Abstract
In an attempt to transduce monocyte-derived dendritic cells (DCs) with a retroviral vector coding for an intracytoplasmic tumor antigen (TAA), we were confronted by the evident dissociation between the ability of the treated DCs to induce a TAA-specific response, and the presence of integrated vector proviral DNA. The TAA, i.e., MAGE-3, was acquired by DCs and presented to immune effectors, thanks to the property of DCs to uptake the apoptotic bodies released by the irradiated vector-producing cells. Indeed, we observed that upon irradiation vector-producing cells underwent apoptotic cell death, monitored by annexin V and propidium iodide staining, and were phagocytosed by DCs. Lymphocytes obtained from a patient affected by a MAGE-3+ melanoma, were stimulated in vitro with autologous DCs previously exposed to irradiated MAGE-3-expressing cells. This procedure led to the induction of MAGE-3-specific cytotoxic effectors, directed against a yet unknown MAGE-3 epitope presented by HLA-A*B5201 molecules. These data demonstrate that DCs can present engulfed human TAAs, thus providing strategies for cancer vaccination.
During the last few years, in vitro analysis of the immunogenic properties of human tumors has allowed the identification and molecular characterization of a wide array of different tumor antigens (TAAs) that are specifically recognized by autologous CD8 and CD4 T cell clones (1).
Despite the presence of TAAs on the tumor cell surface, in vivo presentation of TAAs by professional antigen (Ag)-presenting cells (APCs) is critical for the generation of an effective immune response (2). Among APCs, dendritic cells (DCs) have been shown to be central players of the immune system. They capture and process Ags in peripheral tissues and migrate to lymphoid organs (3, 4), where they activate Ag-specific T cells. Due to these properties, DCs are considered promising tools for cancer immunotherapy. Several approaches for TAAs presentation by DCs' class I molecules have been pursued in the last years. DCs pulsed with class I-restricted synthetic peptides (5) and proteins (6), or with natural peptides eluted from the tumor (7), have been shown to induce an effective and long-lasting antitumor immunity in various murine tumor models (8, 9). The relevance of these animal experiments to the treatment of human cancer has recently been confirmed (5, 10, 11). Alternative strategies to deliver the antigenic epitope into the class I pathway of DCs have been exploited, including viral vectors, naked and plasmid DNA, and RNA and liposomes with nucleic acid (4). DCs engineered for constitutive expression of a given Ag could provide important advantages over Ag-pulsed DCs in terms of stable expression of the target gene product and the possibility of transducing entire TAA gene(s), thus allowing the presentation of yet unknown epitopes. An approach based on the use of apoptotic bodies has recently been proposed. Emerging evidence suggests that “apoptotic cell death” of the TAA-expressing cells is a crucial point to yield Ags that can access the MHC class I pathway of the host APCs (12–14). Based on these observations, DCs previously exposed to apoptotic tumor cells (15, 16) or purified from a tumor lesion (14), were used to immunize mice and rats. In all the tumor models, these DCs were able to prime tumor-specific cytotoxic T lymphocytes (CTLs) and confer long-term protection from parental tumor challenge.
Here, we demonstrate that the above-described pathway of Ag presentation can occur in a human tumor system. Upon phagocytosis and processing of apoptotic Ag-expressing cells, DCs are able to elicit a tumor-specific T cell response against the human TAA MAGE-3. Our experimental system mimics the natural process of DCs maturation, thus allowing efficient up-take and presentation of apoptotic bodies and induction of an effective immune response against both strong viral and weak TAAs. This strategy was utilized to detect the antitumor response of a melanoma patient ex vivo. The study led to the identification of an epitope encoded by a known TAA, indicating the relevance of methods that allow transfer and presentation of entire TAA proteins over the conventionally utilized small peptides. These findings may provide cancer vaccination strategies based on the full exploitation of the TAAs' antigenic potential.
Materials and Methods
Cell Lines.
The melanoma cell line MSR3-B52 was derived by stable transfection of the original MSR3-mel tumor line with HLA-B*5201 cDNA (17). The retroviral vector-producing cell lines SFCMM2 and M3-CSM, coding for the cell surface marker ΔLNGFr and for the HSV-Tk/neo (TN) fusion protein or the MAGE-3 TAA, respectively, have been previously described (18, 19). The 3T3-TN/ΔLNGFR line was derived by transduction of NIH/3T3 cells with the SFCMM2 vector. All the cell lines were cultured in RPMI 1640 supplemented with 2 mM l-glutamine, antibiotics, and 10% FCS.
