Abstract
Objective:
Using meta-analytical techniques, the study compared postoperative adverse events and functional outcomes of stapled versus hand-sewn ileal pouch-anal anastomosis (IPAA) following restorative proctocolectomy.
Background:
The choice of mucosectomy and hand-sewn versus stapled pouch-anal anastomosis has been a subject of debate with no clear consensus as to which method provides better functional results and long-term outcomes.
Methods:
Comparative studies published between 1988 and 2003, of hand-sewn versus stapled IPAA were included. Endpoints were classified into postoperative complications and functional and physiologic outcomes measured at least 3 months following closure of ileostomy or surgery if no proximal diversion was used, quality of life following surgery, and neoplastic transformation within the anal transition zone.
Results:
Twenty-one studies, consisting of 4183 patients (2699 hand-sewn and 1484 stapled IPAA) were included. There was no significant difference in the incidence of postoperative complications between the 2 groups. The incidence of nocturnal seepage and pad usage favored the stapled IPAA (odds ratio [OR] = 2.78, P < 0.001 and OR = 4.12, P = 0.007, respectively). The frequency of defecation was not significantly different between the 2 groups (P = 0.562), nor was the use of antidiarrheal medication (OR = 1.27, P = 0.422). Anorectal physiologic measurements demonstrated a significant reduction in the resting and squeeze pressure in the hand-sewn IPAA group by 13.4 and 14.4 mm Hg, respectively (P < 0.018). The stapled IPAA group showed a higher incidence of dysplasia in the anal transition zone that did not reach statistical significance (OR = 0.42, P = 0.080).
Conclusions:
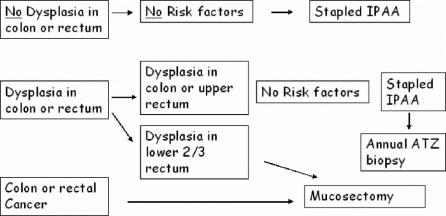
Both techniques had similar early postoperative outcomes; however, stapled IPAA offered improved nocturnal continence, which was reflected in higher anorectal physiologic measurements. A risk of increased incidence of dysplasia in the ATZ may exist in the stapled group that cannot be quantified by this study. We describe a decision algorithm for the choice of IPAA, based on the relative risk of long-term neoplastic transformation.
The present meta-analysis compared hand-sewn versus stapled ileal pouch-anal anastomosis among 21 studies between 1988 and 2003, comprising 4183 patients. Stapled anastomosis (n = 1484) had significantly improved nocturnal continence with higher anal resting and peak squeeze pressures than those with hand-sewn (n = 2699) anastomosis. The stapled group reported higher incidence of dysplasia in the anal transition zone.
Since the modern description of ileal-anal pouch in 1978, restorative proctocolectomy has become the procedure of choice for the majority of patients with ulcerative colitis who require surgery and for a proportion of patients with familial adenomatous polyposis.1 The initial description of the 3-limb ‘S’ pouch with a hand-sewn pouch-anal anastomosis following mucosectomy of the rectal stump was replaced within a short period of time by the 2-limb ‘J’ and the 4-limb ‘W’ pouch, which offered better functional outcomes in comparison with the S-pouch.2,3
Two types of ileal pouch-anal anastomosis (IPAA) have been described: a mucosectomy of the rectal stump followed by a hand-sewn ileal pouch-anal anastomosis.1 Since both ulcerative colitis and familial adenomatous polyposis coli are mucosal diseases, mucosectomy has the advantage of removing the diseased bowel mucosa, particularly if taken down to the dentate line.4 The alternative technique is to retain the mucosa of the rectal stump and perform a stapled pouch-anal anastomosis.5,6 This has the advantage of being quicker to perform, and it involves less manipulation of the anal canal, therefore reducing the risk of postoperative problems with continence.7
Both approaches have disadvantages. Mucosectomy requires greater manipulation of the anal canal with risk of damage to the sphincter mechanism and subsequent alteration in anal sphincter pressure.7 The mucosa of the anal transition zone (ATZ) has a rich sensory innervation, which is involved in discriminating between flatus and stool.8,9 This helps to maintain the anorectal, or ano-pouch, inhibitory reflex. One study reported that the ability to discriminate between flatus and stool was greatly diminished in patients undergoing mucosectomy.10 The stapled IPAA leaves potentially diseased and possibly inflamed rectal mucosa within the vicinity of the anastomosis, which may cause fecal urgency and requires regular follow-up of the ATZ due to the risk of dysplasia and cancer.11 It has been reported that 14% of patients undergoing mucosectomy had adenomas within the ATZ, compared with 28% who had a stapled anastomosis.12
The purpose of the present meta-analysis was to compare outcomes of hand-sewn versus stapled ileal pouch-anal anastomoses in patients undergoing restorative proctocolectomy for inflammatory bowel disease, familial adenomatous polyposis, or cancer. The specific aims of the study were: 1) to evaluate differences between the 2 anastomotic techniques in terms of postoperative complications, functional outcomes, anorectal physiology, quality of life assessment, and neoplastic transformation; and 2) to determine the degree of heterogeneity between studies reviewed.
