Abstract
Objective:
To trace the evolution of pancreaticoduodenectomy from the decade of the 1960s through the first decade of the new Millenium, through the experience of one surgeon doing 1000 consecutive operations.
Summary Background Data:
A regional resection of the head of the pancreas was first performed successfully by Kausch in 1909. The operation was popularized by Whipple in 1935, who reported 3 pancreaticoduodenectomies. Because of a hospital mortality of approximately 25%, the operation was performed infrequently until the 1980s. From the 1980s on, experience with this complex alimentary tract operation increased, and high-volume centers developed. This resulted in a significant drop in hospital mortality and allowed institutions and individuals to gain large experiences.
Methods:
Between March 1969 and May 2003, 1000 consecutive pancreaticoduodenectomies were performed by a single surgeon. A retrospective review of a prospectively maintained database was performed to determine the management and outcome of these patients, as well as to document the evolution of this operative procedure over 5 decades.
Results:
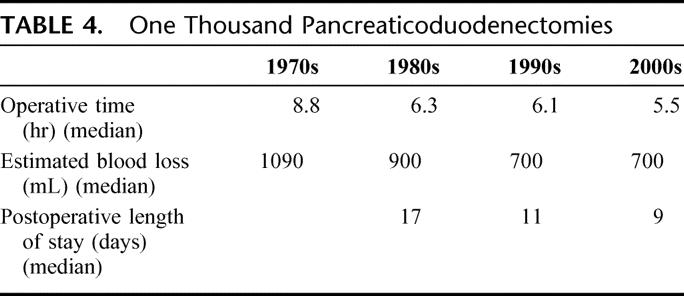
The median operative time decreased significantly over the decades, being 8.8 hours in the 1970s and 5.5 hours during the 2000s. Postoperative length of stay dropped from a median of 17 days in the 1980s to 9 days in the 2000s. There were only 10 postoperative/hospital deaths, for a mortality of 1%. A total of 405 patients underwent pancreaticoduodenectomy for adenocarcinoma of the head of the pancreas. Overall 5-year survival was 18%; for the lymph node-negative patients, it was 32%; and for node-negative, margin-negative patients, it was 41%.
Conclusions:
Pancreaticoduodenectomy has become a commonly performed operation in many tertiary care centers. Operative time, blood loss, and length of stay have dropped substantially. The operation has become safe, with a low hospital mortality. It has become an effective operation for pancreatic cancer in those patients in whom their tumor is margin negative and node negative.
A total of 1000 consecutive pancreaticoduodenectomies were performed by one surgeon from 1969 to 2003. The evolution of the diagnosis and management of patients undergoing this operation over the 5 decades is documented. There were 10 deaths for a hospital mortality of 1%.
The first successful local resection of a periampullary tumor was performed by Dr. William Stewart Halsted in 1898.1 The patient was a 58-year-old woman with obstructive jaundice. Halsted resected a segment of the second portion of the duodenum, including the tumor, and anastomosed the duodenum end to end. He then reimplanted the bile and pancreatic ducts. The first successful regional resection for a periampullary tumor was performed by the German surgeon from Berlin, Kausch, in 1909, and reported in 1912.2 The regional operative procedure for periampullary tumors was popularized by Whipple in a paper published in 1935.3 In this paper, 3 patients were reported who underwent regional resection performed in 2 stages. Two of the 3 patients survived. Between 1912 and Whipple’s report in 1935, a small number of patients in Europe underwent a regional resection of a periampullary tumor successfully. Following Whipple’s report, the operative procedure became widely known but was still infrequently performed. By the end of Whipple’s career, he had only performed 37 such procedures.4
During the 1960s and 1970s, few pancreaticoduodenectomies were performed because of a hospital mortality in the range of 25%. However, during the 1980s and 1990s, experience performing pancreaticoduodenectomy increased, and large volume “centers of excellence” developed. These high-volume centers acquired a substantial experience, and mortality decreased to below 5%.5–8 In recent years at the Johns Hopkins Hospital, more than 200 pancreaticoduodenectomies have been performed annually. This has allowed individual surgeons to develop significant experiences. Between 1969 and 2003, 1000 consecutive pancreaticoduodenectomies were performed by a single surgeon (J.L.C.) at the Johns Hopkins Hospital. This report reviews that experience and documents the changes that have occurred with this operative procedure over 5 decades.