Generation and Retroviral “Vector-Mediated Transduction” of Monocyte-Derived DCs.
Peripheral blood mononuclear cells (5–6 × 107) were allowed to adhere to plastic for 1 h at 37°C. The adherent cells were then cultured in RPMI 1640/10% FCS supplemented with 10 ng/ml lipopolysaccharide, 800 units/ml granulocyte–macrophage colony-stimulating factor (Schering-Plough), 100 units/ml IL-4 (a gift from P. Coulie, Ludwig Institute for Cancer Research, Brussels, Belgium), 2 mM l-glutamine, 50 mM 2-mercaptoethanol. At day 2 of culture, differentiating DCs were transduced by cocultivation with a monolayer of irradiated (100 Gy) vector-producing cells in the presence of polybrene (4 μg/ml). After 72 h, DCs were harvested and seeded in fresh medium. Forty-eight hours later, DCs were analyzed for ΔLNGFr expression by flow cytometry with the mAb 20.4 (American Type Culture Collection) and used as stimulators. The transduction procedures did not alter the immunophenotype or the stimulatory capacity of DCs (data not shown).
Stimulation of Peripheral Blood Lymphocytes (PBLs) and Tumor-Infiltrating Lymphocytes by Transgene-Loaded Autologous DCs.
PBLs (2 × 106) from a TN-immune patient (18) were stimulated in vitro with autologous irradiated (50 Gy) DCs (5 × 105) previously cocultured with irradiated SFCMM2 cells. Lytic activity of the effectors was tested after one round of stimulation. In particular, T-blast-induced and DC-induced effectors were tested respectively at days 8 and 12 after stimulation. Lymphocytes (2 × 106) obtained from a lesion of the MSR3 melanoma patient (HLA-A1, A*1101; B*3701, B*5201; Cw6) were mixed with irradiated DCs (2 × 105) previously cocultured with irradiated M3-CSM vector-producing cells. Cultures were restimulated after 10 days in the same condition; while the third stimulation was performed by using irradiated autologous T-blasts (2 × 106) transduced with the same vector. Three days after the first stimulation, a final concentration of 10 units/ml of IL-2 (Chiron) was added to each culture. Lytic activity of the effectors was tested 8 days after the last restimulation in a 4-h chromium release assay against appropriate target cells.
Induction and Detection of Apoptosis.
M3-CSM vector-producing cells were irradiated at 100 Gy by using an x-ray source. Apoptotic cell death was assayed by using annexin V-FITC and propidium iodide, according to the manufacturer's instructions. Negative controls were performed on nonirradiated vector-producing cells.
Phagocytosis of Apoptotic Cells.
M3-CSM vector-producing cells were labeled with the PHK-26 red fluorescent dye, irradiated, and added to a 2-day culture of DCs. Uptake of apoptotic cells by DCs was tested by flow cytometry and confocal microscopy analyses of the DCs population after 24 and 48 h.
Confocal Microscopy Analysis.
DCs were allowed to adhere on glass slides coated with poly-l-lysine and fixed in cold Et-OH for 1 min. DCs were then incubated with FITC-labeled HLA-DR mAb. The analysis was performed with a confocal laser scanning microscope system (MRC-1024; Bio-Rad) attached to a microscope (Axioplan; Zeiss) equipped with a krypton/argon laser.
Cloning of HLA Class I Alleles.
Total RNA was prepared from MSR3 PBLs by the RNeasy Total RNA Kit (Qiagen, Hilden, Germany). cDNA obtained from MSR3 PBLs total RNA was amplified by PCR using primer pairs suitable for specific amplification and directional cloning of HLA-A, -B, and -C full-length coding regions (gift of Soo Young Yang, Memorial Sloan-Kettering Cancer Center, New York). The 1.1-kb PCR products were subcloned into the eukaryotic expression vector pcDNA3.1 (Invitrogen) and sequenced to verify the correspondence to the published DNA sequence.
Production of Subfragments of MAGE-3.
