Abstract
Purpose
To propose an integration index of home care delivery to older persons, to study its validity and to apply it to home care services of European cities.
Theory
Home care delivery integration was based on two dimensions referring to process-centred integration and organisational structure approach.
Method
Items considered as part of both dimensions according to an expert consensus (face validity) were extracted from a standardised questionnaire used in “Aged in Home care” (AdHoc) study to capture basic characteristics of home care services. Their summation leads to a services' delivery integration index. This index was applied to AdHoc services. A factor analysis was computed in order to empirically test the validity of the theoretical constructs. The plot of the settings was performed.
Results
Application of the index ranks home care services in four groups according to their score. Factor analysis identifies a first factor which opposes working arrangement within service to organisational structure bringing together provisions for social care. A second factor corresponds to basic nursing care and therapies. Internal consistency for those three domains ranges from 0.78 to 0.93. When plotting the different settings different models of service delivery appear.
Conclusion
The proposed index shows that behind a total score several models of care delivery are hidden. Comparison of service delivery integration should take into account this heterogeneity.
Keywords: integrated care, measurement of integration, integration index, older people, Europe, home care
Introduction
Many observers of contemporary long-term care emphasise the disadvantages of fragmented care [1–4]. Despite obvious cross-national differences in the structure of health and social care for vulnerable older persons there is evidence in almost all countries of poorly coordinated services [5]. This poor co-ordination is due particularly to the separation of health and social services, which is common in many countries [6]. Most of existing care systems do not fit well with the complex needs of people with numerous, simultaneous, chronic, disabling conditions.
There are several arguments in favour of integration of care for older persons. Fiscal concerns about an increase of an older population in need of long term care [7] have led to rationalisation of care trajectories by optimising resource use and homogenising practices. The supportive network for vulnerable older persons with complex care needs is frequently insufficient and the housing condition is often not adapted to meet those needs. The vulnerable older persons, therefore, need an elaborate and flexible combination of intervention [8]. Countries have attempted to overcome the fragmentation of services and reach a more coordinated care package [9]. Several countries have undertaken demonstration projects aiming to create comprehensive integration of care for the elderly [10–16]. To-day integration of care for older persons has become a central issue in care reform [17,18].
Because of the centrality of supporting people at home it makes sense to consider the degree of service delivery integration of home care. In most of the major OECD countries, following the promotion of policies of de-institutionalisation and community-based care, the proportion of persons over 65 receiving home care out-weighs the proportion receiving residential care [19]. The newly promoted organisational models of care favour case management within a multidisciplinary team, doing initial geriatric assessment and follow up. Those new models of care are used in most European countries as mainstream services such as in England and the Netherlands or model projects such as in Germany, France and Italy.
The integrated care literature has established that there are several models with different levels of integration for chronically ill and disabled persons, especially for frail older persons [8,20–22], and that that integration is a multidimensional concept with different approaches [5,8,23]. This means, that within this overall framework of integration, there are several independent dimensions.
Since integration is a mean to improve the services in relation to quality of health and social care [24] it may be interesting to refer to the Donabedian [25] framework on quality of care which identifies three approaches: structure, process and outcomes. The two first dimensions are considered as main features of integration in the scientific literature [5,8,23]. Structure focuses on the resources available to care providers and to organisation. The process of care involves the approach taken to care delivery. It may be possible to gather the items of both dimensions in an integration index. The purposes of this study were to build a service delivery integration index based on organisational structure and process-centred features of home care supply, to study its validity and to apply it to Home care services of several European cities.
Methods
Material
We used data from the “the Aged in Home care”(AdHoc) study [26] designed by members of the inter-RAI organisation (www.interrai.org) to compare outcomes of different models of home care for older persons in 11 European countries – the Czech Republic, Denmark, England, Finland, France, Germany, Iceland, Italy, the Netherlands, Norway and Sweden.