Clinical Material
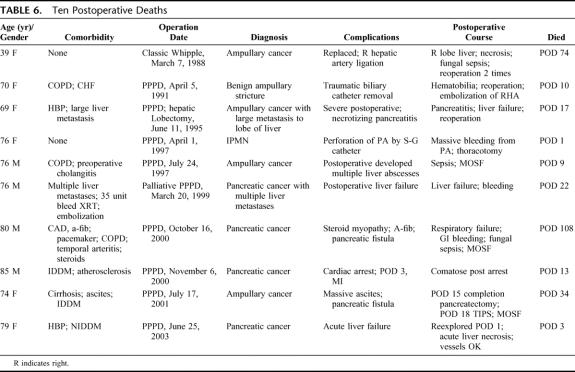
Between March 1969 and May 2003, 1000 consecutive pancreaticoduodenectomies were performed by a single surgeon. One was performed in the decade of the sixties, 2 in the 1970s, 63 in the 1980s, 587 during the 1990s, and 347 during the first 3.5 years of the new millennium. Ages ranged from 15 years to 103 years. Mean age was 63.4 years. Seventy patients were in their 80s, one in the 90s, and one patient was 103 years old. A total of 549 were male, and 451 were female. A total of 652 patients had a periampullary adenocarcinoma (pancreatic 405, ampullary 113, distal cholangiocarcinoma 95, duodenal 39) (Table 1). Eighty-nine patients had chronic pancreatitis, 57 patients had neuroendocrine tumors, and 47 patients had adenomas involving their ampulla or duodenum. The remainder had a variety of neoplasms, many were cystic tumors, and in recent years there has been an increasing number of patients with intraductal papillary mucinous neoplasms (53patients). A total of 900 patients were white, 54 were black, and 46 were other.
TABLE 1. Indications for Pancreaticoduodenectomy
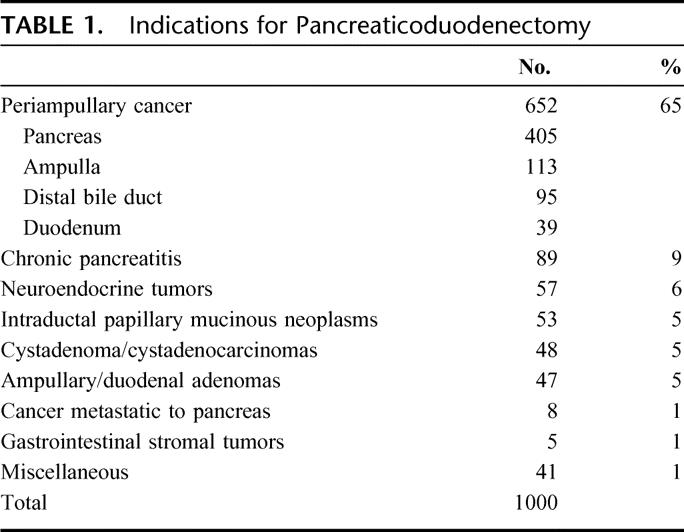
Presenting symptoms included jaundice in 72%, weight loss in 45%, and abdominal pain in 34%. The patients originated from 33 of the 50 states in the United States, and 6 foreign countries. The majority of patients were evaluated with a computed tomography (CT) scan (Table 2). In earlier years, angiography was used with great frequency to stage patients, but this has not been used in recent years. Magnetic resonance imaging/magnetic resonance cholangiopancreatography (MRI/MRCP) continue to be used only infrequently. Percutaneous transhepatic cholangiography previously was performed in the majority of patients (67% in 1998), but its use has decreased substantially (13% in 2003). Many patients are referred to Hopkins with a biliary endostent in place.
