Abstract
Objective:
We conducted a double-blinded randomized controlled trial to investigate the short- to mid-term neurosensory effect of prophylactic ilioinguinal neurectomy during Lichtenstein repair of inguinal hernia.
Method:
One hundred male patients between the age of 18 and 80 years with unilateral inguinal hernia undergoing Lichtenstein hernia repair were randomized to receive either prophylactic ilioinguinal neurectomy (group A) or ilioinguinal nerve preservation (group B) during operation. All operations were performed by surgeons specialized in hernia repair under local anesthesia or general anesthesia. The primary outcome was the incidence of chronic groin pain at 6 months. Secondary outcomes included incidence of groin numbness, postoperative sensory loss or change at the groin region, and quality of life measurement assessed by SF-36 questionnaire at 6 months. All follow-up and outcome measures were carried out by a designated occupational therapist at 1 and 6 months following surgery in a double-blinded manner.
Results:
The incidence of chronic groin pain at 6 months was significantly lower in group A than group B (8% vs. 28.6%; P = 0.008). No significant intergroup differences were found regarding the incidence of groin numbness, postoperative sensory loss or changes at the groin region, and quality of life measurement at 6 months after the operation.
Conclusions:
Prophylactic ilioinguinal neurectomy significantly decreases the incidence of chronic groin pain after Lichtenstein hernia repair without added morbidities. It should be considered as a routine surgical step during the operation.
This prospective randomized study evaluated the neurosensory effect of prophylactic ilioinguinal neurectomy during Lichtenstein repair of inguinal hernia. Prophylactic ilioinguinal neurectomy is associated with lower incidence of chronic groin pain without added morbidities. It should be recommended as a routine surgical step during the operation.
Chronic groin pain is a significant problem following open inguinal hernia repair, with a reported incidence ranging from 19% to 62.9%.1–3 Although the pain is often mild in nature, quality of life studies have shown that chronic pain, irrespective of severity, can significantly interfere with normal daily activities.4,5 Moreover, the condition can sometimes be debilitating and treatment is often difficult and challenging.
The ilioinguinal nerve is a sensory nerve that innervates the skin over the groin region, the medial aspect of the thigh, the upper part of the scrotum and the penile root. It is normally encountered during open repair of inguinal hernia. Traditional surgical teaching dictates that the nerve should be preserved at all times during repair because of the supposed morbidity associated with cutaneous sensory loss and chronic groin pain following nerve injury. However, some reports suggested that elective excision of ilioinguinal nerve causes minimal morbidities and was not considered incapacitating by most patients.6,7 In addition, ilioinguinal neurectomy is a well-documented effective treatment of relieving chronic groin pain following open hernia repair, achieving more favorable outcomes than nerve block or mesh removal alone.8–10 More recently, retrospective studies have shown that excision of ilioinguinal nerve during herniorrhaphy were associated with a lower incidence of chronic groin pain after the operation.11–13
In this trial, we studied the effect of prophylactic ilioinguinal neurectomy on the incidence and the severity of chronic groin pain after Lichtenstein repair in a prospective randomized controlled manner. The associated neurosensory disturbances and the quality of life were also investigated.
MATERIALS AND METHODS
Study Protocol
This prospective study was conducted in a university-affiliated hernia center between January 2003 and June 2004. Ethical approval was granted by the Research Ethics Committee of the Chinese University of Hong Kong. Informed consents for the study were obtained from all patients. All patients between the age of 18 and 80 years undergoing elective unilateral Lichtenstein hernia repair were considered eligible. Those with bilateral inguinal hernia, recurrent hernia, irreducible or strangulated hernia, large inguinal-scrotal hernia, history of previous abdominal incision, peripheral neuropathy, impaired cognitive function, limited mobility, and female gender were excluded. Standard Lichtenstein tension-free mesh repair was the adopted procedure performed either under local anesthesia or general anesthesia at the discretion of individual patient. All operations were performed by the 4 designated surgeons specialized in hernia repair allocated in a random manner. The primary outcome was the incidence of chronic groin pain at 6-month after surgery. Secondary outcomes included incidence of groin numbness, postoperative sensation loss or changes at the groin region, and quality of life measurement assessed by the Chinese version of SF-36 questionnaire14 at 6-month follow-up.
