within 48 hours of arrival, patients were taken to the operating room for excision of full-thickness wounds with autograft coverage. If enough autograft was not available, remaining open wounds were covered with Integra (Integra Life Sciences, Plainsborough, NJ) or allograft skin until donor sites were healed and could be reharvested. Staged operations continued until the wounds were healed. Grafted wounds were treated with vacuum dressings, mafenide acetate soaks, or silver impregnated dressings until postoperative day 4 when the wounds were inspected and placed back into antimicrobial dressings until healed.
Patients at risk for airway compromise were intubated during resuscitation and underwent bronchoscopic evaluation for possible inhalation injury. Once any facial edema had subsided and ventilator settings were minimized, extubation proceeded if negative inspiratory force was greater than 30 mm Hg with the absence of tachypnea, hypercarbia, or hypoxia while on continuous positive airway pressure without ventilator breaths. Patients felt to be at risk for mechanical ventilation for more than 21 days underwent percutaneous tracheostomy. Ventilator days were counted as the number of days that the patient required machine-assisted breaths.
Patients remained hospitalized until they were ambulatory and taking an adequate regular diet, and wound care could be managed by the patient or the patient’s family. For civilian patients, outpatient treatment consisting of minor wound care and routine rehabilitation generally occurred at home with assistance from the family and/or Home Health services when available, enabling discharge which could occur on any day of the week. Once suitable for discharge, military patients were housed locally after assignment to the Medical Hold Brigade of Fort Sam Houston for Army personnel, or its equivalent, for the other services during outpatient treatment. These assignments were only made on weekdays; therefore, discharge was not possible on weekends and holidays. Outpatient minor wound care was performed by USAISR personnel or by the family.
Statistical Analysis
Data were analyzed using SAS version 8.1 (SAS Institute Inc., Cary, NC). Univariate analyses were performed using 2-sample Student t tests for continuous variables and χ2 tests for categorical variables. One-way ANOVA on ranks with Dunn’s test for significant differences was used for those with multiple comparisons and continuous data. Multiple logistic regressions with sequential stepwise selection were performed to identify significant predictors of mortality in the population. Pearson correlation coefficients were calculated to determine relationships between continuous variables, between dichotomous and continuous variables (point-biserial correlation), and between dichotomous variables exclusively (ϕ correlation). Statistical significance was attributed at P < 0.05 throughout. Continuous data are presented as mean ± SD unless otherwise noted.
RESULTS
Demographics
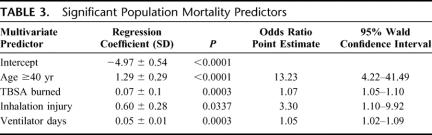
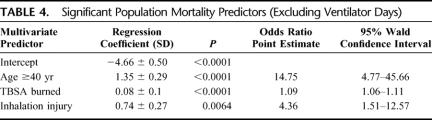
During the collection period from April 2003 to May 2005, a total of 751 patients were admitted to the USAISR Burn Center. A total of 273 (36%) of these patients were injured during military operations, of whom 106 were transported by the USAISR Flight Team from Germany. This population differed demographically from the civilian population in several ways. Military injuries occurred in a younger population (41 ± 19 vs. 26 ± 7 years for civilian and military respectively, P < 0.0001) with a longer time from injury to arrival to the burn center (1 ± 5 days vs. 6 ± 5, P < 0.0001). When considering only the military group because those with larger burns might be transported more expeditiously, we found that those grouped with total body surface area (TBSA) burns of 11% to 20%, 21% to 40%, and those with >40% burns all had shorter times of transport to the USAISR than those with <10% TBSA burns (P < 0.05) (Fig. 1). However, for each of these groups military patients still had statistically longer times from injury to arrival at the burn center than the civilian group. Military patients had a higher incidence of associated nonburn injuries (11% civilian vs. 37% military, P < 0.0001) resulting in higher mean overall ISS (ISS 5 ± 8 civilian vs. 9 ± 11 military, P < 0.0001, median 1 for civilians, 4 for military) (Fig. 2).
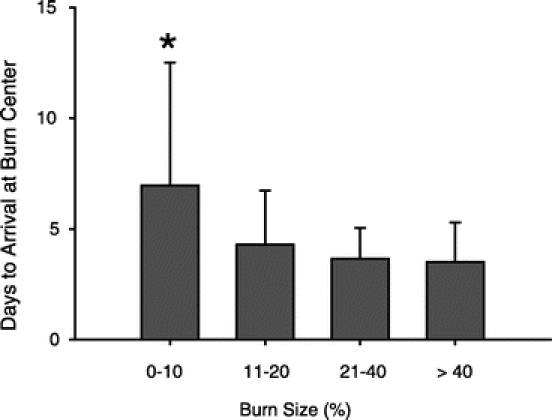
FIGURE 1. Bar graph of time to arrival for military patients at the USAISR Burn Center from the time of injury. *Significant difference from all other groups.