Subfragments of MAGE-3 gene (979-, 629-, and 327-bp fragments) were obtained by double digestions of MAGE-3 cDNA with BglII and EcoRI, HindIII, or BanI, respectively. The fragments were cloned into the pcDNA3.1 and transfected into Cos-7 cells along with the HLA-B*5201 gene.
Transfection of Cos-7 Cells and Tumor Necrosis Factor (TNF) Release Assay.
Transient transfection was performed by the DEAE-dextran-chloroquine method (20). Briefly, 1.5 × 104 Cos-7 cells were transfected with 100 ng of plasmid containing the relevant cDNA. After 24 h, transfected Cos-7 cells were tested in a TNF release assay as previously described (21).
Results and Discussion
Engineered DCs Are Able to Induce a Transgene-Specific T Cell Response.
The rationale of the experiments described in this section was to test the efficiency of retroviral vectors in transducing monocyte-derived human DCs (22, 23) and to assess their ability in inducing a specific immune response against the product of the transgenes. This was investigated by the use of two different Ags. The first is the highly immunogenic fusion protein (TN) containing the herpes simplex virus thymidine kinase (HSV-Tk) and the neomycin phosphotransferase (18). This Ag was used to provide the proof-of-principle for the feasibility of this approach. The second system utilizes as target the well-known TAA MAGE-3 (1). Two vector-producing cell lines were independently established for transfer and expression of each of the two Ags in human DCs. In addition to the cDNA of the relevant Ags, the two vectors encode for a truncated form of the low affinity human nerve growth factor receptor (ΔLNGFr) as cell surface marker (18, 19, 24). Transduction was attempted by cocultivation of DCs on a monolayer of irradiated vector-producing cells. After the transduction procedure, DCs were analyzed for the expression of the cell surface marker, as measure of gene transfer efficiency, and used as stimulators to induce a transgene-specific immune response.
Acquisition by DCs of the vector-encoded cytoplasmic Ag (i.e., TN) was measured by the ability of manipulated DCs to stimulate a specific immune response. To maximize the chance of identifying a biologically relevant response, we utilized as responder cells, lymphocytes obtained from a patient previously exposed to the TN gene product during a gene therapy trial (18). In vitro stimulation was performed with autologous DCs treated to express the TN fusion protein. Upon cocultivation with irradiated vector-producing cells, DCs induced a strong HLA class I-restricted (data not shown) immune response against the TN transgene product (Fig. 1A).
Figure 1.
DCs exposed to irradiated vector-producing cells induce CTLs specific for the vector-encoded transgene product. (A) PBLs (106) from a TN-immune patient were stimulated in vitro by 5 × 105 autologous DCs untreated (○) or cocultured with irradiated vector-producing SFCMM2 cells (●). As positive control, PBLs were stimulated with 106 autologous activated T-blasts expressing high level of the TN gene, the natural target of the immune response (■). (B) PBLs (106) from a TN-immune patient were stimulated in vitro by 5 × 105 autologous DCs cocultured with irradiated 3T3TN/ΔLNGFr cells, expressing the TN gene, but unable to produce any vector particle (▴), with irradiated vector-producing SFCMM2 cells (●), or exposed (three cycles) to their cell-free culture media containing SFCMM2-encoding retroviral particles (□). On day 12, CTL activity was tested against autologous T-blasts expressing the TN gene, in a standard chromium release assay at the indicated effector-to-target cell (E:T) ratios.
Acquisition by DCs of Intracytoplasmic Ags Is Dependent on Apoptotic Cell Death of the Vector-Producing Cells.
Together, these data demonstrate that DCs cocultured with irradiated vector-producing cells were able to induce a transgene-specific, class I-restricted immune response. However, despite this observation, we were unable to detect the presence of integrated vector DNA coding for the cell-surface and the intracytoplasmic Ags in the manipulated population of DCs by Southern blot analysis (data not shown).
To study the possible role of the retroviral vector machinery in the acquisition of the intracytoplasmic Ag by DCs, experiments were performed in which DCs were cocultured with an irradiated cell line expressing the TN gene but unable to produce vector particles. DCs cocultured with the irradiated TN-expressing cells in the absence of retroviral particles induced a TN-specific response identical to that produced by DCs cocultured with vector-producing cells (Fig. 1B). These results demonstrate that the vector-encoded cytoplasmic Ags gained access to the HLA class I pathway of DCs by a retrovirus-independent mechanism. Moreover, because DCs exposed to culture media of vector-producing cells were not able to induce any detectable immune response (Fig. 1B), the response induced by TN-expressing cells was not the result of the presence of soluble Ags.