TABLE 2. Preoperative Imaging
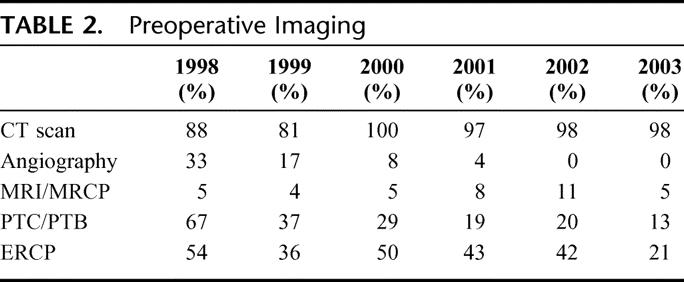
A total of 787 patients underwent a pylorus-preserving pancreaticoduodenectomy, and 213 underwent a classic pancreaticoduodenectomy (Table 3). A total of 955 patients underwent resection of the head, neck and uncinate process of the pancreas, with the remaining 45 patients undergoing a total pancreatectomy. In those 200 patients in whom the information was available, the texture of the gland was normal in 39%, moderately firm in 36%, and firm and fibrotic in 26%. Eighty-seven percent of the patients underwent reconstruction with a pancreaticojejunostomy, with the remaining 13% undergoing a pancreaticogastrostomy. Portal or superior mesenteric vein resection was carried out in 2% of the patients.
TABLE 3. One Thousand Pancreaticoduodenectomies
Clinical Course
The median operative time has decreased significantly over the decades, being 8.8 hours during the 1970s and dropping to 5.5 hours during the 2000s (Table 4). Blood loss has also decreased, with a median blood loss of >1 L in the 1970s dropping to 700 mL in the 2000s. Sixty-eight percent of the patients undergoing pancreaticoduodenectomy did not require a blood transfusion during the operative procedure, with the remaining 32% receiving 1 or more units of blood. Postoperative length of stay has dropped significantly from a median of 17 days in the 1980s to 9 days in the 2000s.
TABLE 4. One Thousand Pancreaticoduodenectomies
Forty-one percent of the patients developed a postoperative complication (Table 5). The most common was delayed gastric emptying (the need for a nasogastric tube 7 or more days after surgery) in 18%. The development of a pancreatic cutaneous fistula (output of 30 mL or more per day with an amylase 3 times serum level 7 days after surgery) in 12% of patients was the second most common complication. A wound infection developed in 7% of patients; 2.7% of the patients required reoperation for a complication, the most common being bleeding in 9 patients, an abdominal abscess in 7 patients, and wound dehiscence in 4 patients.
