The obesity epidemic in the United Kingdom is out of control, and none of the measures being undertaken show signs of halting the problem, let alone reversing the trend. The United States is about 10 years ahead in terms of its obesity problem, and it has an epidemic of type 2 diabetes with obesity levels that are rocketing. Obesity is a global problem—levels are rising all over the world. Moreover, certain ethnic groups seem to be more sensitive than others to the adverse metabolic effects of obesity. For example, high levels of diabetes and related diseases are found in South Asian and Arab populations. Although most of the medical complications and costs of obesity are found in adults, obesity levels are also rising in children in the UK and elsewhere.
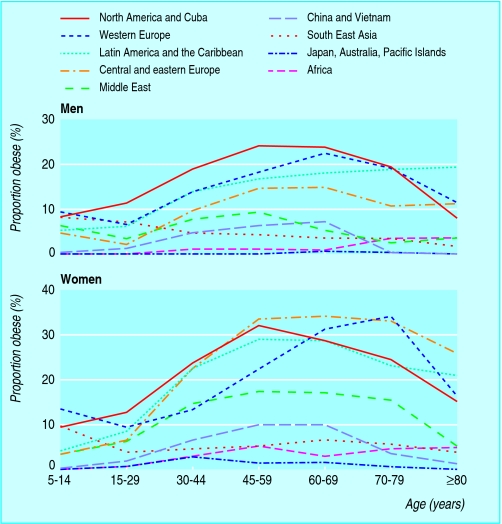
Figure 1.
Prevalence of obesity worldwide. Adapted from Haslam D, James WP. Lancet 2005;366: 1197-209
Table 1.
Definition of obesity
| • Obesity is excess body fat accumulation with multiple organ-specific pathological consequences |
| • Obesity is categorised by body mass index (BMI), which is calculated by weight (in kilograms) divided by height (in metres) squared. A BMI > 30 indicates obesity and it is reflected by an increased waist circumference |
| • Waist circumference is a better assessor of metabolic risk than BMI because it is more directly proportional to total body fat and the amount of metabolically active visceral fat |
Limited time to act
Obesity can be dealt with using three expensive options:
Treat an almost exponential rise in secondary clinical consequences of obesity
Treat the underlying obesity in a soaring number of people to prevent secondary clinical complications
Reverse the societal and commercial changes of the past 200 years, which have conspired with our genes to make overweight or obesity more normal.
Sheaves of evidence based guidelines give advice on the treatment of all the medical consequences of obesity, and an evidence base for identifying and treating obesity is accumulating. Although the principles of achieving energy balance are known, an evidence base of effective measures for preventing obesity does not exist. The methods of randomised clinical trials are inappropriate, and so some form of continuous improvement methodology is needed.
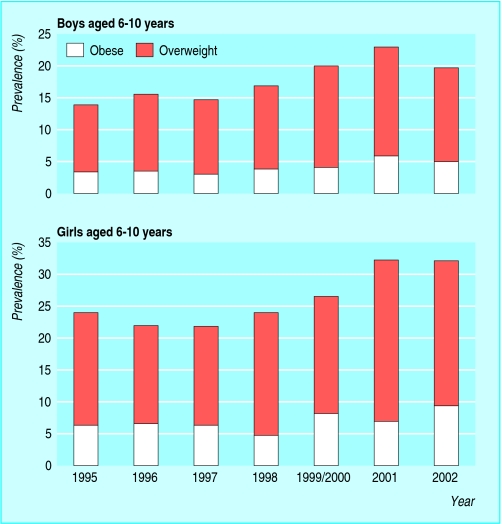
Figure 2.