Baselines Measurement
All baseline measurements were obtained by a designated occupational therapist in the Department of Occupation Therapy for the University before operation. Preoperative pain measurements after various activities (at rest, coughing for 10 times, walking up 3 flights of stairs and cycling for 10 minutes) were assessed by 4-point scale (none, mild, moderate, and severe) after completion of each task by patients. Preoperative incidence of groin numbness and quality of life were documented by a self-filling questionnaire with a 4-point scale (none, mild, moderate, and severe) and the Chinese version of SF-36 questionnaire before operation, respectively.
Randomization and Blinding
Intraoperatively, once the ilioinguinal nerve was identified, a telephone call was made to the randomization center where a research assistant would randomly allocate the patient to either prophylactic ilioinguinal neurectomy (group A) or ilioinguinal nerve preservation (group B) by opening sealed envelopes containing computer-generated code in blocks of 10. The patients were blinded from the treatment assignment throughout and were followed up by the designated occupational therapist who was not involved in the randomization process or the clinical management of the patient.
Intervention
All patients received the standard flat mesh repair according to the technique described by Lichtenstein et al.15 In group A, the whole ilioinguinal nerve was excised as far lateral to the deep ring as possible and medially to where it entered the rectus muscles. The cut ends were left alone without implantation into muscle or ligation. Histologic examination of the nerve was performed to confirm complete excision. Any small cutaneous nerves that interfere with mesh placement were excised as well. In group B, the ilioinguinal nerve was carefully protected throughout the operation. The rest of the procedure was performed in a standardized manner. A monofilament polypropylene mesh (SURGIPRO MESH, Auto Suture, USSC) was anchored with polypropylene sutures (PROLENE, Ethicon, Johnson & Johnson Unit) to the reflected part of inguinal ligament and the floor of the inguinal canal. Extreme care was used during surgery to avoid inclusion of nerve tissue during suturing and mesh placement. The patients were managed in a standard clinical pathway postoperatively and were followed up by the designated occupational therapist at 1 and 6 months after operation.
Follow-up and Outcome Parameters Measurement
During each follow up visit, pain at rest and upon completion of various activities (coughing for 10 times, walking up 3 flights of stairs, and cycling for 10 minutes) were assessed by 4-point scale (none, mild, moderate, or severe). Patients were also requested to fill in a questionnaire regarding pain or discomfort encountered during normal daily activities at home. Chronic groin pain was defined as any discomfort or pain elicited on follow-up or encountered during normal daily activities. Severe pain was defined as pain experienced in any aspects graded moderate or severe at follow-up.
In addition, the groin region was divided into 5 cutaneous areas, namely, outer upper, outer lower, inner upper, inner lower, and scrotal region in relation to the groin incision for sensory assessment. Sensation loss or changes was assessed by the standard Semmes-Weinstein monofilament test performed by the occupational therapist to the 5 regions of each side by the technique described by Bell.16 The nonoperative side of each individual acted as the control. Sensation loss or changes were defined as any asymmetry between corresponding regions of the 2 sides demonstrated by the monofilament test.
Numbness at the groin region and quality of life measurement were assessed by self-filling of a questionnaire in 4-point scale (none, mild, moderate, or severe) and Chinese version of SF-36 during each follow-up, respectively.
