Abstract
Objective To evaluate the cost effectiveness of acupuncture in the management of persistent non-specific low back pain.
Design Cost effectiveness analysis of a randomised controlled trial.
Setting Three private acupuncture clinics and 18 general practices in York, England.
Participants 241 adults aged 18-65 with non-specific low back pain of 4-52 weeks' duration.
Interventions Ten individualised acupuncture treatments over three months from acupuncturists trained in traditional Chinese medicine (n = 160) or usual care only (n = 81).
Main outcome measure Incremental cost per quality adjusted life year (QALY) gained over two years.
Results Total costs to the United Kingdom's health service during the two year study period were higher on average for the acupuncture group (£460; €673; $859) than for the usual care group (£345) because of the costs associated with initial treatment. The mean incremental health gain from acupuncture at 12 months was 0.012 QALYs (95% confidence interval -0.033 to 0.058) and at 24 months was 0.027 QALYs (-0.056 to 0.110), leading to a base case estimate of £4241 per QALY gained. This result was robust to sensitivity analysis. The probabilistic sensitivity analysis showed acupuncture to have a more than 90% chance of being cost effective at a £20 000 cost per QALY threshold.
Conclusion A short course of traditional acupuncture for persistent non-specific low back pain in primary care confers a modest health benefit for minor extra cost to the NHS compared with usual care. Acupuncture care for low back pain seems to be cost effective in the longer term.
Trial registration ISRCTN80764175.
Introduction
In a national survey carried out on behalf of the Department of Health in England and Wales, 40% of the adult population reported having experienced back pain within the preceding 12 months.1 The annual cost of low back pain to the United Kingdom's health service has been estimated at £480m (€703m; $901m), with the annual cost to a general practice with a list size of 10 000 patients estimated at £88 000 in 1994.2 A recent study estimated that the economic burden of low back pain in lost productivity and disability or sickness benefits is £10 668m per year.3
The use of acupuncture as an approach for the management of chronic pain, including low back pain, is receiving increasing recognition from both the public and professionals. Several randomised trials on this topic have, however, been criticised for their quality.4 We assessed the cost effectiveness of acupuncture for the treatment of persistent non-specific low back pain.
Methods
Patients (n = 241) with persistent non-specific low back pain of 4-52 weeks' duration, who were diagnosed as suitable for management in primary care, were recruited to the trial through referral from 43 general practitioners. Patients were randomly allocated either to receive up to 10 acupuncture treatments over three months from acupuncturists trained in traditional Chinese medicine (n = 161) or to receive usual care only (n = 81). Randomisation was in a ratio of 2:1 to the offer of acupuncture to test for effects between acupuncturists. The primary clinical outcome was the bodily pain dimension on the SF-36, measured at 12 and 24 months. After adjusting for baseline score and for any clustering by acupuncturist, we found an estimated intervention effect of 5.6 points (95% confidence interval -0.2 to 11.4, P = 0.06) at 12 months (n = 213) and 8.0 points (2.8 to 13.2, P = 0.003) at 24 months (n = 182; see accompanying clinical paper for details).5 The difference in final pain scores between groups was small, about 10%-15% that of the usual care group. Costs were measured from both an NHS and a societal perspective. Effectiveness was measured as quality adjusted life years (QALYs) gained. Costs were measured in sterling prices for 2002-3. The primary economic analysis is over the 24 month period, as this incorporates comprehensive data on differentials for resource use and provides the most accurate assessment of costs and QALYs gained in the longer term.6
Health outcomes and health resource use
We used the algorithm developed by Brazier et al,7 to devise a single preference based measure of health related quality of life, the SF-6D, from patients' responses to the SF-36 health status questionnaire at baseline and at 3, 12, and 24 months. The algorithm generates an index value where 0 represents death and 1 perfect health, with intermediate values for all remaining health states. The valuations are based on the preference weights obtained for a series of health states defined by the SF-6D from a sample of 611 members of the UK general population. We calculated the area under the curve to measure the QALY gain for each patient.8
We collected details of healthcare utilisation from two main sources: notes from the general practice and a patient completed questionnaire on use of resources. To collect information on the number and type of contacts with general practitioners and practice nurses and drugs prescribed we examined the general practice notes for all participants. Other data on healthcare usage over the 24 months was collected by means of a self completed questionnaire, administered to participants at 12 and 24 months. We also collected information on admissions to hospital, outpatient visits, and other visits to NHS facilities (for example, physiotherapy, chiropractic, and osteopathy services during the preceding 12 months). We collected the date and duration of stays in an NHS hospital from the resource use questionnaire and cross referenced these directly with the relevant hospital. Patients were also asked to document their use of private treatments (physiotherapy, acupuncture, osteopathy, chiropractic services, and other services or products). The resource use questionnaire also included questions relating to the estimation of costs due to lost productivity, including employment status and time lost from work as a result of low back pain.