METHODS
Study Selection
The literature was searched using Medline, Embase, Ovid, and Cochrane database for studies between 1988 and 2004 comparing hand-sewn (H) versus stapled (S) IPAA for patients undergoing restorative proctocolectomy for inflammatory bowel disease, familial adenomatous polyposis, or cancer. The following Mesh search headings were used “hand-sewn anastomosis and ileal pouch” and “stapled anastomosis and ileal pouch.” The following text searches and search headings and their combinations were used: “ileal pouch,” “hand-sewn anastomosis,” “stapled anastomosis,” “ileoanal anastomosis,” “ileal pouch anal anastomosis,” “ileum,” “anal canal,” and “anus.” The “related articles” function was used to broaden the search, and all abstracts, studies, and citations scanned were reviewed. No language restrictions were made. The references from articles were also used. The date of the most recent search was June 2005.
Data Extraction
Two reviewers (R.E.L. and V.A.C.) independently performed the search as well as reviewing and extracting the following data according to a prespecified protocol. First author, year of publication, study population characteristics, study design, inclusion and exclusion criteria, number of subjects, length of follow-up, and short-term and long-term outcomes were recorded.
Inclusion Criteria
Studies had to 1) compare hand-sewn versus stapled IPAA and 2) report on at least one of the outcomes mentioned below. When 2 studies were reported by the same institution, either the one of better quality or the most recent publication was included, unless the study outcomes were mutually exclusive or measured at different time intervals.
Exclusion Criteria
Noncomparative studies were excluded. Within the studies evaluated, endpoints that were not comparable, or it was impossible to calculate these from the published results, were excluded. Studies that displayed a “zero cell” for the outcomes of interest in both groups were excluded from the analysis but were taken into consideration when considering the total sample for the outcomes of interest.
Outcomes of Interest and Definitions
The following outcomes of interest were used to compare the 2 operative techniques:
Adverse outcomes: Anastomotic leak defined as the presence of contrast medium or fecal matter at the level of the anastomosis or ileal pouch during radiologic examination or reoperation. Pouch failure defined as excision of the ileal pouch reservoir any time during follow-up or indefinite proximal diversion. Wound infection defined as the presence of inflammation and/or purulent discharge and/or positive wound swab for bacterial growth. Postoperative mortality defined as death occurring within 30 days of operation from any cause. Additional adverse events studied included anastomotic stricture, pelvic sepsis, histopathologic, endoscopic, or clinical diagnosis of pouchitis, postoperative pouch-related fistulas, including pouch-perineal, pouch-vaginal, and pouch abdominal wall fistulae, failure to construct the pouch intraoperatively, small bowel obstruction, continuing inflammation of the retained rectal mucosa, and neoplastic transformation of the ATZ.
Functional outcomes were evaluated at similar postoperative time intervals between the 2 groups. These included frequency of defecation per 24 hours and at night, incontinence, stool seepage, and pad usage during daytime and nighttime as well as use of antidiarrheal medication. Quality of life and sexual function measures were also compared between the 2 groups.
Anorectal physiologic measures were compared in the 2 groups during similar postoperative time intervals. These included the resting and maximum squeeze pressure of the sphincter complex measured in millimeters of mercury, neorectal threshold volume, and maximum neorectal volume measured in milliliters. The length of the high pressure zone in centimeters was also evaluated in the 2 groups.
Statistical Analysis
Meta-analysis was performed in line with recommendations from the Cochrane Collaboration the Quality of Reporting of Meta-analyses (QUORUM) guidelines.13,14 The effect measures estimated were odds ratio (OR) for dichotomous data and weighted mean difference (WMD) for continuous data, both reported with 95% confidence intervals (CI).15 This ratio represents the odds of an adverse event occurring in the stapled (S) group compared with the hand-sewn (H) ileal pouch anal anastomosis group. An OR of more than 1 favors the stapled group and the point estimate of the odds ratio are considered statistically significant at the P < 0.05 level if the 95% confidence interval does not include the value 1. Studies that contained a zero in one cell for the number of events of interest in one of the 2 groups resulted in problems with the computation of ratio measurement and a value of 0.5 was added in both groups from that particular study.