Statistical Analysis
The calculated sample size was based on the assumption that a minimum difference in incidence of chronic groin pain of 20% would be meaningful and to achieve 80% power with 2-sided P value <0.05 as significant, 47 patients per group were required. Statistical analysis was based on intention-to-treat analysis and was performed with statistical software Statistical Package for Social Science (version 11.0 for Windows, SPSS, Inc., Chicago IL.). Comparisons were carried out by the Pearson χ2 test or Fisher exact test where appropriate for categorical data and Student t test for parametric data. A 2-sided P value of less than 0.05 was considered significant.
RESULTS
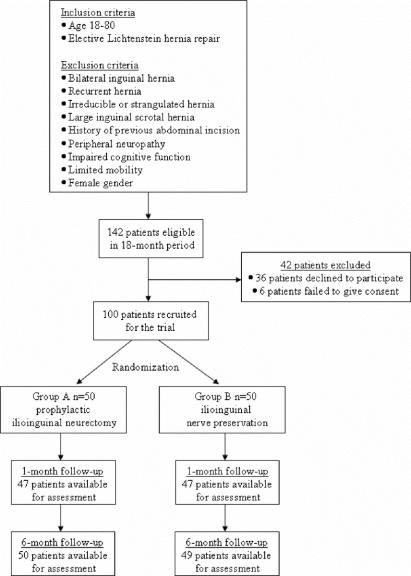
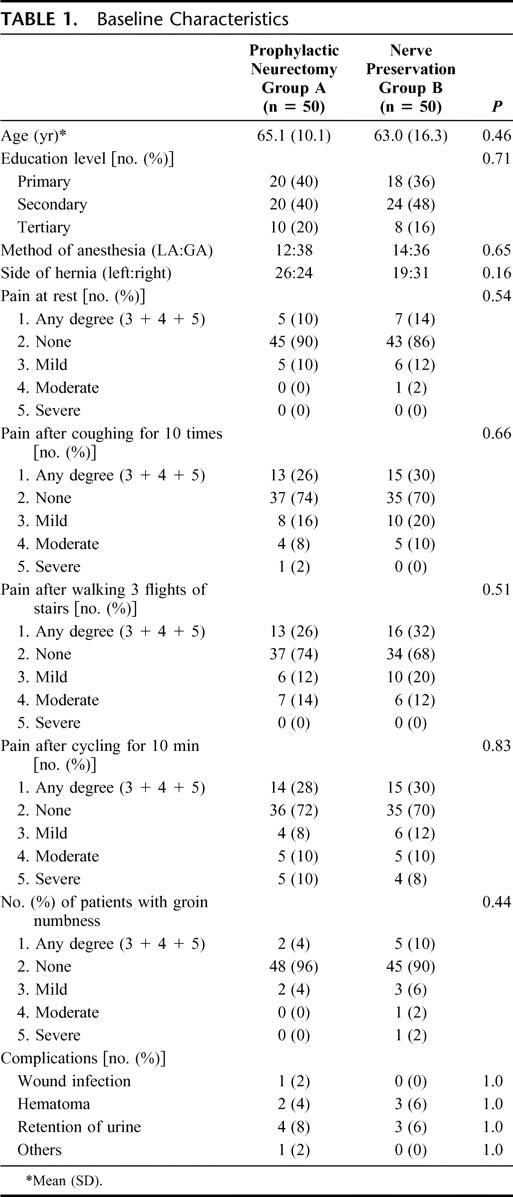
A total of 142 patients were eligible for the study during the 18-month period. Forty-two patients were excluded because 36 patients declined to participate and 6 patients could not give informed consent due to language barrier. A total of 100 patients were randomized with 50 patients in each group. The flow of participants was shown in Figure 1. The mean (SD) age of patients in group A and group B were 65.1 (10.1) and 63.0 (16.3), respectively. The 2 groups were comparable with regard to educational level, method of anesthesia, laterality of hernia, baseline pain measurement during various activities, incidence of groin numbness, and complications. The baseline characteristics of 2 groups of patients are shown in Table 1.
FIGURE 1. Flow diagram of patients.