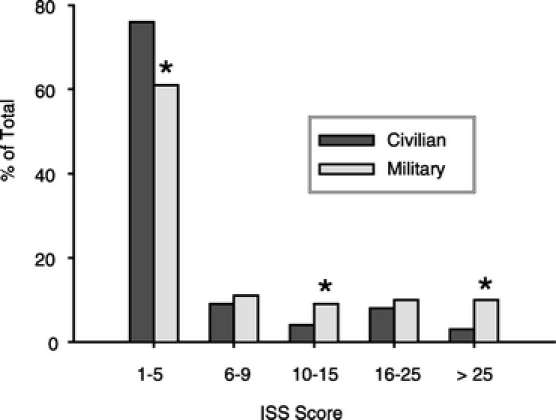
FIGURE 2. Bar graph of ISS scores grouped by severity. *P < 0.01 between groups by χ2 testing.
Burn Characteristics
TBSA burned did not differ between civilian and military populations, but the military group had higher mean full-thickness burns (P < 0.05). The median burn size was 9% TBSA in civilians, and 7% TBSA in burn military. In addition, inhalation injury was significantly more common in the military population (P < 0.05). Burn characteristics of the 2 populations are presented in Table 1. The mode of both populations was less than 10% TBSA burned (Fig. 3) and was similar between the groups. The anatomic distribution of burns differed between civilian and military, with military patients sustaining more head and hand burns and civilians more anterior chest, upper arm, and thigh burns (Fig. 4).
TABLE 1. Burn Characteristics of Military and Civilian Patients
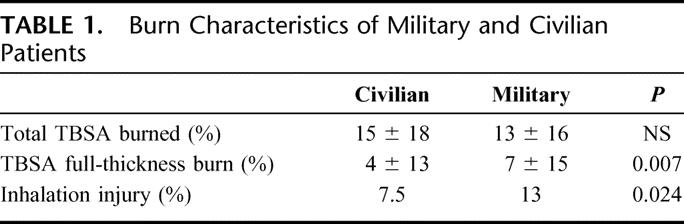
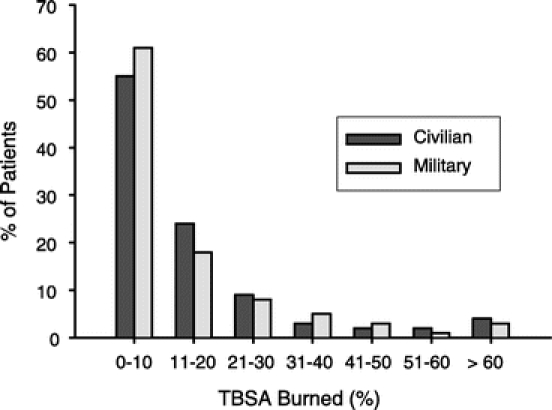
FIGURE 3. Frequency histogram of total burn size in military and civilian groups.
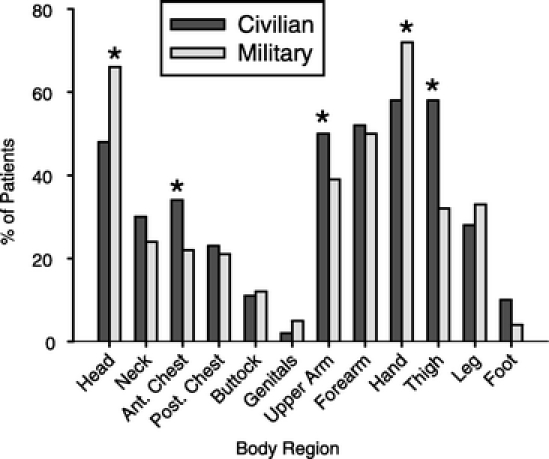
FIGURE 4. Anatomic distribution of burns in military and civilian cohorts. *Significant difference between groups.
Mortality
Overall mortality was 7.1% (34 of 478) in the civilian and 3.8% (10 of 273) in the military group (P = 0.08). When civilians outside the age range of the military cohort of 18 to 48 years were excluded, the civilian group mortality rate of 5.0% (16 of 323) was not significantly different significantly from the military group (P = 0.57). Civilian deaths occurred between 0 and 3 days of arrival in 12 patients (35%), between 4 and 14 days in 9 (26%), and 15 days after arrival in 13 (38%). The military burn deaths occurred between 0 and 3 days of arrival or 3 to 6 days from injury in 3 patients (30%), between 4 and 14 days (6–17 days from injury) in 3 patients (30%), and 15 days after arrival (>17 from injury) in 4 (40%). Only one death occurred in a military patient during evacuation from a combat support hospital in southwest Asia to the USAISR.