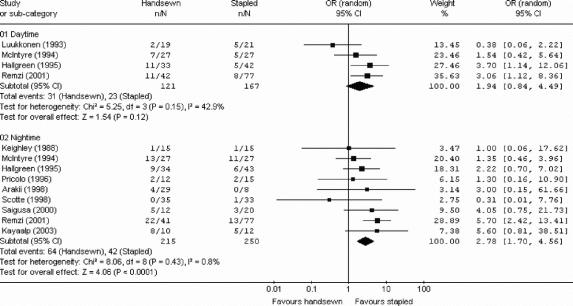
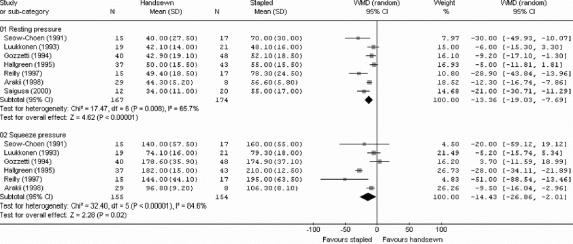
For categorical variables, the ORs were combined with the Mantel-Haenszel χ2 method using a “random effect” meta-analytic technique.16 In a random effect model, it is assumed that there is variation between studies and the calculated odds ratio thus has a more conservative value.17,18 In surgical research, meta-analysis using the random effect model is preferable, particularly because patients that are operated on in different centers have varying risk profiles and selection criteria for each surgical technique. In the Forrest plots shown in Figure 1 and 2, the squares indicate point estimates of treatment effect (OR), with the size of the square representing the weight attributed to each study and 95% confidence intervals indicated by horizontal bars. The diamond represents the summary OR from the pooled studies with 95% CIs. For studies that presented continuous data as mean and range values, the standard deviation (SD) was calculated using statistical algorithms and checked using “bootstrap” resampling techniques. Thus, all continuous data were standardized for the analysis.
FIGURE 1. Meta-analysis illustrating seepage of stool during the day and at night.
FIGURE 2. Meta-analysis of anal manometry.
The quality of the randomized and nonrandomized studies was assessed by using the Newcastle-Ottawa Scale with some modifications to match the needs of this study.19 The quality of the studies was evaluated by examining 3 items: patient selection, comparability of the 3 study groups, and assessment of outcome. Studies achieving 7 or more stars were considered as being of highest quality.
Two strategies were used to quantitatively assess heterogeneity: 1) Graphical exploration with funnel plots was used to evaluate publication bias15,20; and 2) Sensitivity analysis was undertaken for the following subgroups: a) study size more than 50 patients, b) year of publication of greater than 1995, c) studies of higher quality with 7 or more stars, and d) studies reporting outcomes only on J-pouch reservoirs.
Analysis was conducted by using the statistical software Intercooled Stata version 8.0 for Windows (Stata Corporation) and Review Manager Version 4.2 (Cochrane Collaboration, Software Update, Oxford).
RESULTS
Studies Selected
The literature search identified 24 comparative studies matching the selection criteria.7,10,12,21–42 One was excluded from the analysis because after translation it appeared to be a review article.35 A study by Tuckson et al was excluded because of possible crossover of included patients with another study7 as was a study by Lee et al because it was not possible to extract data for any of the outcomes.37 The remaining 21 papers were included for analysis and comprised 6 prospective randomized controlled trials,22,23,26,28,29,32 5 prospective nonrandomized studies,21,27,30,31,33 and 10 retrospective comparative studies.10,12,25,27,36,38–42 On review of the data extraction, there was 100% agreement between the 2 reviewers.
A total of 4183 patients were included in the analysis who underwent formation of an ileal pouch reservoir between 1983 and 2000. A total of 2699 (64.5%) patients underwent a hand-sewn pouch-anal anastomosis with mucosectomy and 1484 (35.5%) patients a stapled pouch-anal anastomosis without mucosectomy. The type of pouch construction was reported for 3976 patients. A total of 3184 (80.1%) patients had a J-pouch (2056 hand-sewn, 1128 stapled IPAA), 743 (18.7%) patients had an S-pouch constructed (529 hand-sewn, 214 stapled IPAA), and 49 (1.2%) had a W-pouch constructed (32 hand-sewn, 17 stapled). Follow-up ranged from 3 to 155 months across the 21 studies, with means of 26.8 months and 19.6 months in the hand-sewn and stapled groups, respectively. A total of 3073 (80.1%) patients underwent proximal diversion at the time of the ileal pouch surgery: 2199 in the hand-sewn group and 874 in the stapled group. The mean age at surgery was 32.5 years in the hand-sewn group and 34.1 years in the stapled group.
The characteristics of the 21 studies are summarized in Table 1. Sixteen studies contained groups that were matched for age,10,12,21–23,26–32,36,38,40,41 17 for gender,10,12,22–24,26–30,32,36,38–42 14 for pouch type,10,22,26–33,36,38,39,41 12 for preoperative diagnosis,22,23,25,28–32,36,38,41,42 and 4 for follow-up.22,29,30,33
TABLE 1. Characteristics of Included Studies
Perioperative Complications
There was no significant difference in the rates of postoperative adverse events between the hand-sewn and stapled IPAA groups as shown in Table 2. There were 5 of 207 (2.4%) reported postoperative deaths. Anastomotic leak occurred in 123 of 1774 (6.9%) patients: with 76 of 865 (8.8%) in the hand-sewn group and 47 of 909 (5.2%) in the stapled group (P = 0.42). Pelvic sepsis occurred in 63 of 878 (7.2%) patients with a hand-sewn pouch-anal anastomoses and in 50 of 1063 (4.7%) patients with a stapled pouch-anal anastomoses, a difference that was not statistically significant (P = 0.21).