Results from Health Survey for England 2002. The most recent Health Survey for England (2004) states that “Between 1995 and 2001, mean BMI increased among boys (from 17.6 to 18.1) and girls (from 18.0 to 18.4) aged 2-15”
In the United Kingdom, even if preventive measures against obesity were successful immediately (so that not one more person became obese) and people who are obese do not gain weight, there would still be an epidemic of diabetes and its complications within 10-20 years. This is because so many young people are already in the clinically “latent” phase of obesity, before the clinical complications present. Treatment of obesity must be prioritised alongside prevention. It will take an unprecedented degree of cooperation between government departments; schools; food, retail, and advertising industries; architects and town planners; and other groups to improve our “toxic” environment. Meanwhile, in their clinics, doctors have to deal with the obesity epidemic one person at a time—a daunting role.
This is the first article in the series
Health consequences
It has been known for centuries that obesity is the cause of serious chronic disease. Only relatively recently has the full spectrum of disease linked to obesity become apparent—for example, recognition that most hypertension, previously considered “essential,” is secondary to obesity. Among preventable causes of disease and premature death, obesity is overtaking smoking.
Table 2.
Health consequences of obesity
| Greatly increased risk (relative risk >3) |
| • Diabetes |
| • Hypertension |
| • Dyslipidaemia |
| • Breathlessness |
| • Sleep apnoea |
| • Gall bladder disease |
| Moderately increased risk (relative risk about 2-3) |
| • Coronary heart disease or heart failure |
| • Osteoarthritis (knees) |
| • Hyperuricaemia and gout |
| • Complications of pregnancy—for example, pre-eclampsia |
| Increased risk (relative risk about 1-2) |
| • Cancer (many cancers in men and women) |
| • Impaired fertility/polycystic ovary syndrome |
| • Low back pain |
| • Increased risk during anaesthesia |
| • Fetal defects arising from maternal obesity |
Economic costs
Every year obesity costs the UK economy £3.5bn (€5.1bn, $6.4bn), and results in 30 000 deaths;18 million days of work taken off for sickness each year. Strategies for primary care that encourage primary prevention of chronic disease, including obesity management, would achieve considerable financial rewards. The Counterweight study on obesity reduction and maintenance showed that obese people take up a greater proportion of time in general practice than non-obese people. Obese patients also need more referral, and are prescribed more drugs across all the categories of the British National Formulary than people of normal weight. Resources are being spent mainly treating the secondary consequences of obesity. Preventing obesity is not encouraged. The Counterweight study also showed that obesity can be managed in a population without a major increase in resources.
Table 3.
Costs attributable to obesity in Scotland in 2003*
|
GP contacts |
Prescribing costs (£) |
|||
|---|---|---|---|---|
| Illness | No | Cost (£) | Per person | Total |
| Obesity |
58 346 |
758 503 |
3 |
2 818 025 |
| Hypertension |
988 493 |
12 850 406 |
179 |
43 650 190 |
| Type 2 diabetes |
65 777 |
855 098 |
409 |
18 901 220 |
| Angina pectoris |
93 178 |
1 211 309 |
720 |
20 348 921 |
| Myocardial infarction |
33 372 |
433 838 |
720 |
14 598 139 |
| Osteoarthritis |
37 003 |
481 045 |
112 |
2 240 485 |
| Stroke |
5829 |
75 777 |
35 |
106 333 |
| Gallstones |
1575 |
20 470 |
67 |
57 448 |
| Colon cancer |
2631 |
34 207 |
0 |
0 |
| Ovarian cancer |
382 |
4967 |
91 |
6970 |
| Gout |
17 321 |
225 170 |
25 |
244 155 |
| Prostate cancer |
0 |
0 |
2949 |
162 609 |
| Endometrial cancer |
0 |
0 |
168 |
14 362 |
| Rectal cancer |
0 |
0 |
1114 |
12 812 |
| Total | 1 303 907 | 16 950 791 | 103 161 670 | |
£1 = €1.40 or US$1.8
Adapted from Walker A. The cost of doing nothing—the economics of obesity in Scotland. University of Glasgow, 2003 (www.cybermedicalcollege.com/Assets/Acrobat/Obesitycosts.pdf)
Benefits of managing obesity
Uniquely among chronic diseases, obesity does not need a scientific breakthrough to be treated successfully. Enough is known about the causes of obesity and that diet, exercise, behaviour therapy, drugs, and even laparoscopic surgery can be effective. The barriers to successful management of obesity are political and organisational ones, along with a lack of resources. In the long term, the cheapest and most effective strategy to improve the health of the population may be to prioritise and provide incentives for the management of obesity. The metabolic and vascular benefits of even modest reductions in weight are well described. Weight loss also enhances fertility in women, improves respiratory function and mental wellbeing, reduces risk of cancers and joint disease, and improves quality of life. Major benefits for individuals from dramatic interventions, like obesity surgery, have been shown. Optimal medical treatment can also produce major weight loss for many patients (outside the constraints of randomised controlled trials). The most striking benefits, however, in proportional terms, are from modest weight loss (5-10%), when fat is particularly lost from intra-abdominal sites. For example, this amount of weight loss increases life expectancy 3-4 years for overweight patients with type 2 diabetes, which is impressive.