Among civilian deaths, the mean burn size was 47% ± 31% TBSA. When the younger subgroup comparable to the military cohort was considered, the mean burn size in those who died was 64% ± 25% TBSA. Among military deaths, the mean burn size was 55% ± 32% TBSA. When 2 outliers were excluded in the military cohort (one with severe ammonia gas inhalation injury and a 2% TBSA partial-thickness burn and one with a C1 spinal cord transection with a 7% TBSA partial-thickness burn), the mean burn size in those who died was 67% ± 6% TBSA.
Mortality Regression Analyses
Univariate comparisons were made between the subset of patients that survived and those that died, the results of which are on Table 2. Variables with a P value of less than 0.2 in the univariate analysis were entered into a logistic regression model. Injury Severity Score, ICU admission, total nonburn Acute Injury Score, hospital length of stay, and ICU days were highly correlated with other variables and were deleted from the model. Age and number of operations were converted to categorical variables with 2 levels (due to nonlinearity with the logit of death based on the Hosmer-Lemeshow goodness-of-fit test). Cutoff points were determined from the 95% confidence intervals during univariate analysis. The cutoff point for age was 40 years (95% CI for lived = 33.3–35.7; died = 45.1–51.4), and number of operations was 2 (95% CI for lived = 1.5–1.9; died = 2.3–3.5). In a stepwise regression fashion, the remaining candidate variables were sequentially entered and removed from the model until all significant predictors of mortality were contained.
TABLE 2. Univariate Analysis of Variables for Association With Mortality
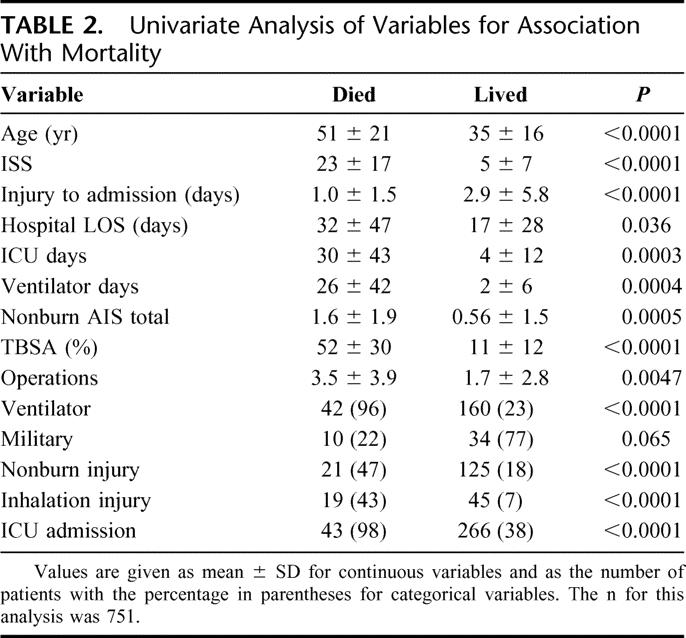
Four important predictors of mortality were found in this population: TBSA burned, age ≥40 years, presence of inhalation injury, and ventilator days (Table 3). Ventilator days was dropped from the model so the data could be used in a purely predictive fashion based on injury characteristics (Table 4), and compared with the model if ventilator days was included. The Hosmer-Lemeshow Goodness-of-fit test revealed no significant departure from good model fit for the model with (P = 0.92) and without (P = 0.99) ventilator days. The area under receiver operator characteristic curve was 0.97 for the model with ventilator days and 0.95 for that without (Fig. 5), indicating excellent predictive performance of the model both with and without this variable. Estimated odds ratios and their 95% confidence interval were determined by the maximum likelihood method. Because the model was developed using a combination of both populations, the area under the receiver operator characteristic curve was determined for the civilian and military separately. We found the areas to be 0.95 for the civilian group and 0.96 for the military, with no significant differences between the two.
TABLE 3. Significant Population Mortality Predictors
TABLE 4. Significant Population Mortality Predictors (Excluding Ventilator Days)
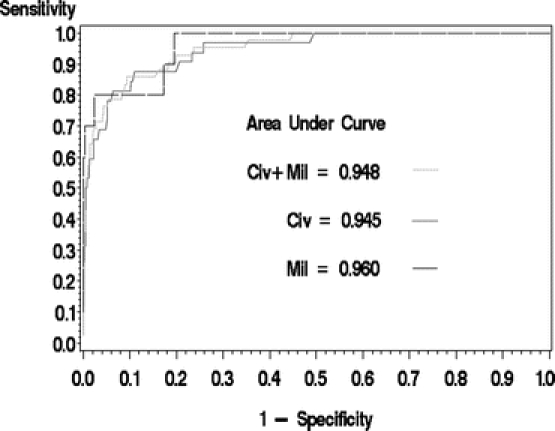
FIGURE 5. Receiver operator characteristic curve for mortality prediction by age, TBSA burned, and presence of inhalation injury. Three separate curves are shown, one with civilian and military patients combined, one with just civilian patients considered, and the last with only military patients considered.