TABLE 1. Baseline Characteristics
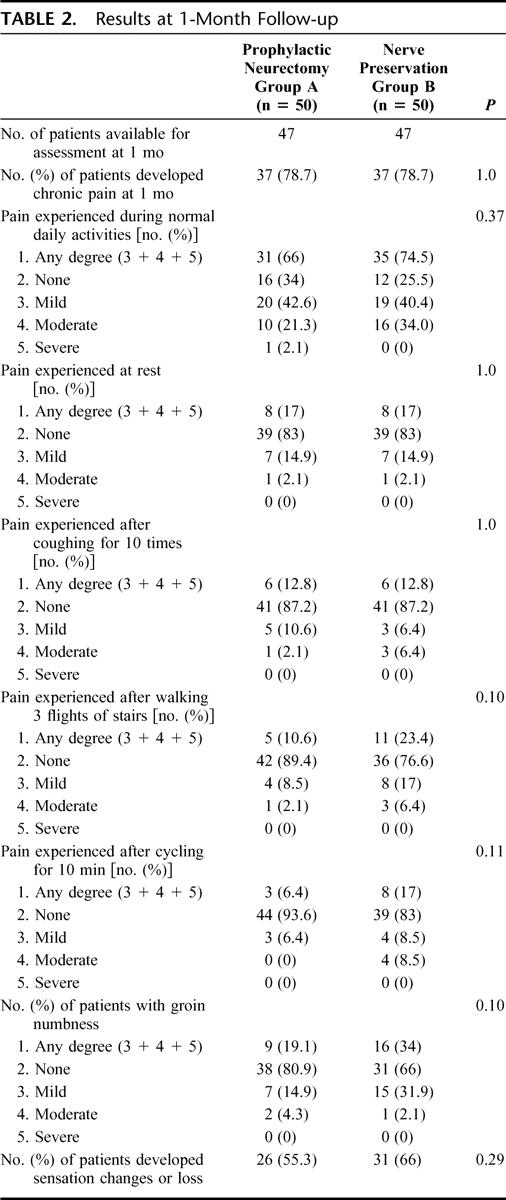
The ilioinguinal nerve was identified in all patients, and complete excision of nerve was confirmed by histology in all patients from group A. Forty-seven patients (95.7%) in both groups were available for assessment at 1 month. The incidence of chronic groin pain, pain experienced during normal daily activities at home and after various activities (at rest, coughing for 10 times, walking up 3 flights of stairs, and cycling for 10 minutes), were similar between the 2 groups. There were no significant differences in the incidence of groin numbness and sensation changes or loss at groin region between the 2 groups. The results at 1 month of follow up are shown in Table 2.
TABLE 2. Results at 1-Month Follow-up
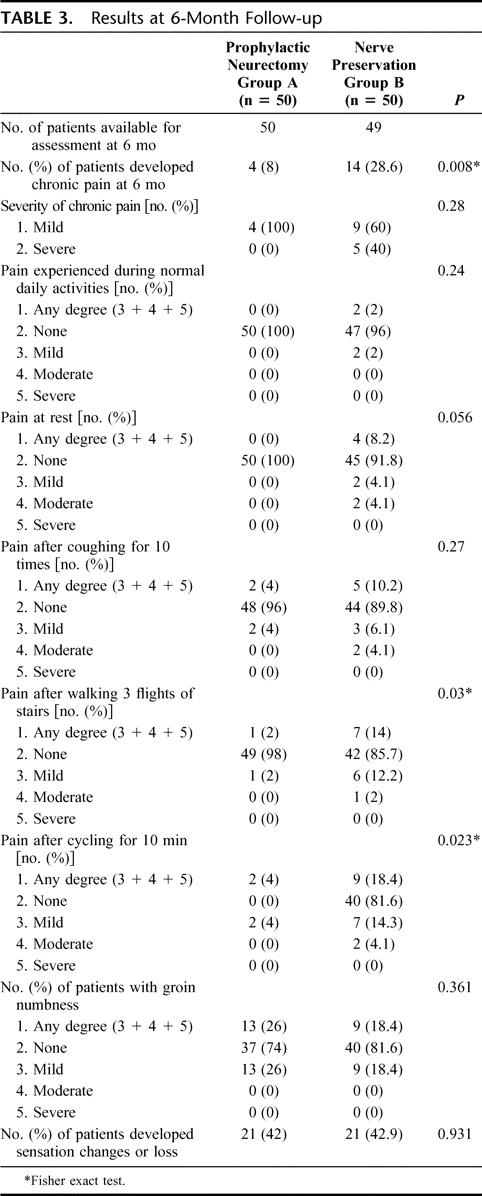
Fifty patients (100%) in group A and 49 patients in group B (98%) were available for assessment at the 6-month follow-up. The incidence of chronic groin pain at 6 months was significantly lower in group A compared with group B (4 [8%] vs. 14 [28.6%]; P = 0.008, Fisher exact test). The incidence of pain experienced after walking 3 flights of stairs and cycling for 10 minutes were significantly lower in group A than group B (1 [2%] vs. 7 [14%]; P = 0.03; 2 [4%] vs. 10 [20.4%]; P = 0.015, Fisher exact test, respectively). The severity of chronic pain developed was comparable between the 2 groups. There were no significant differences in the incidence of pain experienced during normal daily activities at home and after coughing for 10 times at 6 months. The incidences of groin numbness and sensation changes or loss at groin region were also similar between the 2 groups at 6 months. The results are summarized in Table 3.
TABLE 3. Results at 6-Month Follow-up
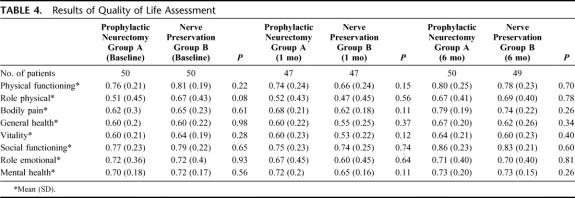