Unit costs
Unit costs are based on the financial year 2002-3. We obtained these from national sources whenever possible, including the Personal Social Services Research Unit Database,9 NHS Reference Costs,10 and the British National Formulary.11 When national costs were unavailable, we obtained local unit costs from the healthcare centres in the trial location. Unit costs for acupuncture delivered in the study reflect payments made to practitioners by York Health Authority for the duration of the study. We matched NHS acupuncture costs to local private sector fees at the start of the study. Time lost from work because of low back pain was valued using age and sex adjusted average daily wage rates from the Office for National Statistics new earnings survey, 2003.12 Table 1 provides details of unit costs. The costs associated with non-prescription drugs and visits for private health care were reported by the patients.
Table 1.
Unit costs of healthcare resources used
| Healthcare resource | Unit | Cost per unit (£) | Details |
|---|---|---|---|
| Acupuncture: | |||
| Initial consultation (60 minutes) | Visit | 34.00 | Treatment costs as met by York Health Authority. NHS costs were linked to local private sector charges at time of study |
| Subsequent treatment (45 minutes) | Visit | 24.00 | Treatment costs as met by York Health Authority |
| Non-study NHS acupuncture | Visit | 24.00 | Cost assumed to be equivalent to costs for study acupuncture treatment |
| Private visit | Visit | 24.00 | Includes private acupuncture sessions for additional treatment after study acupuncture |
| NHS visits*: | |||
| Hospital inpatient8 | Day | 273.00 | Mean cost per inpatient day (generic) |
| Hospital outpatient8 | Visit | 82.00 | Mean cost per outpatient attendance (generic) |
| Hospital pain clinic8 | Visit | 82.00 | |
| General practitioner consultation8 | Visit | 20.00 | Assumes consultation lasts 9.36 minutes |
| Physiotherapy8 | Visit | 18.00 | Assumes visit lasts 30 minutes |
| Other NHS practitioner | Visit | 25.00 | Primary care clinic visit to chiropractor or osteopath (rarely reported) |
| Other costs: | |||
| Private health care | Visit | Various | Patients reported individual costs in trial data |
| Over the counter drugs | Item | Various | Patients reported individual costs in trial data |
| Prescription drugs10 | Item | Various | Specified by dosage and pack size |
| Time off work sick11 | Day | 88.86 | One fifth of average weekly earnings |
NHS visit costs include salary, on-costs, qualifications, overheads, and capital costs.
Cost utility analysis
All economic analyses were carried out on an intention to treat basis. Data on resource use, costs, and health outcomes were analysed with SPSS version 12.0. Despite the potential skewness of cost data, the arithmetic mean and standard t test based confidence intervals are considered appropriate for comparing mean costs between two groups, and the most relevant statistics for informing decision making.13 In estimating the incremental cost effectiveness ratio of acupuncture treatment for low back pain for the base case we did not impute for cases with missing SF-6D data, therefore the cost effectiveness analysis sample included those patients who completed the SF-36 at all four time points and therefore for whom QALYs could be calculated. Data relating to resource use and cost were available for a larger sample of patients, and statistics for these variables are presented for patients who responded.