TABLE 2. Summary Statistics for Short-term and Long-term Outcomes Comparing Handsewn Versus Stapled Ileal Pouch Anal Anastomosis
Pouch-related fistulae occurred in 134 of 2842 (4.7%) patients, of which 114 of 1944 (5.9%) occurred in the hand-sewn group and 20 of 898 (2.2%) in the stapled group (P = 0.31). Of these, 10 were pouch-vaginal, 101 enterocutaneous, and 23 were not specified. A total of 88 of 525 (16.8%) patients developed pouchitis following closure of the ileostomy: 43 in the hand-sewn and 45 in the stapled group (P= 0.81). Stricture of the pouch-anal anastomosis occurred in 102 of 847 (12%) patients, with 59 of 325 (18.2%) occurring in hand-sewn anastomoses and 39 of 312 (12.5%) in stapled (P = 0.20). Pouch failure occurred in 66 of 1737 (3.8%) patients (hand-sewn 45 of 842; 5.3% vs. stapled 21 of 895; 2.3%, P = 0.06): 58 required either permanent diversion (n = 11) or ileal pouch excision (n = 47). In addition, a further 2 patients underwent redo pouch surgery, both in the stapled group.
Functional Outcomes
There was no significant difference between the hand-sewn and stapled IPAA groups with regards to stool frequency per 24 hours, defecation at night, or use of antidiarrheal medication (Table 2). Incontinence to liquid stool was reported in 77 of 285 (27.0%) patients and was more frequent in the hand-sewn group (H: 29.4% vs. S: 22.1%, OR = 2.32, P = 0.009). Seepage during daytime occurred in 54 of 288 (18.8%) patients, and in 106 of 465 (22.8%) patients during the night with no significant difference between the 2 groups for daytime seepage (H: 25.6% vs. S: 13.8%, OR = 1.94, P= 0.12). Seepage at night, however, occurred more frequently in the hand-sewn group, a difference that was statistically significant (H: 29.8% vs. S: 16.8%, OR = 2.78, P < 0.001). These results are summarized in Figure 1. A total of 41 of 298 (13.8%) patients wore protective pads during the day and 45 of 225 (20.0%) used pads overnight. There was no significant difference between the hand-sewn and stapled group groups for daytime pad usage (15.5% vs. 12.4%, OR = 1.33, P = 0.59); however, the use of pads overnight was more common among the hand-sewn group (26.7% vs. 8.1%, OR = 4.12, P = 0.007), which correlated to the higher incidence of nocturnal seepage.
Anorectal Physiology
The results of anorectal physiologic testing are summarized in Table 2 and Figure 2. Anorectal physiologic measurements demonstrated a significant reduction in the resting and squeeze pressure in the hand-sewn IPAA group by 13.4 and 14.4 mm Hg, respectively (P < 0.018). There were no significant differences between the stapled and hand-sewn groups with regards to neorectal volume (P = 0.98) and the length of the high pressure zone (P = 0.10).
Quality of Life
Assessment on the quality of life and impotence following pouch surgery was undertaken by 4 studies.12,27,31,32 Four of 50 (8.0%) male patients (2 stapled, 2 hand-sewn) reported suffering from impotence following ileal pouch surgery.27,31 There were no reported cases of sexual dysfunction among women undergoing pouch surgery. There were no significant differences in the reported quality of life or in reported sexual dysfunction between the 2 groups.
ATZ Pathology
Assessment of continuing inflammation in the retained rectal mucosa and ATZ was undertaken by 3 studies.25,27,29 The ATZ inflammation rate was 3.3% (3 of 92) in the hand-sewn group and 9.9% (9 of 91) in the stapled, resulting in a difference that was not statistically significant (P = 0.16). One of the studies did not report any occurrences of inflammation in any of the groups.27 Three studies reported dysplasia in the ATZ.12,27,29 One of the studies did not report any occurrences of dysplasia in any of the groups.29 The rate of ATZ dysplasia was 7.2% (6 of 83) in the hand-sewn group compared with 18.5% (22 of 119) in the stapled group. Although a trend favoring hand-sewn anastomosis was suggested, the difference did not reach statistical significance (P = 0.08). Assessment of ATZ neoplasia was undertaken by 3 studies,12,27,29 2 of which did not report any neoplasia in any of the groups.27,29 A single case of ATZ cancer was reported in the stapled group.12
Sensitivity Analysis
Sensitivity analysis was performed by comparing outcomes between hand-sewn and stapled IPAA for high-quality studies (≥7 stars), studies published after 1995, studies with more than 50 cases, and for studies reporting outcomes only on J-pouch reservoirs (Table 3). Sensitivity analyses suggested that patients undergoing hand-sewn anastomosis were associated with significantly higher seepage at night and reduction in the anorectal resting and squeeze pressure. The study heterogeneity was reduced, particularly when only high-quality studies were considered, although heterogeneity remained significant when comparing the 2 groups with regards to anal manometry. When sensitivity analysis was performed for comparative studies that only included J-pouch configuration, significant differences were observed favoring the stapled J-pouch group when considering anorectal resting and squeeze pressures. No significant difference was evident between the 2 groups with regards to anastomotic leak, ileal pouch failure, stool frequency, and seepage.