TABLE 5. One Thousand Pancreaticoduodenectomies
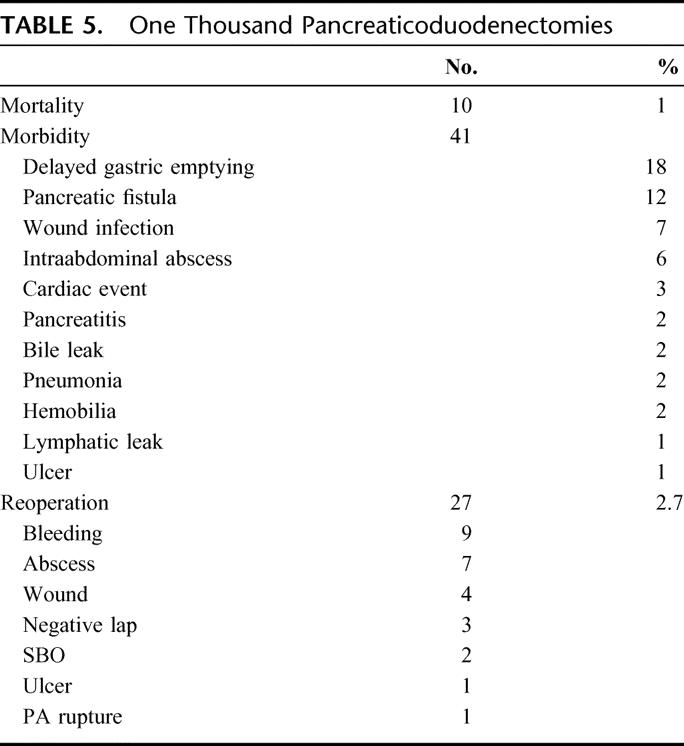
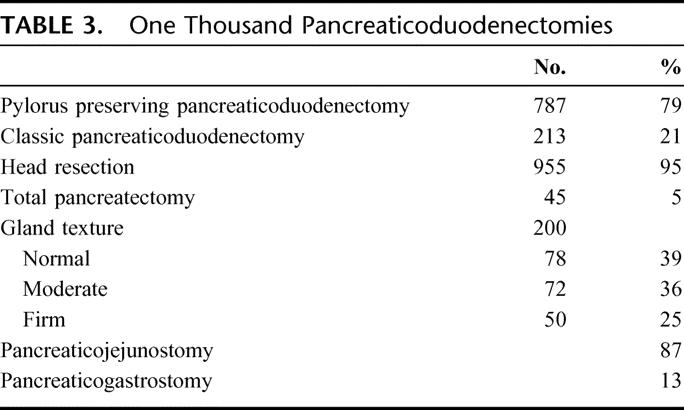
There were 10 postoperative deaths, for a hospital and/or 30 day mortality of 1%. Causes of death were sepsis in 4 patients, postoperative bleeding in 2 patients, myocardial infarction in 1 patient, and hepatic failure in 3 patients (Table 6).
TABLE 6. Ten Postoperative Deaths
Among the 652 patients with periampullary adenocarcinomas, the mean diameter was 3.0 ± 0.1 cm, and the median diameter was 2.6 cm; 73% of the patients had positive nodes. In 4%, the adenocarcinoma was well differentiated, in 59% moderately differentiated, and in 37% the tumor was poorly differentiated. There were 405 adenocarcinomas of the head of the pancreas. One-, three-, and five-year survival was 64%, 27%, and 18% respectively (Fig. 1). Among those patients with negative margins, 5-year survival was 23%; it dropped down to 7% with positive margins (Fig. 2). Among those patients with negative lymph nodes, 5-year survival was 32%, compared with 14% with positive lymph nodes (Fig. 3). There were 64 patients with both node-negative and margin-negative status. The 1-, 3-, and 5-year survivals were 80%, 49%, and 41%, respectively (Fig. 4). The mean survival was 33 months. Among the other 3 periampullary tumors, 5-year survival for distal common bile duct tumors was 22% (24 months mean), for ampullary cancer 5-year survival was 39% (44 months mean), and for duodenal cancer five-year survival was 52% (mean survival not yet reached) (Fig. 5).
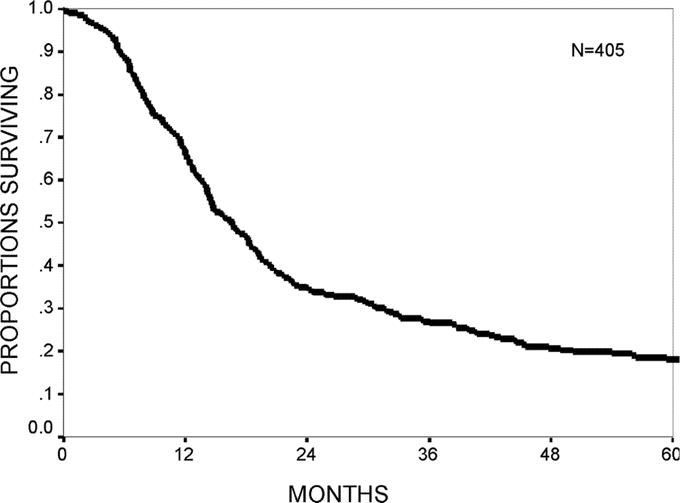
FIGURE 1. Actuarial 5-year survival from 405 patients with adenocarcinoma of the pancreas undergoing a pancreaticoduodenectomy.