To confirm the validity of the base case results we used a probabilistic sensitivity analysis with bootstrapping when the original data were used to provide an empirical estimate of the sampling distribution through repeated resampling from the observed data.14 We carried out sensitivity analyses to test the robustness of the results to changes from the base case by using multiple imputation to impute missing data relating to NHS costs and SF-6D outcomes15; by using lost productivity costs; and by excluding those patients who were permanently unable to work as a result of low back pain, when costs were expected to be higher and outcomes poorer.
Multiple imputation is a Monte Carlo simulation technique where each missing datum case is replaced by a set of plausible estimates that are drawn from the predictive distribution of the missing data given the observed data. In contrast to the more naive approaches previously highlighted, multiple imputation has the advantage that it includes a random component to reflect that imputed values are estimated rather than known with certainty. As such, multiple imputation is likely to produce more accurate estimates of the standard errors and variances of mean health state values at each time point than other methods of imputation.16 We discounted costs and outcomes at 3.5% each during the 12-24 months of the study, the current recommended rate for public sector projects.17 The cost effectiveness of the intervention to the NHS was assessed bearing in mind recent guidance from the National Institute for Health and Clinical Excellence relating to the threshold the NHS can afford to pay for a new technology.6
Results
Table 2 shows the baseline characteristics of those patients receiving acupuncture care or usual care for persistent non-specific low back pain who completed the SF-36 at all four time points (for whom SF-6D and QALY scores could be calculated) compared with those patients with missing SF-36 data at any time point. The group with complete data also formed the sample for the base case analysis of cost effectiveness.
Table 2.
Characteristics of patients treatment for persistent non-specific low back pain for whom quality adjusted life years could be calculated* compared with those with missing SF-6D scores at any time point. Values are percentages (numbers) unless stated otherwise
|
Characteristic
|
Acupuncture group
|
Usual care group
|
||
|---|---|---|---|---|
| Complete SF-6D data (n=110) | Missing SF-6D data (n=49)† | Complete SF-6D data (n=47) | Missing SF-6D data (n=33)1 | |
| Male | 36 (39) | 43 (21) | 34 (16) | 42 (14) |
| In full time employment | 50 (55) | 37 (18) | 55 (26) | 24 (8) |
| Permanently unable to work because of low back pain | 5 (5) | 12 (6) | 0 | 0 |
| Low back pain every day in past week | 91 (50) | 61 (30) | 85 (23) | 73 (24) |
| >5 previous episodes of low back pain | 48 (53) | 47 (23) | 57 (27) | 51 (17) |
| Mean (SD) age in years (range) | 43, 11.0 (21-64) | 41, 10.4 (21-64) | 47, 10.2 (29-64) | 41, 9.8 (20-60) |
| Mean (SD) weeks with current episode of low back pain (range) | 17.2, 13.3 (4-48) | 17.8, 13.8 (4-48) | 17.4, 15.0 (4-48) | 19.2, 16.2 (4-48) |
Complete SF-6D scores at baseline and at 3, 12, and 24 months.
Data were missing for one patient who withdrew from the study shortly after randomisation.
Compared with the base case sample, patients who were excluded were less likely to be in full time employment and to report more than five previous episodes of back pain.
Patients in the acupuncture group had an average of eight sessions with a study acupuncturist (table 3). Seven patients in the acupuncture group and nine in the usual care group received NHS acupuncture during the trial period. Several patients in the acupuncture arm (n = 19) purchased additional private acupuncture.
Table 3.