TABLE 3. Sensitivity Analysis Performed for Studies Comparing Handsewn Versus Stapled Ileal Pouch Anal Anastomosis
Power Calculation for Outcomes of Interest
The overall incidence of seepage at night between studies in the hand-sewn group was 64 of 214 (29.9%) and 42 of 215 (19.5%) in the stapled group. To rule out a 10.4% relative risk reduction with a 5% significance level and 80% power, a traditional randomized controlled trial would require 288 patients in each arm. With regards to dysplasia in the ATZ to rule out an 11.3% relative risk reduction from 18.5% to 7.2% with a 5% significance level and 80% power, a traditional randomized controlled trial would require 154 patients in each arm.
DISCUSSION
The present meta-analysis of 21 studies comparing hand-sewn versus stapled IPAA among 4183 patients suggested that both anastomotic techniques had similar early postoperative outcomes; however, stapled IPAA offered improved nocturnal continence, which was reflected in higher anorectal physiologic measurements. Comparative data on the long-term incidence of dysplasia and cancer in the anal transition zone were inconclusive.
The present meta-analysis reported postoperative adverse events in 20% of patients who underwent restorative proctocolectomy, including ileal pouch failure. This was in line with previously published series quoting complication rates after restorative proctocolectomy between 5% and 30%.32,43 In one study, pelvic sepsis has been thought to occur more frequently in patients undergoing a hand-sewn pouch-anal anastomosis, with an incidence of 15.6% versus 5.5% for hand-sewn and stapled anastomosis, respectively.38 The present meta-analysis did not support this finding, with the incidence of pelvic sepsis being 7.2% versus 4.7% in the hand-sewn and stapled groups, respectively, which are line with previously reported rates of pelvis sepsis following pouch surgery.44,45
The reported pouch failure rate within the present study was 3.8%, lower than a recent descriptive meta-analysis reporting a failure rate of 6.8% at a median follow-up of 36.7 months and increasing to 8.5% in case of follow-up of more than 60 months.45 Other authors have also reported ileal pouch failure rates between 6.8% and 10.5%.45–47 The seemingly low pouch failure rate of the present meta-analysis may be a reflection of the relatively shorter patient follow-up in half of all studies that evaluated short-term functional outcomes rather than long-term ileal pouch survival. A number of these studies excluded patients with pouch failure from their analysis who were either defunctioned or subsequently diverted, following ileal pouch surgery22,25,28,31; and in addition, 5 studies did not report on perioperative complications.10,24–26,32 Reported risk factors for ileal pouch failure included hand-sewn pouch-anal anastomosis, tension on the anastomosis, diagnosis of Crohn's disease, and leakage from either the pouch or the pouch-anal anastomosis.47 In the present study, patients with a hand-sewn anastomosis were associated with a higher ileal pouch failure rate compared with a stapled anastomosis. This finding was not reproducible in 3 of the 4 subgroups of the sensitivity analysis, and it is possible that the higher failure rate in the hand-sewn group may be reflection of the increased patient follow-up in the hand-sewn group.
With regards to functional outcomes, the present meta-analysis demonstrated a significant difference in the occurrence of fecal incontinence and nocturnal seepage, favoring the use of a stapled pouch-anal anastomosis. These findings correlated well with the increased usage of protective pads within the hand-sewn group and are in agreement with previously documented findings. The present meta-analysis also reported significant reduction in the resting tone by 13.3 mm Hg and 14.4 mm Hg for maximum squeeze pressure. With normal values for resting and squeeze pressure within the anal canal being 55.4 ± 15.3 mm Hg and 170.3 ± 81.7 mm Hg, respectively,48 a relative reduction in the squeeze pressure of 8.4% may not manifest itself clinically; however, a 24% reduction in the resting pressure may explain the increased likelihood of nocturnal seepage in the hand-sewn IPAA group.