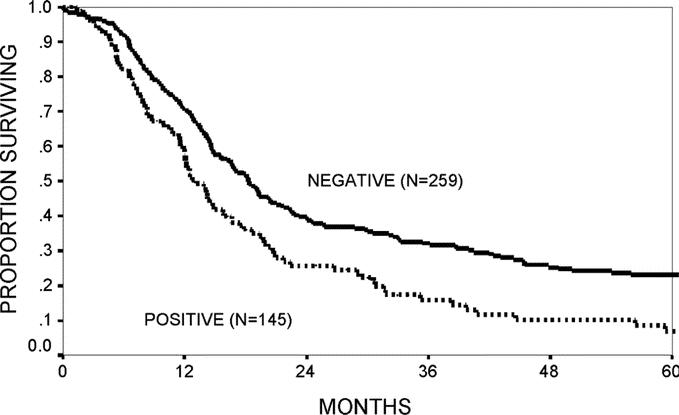
FIGURE 2. Actuarial 5-year survival for margin-negative and margin-positive patients with adenocarcinoma of the pancreas undergoing a pancreaticoduodenectomy.
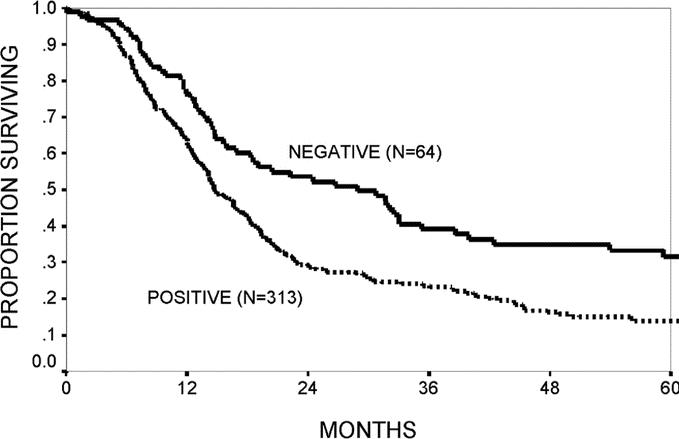
FIGURE 3. Actuarial 5-year survival for node-negative and node-positive patients with adenocarcinoma of the pancreas undergoing a pancreaticoduodenectomy.
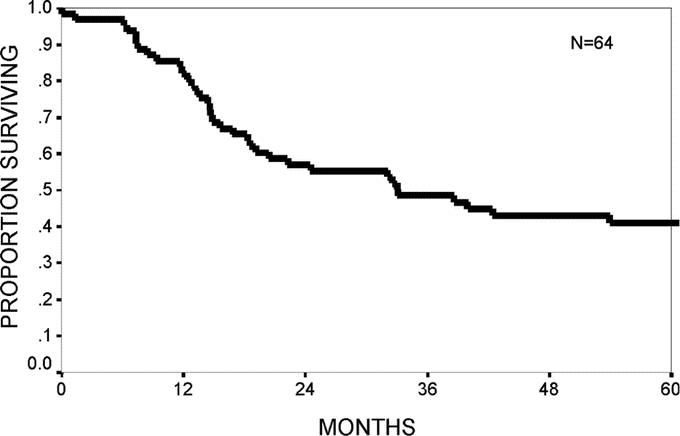
FIGURE 4. Actuarial 5-year survival for patients who were both node negative and margin negative with adenocarcinoma of the pancreas.
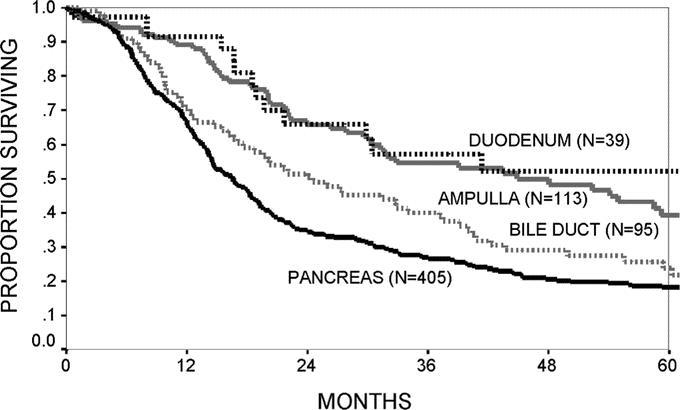
FIGURE 5. Actuarial 5-year survival for patients with adenocarcinoma of the duodenum, ampulla, distal bile duct, and pancreas undergoing a pancreaticoduodenectomy.