In each country, a project co-ordinator selected distinct municipalities providing formal Home Care services that were considered representative of the nation's urban areas. The catchment areas were defined by the targeted population. The target sample size was 400 recipients of home care aged 65 and over. The cities chosen were Amsterdam, Copenhagen, Helsinki, Oslo, Prague, Reykjavik, Stockholm, Amiens (northern France), Ashford and Maidstone (in south-east England), Monza (in Milan's suburb), Nuremberg and Bayreuth (in Bavaria, south Germany). The number of services involved varied from one to twenty-three in the German cities according to services capacity which varied from 20 clients to over a thousand.
A structured questionnaire on services' characteristics (the European-Home Care Service – EU-HCS) was created in common by the persons of the eleven countries in charge of the program. The EU-HCS captured basic structural characteristics and delivery of heterogeneous home care services (eligibility criteria, referral systems, working arrangements within – e.g. standard use of any validated assessment instruments – and, between services, health/social professionals and administrative personnel per patient, total number of patients per year, mean duration of service provision per patient, administrative status, services provided). The information came from the answers on the questionnaire by the person in charge of implementing the project in each country (research or chief nurse).
Detailed client data were collected using the RAI version 2.0 Minimum Data Set for Home Care assessment instrument [27]. These data were not used in the present work.
Conceptual framework
We chose to focus on two dimensions of integration referring to structural organisational approach and process-centred integration. Organisational structure approach to integration involves bringing together staff and resources for different benefits in one single organisation under a single unified hierarchical structure [24]. This allows a single home care agency to provide assistance with different social care (e.g. for instrumental, personal activities of daily living and surveillance), primary health nursing care (e.g. bandaging, catheter management), secondary health care such as therapies. This means at least linkage between provisions which is the first step of integration [17] as opposed to their fragmentation between providers [2]. The process-centred integration focuses on caring activities, collaborative actions or activity undertaken between health and social services organisations and practitioners. This means working arrangements within and between services [24,28] e.g. comprehensive clinical assessment, case manager and hospital discharge management.
Construction of an integration index
All the items considered were extracted from the EU-HCS. To build a services' delivery integration index we included a priori 29 items which have clinical meaning regarding process-centred integration and organisational structure approach. Five items, standardised comprehensive geriatric assessment; multidisciplinary team approach for assessment; team meeting for care planning; participation of general practitioner to team meeting and case manager (the person responsible of organising the care), were considered as working arrangements, facilitating integration within the service. Two items, day and night service provision (24 hours service) and weekend provision were considered as a needed condition for the service in order to provide care continuity which is an aspect of integrated care delivery. One item, hospital discharge management, involved working arrangements facilitating linkage and collaboration between home care and acute hospital. One item was a key characteristic of an integrated organisation: a single entry point [8,24] for referral of potential users at which all their requirements can be assessed and an appropriate provision of services agreed. The 20 other items represented the extent of provisions delivered to older disabled clients by social and health care. The provisions chosen were considered as essential for meeting the complex needs of disabled older persons living at home. Social care included assistance for five instrumental activities of daily living (IADL: cooking, shopping, cleaning, laundry, meals on wheels), assistance for three activities of daily living (ADL: feeding, bathing, dressing) and, two surveillance items (supervision, tele-help). Health care included three basic nursing care (bandaging, decubitus care, catheter management) and three usual technical nursing care (intra venous medication, nutritional therapy, suctioning). The last area included four therapies (occupational, speech, psycho-social and, physiotherapy).
Table 1 shows the list of items used to rate care delivery integration.
Table 1.