Other authors have shown that, following restorative proctocolectomy, there was a reduction in the thickness of the internal anal sphincter as well as the presence of defects within the sphincter.49 This was thought to be due to the trauma caused by mucosectomy as well as the prolonged operative time in performing the mucosectomy and fashioning the hand-sewn anastomosis, during which the anal sphincter is being stretched by retractors. Reduced manipulation of the anal sphincter complex, as occurs in a stapled pouch-anal anastomosis, has been shown to have improved functional outcomes and fewer episodes of incontinence.7 Advocates of the hand-sewn IPAA technique argue that by removing the mucosa of the distal rectum, the risk of dysplasia and ongoing inflammation in the retained rectum is minimized. However, incomplete mucosectomy may still result in disease recurrence.50 Conversely, although the stapled pouch-anal anastomosis ensures that the mucosa of the ATZ remains intact, thereby preserving the normal physiology of the sphincter complex, there is a definitive risk of developing dysplasia within the ATZ. A long-term follow-up study of dysplasia within the ATZ showed the incidence of dysplasia in the ATZ to be 4.5%, with significant correlation to prepouch risk factors, including colorectal cancer or dysplasia.51
Although the present meta-analysis aimed to compare the incidence of dysplasia in the ATZ and ongoing inflammation in the retained rectal mucosa between the hand-sewn and stapled groups, there were insufficient data from the included studies to perform a quantitative analysis. Furthermore, the follow-up period as reported by the analyzed studies (range, 4–155 months) may not have been long enough for the true incidence of dysplasia to be assessed. The limited sample size of the studies reporting on dysplasia is also an important factor that precludes any meaningful conclusions to be drawn on the incidence of this outcome. We were also unable to compare outcomes based on the level of the pouch-anal anastomosis above the dentate line. From the extracted data, there was considerable variation in the placement of the anastomosis (0–4.5 cm), although few studies actually measured the level accurately. It has been reported that, in patients undergoing a stapled pouch-anal anastomosis, those with a lower anastomotic height have better functional outcomes.52
The choice of anastomotic technique would therefore depend on the risk of impairment of bowel function versus the risk of developing dysplasia in the long-term, particularly in patients with familial adenomatous polyposis, as well as ongoing inflammation in the retained rectal mucosa in patients with ulcerative colitis.53,54 Patients with a grossly inflamed distal rectum despite aggressive medical therapy may not be ideal candidates for a stapled IPAA. A suggested algorithm for selecting the choice of anastomotic technique for ileal pouch anal anastomosis is shown in Figure 3.
FIGURE 3. Suggested guidelines for performing hand-sewn or stapled ileal pouch-anal anastomosis and subsequent follow-up for patients undergoing restorative proctocolectomy. Risk factors for ATZ dysplasia or ongoing inflammation include primary sclerosing cholangitis, hereditary cancer, severe inflammation in ATZ, and low rectum.
CONCLUSION
The present meta-analysis supported the selective use of stapled pouch-anal anastomosis in view of its better functional outcomes and less disruption of the anal sphincter mechanism. Ideally, candidates for a stapled technique would include patients without colon or rectal cancer, dysplasia in the rectum, and older patients with compromised sphincter pressure. Comparative studies of longer follow-up and sufficient sample size are needed to accurately quantify the risks of anal canal dysplasia or cancer after restorative proctocolectomy.
Footnotes
Reprints: Paris P. Tekkis, MD, FRCS, Department of Biosurgery and Surgical Technology, St. Mary's Hospital, 10th Floor, QEQM Building, Praed Street, London W2 1NY, United Kingdom. E-mail: p.tekkis@imperial.ac.uk.
REFERENCES
- 1.Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. BMJ. 1978;2:85–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fonkalsrud EW. Total colectomy and endorectal ileal pull-through with internal ileal reservoir for ulcerative colitis. Surg Gynecol Obstet. 1980;150:1–8. [PubMed] [Google Scholar]
- 3.Nicholls RJ, Lubowski DZ. Restorative proctocolectomy: the four loop (W) reservoir. Br J Surg. 1987;74:564–566. [DOI] [PubMed] [Google Scholar]
- 4.Regimbeau JM, Panis Y, Pocard M, et al. Hand-sewn ileal pouch-anal anastomosis on the dentate line after total proctectomy: technique to avoid incomplete mucosectomy and the need for long-term follow-up of the anal transition zone. Dis Colon Rectum. 2001;44:43–50. [DOI] [PubMed] [Google Scholar]