Resource use of patients receiving treatment for persistent non-specific low back pain over 24 months and health related quality of life measured by SF-6D
|
Resource use
|
Acupuncture group
|
Usual care group
|
||
|---|---|---|---|---|
| Mean (SD) | No of patients | Mean (SD) | No of patients | |
| Acupuncture: | ||||
| Study acupuncture* | 8.08 (2.93) | 159 | 0 | 80 |
| NHS acupuncture | 0.32 (1.27) | 123 | 1.27 (4.87) | 59 |
| Private acupuncture | 0.66 (4.03) | 123 | 0.0 (0.00) | 59 |
| Hospital stay (days) | 0.01 (0.09) | 123 | 0.07 (0.37) | 59 |
| Other healthcare visits: | ||||
| General practitioner | 3.78 (3.36) | 123 | 4.25 (4.74) | 59 |
| Outpatient | 0.50 (1.62) | 123 | 0.41 (1.95) | 59 |
| NHS | 8.79 (5.30) | 123 | 9.59 (5.60) | 59 |
| Private | 0.98 (4.68) | 123 | 0.90 (3.65) | 59 |
| Health related quality of life†: | ||||
| Baseline | 59.7 | 159 | 60.7 | 80 |
| 3 months | 71.3 | 146 | 69.9 | 70 |
| 12 months | 72.5 | 134 | 73.0 | 56 |
| 24 months | 74.2 | 113 | 72.9 | 50 |
Significant difference between means P<0.05.
SF-6D score out of 100.
An improvement was found in health related quality of life over the 24 months in both groups, with the acupuncture arm reporting a slightly higher mean health related quality of life score at 24 months (table 3). With the exception of acupuncture, the mean differences between groups were not statistically significant at any time point.
Table 4 documents the mean NHS costs of healthcare resource use for low back pain treatment during the trial. The costs of initial acupuncture treatment differed significantly between the groups. The total mean costs of treatment to the NHS for the acupuncture group (£471.10) were higher than for the usual care group (£332.24) and the difference was statistically significant. The initial acupuncture treatment accounts for about 45% of the total NHS costs of treatment for the acupuncture group.
Table 4.
Mean NHS costs (£) of healthcare resource use for treatment for persistent non-specific low back pain over 24 months
| Resource | Mean (SD) costs for acupuncture care (n=123) | Mean (SD) costs for usual care (n=59) | Difference (95% CI) in mean costs |
|---|---|---|---|
| Acupuncture: | |||
| Study acupuncture | 214.01 (68.49) | — | 196.38 to 231.62* |
| NHS acupuncture | 9.26 (83.27) | 31.46 (120.44) | −52.45 to 82.06 |
| Hospital stay (days) | 2.22 (24.62) | 18.32 (99.66) | −35.07 to 2.49 |
| Other healthcare visits: | |||
| General practitioner | 78.15 (66.89) | 88.07 (95.08) | −34.43 to 14.59 |
| Outpatient | 48.00 (167.30) | 84.78 (256.59) | −99.42 to 25.86 |
| NHS | 87.89 (52.97) | 95.93 (55.99) | −24.91 to 8.82 |
| Drugs for low back pain | 34.12 (114.94) | 16.47 (27.33) | −12.31 to 47.61 |
| Total NHS costs (discounted)* | 471.10 (341.61) | 332.24 (426.50) | 22.91 to 254.82* |
Significant difference between means P<0.05.
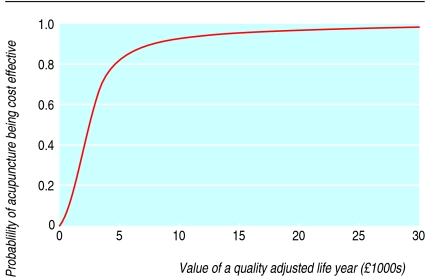
Overall the incremental cost effectiveness ratio for acupuncture in the treatment of low back pain was positive (table 5), with a mean of £4241 at 24 months. The figure shows the probability of the intervention being cost effective using the base case data for a range of cost effectiveness ceilings. Assuming an implicit threshold of a maximum willingness to pay of £20 000 for a QALY, the probability of the cost per QALY of acupuncture for low back pain falling below this threshold value was over 90%.