Rotated factor matrix of each item used to rate integration
| Item | Factors |
|
|---|---|---|
| 1 | 2 | |
| Comprehensive Geriatric Assessment | −0.678 | |
| Team meeting | −0.658 | |
| General Practitioner participating to Team Meeting | −0.704 | |
| Multidisciplinary Team Approach | −0.730 | |
| Case Manager | −0.513 | 0.461 |
| Night and day | 0.609 | 0.659 |
| Week-end | 0.841 | |
| Hospital discharge | 0.441 | |
| Single entry point | ||
| Cooking | 0.880 | |
| Shopping | 0.887 | |
| Cleaning | 0.906 | |
| Laundry | 0.907 | |
| Meals on Wheels | 0.647 | |
| Feeding | 0.692 | |
| Toileting | 0.696 | |
| Dressing | 0.697 | |
| Surveillance | 0.756 | |
| Tele-help | ||
| Bandaging | 0.921 | |
| Decubitus care | 0.906 | |
| Catheter management | 0.872 | |
| Intra-venous therapy | ||
| Nutrition | ||
| Suctioning | ||
| Occupational therapy | 0.573 | |
| Speech therapy | 0.435 | |
| Psychosocial therapy | 0.550 | |
| Physiotherapy | 0.521 | |
Scoring the integration measure
Each of the 29 items was assigned a score of “1” when present. No information on an item was given a “0” score. When there were several services in a catchment area the average of the scores was retained. The summation of individual scores gave a total score range from 0 to 29.
This index was applied to AdHoc home care services in order to compare their level of care delivery integration. We divided the scores obtained into quartiles.
Validation assessment
We assessed the validation of the scale starting with face validity regarding the items chosen. It was based on expert consensus. The experts were the eleven project co-ordinators in charge of AdHoc study, all being involved in care for older persons.
A principal component analysis (PCA) with Varimax rotation on the total items was performed in order to empirically test the validity of the theoretical constructs. The PCA was to be considered as successful in validating the hypothesis theoretical model if there were a clear clinical interpretation consistent with expectation for each identified latent factor. Analysis began assessing the number of underlying dimensions. Cronbach's alpha was used to measure the internal consistency of each domain found: alpha ≥ 0.6 is considered as evidence of an acceptable internal consistency for the considered instrument [29].
Results
Service delivery integration scores for each setting
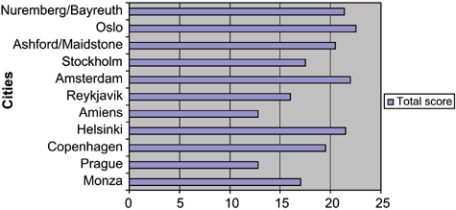
The total score of service delivery integration varied from 12.8 up to 22.5. Figure 1 shows the total integration scores for each setting. The Prague and Amiens areas ranged in the fourth quartile (below 15.2). The Oslo, Amsterdam Helsinki, Nuremberg/Bayreuth and Ashford/Maidstone settings ranked in the first quartile (score above 20), Copenhagen in the second (score between 17.7 and 20) and Stockholm, Monza and Reykjavik scored in the third (score between 15.2 and 17.7).
Figure 1.
Total score of service delivery integration (maximum 29).
Validation assessment
The experts' consensus supported the face validity of the index items.
The PCA applied to the total of items shows two factors accounting for 51% of total variance. The first factor accounting for 32% of variance opposes working arrangements facilitating integration within the service to organisational structure bringing together provisions for social care and hospital discharge. The second factor (20% of the variance) includes mostly items related to health care, week-end and 24 hours provision. The rotated factor matrix shown in Table 1 describes how each item loads on the underlying dimension. Five items did not meet the minimum 0.40 criterion for belonging to any expected domain: single entry point, tele-help and the 3 items of usual technical nursing care: intravenous therapy, nutrition and suctioning. Two items, case manager, day and night service provision, were multidimensional being associated with factor 1 as well as factor 2.
The Cronbach's alpha coefficient was 0.78, 0.93, respectively, for five items of working arrangement within the service (process centred integration) and 11 items of social care domain of factor 1. The Cronbach's alpha coefficient was 0.80 for the 10 items of factor 2. This was computed after deletion of variables not meeting the minimum criterion for belonging to any domain (Table 1).