The quality of life assessment at baseline, 1-month and 6-month follow-up, are shown in Table 4. There were no significant differences in the quality of life assessment between the 2 groups at all time points. One patient in group B died of unrelated medical illness before 6-month follow-up. There was no serious complication after surgery. One patient in group A suffered from wound infection requiring laying open the wound and healed by secondary intention. Two patients in group A and 3 patients in group B developed hematoma following surgery, which recovered by conservative management.
TABLE 4. Results of Quality of Life Assessment
DISCUSSION
Chronic groin pain is one of the most debilitating long-term complications after inguinal hernia repair, which can significantly affect the patient's satisfaction and quality of life after the operation.1–5 A proposed mechanism for the development of postoperative chronic groin pain is the inflammation and fibrosis induced by the mesh, which is in close proximity to the ilioinguinal nerve.17 In addition, unintentional injury or strangulation of the ilioinguinal nerve during suturing may also contribute to the phenomenon. There is increasing evidence to suggest that prophylactic excision of ilioinguinal nerve during open hernia repair is not only associated with minimal morbidities but also can potentially decrease the incidence of chronic groin pain following operation.11–13
The first randomized trial to address this problem by Ravichandran et al was underpowered and no definite conclusion could be made.18 Results from subsequent trials regarding chronic groin pain following elective neurectomy have been inconsistent. Interestingly, in a retrospective review of 191 patients who underwent elective excision of the ilioinguinal nerve during open hernia repair showed that none of the patients developed chronic groin pain at 12 months of follow-up.12 In another retrospective study, Dittrick et al reported a significantly lower incidence of chronic groin pain in patients who had elective neurectomy during open inguinal hernia repair when compared with the control group.11 However, these results were not confirmed in a recent randomized controlled trial by Picchio et al,19 who found similar incidence of chronic groin pain between ilioinguinal nerve excision group and control.