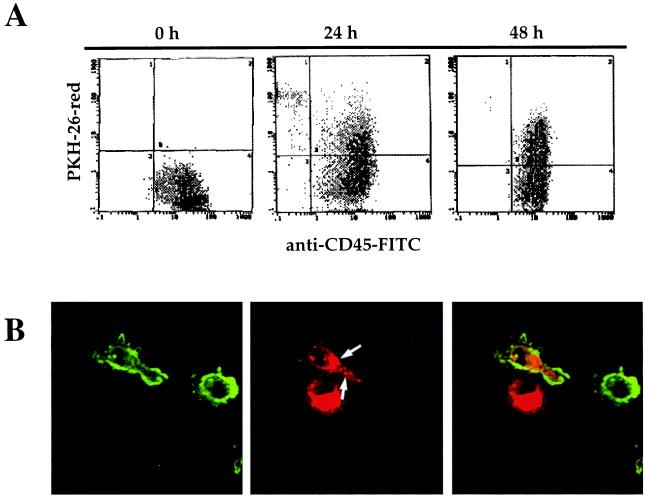
The biological basis for such vector-independent transfer of the Ags to DCs was suggested by the observation that in all our experiments DCs were cocultured with vector-producing cells that were previously irradiated to block their proliferation in culture. It is well known that irradiation may drive cells to apoptosis by mechanisms involving proapoptotic molecules (25). Apoptotic cell death of vector-producing cells was documented by staining with annexin V, an early marker of apoptosis, that was detected on the cell surface of the vector-producing cells 24 h after irradiation (Fig. 2A). Moreover, compaction of nuclear chromatin was highlighted by propidium iodide staining that could also reveal condensed chromatin within the protuberances present on the surface of irradiated cells (Fig. 2B, arrow). To monitor phagocytosis of apoptotic bodies by DCs, vector-producing cells were stained by the red fluorescent dye PKH-26 before x-irradiation. One-third of DCs took up apoptotic bodies from the irradiated vector-producing cells within 24 h, with the proportion of positive cells increasing over time (Fig. 3A). Moreover, the presence of fluorescent bodies within the cytoplasm of DCs was confirmed by confocal microscopy (Fig. 3B, arrow). Appropriate control experiments with nonirradiated vector-producing cells confirmed the complete dependence of the phenomenon on irradiation (data not shown). Finally, the active role of irradiation-induced apoptosis in transfer of the transgene product to DCs was demonstrated by the observation that nonirradiated vector-producing cells failed to induce a transgene-specific T cell response (data not shown). Together, these results are consistent with the source of the cytoplasmic transgene-encoded Ag being material derived from apoptotic vector-producing cells. A similar mechanism has been described to occur in a model of influenza virus-induced apoptosis (12).
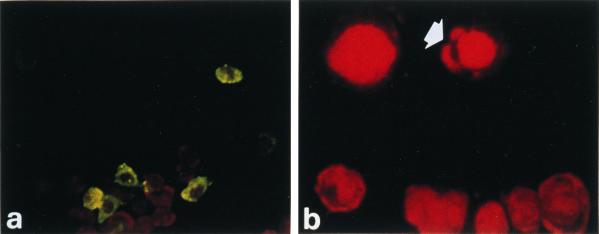
Figure 2.
X-ray irradiation induces apoptotic cell death of retrovirus-producing cells. Irradiated (100 Gy) M3-CSM cells were cultured for 24 h, after which the cells were stained with annexin V-FITC (a), an early marker of apoptosis, and propidium iodide (b) that allowed visualization of condensed nuclear chromatin. The arrow indicates condensed chromatin in the cell surface blebs.
Figure 3.
Uptake of apoptotic bodies by DCs during differentiation. DCs, at day 2 of culture, were cocultivated with irradiated M3-CSM cells, previously labeled with red fluorescent dye PKH-26. Flow cytometry analysis (A) for PKH-26-red and CD45-FITC expression by DCs was performed after 24 and 48 h of cocultivation. Confocal microscopy analysis (B) showed the presence of intracellular apoptotic bodies (red staining) within the cytoplasm of DCs labeled with a HLA-DR-FITC mAb (green staining).