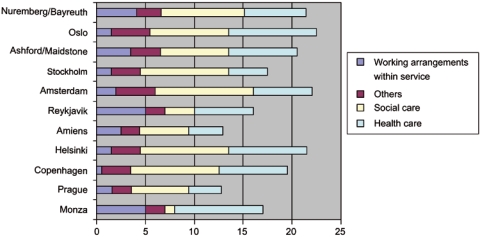
Figure 2 shows the scores of the different domains contributing to service delivery integration: working arrangement within the service, social care, health care and others (corresponding to various working arrangements), respectively.
Figure 2.
Scores of different domains contributing to service delivery integration.
Monza, and Reykjavik have the highest score for process-centred integration. They are the only settings with all working arrangements within the service. Nuremberg/Bayreuth (score 4.1) is also ranking in the upper quartile. Ashford/Maidstone (score 3.5) has not a general practitioner (GP) participating to team meeting and not always a case manager such as Amiens. Amsterdam (score 2) has no case manager, no multidisciplinary team approach and no participation of GP. Oslo, Helsinki, Copenhagen, Stockholm and Prague rank in the lowest quartile having less than two items of working arrangements within the service.
Regarding social care Amsterdam, Copenhagen, Helsinki, Oslo, Stockholm and Nuremberg/Bayreuth rank in the first quartile their home care services are providing all or most kinds of provisions. Ashford/Maidstone, Prague, Amiens do not supply all types of care. Reykjavik and Monza rank in the fourth quartile delivering very few social provisions.
Regarding health care Monza, Oslo and Helsinki supply most of the provisions. Copenhagen, Ashford/Maidstone and Nuremberg/Bayreuth (score between 6.2 and 7.6) rank in the second quartile because of a lack of supply of few therapies and usual technical nursing care. Amsterdam and Reykjavik rank in the third quartile (4.8–6.2). In the former, therapies are not delivered whereas in the latter, the same applies for usual technical nursing care and some therapies. Prague and Amiens and Stockholm rank in the fourth quartile providing very few therapies and nursing care.
The results of the combination of the different domains of service delivery integration are seen in Figure 3 which represents the plot of settings. Three models appear. The first corresponds to extensive social care with very little process-centred integration Oslo, Stockholm, Helsinki, Copenhagen and Amsterdam are representative of this model. Health care is more (Oslo) or less (Amsterdam) associated. The second model includes working arrangement within the service with predominance of health care and few or no social care delivery. Monza is typical of this model. Reykjavik is close to it and Ashford/Maidstone is less typical.
Figure 3.
Plot of settings.
Nuremberg/Bayreuth is a mix of those two models having working arrangement within services together with social care. The third type is represented by two settings Amiens and Prague having few provisions and few or no working arrangement of integration.
Discussion
Integration represents a “set of methods and models of the funding, administrative, organisational, service delivery and clinical levels to create connectivity, alignment and collaboration within and between the care and the cure sectors” [30].
This paper has offered both a rationale and model of assessment of process-centred and organisational structure components of services delivery integration of home care. By concentrating on those aspects it focuses on working arrangements that have been major strategies at organisational levels to reduce services fragmentation.
The validation of the total service delivery integration index could not be based on a comparison with a gold standard that does not exist. Results of the PCA do not support the simple distinction between two dimensions of service delivery integration referring to process-centred integration and structural organisational approach. No setting had together all the items of both dimensions. We found a first factor which opposes those having a large extent of social care delivered by a single service with few or no items of working arrangements within the service to those having on the contrary all or most of the items of working arrangements but offering few or no social provisions. An internal consistency was found for the items of both domains. Three items of working arrangements, comprehensive geriatric assessment, multidisciplinary team approach and team meeting whereas linked together were not always present altogether depending how care were organised. In Amsterdam, the comprehensive geriatric assessment was made by one nurse only without a multidisciplinary team approach. She met afterwards with the other carers. In Oslo, there was no standardised comprehensive geriatric assessment but a multidisciplinary team approach for assessment. The participation of GP to team meeting is an important issue for care delivery integration and was present in only three settings. A case manager was present in half of the settings and its functions were not homogeneous.