DISCUSSION
Pancreaticoduodenectomy, or the Whipple procedure, is a complex high-risk general surgical procedure. It was first performed successfully early in the 20th century, but was rarely performed before 1935, when Whipple published his classic paper in the Annals of Surgery.3 Subsequently, because of a hospital mortality in the range of 25%, it was performed infrequently until the 1980s and 1990s. During those 2 decades, several institutions around the world became interested in performing the Whipple procedure, and started attracting large numbers of patients with benign and malignant diseases treated by pancreaticoduodenectomy. Regionalization in some areas resulted, and centers of excellence developed.6–9 Institutions performing large volumes of these procedures started reporting their results, with a substantially decreased hospital mortality.7–9 Surgeons at the Johns Hopkins Hospital became interested in this disease in the early 1980s at a time when very few pancreaticoduodenectomies were performed annually. Volumes started growing, and since 1994 more than 100 pancreaticoduodenectomies have been performed yearly at the Johns Hopkins Hospital, and for the past 6 years over 200 have been performed yearly. During this era, mortality at the Johns Hopkins Hospital for pancreaticoduodenectomies has dropped dramatically.5,9
In the 1000 consecutive patients reported in this paper, there were only 10 postoperative deaths. These 10 patients represented a somewhat higher risk group than the larger group as a whole. Average age was 72.4 years, in contrast to an average age of 63.4 years in the entire group. Eight of these 10 patients were over 70 years of age, 6 were over 75 years of age, and 2 of the patients were in their 80s. Three of the patients had diabetes, 3 had chronic obstructive pulmonary disease, 2 had coronary artery disease, with 1 patient having a pacemaker in place. One patient was on large doses of prednisone daily for temporal arteritis and had a significant myopathy. One patient had widespread metastases to the liver. He had undergone a 35-unit bleed that was not controllable with radiotherapy and gastroduodenal artery embolization, and a palliative pancreaticoduodenectomy was performed in an attempt to control the bleeding.
Even though 10 deaths are a low number of deaths among 1000 patients, when these 10 deaths are examined closely some were potentially avoidable. Two patients bled to death postoperatively: 1 from the insertion of a Swan Ganz catheter that perforated the pulmonary artery and a second who had accidental traumatic removal of a percutaneous transhepatic biliary drainage tube that resulted in uncontrollable hematobilia. Another patient had division of a replaced right hepatic artery during the operative procedure 16 years ago when that anatomic anomaly was not generally appreciated. No attempt was made at repair during the procedure. All 3 of those patients had avoidable complications. In addition, in retrospect, there were 5 patients in whom the indication for a pancreaticoduodenectomy could have been questioned. One patient with temporal arteritis on alternating days of 60 and 40 mg of prednisone had a severe myopathy, and was never able to be weaned from the ventilator. A second patient had his liver replaced, with metastases, but had a significant ongoing bleed from a pancreatic cancer invading the duodenum. The bleeding was not controlled with radiotherapy or embolization of the gastroduodenal artery, and the patient underwent a palliative pancreaticoduodenectomy. A third patient underwent a Whipple procedure plus a right hepatic lobectomy for an ampullary cancer with a large liver metastasis. A fourth patient preoperatively had severe cholangitis and postoperatively developed multiple liver abscesses and sepsis. A fifth patient had cirrhosis and ascites, but no portal hypertension. In retrospect, one could question the indication for pancreaticoduodenectomy in each of these patients.