High-capturing and processing activity associated with low-stimulating properties are specific features of immature DCs (13). This functional profile is characterized by the absence of CD83 expression on the cell surface (13). On the contrary, mature CD83+ DCs show reduced Ag-uptake capabilities and enhanced Ag-presenting functions (13). In vitro, the transition between the two stages is achieved by the exposure of differentiating DCs to inflammatory stimuli (26). This maturation pathway also occurs in vivo, once the immature DCs uptake Ags in peripheral tissues, undergo maturation, and migrate to the T cell areas of lymph nodes, where a T cell response is primed (26). In our system, this two-step process was mimicked. DCs were exposed to apoptotic vector-producing cells at day 2 of culture, when they had an immature phenotype (i.e., CD1a+ CD83−; data not shown) and thus can engulf apoptotic cells with high efficiency (Fig. 3). During cocultivation, DCs underwent maturation, probably triggered by the presence of apoptotic bodies (27) and by the addition to the culture media of low amounts of lipopolysaccharide (see Materials and Methods). At day 5, when DCs were harvested and used to stimulate a T cell response, CD1a expression was downmodulated, while 40–80% of the cells were CD83+, with high expression level of CD86, CD80, HLA-class I, and -class II molecules (data not shown). This profile is characteristic of mature DCs able to trigger an efficient immune response.
DCs Induce a TAA-Specific Response upon Phagocytosis of Apoptotic Cells.
Our data concerning the induction of a TN-specific T cell response are consistent with the results obtained in a model of influenza virus-induced apoptosis (12). The central role of this presentation pathway in the induction of tumor immunity has been recently addressed in mice (14, 15) and rats (16). However, no experimental evidence is yet available on the role of such mechanism in the induction of a specific T cell response against defined human TAAs.
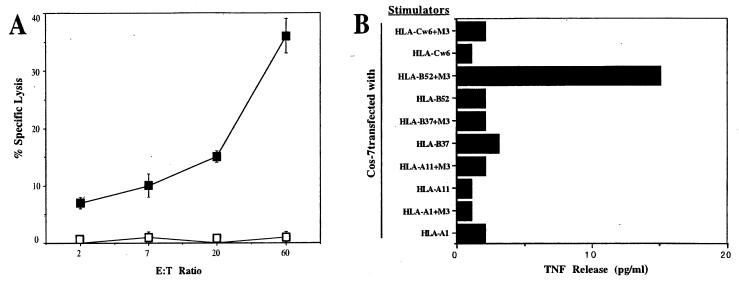
To investigate whether our approach can induce a tumor-specific immune response, we utilized a cell line producing the M3-CSM retroviral vector (19), coding for the ΔLNGFr marker and for the MAGE-3 TAA (1). Intracellular processing of MAGE-3 generates at least five peptides presented by HLA-A1, -A2, -A24, -B37, and -B44. The M3-A1 epitope has been recently shown to have an active role in the control of tumor growth in clinical trials of cancer vaccination with tumor peptides (28). Lymphocytes collected from a MAGE-3+ melanoma lesion of an HLA-A1, -B37 patient (17) were stimulated in vitro by autologous DCs previously exposed to irradiated M3-CSM vector-producing cells. After three rounds of in vitro stimulation, the effector population, referred to as MSR3-M3, specifically killed autologous target cells expressing MAGE-3 (Fig. 4A). However, these effectors did not recognize Cos-7 cells expressing MAGE-3 along with either HLA-A1 or HLA-B*3701 molecules (Fig. 4B), indicating that another, yet unknown epitope was involved. Indeed, specific TNF release was detected when MSR3-M3 effectors were challenged with Cos-7 cells transfected with MAGE-3 and HLA-B*5201 cDNAs (Fig. 4B).
Figure 4.