Items of health care including basic nursing care and therapies constitute a second factor. Technical nursing care does not meet the minimum 0.40 criterion for belonging to this dimension. Therefore, our model supports the existence, in most settings, of barrier between health and social care, which in home care is manifested in separation of nursing care from assistance for ADL and IADL. Technical nursing care however are not components of health care as important as basic nursing care and therapies.
Three items, hospital discharge management, 24 hours (day and night) and week-end provisions depend on inter-organisational working [31]. The first (and to a certain extent 24 hours provision) was associated with social care. The second and third items were found with health care. Those findings are consistent with clinical interpretation. Social care is a major issue for hospital discharge and some may be necessary at night. Basic nursing care needs implementation during week-end and eventually day and night. Single entry point, whereas considered as a key characteristic of an integrated organisation, was not belonging to any dimension. It was present in two cities only (Amsterdam and Oslo).
The paper illustrates application of the model to home care services of several European city areas. The index allows, by capturing basic characteristics of heterogeneous home care services, to compare the degree of integration of their delivery. Integration scores have the advantage of being easy to use. But it has some practical disadvantages of communication as it exposes to value judgment according to integration level.
The total score masks some differences that are better seen when examining the combination of different domains (e.g. Monza and Stockholm Figure 2). It appears that there are various models of service delivery integration due to various combinations of domains. A first model reflects a large extent of social provisions given by a unique service with working arrangements facilitating care continuity (e.g. hospital discharge) and eventually single entry point. The four Nordic cities and Amsterdam management are typical of this model where assistance for ADL is part of social care and basic nursing care is supplied. It is mainly a medico-social model of answer to disability of older people but the extent of health provisions varies especially regarding therapies. Oslo and Helsinki to a lesser extent providing therapies are the only settings without a barrier between health and social care whereas Amsterdam and Stockholm are not delivering therapies. A second model includes working arrangement within the service but mainly for providing basic nursing and technical nursing care and therapies. Monza is typical of it. The core of social provisions for disabled people is not supplied. It corresponds to a medical model of answer to disability of older persons. Reykjavik corresponds to the same type of model but with more social care and less therapies. Ashford/Maidstone is rather of this type but with less components of working arrangements within services and with more social care. A third model is characterised by the separation of supply for ADL and for domestic tasks (IADL). Assistance for ADL is part of nursing care. This is the case for Prague and Amiens. It corresponds to a fragmented model with several small home nursing care and home help services. Nuremberg/Bayreuth is a mix of the models. There are variations in working arrangements and of extent of provisions between the 23 German home care services of this study.
One of the goals of the AdHoc study was to compare outcomes of different models of home care. The proposed service delivery integration index of Home care included organisational structure and process-centred patterns that are two components of the framework to analyse quality of care [25]. Then this index may be a way for evaluation of the two first components (structure and process) of quality of care.
The service delivery integration of Home care may be influenced by a whole array of local factors, not considered in this work. The problems of integration of the communication and information were not considered. It was neither our matter to look at the interactions between organisational nor behavioural aspects of care integration which are crucial to study [32]. We did not explore behavioural aspects of both professionals and service users at the clinical level. At this level staff and patients may bridge some gaps inherent in any system, however well supposedly integrated [33]. Moreover, our quantitative approach to evaluating service delivery integration is not identifying the clients' experience of receiving care, and, therefore, is at risk of missing its key features [24]. All those aspects require other methods of approach of integration. It may also be influenced by more general factors such as structural arrangement of responsibility for funding organising and providing care for older persons, which are part of an integrated system of care [5,34]. Therefore, we will look in the future at possible relationships between levels of service delivery integration and structural arrangements, at more macro level.
In conclusion, the proposed service delivery integration index appears to be valid to assess structural and procedural aspects of home care delivery. Including components of quality of care it may be a first step for its evaluation. It allows, also, by using basic characteristics of heterogeneous home care services to compare the degree of service delivery integration and to identify different types of care delivery. Comparison of integration should however take into account this heterogeneity. Further research will show whether the sites with a higher service delivery integration score provide better outcomes of care compared to those with lower scores. This may be achieved when the analysis of the one year follow-up of the 4000 clients of home care will be completed, by crossing the outcomes with the service delivery integration scores.