Outcomes
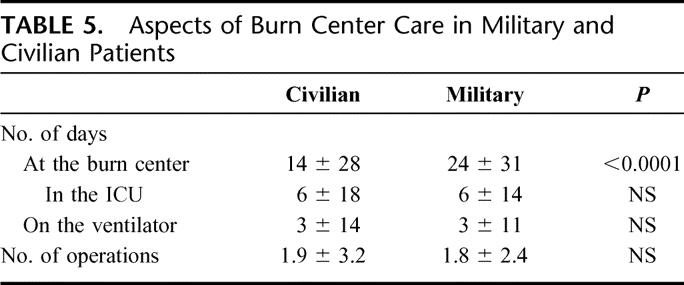
Results of univariate comparisons between aspects of burn center care for both cohorts are presented in Table 5. Military patients in this population had a longer overall hospital length of stay, although no difference was seen in length of ICU stay or in time spent on the ventilator. In addition, both cohorts underwent a similar number of operations (including excision and grafting, wound debridement, and other procedures such as fracture fixation). Of the patients in both groups with dispositions, most were discharged to outpatient care at home (91% of civilians and 96% of military patients); 6.1% of civilians and 1.6% of military patients were transferred from the burn center to an inpatient care facility (for rehabilitation, ongoing acute care, or skilled nursing). The remainder of patients had other dispositions, including inpatient transfer to another burn center (1 civilian), or leaving against medical advice (2 civilians). Gross functional outcomes were good (previous level of function in activities of daily living) in 94% of civilians and 92% of military patients. Gross functional outcomes were moderate (cares for self with some occasional assistance) in 5% of civilians and 6% of military, and severe (requires assistance with daily care) in 1% of civilians and 2% of military. No gross functional outcomes were statistically different between groups.
TABLE 5. Aspects of Burn Center Care in Military and Civilian Patients
DISCUSSION
This is the first analysis of differences in outcomes between civilian and military patients treated at the same center during a military conflict. In this analysis, we showed that results such as mortality and gross function after discharge did not differ between civilian and military despite group dissimilarities for age (higher in the civilian group), full-thickness burn (higher in the military group), inhalation injury (higher in the military group), and associated nonburn injuries (higher in the military group). When age was controlled by excluding all civilian subjects outside the range of age for the military group (18–58 years), any perceptible differences further diminished in size. Analysis of variables associated with mortality revealed again that age, burn size, inhalation injury, and number of days on the ventilator were the best predictors of mortality. These data show that outcomes similar to that of civilians can be predicted for evacuated military patients despite burns sustained in austere environments in combat situations.
Interestingly, we found that total burn size was similarly distributed across both populations at approximately 15% TBSA burned. However, the extent of full-thickness burns was higher in the military group, which might be explained by the different distribution of burn mechanism. In this conflict, many injuries have been from explosions, which generate high amounts of heat in a flame ball as well as blast overpressure and penetrating fragments.8 Most other injuries have been due to munitions and other flame causes (Kauvar DL et al, Journal of Surgical Research). Conversely, in the civilian population, burns were often due to other causes such as scalds with hot liquids and contact burns; flame burns were frequent but were generally not associated with explosions. These differing causes of burn have differing propensities to induce full-thickness wounds. The areas of the body burned were also different between the populations. Chest, upper arm, and thigh burns were more common in civilians, and head and hand burns were more common in the military. This is likely due to the presence of military personal protective equipment worn over the torso, head, eyes, arms, and legs. The entire face and the hands, however, are not as protected.
We found no differences in mortality between these groups even after excluding those above age 48 years (the oldest burned military patient), indicating that, once evacuated, similar mortality can be predicted for the civilian compared with the military patient despite longer time to definitive care, greater amount of full-thickness burns, higher incidence of inhalation injury, and more associated nonburn injuries. All patients were treated similarly after arrival at the burn center with early total excision of the burn wound, modern critical care techniques, and aggressive rehabilitation. An argument can be made, however, that the military group is also more suited for better outcomes because of better overall health prior to injury and on-site first aid rendered by trained medics immediately after the injury. These must be considered as systematic variables that cannot be controlled, and the reader will come to his/her own conclusions.
Time to arrival for definitive care, on average 5 days more for the military group, was certainly due to evacuations of over 7000 miles through several levels of care with up to 5 different treating teams. Even for patients with the most severe burns who might have been expected to have a more expeditious evacuation facilitated by the USAISR Burn Flight Team, the average was still 4 ± 2 days. These figures are important when considering how early excision, wound complications, sepsis, and metabolic complications have been noted to increase with greater time to definitive excision.9,10 However, we found average arrival time had no effect on mortality or number of operations. Total length of hospital stay may have been longer due to greater infectious complications, although this variable was not measured in this study. This concept is in keeping with the findings of Wu et al9 who demonstrated that length of stay was longer in those with delayed excision and grafting while mortality was not different.