DCs exposed to irradiated M3-CSM vector-producing cells induce CTLs specific for the MAGE-3 human TAA. (A) Lymphocytes derived from a MAGE-3+ melanoma lesion were in vitro stimulated with 2 × 105 autologous DCs cocultured with x-irradiated M3-CSM vector-producing cells. Lytic activity of the effectors was tested against autologous T-blasts untreated (□) or transduced with the M3-CSM vector (■) in a standard chromium release assay at the indicated effector-to-target cell (E:T) ratios. (B) DCs-induced MAGE-3-specific effectors, referred to as MSR3-M3, recognize an HLA-B*5201-restricted MAGE-3 epitope. Cos-7 cells were cotransfected with cDNA encoding the autologous HLA alleles alone, or together with MAGE-3 cDNA. Production of TNF by MSR3-M3 effectors was measured after 20 h of coculture with the transfected cells.
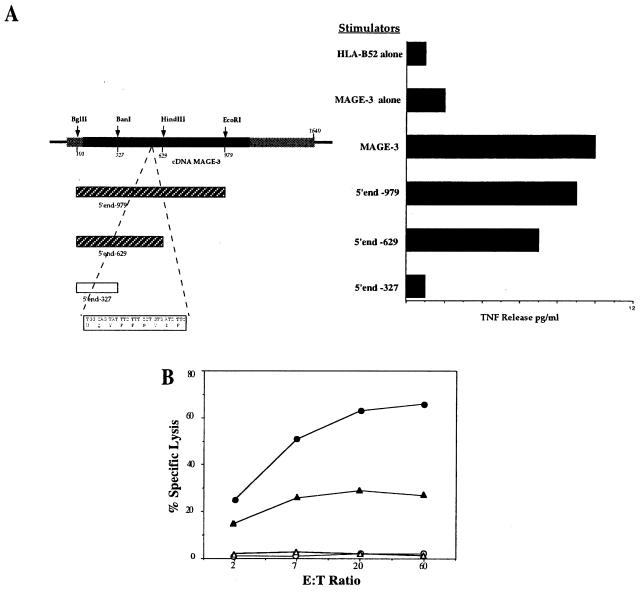
To identify the sequence coding for the antigenic peptide(s) recognized by MSR3-M3, EcoRI, HindIII, and BanI enzymes were used to generate progressive deletions from the 3′ end of the MAGE-3 cDNA. The three subfragments of 979, 629, and 327 bp (Fig. 5A) were cotransfected with HLA-B*5201 into Cos-7 cells. Specific TNF release was observed in the presence of the 629-bp fragment but not for the 327-bp fragment, indicating that the antigenic peptide had to be encoded between nucleotides 327 and 629 (Fig. 5A). By screening this region for peptides carrying HLA-B*5201 binding motif (i.e., Asp in position 2 and Phe or Ile in position 9/10) (29), one nonapeptide was identified, WQYFFPVIF (amino acids 143–151). This peptide, referred to as M3.143–151, sensitized autologous T cells (T-blasts) to lysis by MSR3-M3 (Fig. 5B). Most importantly, the autologous tumor cells processed and presented the M3.143–151 epitope as demonstrated by the killing of the MSR3-B52 melanoma cell line (Fig. 5B).
Figure 5.
Identification of the antigenic peptide recognized by MSR3-M3 effectors. (A) (Top Left) The MAGE-3 ORF is shown as a filled box; the numbering of the sequence is relative to the 5′ end of the cDNA. Three subfragments derived from MAGE-3 cDNA were cotransfected into Cos-7 cells along with HLA-B*5201, those recognized by MSR3-M3 effectors (hatched boxes) are indicated. The peptide coding sequence present in subfragments 979 bp and 629 bp, but not in subfragment 327 bp is shown (Bottom Left). (Right) Production of TNF by MSR3-M3 cells was measured after 20 h of coculture with the transfected cells. As control, Cos-7 cells were transfected with HLA-B*5201 alone or together with the full-length MAGE-3 cDNA. (B) MSR3-M3 effectors recognized peptide M3.143–151 and killed the autologous tumor cells. MSR3-M3 effectors were tested in a standard cytotoxicity assay against the autologous MSR3-B52 (▴) and HLA-unrelated (▵) melanomas, and autologous activated T-blasts, in the presence (●) or in the absence (○) of 3 μM of peptide WQYFFPVIF.