Table 4.
Estimated metabolic and vascular benefits of 10% weight loss
| Blood pressure |
| • Fall of about 10 mm Hg in systolic and diastolic blood pressure in hypertensive patients |
| Diabetes |
| • Fall of up to 50% in fasting glucose for newly diagnosed patients |
| People at risk for diabetes, such as those with impaired glucose tolerance |
| • >30% fall in fasting or two hour insulins |
| • >30% increase in insulin sensitivity |
| • 40-60% fall in incidence of diabetes |
| Lipids |
| • Fall of 10% in total cholesterol |
| • Fall of 15% in low density lipoprotein cholesterol |
| • Fall of 30% in triglycerides |
| • Rise of 8% in high density lipoprotein cholesterol |
| Mortality |
| • >20% fall in all cause mortality |
| • >30% fall in deaths related to diabetes |
| • >40% fall in deaths related to obesity |
Obesity management includes priority treatment of risk factors for cardiovascular disease. The benefits of treatment are greater for overweight and obese people because their risks are higher. Primary prevention of obesity and overweight would prevent much secondary disease. Many people do stay at normal weight, but there is no proven effective intervention.
Beyond BMI
The most clinically telling physical sign of serious underlying disease is increased waist circumference, which is linked to insulin resistance, hypertension, dyslipidaemia, a proinflammatory state, type 2 diabetes, and coronary heart disease. More than 250 years ago, Giovanni Battista Morgagni used surgical dissection to show visceral fat. He linked its presence to hypertension, hyperuricaemia, and atherosclerosis. Jean Vague (in the 1940s and '50s) and Per Bjorntorp (in the 1980s) led the interest in gender specific body types of android and gynoid fat distribution. Pear shaped women tend to carry metabolically less active fat on their hips and thighs. Men generally have more central fat distribution, giving them an apple shape when they become obese, although obese women can have a similar shape.
Figure 3.
Stereotypical apple (metabolically harmful, more common in men) and pear (metabolically protective and more common in women) shapes. Making obesity an object of humour has impeded the understanding of its medical consequences. Obesity can contribute to musculoskeletal and psychological problems and have profound effects on quality of life
Cross-sectional studies show that waist to hip ratio is a strong correlate of other diseases. Prospective studies, however, show a large waist as the strongest anthropometric predictor of vascular events and diabetes because it predicts risk independently of BMI, hip circumference, and other risk factors.
Management of obesity in the UK
Clinical practice in the UK focuses on secondary prevention for chronic diseases. Obesity is often neglected in evidence based approaches to managing its consequences. One problem is in recording the diagnosis.
Computerised medical records and better linking of datasets will help monitor efforts to reduce obesity locally and nationally. The UK Counterweight audit showed that height and weight are measured in about 70% of primary care patients only. The diagnosis of obesity is rarely recorded in reports from hospital admissions or outpatient attendance. A survey of secondary prevention of coronary heart disease shows that, despite the importance of obesity as a coronary heart disease risk factor, it is still poorly managed, even in high risk patients. Although patients with type 2 diabetes are often overweight, most are managed in primary care and few regularly see a dietician.