Most burns sustained in the civilian sector are unintentional11 and are not commonly associated with additional injuries other than inhalation injury. Because burns in wartime are associated with active intent to do harm through any means possible, other injuries in addition to burn or inhalation injury might be expected. Indeed, we found that other injuries such as penetrating abdominal injuries and long-bone fractures were more common in the military group (11% for civilians vs. 37% for military) yielding higher Injury Severity Scores. Yet, despite the increased incidence of other injuries, we found no overall group differences in mortality or increased ICU stay or ventilator days. This is in contrast to the findings of Santaniello et al12 and Hawkins et al.13 who showed an increase in mortality when other trauma was added to burn. When nonburn acute injury score (AIS) and presence of nonburn injury were considered separately in a univariate analysis of mortality, a significant difference was found between those who lived and those who died. However, in developing an overall model predicting mortality, these variables were excluded because of covariance with burn size, inhalation injury, or ventilator days. A reason for this may be that burns and inhalation injury alone induce the majority of injury response requiring ICU care, making the other injuries insignificant in comparison when considering outcomes in this population, which was smaller than those considered by Santaniello et al12 and Hawkins et al.13 Nevertheless, we can conclude convincingly that the overriding factors to consider in mortality predictions, which might be used for triage of relatively young military patients in the far-forward levels of care, are primarily burn size and inhalation injury. In considering other outcomes, it must be noted that the total length of hospital stay, even after arriving at the burn center, was longer for the military patients. No discharges on weekends or holidays may have partially accounted for the longer stays, but treatment of other injuries must also be considered.
In our analysis of factors affecting mortality, we found that age >40 years, burn size, and inhalation injury were the most significantly associated, as have many others.14–17 However, we found that number of days on the ventilator was also included in the final model and improved the accuracy. Number of ventilator days has also been found to be highly significant among factors predicting mortality after severe burn in children.18,19 The same authors also included the development of sepsis in their final predictive model, which we did not measure. Among the variables that were initially significant between those survivors and nonsurvivors but were removed from the final model for covariance were the ISS and nonburn AIS, which were already discussed, and overall length of hospital stay, days in the ICU, and operations, which can be explained by covariance with burn size. The last univariate variable of initial significance was the length of time from injury to arrival to the USAISR, with less time being associated with higher mortality. Perhaps this was associated with those with larger burns taking less time in transit for both the civilian and military, and thus would be covariate with burn size.
In the overall analysis, we found that civilian burns and military burns treated at this center were similar in size, which is roughly akin to the average burn size reported from the ABA Burn Registry in 1995 (14% TBSA).20 We also found that the time to death in those who died, time on the ventilator, ICU stay, and functional outcomes were also roughly equivalent. These data have great significance in military casualty planning and show that the severity and outcomes of burns received using traditional weaponry are similar to those received in civilian centers. It also shows that military readiness for burn combat casualties can be maintained by operation of a military hospital that accepts civilian injuries.
In 1970, Allen et al from the 106th Hospital in Yokohama Japan reported results of treatment of burned patients from the Vietnam conflict.21 Almost all military personnel injured in Vietnam were evacuated through Japan, and this was the designated burn center. However, most patients were evacuated to this hospital after a prolonged stay in theater (up to 30 days, COL (retired) Basil A. Pruitt, personal communication). They found a mortality rate of 7.9% in 1963 burned patients treated in 1967 and 1968. This did not include the early deaths of patients treated in theater. We treated 273 patients from Iraq and Afghanistan in a 2-year period with a mortality rate of 3.8%, a 48% decline. This was statistically different with a P value of 0.016 by χ2. Analysis of changes in mortality by burn size was not done due to lack of statistical power in specified cells. These data indicate that indeed burn-related mortality has improved significantly since the Vietnam conflict perhaps due to more rapid and safe evacuation, early excision and grafting, and better critical care techniques.
CONCLUSION
We have shown that mortality is similar between civilians and military personnel injured in combat zones when treated at the same center despite higher incidences of other injuries, inhalation injury, and longer times to definitive care even when adjusted for age of the patients.
Discussions
Dr. David N. Herndon (Galveston, Texas): The authors have transported patients from an extremely austere environment, with almost 5 days in transport, with care by five or six different treatment teams, and show a similar morbidity and mortality to civilians that come directly to their burn center. This is a testimony to the military’s efficiency.
Although there are questions that can be brought up about delay in resuscitation experienced by the military patients, this deals with the initial hypothesis that such a tortuous route for young soldiers would cause difficulties. In particular, Dr. Wolf has shown in some elegant papers with larger burns and greater numbers that delay in resuscitation is a major contributor to mortality and morbidity in burn pediatric patients. I am wondering if this in particular series he was able to look at delay in resuscitation. Perhaps if he eliminates all burns under 10% in this analysis, extends the period of observation, and looks at more patients with severe injuries that would be predicted to die, his prediction equations could look at other factors.