Our randomized study revealed that the incidence of chronic groin pain during normal daily activities was similar between the 2 groups which compliment the findings by Picchio et al.19 However, in addition, we found significantly fewer patients in the neurectomy group developed chronic groin pain upon exertion (cycling for 10 minutes and walking up 3 flights of stairs), which has not been previously studied.
The other potential disadvantage of ilioinguinal nerve excision is the morbidity associated with sensory loss over the groin region as well as its impact on quality of life. The previous study by Picchio et al reported increased incidence of sensory loss to pain and touch around the groin region in patients who had nerve excision during open hernia repair.19 However, the current study clearly demonstrated that elective excision of the ilioinguinal nerve was not associated with additional morbidities in neurosensory disturbances, groin numbness or quality of life at the 6-month follow-up. We postulated that the sensory loss caused by neurectomy might be compensated by cross-innervations from contralateral cutaneous nerves. Furthermore, direct meaningful comparison between Picchio et al19 and that of our study is not possible because their methodology used for testing skin sensation was not described. Semmes-Weinstein monofilament testing was adopted in the present study to provide a more standard and objective method to measure skin sensitivity.
Several design improvements to previous trials have been incorporated into the present study. First, a designated occupational therapist who was blinded to the treatment given, and experienced in pain and neurosensory assessment was appointed to carry out all outcome measurement, hence providing more reliable measurements of all outcome parameters. Second, during each follow-up, all patients were challenged by being asked to complete a series of tasks before the pain assessment. Therefore, we were able to examine the effects of exertion on groin pain after surgery, which may better reflect their pain experience during everyday activities. Finally, in this day and age when patient satisfaction is paramount, we included the quality of life assessment in our trial, which provides the clinician a more unique view on the effects of the surgery from the patients’ perspective.
The present study has several limitations. We are not able to demonstrate any significant differences in terms of postoperative incidence or severity of chronic groin pain at rest, during normal daily activities and after coughing between the 2 groups, which can be due to β errors. In addition, meaningful assessment of chronic pain at 1 month may not be possible in the presence of early postoperative swelling and pain, and we speculate that this may contribute to the no differences in incidence of chronic pain at 1 month in contrast to 6 months. Another limitation of the study is that the long-term effect of ilioinguinal neurectomy was not investigated. It is possible that differences in the incidence of chronic pain between the groups, as well as the quality of life measurements will change with longer follow-up duration. Larger clinical trials involving more patients and longer follow-up are warranted to study the long-term effect of prophylactic neurectomy in patients undergoing Lichtenstein repair. Lastly, although we are able to show that prophylactic neurectomy decreases the incidence of chronic pain, the exact reasoning behind this phenomenon remains unknown. Further histologic or nerve conduction studies are required to deduce the exact mechanism.
CONCLUSION
The results of this prospective randomized trial demonstrate that prophylactic excision of ilioinguinal nerve during Lichtenstein inguinal hernia repair decreases the incidence of exertional chronic groin pain after surgery. Furthermore, the procedure is not associated with additional morbidities in terms of local cutaneous neurosensory disturbances or deterioration in quality of life. Ilioinguinal neurectomy should be considered as a routine surgical step during open mesh hernia repair.
ACKNOWLEDGMENTS
The authors thank Frederick Au Lap Yan, Department Manager in Occupational Therapy, and Josephine Wong Man Wah, MSc in Health Care, Department of Occupational Therapy for their input in the study design and logistics.
Footnotes
Reprints: Enders Kwok-Wai Ng, FRCS Ed, Department of Surgery, Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, NT, Hong Kong SAR, China. E-mail: endersng@surgery.cuhk.edu.hk.