Table 5.
Cost effectiveness of acupuncture care or usual care for treatment of persistent non-specific low back pain
| Variable | Mean (SD) acupuncture care | Mean (SD) usual care | Difference (95% CI) in means |
|---|---|---|---|
| Base case: | |||
| Mean NHS cost, discounted (£) | 459.70 (376.39); n=105 | 345.21 (550.44); n=44 | 114.50 (−39.74 to 268.73) |
| QALY gain (SF-6D) | 1.453 (0.248); n=105 | 1.426 (0.191); n=44 | 0.027 (−0.056 to 0.110) |
| ICER (£): base case | — | — | 4241 (191 to 28 026) |
| Imputation: | |||
| Mean NHS cost, discounted (£) | 460.20 (338.67); n=159 | 338.14 (421.38); n=80 | 122.07 (22.61 to 221.52*) |
| QALY gain (SF-6D) | 1.459 (0.247); n=159 | 1.430 (0.208); n=80 | 0.029 (−0.034 to 0.092) |
| ICER (£): imputation | — | — | 4209 (182 to 27 899) |
QALY=quality adjusted life year; ICER=incremental cost effectiveness ratio.
Significant difference between means P<0.05.
Figure 1.
Cost effectiveness acceptability curve of acupuncture for persistent non-specific low back pain using base case data for range of cost effectiveness ceilings
Sensitivity analyses
When multiple imputation was used to impute missing data relating to NHS costs or QALYs, the incremental cost effectiveness ratio for acupuncture treatment of low back pain was £4209 at 24 months (table 5). When patients who were permanently unable to work because of low back pain were excluded the incremental cost was reduced and the QALYS gained increased compared with the base case, resulting in improved cost effectiveness for acupuncture treatment (table 6).
Table 6.
Sensitivity analyses
| Variable | Sample size | Incremental cost (£) | QALYs gained | Incremental cost per QALY gained (£) |
|---|---|---|---|---|
| Base case* | 149 | 114.50 | 0.027 | 4241 |
| Imputation of QALYs and cost*† | 239 | 122.07 | 0.029 | 4209 |
| Excluding patients permanently unable to work because of low back pain | 142 | 82.06 | 0.039 | 2104 |
| Inclusion of patient costs | 132 | 132.18 | 0.043 | 3074 |
| Inclusion of patient plus lost productivity costs | 129 | −248 | 0.058 | Acupuncture dominant (cost per QALY gained <0) |
QALY=quality adjusted life year.
See table 5.
Using multiple imputation to predict missing values.
The inclusion of productivity costs noticeably improved cost effectiveness, with this scenario indicating overall cost savings from using acupuncture treatment (table 6).
Discussion
Acupuncture treatment for persistent non-specific low back pain confers a modest benefit to health, as measured by quality adjusted life years (QALYs), at relatively minor extra cost to the NHS compared with usual care. This finding is complemented by the clinical results detailed in the accompanying paper, which found weak evidence of an effect on pain at 12 months but stronger evidence of a small benefit at 24 months.5 We estimated the incremental cost effectiveness to be £4241 per QALY gained in the base case. This represents a conservative estimate because it excludes cost savings associated with productivity gains. From a societal perspective when gains in productivity are included then acupuncture care for low back pain becomes dominant in that it is less expensive and confers greater health benefits than usual care. It is likely, however, that this represents an underestimate of the cost per QALY because the quality of life measure will in part take into account this improved productivity.