As he has previously shown, during hospitalization the incidence of sepsis or the occurrence of sepsis grossly affects overall outcome. I do not see mention of sepsis in this study. I wonder if that was looked at.
Renal failure, heretofore a prominent cause of death in the Vietnam and Korea eras particularly, is not mentioned here, and might be of interest, as in Dr. Wolf’s other papers he did show that renal failure contributed significantly to morbidity.
With so many different treatment teams interacting with these traumatized patients, one might also wonder whether complications that are extremely pertinent to burn care, such as compartment syndromes from overresuscitation. Abdominal compartment syndromes or muscular compartment syndromes might have been increased in the population of the military patients. Perhaps again, the number of patients analyzed in this study with the degree of severity of injury is insufficient to unmask these particular effects.
One might ask whether there is a survivor effect. Though Dr. Wolf mentioned the patient who died in Landstuhl, are there any unrecorded deaths that might have mitigated against the outstanding and surprising results demonstrated here?
We have often noticed that patients who arrive from South America and Mexico, and in previous studies of your own with large burns survive as well as those admitted directly to our burn center. They may stay in hospitals a little bit longer than patients admitted directly. I often wondered about who died before they got here, and is this observation survival of the fittest or that the fittest survive?
I think your data could address that issue by going back to the original injury. I guess you have to eliminate those that die at the scene. That would be of some interest since your civilians almost entirely make it directly to the institution, although there are some mortalities at the scene there as well.
The other minor point, but one that really bears a little more discussion is the tremendous length of stay difference between the military and the civilians. As a taxpayer, I am particularly interested in this issue, Dr. Wolf, and maybe you could enlighten me as to the cause of this great disparity.
Dr. Steven E. Wolf (Fort Sam Houston, Texas): The first question had to do with IV access. Dr. Herndon and I did a study several years ago presented here, I believe, where we looked at deaths in children with greater than 80% burns and performed a large multivariate logistic regression, much more complex than we have done here, and found that time to IV access was a significant variable in determining who would live and die.
In the military patients, there is an embedded medic or corpsman with the unit that obtains IV access generally within 15 minutes, which is even better than it would be in the civilian population. So we did not analyze that. The emergency records for IV access also are not really reliable from way downrange.
In this study, we first wanted to show that civilians in the military are basically the same. So now we can take that and put them both together and do a more in-depth analysis to predict exactly who is going to live or die. Less than 10% total body surface area burns generally don’t. So we will take your advice and do that.
The second question had to do with the incidence of sepsis. My answer would be the same, in that we again wanted to make sure that the civilians and the military were the same. And we will go back and do another analysis of that hopefully in a future publication.
Renal failure during resuscitation, we have not seen that. We have had no incidences of renal resuscitation failure in the military patients coming back yet. However, as you can imagine, we have the converse problem which you brought up, which is overresuscitation, which I refer to as resuscitation morbidity. And because of the transfer between teams, strict attention to volumes being infused all the time is not optimal, so you occasionally end up with overresuscitation. Many of these soldiers are coming back with fasciotomies and the like and had some problems with that.
To address that issue, we are now undergoing a long-term project where we are going to automate resuscitation from the level of the FST on back where PDA machines assist practitioners in making changes in the IV fluid infusion rates based on the feedback from the patient to hopefully alleviate some of these problems.
We made a big point about looking for other deaths, as you would imagine. Because if we had half the people dying in the combat support hospital or there was a significant amount of deaths in the flights from the hospitals in Iraq to Landstuhl, that would, of course, have made a big difference. It turns out there is only the one from the FST and back.
For the length of stay issue. It is better than it was. Over the last couple of years, we have made significant improvements and great strides in this. And we will continue to do so.
Dr. P. William Curreri (Mobile, Alabama): Dr. Wolf and his associates have compared mortality and a variety of other morbid conditions in a civilian population and a military population of burned individuals admitted to the USAISR. They have very nicely shown that after age adjustment, outcomes are similar in both populations and that would be expected in a superior burn treatment center.
I had similar questions as Dr. Herndon regarding the information provided in your abstract. My concern was that, although at the USAISR outcomes were similar, it concerns me that there was a great difference in admission time to the USAISR in the two populations. That is, the civilian population was admitted at 24 hours, whereas the military burned individuals were admitted at 6 days.
My concern was: how many patients suffered morbidity or mortality with fairly significant injuries after that 24-hour period in the theater of operation or during evacuation? Maybe you could elaborate on that.
Dr. Steven E. Wolf (Fort Sam Houston, Texas): In admission time criteria, again, we had no deaths in between the FSTs, which is level 2 on up to our place, except for the one that I didn’t include in the analysis.