- 5.Heald RJ, Allen DR. Stapled ileo-anal anastomosis: a technique to avoid mucosal proctectomy in the ileal pouch operation. Br J Surg. 1986;73:571–572. [DOI] [PubMed] [Google Scholar]
- 6.Kmiot WA, Keighley MR. Totally stapled abdominal restorative proctocolectomy. Br J Surg. 1989;76:961–964. [DOI] [PubMed] [Google Scholar]
- 7.Tuckson W, Lavery I, Fazio V, et al. Manometric and functional comparison of ileal pouch anal anastomosis with and without anal manipulation. Am J Surg. 1991;161:90–95. [DOI] [PubMed] [Google Scholar]
- 8.Duthie HL, Gairns FW. Sensory nerve-endings and sensation in the anal region of man. Br J Surg. 1960;47:585–595. [DOI] [PubMed] [Google Scholar]
- 9.Miller R, Lewis GT, Bartolo DC, et al. Sensory discrimination and dynamic activity in the anorectum: evidence using a new ambulatory technique. Br J Surg. 1988;75:1003–1007. [DOI] [PubMed] [Google Scholar]
- 10.Saigusa N, Kurahashi T, Nakamura T, et al. Functional outcome of stapled ileal pouch-anal canal anastomosis versus hand-sewn pouch-anal anastomosis. Surg Today. 2000;30:575–581. [DOI] [PubMed] [Google Scholar]
- 11.Slors JF, Ponson AE, Taat CW, et al. Risk of residual rectal mucosa after proctocolectomy and ileal pouch-anal reconstruction with the double-stapling technique: postoperative endoscopic follow-up study. Dis Colon Rectum. 1995;38:207–210. [DOI] [PubMed] [Google Scholar]
- 12.Remzi FH, Church JM, Bast J, et al. Mucosectomy vs. stapled ileal pouch-anal anastomosis in patients with familial adenomatous polyposis: functional outcome and neoplasia control. Dis Colon Rectum. 2001;44:1590–1596. [DOI] [PubMed] [Google Scholar]
- 13.Clarke M, Horton R. Bringing it all together: Lancet-Cochrane collaborate on systematic reviews. Lancet. 2001;357:1728. [DOI] [PubMed] [Google Scholar]
- 14.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. [DOI] [PubMed] [Google Scholar]
- 15.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–748. [PubMed] [Google Scholar]
- 17.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 18.Sterne JA, Davey Smith G. Sifting the evidence: what's wrong with significance tests? BMJ. 2001;322:226–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Athanasiou T, Al-Ruzzeh S, Kumar P, et al. Off-pump myocardial revascularization is associated with less incidence of stroke in elderly patients. Ann Thorac Surg. 2004;77:745–753. [DOI] [PubMed] [Google Scholar]
- 20.Egger M, Smith GD. Misleading meta-analysis. BMJ. 1995;311:753–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Araki Y, Isomoto H, Tsuzi Y, et al. Functional outcome of double-stapled and transanal ileal pouch-anal anastomosis after proctocolectomy. Kurume Med J. 1998;45:209–213. [DOI] [PubMed] [Google Scholar]
- 22.Choen S, Tsunoda A, Nicholls RJ. Prospective randomized trial comparing anal function after hand sewn ileoanal anastomosis with mucosectomy versus stapled ileoanal anastomosis without mucosectomy in restorative proctocolectomy. Br J Surg. 1991;78:430–434. [DOI] [PubMed] [Google Scholar]
- 23.Cohen Z, McLeod RS, Stephen W, et al. Continuing evolution of the pelvic pouch procedure. Ann Surg. 1992;216:506–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gemlo BT, Belmonte C, Wiltz O, et al. Functional assessment of ileal pouch-anal anastomotic techniques. Am J Surg. 1995;169:137–141 ; discussion 141–142. [DOI] [PubMed]
- 25.Gozzetti G, Poggioli G, Marchetti F, et al. Functional outcome in hand-sewn versus stapled ileal pouch-anal anastomosis. Am J Surg. 1994;168:325–329. [DOI] [PubMed] [Google Scholar]
- 26.Hallgren TA, Fasth SB, Oresland TO, et al. Ileal pouch anal function after endoanal mucosectomy and hand-sewn ileoanal anastomosis compared with stapled anastomosis without mucosectomy. Eur J Surg. 1995;161:915–921. [PubMed] [Google Scholar]
- 27.Kayaalp C, Nessar G, Akoglu M, et al. Elimination of mucosectomy during restorative proctocolectomy in patients with ulcerative colitis may provide better results in low-volume centers. Am J Surg. 2003;185:268–272. [DOI] [PubMed] [Google Scholar]
- 28.Keighley MR, Yoshioka K, Kmiot W. Prospective randomized trial to compare the stapled double lumen pouch and the sutured quadruple pouch for restorative proctocolectomy. Br J Surg. 1988;75:1008–1011. [DOI] [PubMed] [Google Scholar]
- 29.Luukkonen P, Jarvinen H. Stapled vs hand-sutured ileoanal anastomosis in restorative proctocolectomy: a prospective, randomized study. Arch Surg. 1993;128:437–440. [DOI] [PubMed] [Google Scholar]
- 30.McIntyre PB, Pemberton JH, Beart RW Jr, et al. Double-stapled vs. hand-sewn ileal pouch-anal anastomosis in patients with chronic ulcerative colitis. Dis Colon Rectum. 1994;37:430–433. [DOI] [PubMed] [Google Scholar]