A potential limitation of the cost effectiveness study relates to the use of a patient completed questionnaire to obtain information on use of resources. This method can be criticised on the basis that it may be the subject of recall bias. On a practical level, however, this method offers an appropriate and efficient mechanism for obtaining this information. To minimise the risk of recall bias for hospital episodes related to low back pain, the date and duration of hospital stays were collected from the resource use questionnaire and cross referenced directly with the relevant hospital. A further limitation is the proportion of missing data for the base case analysis. This amount of missing data is not unusual for community based interventions and also reflects the extended duration (24 months) of the randomised controlled trial. Principally this indicates failure of a proportion of patients to complete the SF-36 at all four time points. Although the amount of missing data may affect the generalisability of the findings, the characteristics of patients excluded from the base case analysis were broadly similar to those who were included.
We assessed the cost effectiveness of acupuncture treatment for low back pain using systematic and transparent methods. A previous study assessed the cost effectiveness of acupuncture for headache using similar methods to those reported here but over a shorter period (12 months) and estimated the incremental cost effectiveness ratio to be £9180.18 As the authors note, however, the incremental cost effectiveness ratio is likely to reduce over longer periods because of increased gains in QALYs. It is difficult to assess the extent to which our results are comparable to those of other studies assessing interventions for low back pain because few studies have assessed the relative costs and effectiveness of treatments for low back pain. Studies have tended to assess effectiveness or costs in isolation and have tended not to use a generic outcome measure such as QALYs that would facilitate comparisons across alternative interventions. One study concluded that chiropractic treatment was more effective than outpatient management for patients with chronic or severe low back pain but did not assess the relative costs of each intervention.19 More recently trials have been reported of physiotherapy, exercise, and manipulation for low back pain.20,21 The trial of physiotherapy did not report cost effectiveness.20 The United Kingdom back pain exercise and manipulation trial showed exercise to have an incremental cost effectiveness ratio of £8300 compared with “best care,” but it did not compare interventions with usual care.21 The open and pragmatic nature of our trial allowed acupuncture care to be compared with usual care in everyday practice. Given that usual care comprised a mix of interventions,5 it was, however, not possible to isolate the costs and effectiveness of individual treatments as part of the package of usual care.22
Recent guidance from NICE indicates that a ceiling ratio of £20 000 per QALY represents the threshold of what the NHS can afford to pay for additional QALYs, unless other arguments exist for adopting the technology.6 If £20 000 is taken as the maximum acceptable cost effectiveness ratio, then acupuncture for the treatment of low back pain seems cost effective.
On the basis of our findings of cost effectiveness, longer term reduction in pain, and the acceptability of acupuncture care to patients as reported in the accompanying clinical paper,5 commissioners of musculoskeletal services would be justified to consider making available the referral of patients in primary care to a short course of traditional acupuncture care for persistent non-specific low back pain.
An evidence base showing the cost utility of acupuncture and other short term packages of care, such as massage, osteopathy, chiropractic, or physiotherapy could facilitate the development of NHS policy on the basis of affordability and allow patients with low back pain to choose their treatment.
What is already known on this topic
Many people seek acupuncture care for low back pain
No rigorous assessments have been made of the cost effectiveness of such care
What this study adds
A short course of acupuncture (up to 10 sessions) for low back pain is associated with increased costs to the United Kingdom's health service but improved health related quality of life in the long term
If decision makers are willing to pay up to £20 000 to gain one quality adjusted life year, then acupuncture for low back pain seems cost effective
We thank the patients, primary care staff, and acupuncturists; Lucy Thorpe and the trial advisory group members, Trevor Sheldon, Sally Bell-Sayer, and David Laverick; and Anne Morgan and Tessa Peasbody who contributed to the economic analysis. ©Crown copyright 2006.
Contributors: KJT was principal investigator and implemented the study. JB developed the economic evaluation protocol. LT, HMacP, and JB secured funding for the 24 month follow up. LT collected costing data. JR and JB carried out the economic analysis. JR wrote the original draft with JB. All authors commented on the draft and the interpretation of the findings. JR and JB are guarantors.