The final 2 deaths were from a myocardial infarction and the development of acute massive liver failure. The patient with liver failure was reexplored and both the hepatic artery and portal vein were open, and at autopsy 3 days later again both vessels were patent. The patient presumably had an idiosyncratic reaction to a drug. Each of these deaths presumably was unavoidable.
The Johns Hopkins Hospital, as well as other high-volume centers throughout the country, have reported a substantial drop in hospital mortality for pancreaticoduodenectomy, in the range of 5% or lower.5–9 Even though this is still somewhat controversial, many think that large volume is a surrogate marker for improved outcomes, at least as measured by hospital mortality. However, there are no universally accepted definitions of high volume. It has been our bias that a surgeon should be doing at least 15 pancreaticoduodenectomies a year to be considered high volume. There are obviously many factors responsible for the significant drop in hospital mortality, besides high volume. If a patient is malnourished preoperatively, nutrition can be improved by a variety of parenteral and/or enteral means. Critical care anesthesia is now at a level where anesthetic deaths have been reduced to a minimum. Excellent intensive care units are available in many hospitals, with trained intensivists contributing to postoperative care. If organ failure develops, support is readily available. In addition, because of the high volume, surgeons have become more aware of the various anatomic anomalies that can appear, intraoperative mishaps are fewer, operative time and blood administration have decreased, and these factors, perhaps, also have played an important role in the decreased mortality. Institutions with high volumes have developed teams of physicians and nurses who are experienced and comfortable in caring for these patients preoperatively, intraoperatively, and postoperatively. Very efficient and effective critical care pathways have been developed that may also have contributed to a significant drop in hospital mortality, and a substantial drop in postoperative stay.9–11
Another benefit from an increased volume of Whipple operations has been the ability to perform single institution prospective randomized clinical studies, in an effort to improve care and outcome. At our institution, in those patients explored for a potential Whipple operation who were found to be unresectable, prospective randomized studies were carried out evaluating the efficacy of a prophylactic gastrojejunostomy,12 and the efficacy of a chemical splanchnicectomy13 to improve palliation. In those patients who underwent a pancreaticoduodenectomy, prospective randomized clinical trails have been carried out evaluating pancreaticojejunostomy versus pancreaticogastrostomy,14 octreotide administration,15 and fibrin glue application,16 as a means of decreasing the incidence of postoperative pancreatic cutaneous fistulas. Currently, a prospective randomized study is in progress at our institution evaluating the efficacy of a pancreatic duct stent in decreasing the incidence of postoperative fistula. The efficacy of erythromycin, to decrease the incidence of postoperative delayed gastric emptying, was evaluated in a prospective randomized study.17 Finally, a prospective randomized study was carried out in our institution evaluating pylorus-preserving pancreaticoduodenectomy without a retroperitoneal node dissection, versus a classic Whipple and a retroperitoneal lymphadenectomy, looking at their effect on long-term survival for patients with periampullary adenocarcinomas.18 Such studies can be difficult to carry out when many institutions are involved, and patient accrual tends to be slow. When a single institution has a large volume of clinical material, and all of those participating in the care agree to participate, patient accrual is rapid.
Finally, another advantage of high volume surgery in an institution is that it allows that institution to train surgeons to perform complex high-risk tertiary surgical procedures. These surgeons can subsequently take their experience and expertise to other institutions and provide that same level of care to develop another center of excellence.
When one looks at survival following pancreaticoduodenectomy for patients with periampullary carcinomas today, compared with several decades ago, survival is clearly improved. Decreasing hospital mortality from 25% to below 5% certainly has helped improve survival. There are many institutions in whom patients with pancreatic cancer treated by the Whipple operation have a 5-year survival rate of approximately 20%. This has to be compared with survival rates of less than 5% in the past. In addition, looking at those patients with pancreatic cancer in the present series who had negative nodes and negative margins, those patients presumably with small early pancreatic cancers, the 1-, 3-, and 5-year survival rates were 80%, 49%, and 41%, respectively. The multiple reasons for the improved survival are not entirely clear. It is unlikely that surgery will play a significant role in the further improvement of long-term survival following pancreaticoduodenectomy for the 4 periampullary adenocarcinomas. Further improvement will come from neoadjuvant and/or adjuvant therapy with radiotherapy and chemotherapy, as well as with immunotherapy. The past 2 decades have seen a significant improvement in the way periampullary cancers are managed surgically. The next few decades, with the introduction of tumor markers, and improved neoadjuvant and adjuvant therapy, will almost certainly result in significant improvements in long-term survival.