The results of this study show that a strong cytotoxic T cell response, specific for the HSV-Tk viral protein, can be induced by human DCs exposed to apoptotic HSV-Tk-expressing murine cells. Moreover, we provide evidence that the same mechanism can be exploited to induce a class I-restricted cytotoxic response against human TAAs. DCs exposed to apoptotic cells expressing MAGE-3 are able to induce a MAGE-3-specific response. Noteworthy, although MAGE-3 peptides have been shown previously to be processed and presented by the patient's HLA-A1 and B*3701 alleles, the response we detected was directed against a MAGE-3 epitope presented by HLA-B*5201. Thus, suggesting that phagocytosis and processing of apoptotic Ag-expressing cells, rather than pulsing with synthetic peptides, allows DCs to present all the relevant peptides and thus to expand CTL populations that could, indeed, have an immunodominant role in tumor rejection.
The data from this study provide the rationale for the development of a strategy for cancer vaccination that mimics Ag presentation at the tumor site, as recently described by Chiodoni et al. (14) in a murine model. In our system, the autologous tumor cells, that often are not available, are replaced by NIH/3T3 murine fibroblasts overexpressing one or more defined human TAAs. We believe that the use of a xenogeneic cell line as source of apoptotic bodies might represent a useful tool to avoid/limit the induction of auto-immune responses. However, we can foresee the development of alternative sources of apoptotic bodies characterized by the expression of large amounts of transfected TAAs, and by the ability to generate apoptotic cells that can access the HLA class I pathway of DCs with high efficiency. Patient-derived DCs loaded ex vivo with the described apoptotic cells might be used as cancer vaccines in patients whose neoplasms express known TAAs.
Acknowledgments
We thank A. Manfredi and K. Fleischhauer for helpful discussion. This work was supported by grants from the Italian Association for Cancer Research and from the Ministry of Health (Ricerca finalizzata RF 98.51). S.T. is the recipient of a fellowship from the Italian Foundation for Cancer Research.
Abbreviations
- DC
dendritic cell
- TAA
tumor antigen
- Ag
antigen
- APC
Ag-presenting cell
- TN
fusion protein between the thymidine kinase of herpes simplex virus and the neomycin phosphotransferase
- CTL
cytotoxic T lymphocyte
- PBL
peripheral blood lymphocyte
- TNF
tumor necrosis factor
- HSV-Tk
herpes simplex virus thymidine kinase
Footnotes
Article published online before print: Proc. Natl. Acad. Sci. USA, 10.1073/pnas.040540197.
Article and publication date are at www.pnas.org/cgi/doi/10.1073/pnas.040540197
References
- 1.Boon T, Coulie P G, Van den Eynde B. Immunol Today. 1997;18:267–268. doi: 10.1016/s0167-5699(97)80020-5. [DOI] [PubMed] [Google Scholar]
- 2.Lanzavecchia A. Science. 1993;260:937–944. doi: 10.1126/science.8493532. [DOI] [PubMed] [Google Scholar]
- 3.Austyn J M. J Exp Med. 1996;183:1287–1292. doi: 10.1084/jem.183.4.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Banchereau J, Steinman R M. Nature (London) 1998;392:245–252. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- 5.Celluzzi C M, Mayordomo J I, Storkus W J, Lotze M T, Falo L G J. J Exp Med. 1996;183:283–287. doi: 10.1084/jem.183.1.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paglia P, Chiodoni C, Rodolfo M, Colombo M P. J Exp Med. 1996;183:317–322. doi: 10.1084/jem.183.1.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zitvogel L, Mayordomo J I, Tjandrawan T, DeLeo A B, Clarke M R, Lotze M T, Storkus W J. J Exp Med. 1996;183:87–97. doi: 10.1084/jem.183.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mayordomo J I, Zorina T, Storkus W J, Zitvogel L, Celluzzi C, Falo L D, Melief C J, Ildstat S T, Kast W M, Deleo A B, Lotze M T. Nat Med. 1995;1:1297–1302. doi: 10.1038/nm1295-1297. [DOI] [PubMed] [Google Scholar]