The first revision of the general medical services contract gives practices eight points for creating registers of obese adults, but this is only a start in readiness for a more emphatic second revision of the contract. BMI is seldom measured in people of normal weight so their progression to becoming overweight is missed, and with it the opportunity to prevent more than half of the burden of diabetes in the UK.
Producing a register of obese individuals is futile unless something is done with the list. Weight management and measurement of fasting lipid profile, glucose, and blood pressure should be encouraged. This could be used to identify people at high risk of cardiovascular disease and diabetes through risk factors related to obesity, which individually might fall below treatment thresholds. Without these steps the contract creates more work with no clinical benefit. The arguments are strong for awarding points for assessing obese individuals and offering weight management programmes. The clinical and economic benefit will be extended if effective obesity prevention strategies can be developed. These are not alternative strategies: strategies are needed for both prevention and treatment with ongoing monitoring and evaluation.
Conclusion
Obesity affects almost every aspect of life and medical practice. The rise in obesity and its complications threatens to bankrupt the healthcare system. Early treatment and prevention offer multiple long term health benefits, and they are the only way towards a sustainable health service. Doctors in all medical and surgical specialties can contribute.
The figure showing obesity in English girls and boys aged 6-10 uses data from Health Survey for England 2002 (using criteria of the International Obesity Task Force for overweight and obesity), and is adapted from British Medical Association Board of Science. Preventing childhood obesity, 2005 (www.bma.org). The box showing health consequences of obesity is adapted from International Obesity Taskforce (www.iotf.org/.../slides/IOTF-slides/sld016.htm). The box showing metabolic and vascular benefits of 10% weight loss is adapted from Jung RT. Obesity as a disease. Br Med Bull 1997;53: 307-21.
The ABC of obesity is edited by Naveed Sattar (nsattar@clinmed.gla.ac.uk), professor of metabolic medicine, and Mike Lean, professor of nutrition, University of Glasgow. The series will be published as a book by Blackwell Publishing early in 2007.
Competing interests: DH has received honorariums for presentations and advisory board attendance from Sanofi-Aventis, Abbott, Roche and GlaxoSmithKline. NS has received fees for consulting and speaking from Sanofi-Aventis, GlaxoSmithKline, and Merck, and from several companies in the field of lipid lowering therapy. ML has received personal and departmental funding from most major pharmaceutical companies involved in obesity research, and from several food companies. A full list can be seen on www.food.gov.uk/science/ouradvisors/ACR/
References
- • Haslam D, James WP. Obesity. Lancet 2005;366: 1197-209. [DOI] [PubMed] [Google Scholar]
- • Torgerson JS, Hauptman J, Boldrin MN, Sjostrom L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care 2004;27: 155-61. [DOI] [PubMed] [Google Scholar]
- • James WP, Astrup A, Finer N, Hilsted J, Kopelman P, Rossner S, et al. Effect of sibutramine on weight maintenance after weight loss: a randomized trial. STORM Study Group. Sibutramine Trial of Obesity Reduction and Maintenance. Lancet 2000;356: 2119-25. [DOI] [PubMed] [Google Scholar]
- • McQuigg M, Brown J, Broom J, Laws RA, Reckless JP, Noble PA, et al. Counterweight Project Team. Empowering primary care to tackle the obesity epidemic: the Counterweight Programme. Eur J Clin Nutr 2005;59: 93-100. [DOI] [PubMed] [Google Scholar]
- • De Bacquer D, De Backer G, Cokkinos D, Keil U, Montaye M, Ostor E, et al. Overweight and obesity in patients with established coronary heart disease: are we meeting the challenge? Eur Heart J 2004;25: 121-8. [DOI] [PubMed] [Google Scholar]
- • Scottish Intercollegiate guidelines (www.sign.ac.uk)
- • National Institute of Health guidelines (www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.htm)