Acknowledgments
The AdHoc Project was funded by the European Commission under the Vth Framework Programme grant QLK6-2000-00002. The authors wish to express their gratitude to inter-RAI and the full AdHoc research team and to Béatrice Beaufils for her advice for statistical analysis.
Contributor Information
Jean-Claude Henrard, Professor of Public Health and former Director Health and Ageing research unit Versailles-Saint-Quentin-en-Yvelines University, Centre of Gerontology, Sainte Périne Hospital, Paris, France.
Joël Ankri, Health and Ageing research unit Versailles-Saint-Quentin-en-Yvelines University, Centre of Gerontology, Sainte Périne Hospital, Paris, and INSERM U687, Saint-Maurice, France.
Dinnus Frijters, Utrecht, the Netherlands and EMGO, Free University Medical Centre, Amsterdam, The Netherlands.
Iain Carpenter, Centre for Health Services Studies, University of Kent, Canterbury, United Kingdom.
Eva Topinkova, Professor in Medicine/Geriatrics Department Geriatrics, 1st Faculty of Medicine, Charles University and Institute of Postgraduate Medical Education, Prague, Czech Republic.
Vjenka Garms-Homolova, Alice Salomon University of Applied Sciences, Institute for Health Analysis and Social Concepts, Berlin, Germany.
Harriett Finne-Soveri, National Research and Development Centre for Welfare and Health (Stakes)/CHESS, Helsinki, Finland.
Liv Wergeland Sørbye, The Diakonhjemmet University College, Oslo, Norway.
Palmi V. Jónsson, Department of Geriatrics, Landspitali University Hospital, University of Iceland, Reykjavik, Iceland.
Gunnar Ljunggren, Centre for Gerontology and Health Economics, Karolinska Institute and Stockholm County Council, Stockholm, Sweden.
Dr Marianne Schroll, Bispebjerg Hospital, Copenhagen University, Denmark.
Cordula Wagner, (Dutch Institute for Primary Care Research), Utrecht, The Netherlands.
Roberto Bernabei, Department of Geriatrics, Catholic University, Rome, Italy.
Reviewers
Berrie Middel, Dr, University of Groningen, Department of Health Sciences Groningen, The Netherlands
Jill Manthorpe, Professor of Social Work, Co-Director of the Social Care Workforce Research Unit, King's College London, United Kingdom
Richard Pieper, PhD, Professor of Sociology, Urban Studies and Social Planning, University of Bamberg, Germany
References
- 1.Weissert WG. The national channeling demonstration: what we knew, know now, and still need to know. Health Services Research. 1988 Apr;23(1):175–87. [PMC free article] [PubMed] [Google Scholar]
- 2.Henrard J-C, Cassou B, Le Disert D. The effects of system characteristics on policy implementation and functioning of care for the elderly in France. International Journal of Health Services. 1990;20(1):125–39. doi: 10.2190/FE58-K9NC-8C43-5E75. [DOI] [PubMed] [Google Scholar]
- 3.Jamieson A. Trends in Home-care policies. In: Jamieson A, editor. Home care for older people in Europe. Oxford: Oxford University Press; 1991. pp. 99–117. [Google Scholar]
- 4.Bergman H, Beland F, Lebel P, Contandriopoulos AP, Tousignant P, Brunelle Y. Care for Canada's frail elderly population: fragmentation or integration? Canadian Medical Association Journal. 1997 Oct 15;157(8):1116–21. [PMC free article] [PubMed] [Google Scholar]
- 5.Kodner DL. In pursuit of evidence based integrated care [editorial] International Journal of Integrated Care [serial online] 2000 Jan 11;1 doi: 10.5334/ijic.5. Available from: URL: http://www.ijic/org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jamieson A. Issues in home care services. In: Caring for frail elderly people: policies in evolution. Paris: Organisation for Economic Co-operation and Development (OECD); 1996. pp. 67–79. (OECD Social policy studies; no. 19) [Google Scholar]