- 9.Zhou L J, Tedder T F. Proc Natl Acad Sci USA. 1996;93:2588–2592. doi: 10.1073/pnas.93.6.2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imro M A, Manici S, Russo V, Consogno G, Bellone M, Rugarli C, Traversari C, Protti M P. Cancer Res. 1999;59:2287–2291. [PubMed] [Google Scholar]
- 11.Nestle F O, Alijagic S, Gilliet M, Sun Y, Grabbe S, Dummer R, Burg G, Schadendorf D. Nat Med. 1998;4:328–332. doi: 10.1038/nm0398-328. [DOI] [PubMed] [Google Scholar]
- 12.Albert M L, Sauter B, Bhardwaj N. Nature (London) 1998;392:86–89. doi: 10.1038/32183. [DOI] [PubMed] [Google Scholar]
- 13.Albert M L, Pearce S F, Francisco L M, Sauter B, Roy P, Silverstein R L, Bhardwaj N. J Exp Med. 1998;188:1359–1368. doi: 10.1084/jem.188.7.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chiodoni C, Paglia P, Stoppacciaro A, Rodolfo M, Parenza M, Colombo M P. J Exp Med. 1999;190:125–133. doi: 10.1084/jem.190.1.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ronchetti A, Rovere P, Iezzi G, Galati G, Heltai S, Protti M P, Garancini M P, Manfredi A A, Rugarli C, Bellone M. J Immunol. 1999;163:130–136. [PubMed] [Google Scholar]
- 16.Henry F, Boisteau O, Bretaudeau L, Lieubeau B, Meflah K, Gregoire M. Cancer Res. 1999;59:3329–3332. [PubMed] [Google Scholar]
- 17.Tanzarella S, Russo V, Lionello I, Dalerba P, Rigatti D, Bordignon C, Traversari C. Cancer Res. 1999;59:2668–2674. [PubMed] [Google Scholar]
- 18.Bonini C, Ferrari G, Verzeletti S, Servida P, Zappone E, Ruggieri L, Ponzoni M, Rossini S, Mavilio F, Traversari C, Bordignon C. Science. 1997;276:1719–1724. doi: 10.1126/science.276.5319.1719. [DOI] [PubMed] [Google Scholar]
- 19.Fleischhauer K, Tanzarella S, Russo V, Sensi M L, van der Bruggen P, Bordignon C, Traversari C. J Immunol. 1997;159:2513–2521. [PubMed] [Google Scholar]
- 20.Coulie P G, Brichard V, Van Pel A, Wolfel T, Schneider J, Traversari C, Mattei S, De Plaen E, Lurquin C, Szikora J P, et al. J Exp Med. 1994;180:35–42. doi: 10.1084/jem.180.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Traversari C, van der Bruggen P, Van den Eynde B, Hainaut P, Lemoine C, Ohta N, Old L, Boon T. Immunogenetics. 1992;35:145–152. doi: 10.1007/BF00185107. [DOI] [PubMed] [Google Scholar]
- 22.Sallusto F, Lanzavecchia A. J Exp Med. 1994;179:1109–1118. doi: 10.1084/jem.179.4.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Romani N, Gruner S, Brang D, Kampgen E, Lenz A, Trockenbacher B, Konwalinka G, Fritsch P O, Steinman R M, Schuler G. J Exp Med. 1994;180:1111–1120. doi: 10.1084/jem.180.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mavilio F, Ferrari G, Rossini S, Nobili N, Bonini C, Casorati G, Traversari C, Bordignon C. Blood. 1994;83:1988–1997. [PubMed] [Google Scholar]
- 25.Hannun Y A. Blood. 1997;89:1845–1853. [PubMed] [Google Scholar]
- 26.Lanzavecchia A. Curr Opin Immunol. 1996;8:348–354. doi: 10.1016/s0952-7915(96)80124-5. [DOI] [PubMed] [Google Scholar]
- 27.Rovere P, Vallinoto C, Bondanza A, Crosti M C, Rescigno M, Ricciardi-Castagnoli P, Rugarli C, Manfredi A A. J Immunol. 1998;161:4467–4471. [PubMed] [Google Scholar]
- 28.Marchand M, van Baren N, Weynants P, Brichard V, Dréno B, Tessier M H, Rankin E, Parmiani G, Arienti F, Humblet Y, et al. Int J Cancer. 1999;80:219–230. doi: 10.1002/(sici)1097-0215(19990118)80:2<219::aid-ijc10>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 29.Rammensee H G, Friede T, Stevanoviic S. Immunogenetics. 1995;41:178–228. doi: 10.1007/BF00172063. [DOI] [PubMed] [Google Scholar]