REFERENCES
- 1.Bay-Nielsen M, Perkins FM, Kehlet H. Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg. 2001;233:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cunningham J, Temple WJ, Mitchell P, et al. Cooperative hernia study: pain in the postrepair patient. Ann Surg. 1996;224:598–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Callesen T, Bech K, Kehlet H. Prospective study of chronic pain after groin hernia repair. Br J Surg. 1999;86:1528–1531. [DOI] [PubMed] [Google Scholar]
- 4.Poobalan AS, Bruce J, King PM, et al. Chronic pain and quality of life following open inguinal hernia repair. Br J Surg. 2001;88:1122–1126. [DOI] [PubMed] [Google Scholar]
- 5.Courtney CA, Duffy K, Serpell MG, et al. Outcome of patients with severe chronic pain following repair of groin hernia. Br J Surg. 2002;89:1310–1314. [DOI] [PubMed] [Google Scholar]
- 6.Wantz GE. Testicular atrophy and chronic residual neuralgia as risks of inguinal hernioplasty. Surg Clin North Am. 1993;73:571–581. [DOI] [PubMed] [Google Scholar]
- 7.Pappalardo G, Guadalaxara A, Illomei G, et al. Prevention of postherniorrhaphy persistent pain: results of a prospective study. Int Surg. 1999;84:350–353. [PubMed] [Google Scholar]
- 8.Amid PK. Causes, prevention, and surgical treatment of post herniorrhaphy neuropathic inguinodynia: triple neurectomy with proximal end implantation. Hernia. 2004;8:343–349. [DOI] [PubMed] [Google Scholar]
- 9.Starling JR, Harms BA. Diagnosis and treatment of genitofemoral and ilioinguinal neurectomy. World J Surg. 1989;13:586–591. [DOI] [PubMed] [Google Scholar]
- 10.Madura JA, Madura JA 2nd, Copper CM, et al. Inguinal neurectomy for inguinal nerve entrapment: an experience with 100 patients. Am J Surg. 2005;189:283–287. [DOI] [PubMed] [Google Scholar]
- 11.Dittrick GW, Ridl K, Kuhn JA, et al. Routine ilioinguinal nerve excision in inguinal hernia repairs. Am J Surg. 2004;188:736–740. [DOI] [PubMed] [Google Scholar]
- 12.Tsakayannis DE, Kiriakopoulos AC, Linos DA. Elective neurectomy during open, ‘tension free’ inguinal hernia repair. Hernia. 2004;8:67–69. [DOI] [PubMed] [Google Scholar]
- 13.Tons HW Ch, Kupczyk-Joeris D, Rotzscher VM, et al. Chronic inguinal pain following Shouldice repair of primary inguinal hernia. Contemp Surg. 1990;37:24–30. [Google Scholar]
- 14.Lam CL, Gandek B, Ren XS, et al. Tests of scaling assumption and construct validity of the Chinese (HK) version of the SF-36 Health Survey. J Clin Epidemiol. 1998;51:1139–1147. [DOI] [PubMed] [Google Scholar]
- 15.Lichtenstein IL, Shulman AG, Amid PK, et al. The tension-free hernioplasty. Am J Surg. 1989;157:188–193. [DOI] [PubMed] [Google Scholar]
- 16.Bell JA. Semmes-Weinstein monofilament testing for determining cutaneous light touch/deep pressure sensation. Star. 1984:44(2). [Google Scholar]
- 17.Heise CP, Starling JR. Mesh inguinodynia: a new clinical syndrome after inguinal herniorrhaphy? J Am Coll Surg. 1998;187:514–518. [DOI] [PubMed] [Google Scholar]
- 18.Ravichandran D, Kalambe BG, Pain JA. Pilot randomized controlled study of preservation or division of ilioinguinal nerve in open mesh repair of inguinal hernia. Br J Surg. 2000;87:1166–1167. [DOI] [PubMed] [Google Scholar]
- 19.Picchio M, Pallimento D, Attanasio U, et al. Randomized controlled trial of preservation or elective division of ilioinguinal nerve on open inguinal hernia repair with polypropylene mesh. Arch Surg. 2004;139:755–758. [DOI] [PubMed] [Google Scholar]