- 7.Meerding W, Polder J, Bonneux L, Koopmanschap M, Van der Maas P. Health-care costs of ageing. Lancet. 1998 Jan 10;351(9096):140–1. doi: 10.1016/s0140-6736(05)78119-8. [DOI] [PubMed] [Google Scholar]
- 8.Johri M, Beland F, Bergman H. International experiments in integrated care for the elderly: a synthesis of the evidence. International Journal of Geriatic Psychiatry. 2003 Mar;18(3):222–35. doi: 10.1002/gps.819. [DOI] [PubMed] [Google Scholar]
- 9.Organisation for Economic Co-operation and Development (OECD) Caring for frail elderly people: policies in evolution. Paris: OECD; 1996. (OECD Social Policy Studies; no. 19) [Google Scholar]
- 10.Challis D, Darton R, Johnson L. Clients and the outcome of care. In: Challis D, Darton R, Johnson L, Stone M, Traske K, editors. Care management and health care of older people: the Darlington Community Care Project. Aldershot: Ashgate Publishing Limited; 1995. pp. 181–4. [Google Scholar]
- 11.Eng C, Pedulla J, Eleazer GP, McCann R, Fox N. Program of All-inclusive Care for the Elderly (PACE): an innovative model of integrated geriatric care and financing. Journal of the American Geriatric Society. 1997 Feb;45(2):223–32. doi: 10.1111/j.1532-5415.1997.tb04513.x. [DOI] [PubMed] [Google Scholar]
- 12.Manton KG, Newcomer R, Lowrimore GR, Vertrees JC, Harrington C. Social/health maintenance organisation and fee-for-service health outcomes over time. Health Care Financing Review. 1993 Winter;15(2):173–202. [PMC free article] [PubMed] [Google Scholar]
- 13.Newcomer R, Harrington C, Manton KG, Lynch MA. A response to representatives from the social HMOs regarding program evaluation. The Gerontologist. 1995 Jun;35(3):292–3. doi: 10.1093/geront/35.3.292. [DOI] [PubMed] [Google Scholar]
- 14.Landi F, Lattanzio F, Gambassi G, Zuccala G, Sgadari A, Panfilo, et al. A model for integrated home care of frail older patients: the Silver Network project. SILVERNET-HC Study Group. Aging Clinical and Experimental Research. 1999 Aug;11(4):262–72. doi: 10.1007/BF03339667. [DOI] [PubMed] [Google Scholar]
- 15.Bernabei R, Landi F, Gambassi G, Sgadari A, Zuccala G, Mor V, et al. Randomised trial of impact of model of integrated care and case management for older people living in the community. British Medical Journal. 1998 May 2;316(7141):1348–51. doi: 10.1136/bmj.316.7141.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bergman H, Beland F, Perrault A. The global challenge of understanding and meeting the needs of the frail older population. Aging Clinical and Experimental Research. 2002 Aug;14(4):223–5. doi: 10.1007/BF03324442. [DOI] [PubMed] [Google Scholar]
- 17.Leutz WN. Five laws for integrating medical and social services: lessons from the United States and the United Kingdom. Milbank Quarterly. 1999;77(1):77–110. doi: 10.1111/1468-0009.00125. iv–v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kodner DL. The quest for integrated systems of care for frail older persons. Aging Clinical and Experimental Research. 2002 Aug;14(4):307–13. doi: 10.1007/BF03324455. [DOI] [PubMed] [Google Scholar]
- 19.Anderson GF, Hussey PS. Population aging: a comparison among industrialised countries. Health Affairs (Millwood) 2000 May-Jun;19(30):191–203. doi: 10.1377/hlthaff.19.3.191. [DOI] [PubMed] [Google Scholar]
- 20.Hardy B, Mur-Veeman I, Steenbergen M, Wistow G. Inter-agency services in England and The Netherlands: a comparative study of integrated care development and delivery. Health Policy. 1999 Aug;48(2):87–105. doi: 10.1016/s0168-8510(99)00037-8. [DOI] [PubMed] [Google Scholar]