Funding: This study was funded by the UK NHS Executive health technology programme. The views and opinions expressed do not necessarily reflect those of the NHS Executive. York Health Authority funded the treatment costs of the acupuncture. The National Coordinating Centre for Health Technology Assessment reviewed the protocol and the final report but had no direct involvement in the research process. KJT and JB joined the commissioning group of the National Coordinating Centre for Health Technology Assessment after funding for this study was awarded. JonNicholl is currently chair of the National Coordinating Centre for Health Technology Assessment commissioning group.
Competing interests: None declared.
Ethical approval: This study was approved by York research ethics committee.
References
- 1.Department of Health. The prevalence of back pain in Great Britain in 1998. London: Government Statistical Service, 1999.
- 2.Clinical Standards Advisory Group on Back Pain. Back pain: epidemiology and costs. London: HMSO, 1994.
- 3.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain 2000;84: 95-103. [DOI] [PubMed] [Google Scholar]
- 4.Ezzo J, Berman B, Hadhazy VA, Jadad AR, Lao L, Singh BB. Is acupuncture effective for the treatment of chronic pain? A systematic review. Pain 2000;86: 217-25. [DOI] [PubMed] [Google Scholar]
- 5.Thomas KJ, MacPherson H, Thorpe L, Brazier J, Fitter M, Campbell M, et al. Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain. BMJ 2006. doi: 10.1136/bmj.38878.907361.7C. [DOI] [PMC free article] [PubMed]
- 6.National Institute of Clinical Excellence. Guide to the methods of technology appraisal. London: NICE, April 2004. [PubMed]
- 7.Brazier J, Roberts J, Deverill M. The estimation of a preference based measure of health from the SF-36. J Health Econ 2002;21: 271-92. [DOI] [PubMed] [Google Scholar]
- 8.Mathews JNS, Altman D, Campbell MJ. Analysis of serial measurements in medical research. BMJ 1990;300: 230-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Netten A, Rees T, Glenys H. Unit costs of health and social care. Canterbury, University of Kent: Personal Social Services Research Unit, 2001.
- 10.NHS Executive. NHS reference costs. London: NHS Executive, 2004.
- 11.British Medical Association, Royal Pharmaceutical Society of Great Britain. British national formulary. London: BMA, RPS, 2002. (No 43).
- 12.Office for National Statistics. New earnings survey, 2003. London: ONS.
- 13.Thompson SG, Barber JA. How should cost data in pragmatic randomized trials be analysed? BMJ 2000;320: 1197-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glick H, Briggs AH, Polsky D. Quantifying stochastic uncertainty and presenting results of cost effectiveness analyses. Expert Rev Pharmacoecon Outcomes Res 2001;1: 25-36. [DOI] [PubMed] [Google Scholar]
- 15.Rubin DB. Multiple imputation for non-response in surveys. New York: Wiley, 1987.
- 16.Manca A, Palmer S. Handling missing data in patient-level cost-effectiveness analysis alongside randomized clinical trials. Applied Health Econ Health Policy 2005;4: 65-75. [DOI] [PubMed] [Google Scholar]
- 17.HM Treasury. The green book appraisal and evaluation in central government. London: Stationery Office, 2003.
- 18.Wonderling D, Vickers AJ, Grieve R, McCartney R. Cost effectiveness analysis of a randomised trial of acupuncture for chronic headache in primary care. BMJ 2004;328: 747-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meade TW, Dyer S, Browne W, Townsend J, Frank AO. Low back pain of mechanical origin: randomised comparison of chiropractic and hospital outpatient treatment. BMJ 1990;300: 1431-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frost H, Lamb S, Doll H, Taffe Carver P, Stewart Brown S. Randomised controlled trial of physiotherapy compared with advice for low back pain. BMJ 2004;329: 708-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.UK BEAM Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: cost effectiveness of physical treatments for back pain in primary care. BMJ 2004;329: 1381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.MacPherson H. Pragmatic clinical trials. Complement Ther Med 2004;12: 136-40. [DOI] [PubMed] [Google Scholar]