Footnotes
Reprints: John L. Cameron, MD, Johns Hopkins Hospital, 600 N. Wolfe Street, Blalock 679, Baltimore, MD 21287. E-mail: jcameron@jhmi.edu.
REFERENCES
- 1.Halsted WS. Contributions to the surgery of the bile passages, especially of the common bile duct. Boston Med Surg J. 1899;141:645–654. [Google Scholar]
- 2.Kausch W. Das carcinoma der papilla duodeni und seine radikale entfeinung. Beitr Z Clin Chir. 1912;78:439–486. [Google Scholar]
- 3.Whipple A, Parsons WB, Mullins CR. Treatment of carcinoma of the ampulla of Vater. Ann Surg. 1935;102:763–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whipple AO. A reminiscence: pancreaticoduodenectomy. Rev Surg. 1963;20:221–225. [PubMed] [Google Scholar]
- 5.Cameron JL, Pitt HA, Yeo CJ, et al. One-hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg. 1993;217:430–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trede M, Schwall G, Saeger H-D. Survival after pancreaticoduodenectomy: 118 consecutive resections without an operative mortality. Ann Surg. 1990;211:447–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fernandez-del Castillo C, Ratner DW, Warshaw AL. Standards for pancreatic resection in the 1990s. Arch Surg. 1995;130:295–300. [DOI] [PubMed] [Google Scholar]
- 8.Lieberman MD, Kilburn H, Lindsey M, et al. Relation of perioperative deaths to hospital volume among patients undergoing pancreatic resection for malignancy. Ann Surg. 1995;222:638–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gordon TA, Burleyson GP, Tielsch JM, et al. The effects of regionalization on cost and outcome for one general high-risk surgical procedure. Ann Surg. 1995;221:43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sosa JA, Bowman HM, Gordon TA, et al. Importance of hospital volume in the overall management of pancreatic cancer. Ann Surg. 1998;228:429–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gordon TA, Bowman HM, Tielsch JM, et al. Statewide regionalization of pancreaticoduodenectomy and its effect on in- hospital mortality. Ann Surg. 1998;228:71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lillemoe KD, Cameron J, Hardacre JM, et al. Is prophylactic gastrojejunostomy indicated for unresectable periampullary cancer? A prospective randomized trial. Ann Surg. 1999;230:322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lillemoe KD, Cameron JL, Kaufman HS, et al. Chemical splanchnicectomy in patients with unresectable pancreatic cancer: a prospective randomized trial. Ann Surg. 1993;217:447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yeo CJ, Cameron JL, Maher MM, et al. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 1995;222:580–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yeo CJ, Cameron JL, Lillemoe KD, et al. Does prophylactic octreotide decrease the rates of pancreatic fistula and other complications after pancreaticoduodenectomy? Ann Surg. 2000;232:419–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lillemoe KD, Cameron JL, Kim MP, et al. Does fibrin glue sealant decrease the rate of pancreatic fistula after pancreaticoduodenectomy? Results of a prospective randomized trial. J Obstet Gynecol Surg. 2004;8:766–774. [DOI] [PubMed] [Google Scholar]
- 17.Yeo CJ, Barry MK, Sauter PK, et al. Erythromycin accelerates gastric emptying following pancreaticoduodenectomy: a prospective, randomized placebo controlled trial. Ann Surg. 1993;218:229–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yeo CJ, Cameron JL, Lillemoe KD, et al. Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma: 2. Randomized controlled trial evaluating survival, morbidity, and mortality. Ann Surg. 2002;236:355–366. [DOI] [PMC free article] [PubMed] [Google Scholar]