So that goes to show probably ānd this is a point that ought to be made īs that these are military guys, right? They exercise and are generally fit. And we are comparing them to a population of civilians who may or may not be fit. So it is a testament to how well young fit people can tolerate something like this or how well a person who is fit can tolerate a significant injury and that they do make it back okay. So the admission time, although we would like it to be less than that, for logistical reasons it is simply impossible to get them back any sooner than 4 days.
Now, as far as an increase in morbidity, yes, anecdotally these guys have an increased rate of fasciotomies and open abdomens as compared with civilians. And that is something that we have to deal with. And hopefully, with our automated resuscitation scheme, that may help.
Dr. John A. Morris, Jr. (Nashville, Tennessee): Do your burn excisions occur in theater in San Antonio? If they are occurring in San Antonio, does that give us some interesting other comparisons with the civilian population?
Dr. Steven E. Wolf (Fort Sam Houston, Texas): No burn excisions take place outside of San Antonio in military patients. What happens is they may get escharotomies and fasciotomies done anywhere downrange (outside of the continental United States). They don’t get excisions done downrange.
So the application then would be: what happens if you get excised 6 days later as compared to if you get done in the first couple of days? Dr. Herndon and I have done some of that work already and shown that indeed there doesn’t appear to be, at least in our hands, any difference in mortality, but there was a clear increase in the incidence in sepsis and more wound complications. So later excision does appear to increase morbidity in some studies. We did not use that in this study, however.
Dr. Loring W. Rue, III (Birmingham, Alabama): The reduction in mortality between Vietnam and the current era is impressive. Have you had a chance to look at the comprehensive database you maintain for the civilian experience during the Vietnam era?
Dr. Steven E. Wolf (Fort Sam Houston, Texas): We have not. And that is an excellent suggestion. We are in the process of digitizing all that information from the green books that you know about. When we have that, we may be able to make that same comparison from the Vietnam era.
Dr. Basil A. Pruitt, Jr. (San Antonio, Texas): You mention that a 20% or greater burn or a need for ICU care were the criteria for sending a team. Are there other criteria such as mechanical trauma, infections, or other complications that would influence your decision about sending a team to escort the patients to the Burn Center?
Another concern is the time of admission. In all studies of burn mortality, there is a real break in the slope of the death rate at 10 days. Consequently, if you want to look really good, you don’t admit a burn to your unit until they are 10 days or more post-burn. Your burns from the theater of operations came at an average of 6 days. What happened in that 6 days to the total of all patients burned in Iraq and Afghanistan? Since the casualty registry is still being developed by Dr. Holcomb, how do you know you picked up all the deaths that occurred before they got to you?
Finally, we read in the newspaper that it is often the improvised explosive devices that cause injuries. Consequently, there must be mechanical injury in some of the burn patients. Since most of the military burns were of limited extent (median size, 7% of the body surface), one would think that mechanical injury would have a predominant effect on mortality and I wonder whether you observed such.
Dr. Steven E. Wolf (Fort Sam Houston, Texas): The first question had to do with the criteria for deploying a “smart team,” which is the military terminology for any of these specialized teams. The burn team is just one of these. We have other ones for infectious disease and all kinds of other things.
Our deployment criteria are basically for those with greater than 20% total body surface area burns or those on a ventilator. If they happen to have other significant injuries, a head injury, for instance, and they are burned as well, they are most likely going to be on a ventilator. That is how we catch those patients as well.
The 10-day criterion is one that you have talked about before. The real question comes, though: how do we know we got everybody in those first 10 days? The military is good at recordkeeping ānd all of it is digital now s̄o we evaluated all of the downrange databases and scoured them if we had any other deaths. In fact, there was only one that was found, and we knew about it. This was a guy that we were getting ready to put on the plane and was not doing well, so turned around and went back to Landstuhl Medical Center with him, and he eventually died of hypotension and sepsis.
The last question had to do with mechanical injury. We were surprised by this as well. The military patients clearly had a higher incidence of other injuries associated with these explosions and bullets and what-not that are going on in a war zone, so we thought their outcomes would be different. However, that was not the case in that the other injuries in the stepwise regression ended up falling out as a predictor of mortality. Now that is for mortality, that is not for morbidity. So I think that is something we have to consider. But we do know, however, they didn’t need any more operations and they didn’t need any more time in the ICU, didn’t need any more time on the ventilator associated with these other injuries. But what is likely to come out is stuff during rehabilitation and reconstruction and do they have more needs long term, there more amputees, etc. And that will be the subject of further investigation by our group.
Footnotes
Supported by National Institute of General Medical Sciences Grant No. RO1-GM0633081.
The opinions or assertions contained herein are solely the views of the authors and should not be construed as official or reflecting the views of the Department of Defense or United States Government.