- 31.Pricolo VE, Potenti FM, Luks FI. Selective preservation of the anal transition zone in ileoanal pouch procedures. Dis Colon Rectum. 1996;39:871–877. [DOI] [PubMed] [Google Scholar]
- 32.Reilly WT, Pemberton JH, Wolff BG, et al. Randomized prospective trial comparing ileal pouch-anal anastomosis performed by excising the anal mucosa to ileal pouch-anal anastomosis performed by preserving the anal mucosa. Ann Surg. 1997;225:666–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rossi HL, Brand MI, Saclarides TJ. Anal complications after restorative proctocolectomy (J-pouch). Am Surg. 2002;68:628–630. [PubMed] [Google Scholar]
- 34.Williams NS, Marzouk DE, Hallan RI, et al. Function after ileal pouch and stapled pouch-anal anastomosis for ulcerative colitis. Br J Surg. 1989;76:1168–1171. [DOI] [PubMed] [Google Scholar]
- 35.Wolff BG, Dozois RR. Ileo-anal anastomosis: surgical anastomosis with mucosectomy or stapled anastomosis without mucosectomy? Ann Chir. 1993;47:963–966. [PubMed] [Google Scholar]
- 36.Ziv Y, Fazio VW, Church JM, et al. Stapled ileal pouch anal anastomoses are safer than hand-sewn anastomoses in patients with ulcerative colitis. Am J Surg. 1996;171:320–323. [DOI] [PubMed] [Google Scholar]
- 37.Lee PY, Fazio VW, Church JM, et al. Vaginal fistula following restorative proctocolectomy. Dis Colon Rectum. 1997;40:752–759. [DOI] [PubMed] [Google Scholar]
- 38.Fukushima T, Sugita A, Koganei K, et al. The incidence and outcome of pelvic sepsis following hand-sewn and stapled ileal pouch anal anastomoses. Surg Today. 2000;30:223–227. [DOI] [PubMed] [Google Scholar]
- 39.Gecim IE, Wolff BG, Pemberton JH, et al. Does technique of anastomosis play any role in developing late perianal abscess or fistula? Dis Colon Rectum. 2000;43:1241–1245. [DOI] [PubMed] [Google Scholar]
- 40.Wettergren A, Gyrtrup HJ, Grosmann E, et al. Complications after J-pouch ileoanal anastomosis: stapled compared with hand-sewn anastomosis. Eur J Surg. 1993;159:121–124. [PubMed] [Google Scholar]
- 41.Scotte M, Del Gallo G, Steinmetz L, et al. Ileoanal anastomosis for ulcerative colitis: results of an evolutionary surgical procedure. Hepatogastroenterology. 1998;45:2123–2126. [PubMed] [Google Scholar]
- 42.Sugerman HJ, Newsome HH. Stapled ileoanal anastomosis without a temporary ileostomy. Am J Surg. 1994;167:58–65. [DOI] [PubMed] [Google Scholar]
- 43.Dayton MT, Larsen KP. Outcome of pouch-related complications after ileal pouch-anal anastomosis. Am J Surg. 1997;174:728–731. [DOI] [PubMed] [Google Scholar]
- 44.Farouk R, Dozois RR, Pemberton JH, et al. Incidence and subsequent impact of pelvic abscess after ileal pouch-anal anastomosis for chronic ulcerative colitis. Dis Colon Rectum. 1998;41:1239–1243. [DOI] [PubMed] [Google Scholar]
- 45.Hueting WE, Buskens E, van der Tweel I, et al. Results and complications after ileal pouch anal anastomosis: a meta-analysis of 43 observational studies comprising 9,317 patients. Dig Surg. 2005;22:69–79. [DOI] [PubMed] [Google Scholar]
- 46.Tulchinsky H, Hawley PR, Nicholls J. Long-term failure after restorative proctocolectomy for ulcerative colitis. Ann Surg. 2003;238:229–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.MacRae HM, McLeod RS, Cohen Z, et al. Risk factors for pelvic pouch failure. Dis Colon Rectum. 1997;40:257–262. [DOI] [PubMed] [Google Scholar]
- 48.Kritasampan P, Lohsiriwat S, Leelakusolvong S. Manometric tests of anorectal function in healthy adult Thai subjects. J Med Assoc Thai. 2004;87:536–542. [PubMed] [Google Scholar]
- 49.Silvis R, van Eekelen JW, Delemarre JB, et al. Endosonography of the anal sphincter after ileal pouch-anal anastomosis: relation with anal manometry and fecal continence. Dis Colon Rectum. 1995;38:383–388. [DOI] [PubMed] [Google Scholar]
- 50.Ziv Y, Fazio VW, Sirimarco MT, et al. Incidence, risk factors, and treatment of dysplasia in the anal transitional zone after ileal pouch-anal anastomosis. Dis Colon Rectum. 1994;37:1281–1285. [DOI] [PubMed] [Google Scholar]
- 51.Remzi FH, Fazio VW, Delaney CP, et al. Dysplasia of the anal transitional zone after ileal pouch-anal anastomosis: results of prospective evaluation after a minimum of ten years. Dis Colon Rectum. 2003;46:6–13. [DOI] [PubMed] [Google Scholar]
- 52.Annibali R, Oresland T, Hulten L. Does the level of stapled ileoanal anastomosis influence physiologic and functional outcome? Dis Colon Rectum. 1994;37:321–329. [DOI] [PubMed] [Google Scholar]
- 53.Tytgat GN, Gopinath N. Recurrent polyps in the ileo-anal pouch or rectum in familial adenomatous polyposis. Eur J Cancer. 1995;31:1154–1159. [DOI] [PubMed] [Google Scholar]
- 54.Thompson-Fawcett MW, Mortensen NJ, Warren BF. ‘Cuffitis’ and inflammatory changes in the columnar cuff, anal transitional zone, and ileal reservoir after stapled pouch-anal anastomosis. Dis Colon Rectum. 1999;42:348–355. [DOI] [PubMed] [Google Scholar]