- 21.Frossard M. Coordination, intégration, réseaux et évaluation socio-économiques. In: Henrard J-C, Firbank O, Clément S, Frossard M, Lavoie JP, Vézina A, editors. Personnes âgées dépendantes en France et au Québec. Paris: INSERM; 2001. pp. 283–302. [Google Scholar]
- 22.Glendinning C. Breaking down barriers: integration health and care services for older people in England. Health Policy. 2003 Aug;65(3):139–51. doi: 10.1016/s0168-8510(02)00205-1. [DOI] [PubMed] [Google Scholar]
- 23.Gröne O, Garcia-Barbero M. Integrated care. A position paper of the WHO European office for integrated health care services. International Journal of Integrated Care [serial online] 2001 Jun 1;1 Available from: URL: http://www.ijic.org/ [PMC free article] [PubMed] [Google Scholar]
- 24.Alaszewski A, Billings J, Coxon K. Integrated health and social care for older persons: theoretical and conceptual issues. In: Leichsenring K, Alaszewski AM, editors. Providing integrated health and social care for older persons: a European overview of issues at stake. Aldershot: Ashgate Publishing Limited; 2004. pp. 53–94. [Google Scholar]
- 25.Donabedian A. Evaluating the quality of medical care. 1966. Milbank Quarterly. 2005;83(4):691–729. doi: 10.1111/j.1468-0009.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carpenter GI, Gambassi G, Topinkova E, Schroll M, Finne-Soveri H, Henrard J-C, et al. Community care in Europe: The Aged in Home Care project (AdHOC) Aging Clinical and Experimental Research. 2004 Aug;16(4):259–69. doi: 10.1007/BF03324550. [DOI] [PubMed] [Google Scholar]
- 27.Morris JN, Fries BE, Steel K, Ikegami N, Bernabei R, Carpenter GI, et al. Comprehensive clinical assessment in community setting: applicability of the MDS-HC. Journal of the American Geriatric Society. 1997 Aug;45(8):1017–24. doi: 10.1111/j.1532-5415.1997.tb02975.x. [DOI] [PubMed] [Google Scholar]
- 28.Boult C, Kane RL, Brown R. Managed care of chronically ill older people the US experience. British Medical Journal. 2000 Oct 21;321(7267):1011–4. doi: 10.1136/bmj.321.7267.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. [Google Scholar]
- 30.Kodner D, Spreeuwenberg C. Integrated care: meaning, logic, application and, implications – a discussion paper. International Journal of Integrated Care [serial online] 2002 Nov 14;2 doi: 10.5334/ijic.67. Available from: URL: http://www.ijic.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hudson B. Interprofessionality in health and social care: the Achilles' heel of partnership? Journal of Interprofessional Care. 2002 Feb;16(1):7–17. doi: 10.1080/13561820220104122. [DOI] [PubMed] [Google Scholar]
- 32.Browne G, Roberts J, Gafni A, Byrne C, Kertyzia J, Loney P. Conceptualising and validating the Human Services Integration Measure. International Journal of Integrated Care [serial online] 2004 May 19;4 doi: 10.5334/ijic.98. Available from: URL: http://www.ijic.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cook RI, Render M, Woods DD. Gaps in the continuity of care and progress on patient safety. British Medical Journal. 2000 Mar 18;320(7237):791–4. doi: 10.1136/bmj.320.7237.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Illsley R, Jamieson A. Contextual and structural influences on adapting to changes. In: Jamieson A, Illsley A, editors. Contrasting European policies for the care of older people. Aldershot, England: Svebury Gower Publishing Co.; 1990. pp. 83–94. [Google Scholar]