Reprints: Steven E. Wolf, MD, U.S. Army Institute of Surgical Research, Burn Center, 3400 Rawley E. Chambers, Building 3611, Fort Sam Houston, TX 79234-3611. E-mail: steven.wolf@amedd.army.mil.
REFERENCES
- 1.Cancio LC, Horvath EE, Barillo DJ, et al. Burn support for Operation Iraqi Freedom and related operations, 2003–2004. J Burn Care Rehabil. 2005;26:151–161. [DOI] [PubMed] [Google Scholar]
- 2.Sidel’nikov VO, Paramonov BA, Tatarin SN. Medical care for the burnt in modern local military conflicts. Voen Med Zh. 2002;323:35–39. [PubMed] [Google Scholar]
- 3.Shafir R, Nili E, Kedem R. Burn injury and prevention in the Lebanon War, 1982. Isr J Med Sci. 1984;20:311–313. [PubMed] [Google Scholar]
- 4.Kirksey TD, Dowling JA, Pruitt BA Jr, et al. Safe expeditious transport of the seriously burned patient. Arch Surg. 1968;96:790–794. [DOI] [PubMed] [Google Scholar]
- 5.Treat RC, Sirinek KR, Levine BA, et al. Air evacuation of thermally injured patients: principles of treatment and results. J Trauma. 1980;20:275–279. [DOI] [PubMed] [Google Scholar]
- 6.Lund CC, Browder NC. The estimation of areas of burns. Surg Gynecol Obstet. 1944;79:352–358. [Google Scholar]
- 7.Pruitt BA Jr, Mason AD, Moncrief JA. Hemodynamic changes in the early post-burn period: the influence of fluid administration and of a vasodilator (hydralazine). J Trauma. 1971;11:36–46. [DOI] [PubMed] [Google Scholar]
- 8.DePalma RG, Burris DG, Champion HR, et al. Current concepts: blast injuries. N Engl J Med. 2005;352:1335–1342. [DOI] [PubMed] [Google Scholar]
- 9.Wu XW, Herndon DN, Spies M, et al. Effects of delayed wound excision and grafting in severely burned children. Arch Surg. 2002;137:1049–1054. [DOI] [PubMed] [Google Scholar]
- 10.Hart DW, Wolf SE, Chinkes DL, et al. Effects of early excision and aggressive enteral feeding on hypermetabolism, catabolism, and sepsis after severe burn. J Trauma. 2003;54:755–761. [DOI] [PubMed] [Google Scholar]
- 11.Forjuoh SN. The mechanisms, intensity of treatment, and outcomes of hospitalized burns: issues for prevention. J Burn Care Rehabil. 1998;19:456–460. [PubMed] [Google Scholar]
- 12.Santaniello JM, Luchette FA, Esposito TJ, et al. Ten year experience of burn, trauma, and combined burn/trauma injuries comparing outcomes. J Trauma. 2004;57:696–701. [DOI] [PubMed] [Google Scholar]
- 13.Hawkins A, MacLennan PA, McGwin G Jr, et al. The impact of combined burn and trauma on patient mortality. J Trauma. 2005;58:284–288. [DOI] [PubMed] [Google Scholar]
- 14.Ryan CM, Schoenfeld DA, Thorpe WP, et al. Objective estimates of probability of death from burn injuries. N Engl J Med. 1998;338:362–366. [DOI] [PubMed] [Google Scholar]
- 15.Tobiasen J, Hiebert JH, Edlich RF. Prediction of burn mortality. Surg Gynecol Obstet. 1982;154:711–714. [PubMed] [Google Scholar]
- 16.Smith DL, Cairns BA, Ramadan F, et al. Effect of inhalation injury, burn size, and age on mortality: a study of 1447 consecutive burn patients. J Trauma. 1994;37:655–659. [DOI] [PubMed] [Google Scholar]
- 17.Moreau AR, Westfall PH, Cancio LC, et al. Development and validation of an age-risk score for mortality predication after thermal injury. J Trauma. 2005;58:967–972. [DOI] [PubMed] [Google Scholar]
- 18.Wolf SE, Rose JK, Desai MH, et al. Mortality determinants in massive pediatric burns: an analysis of 103 children with > or = 80% TBSA burns (> or = 70% full-thickness). Ann Surg. 1997;225:554–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spies M, Herndon DN, Rosenblatt JI, et al. Prediction of mortality from catastrophic burns in children. Lancet. 2003;361:989–994. [DOI] [PubMed] [Google Scholar]
- 20.Saffle JR, Davis B, Williams P. Recent outcomes in the treatment of burn injury in the United States: a report from the American Burn Association Patient Registry. J Burn Care Rehabil. 1995;16:219–232. [DOI] [PubMed] [Google Scholar]
- 21.Allen BD, Whitson TC, Henjyoji EY. Treatment of 1,963 burned patients at 106th General Hospital, Yokohama, Japan. J Trauma. 1970;10:386–392. [DOI] [PubMed] [Google Scholar]