Abstract
Evidence indicates that a diet rich in omega (ω)-6 polyunsaturated fatty acids (PUFAs) [e.g., linoleic acid (LA)] increases prostate cancer (PCa) risk, whereas a diet rich in ω-3 decreases risk. Precisely how these PUFAs affect disease development remains unclear. So we examined the roles that PUFAs play in PCa, and we determined if increased ω-3 consumption can impede tumor growth. We previously demonstrated an increased expression of an ω-6 LA-metabolizing enzyme, 15-lipoxygenase-1 (15-LO-1, ALOX15), in prostate tumor tissue compared with normal adjacent prostate tissue, and that elevated 15-LO-1 activity in PCa cells has a protumorigenic effect. A PCa cell line, Los Angeles Prostate Cancer-4 (LAPC-4), expresses prostate-specific antigen (PSA) as well an active 15-LO-1 enzyme. Therefore, to study whether or not the protumorigenic role of 15-LO-1 and dietary ω-6 LA can be modulated by altering ω-3 levels through diet, we surgically removed tumors caused by LAPC-4 cells (mouse model to simulate radical prostatectomy). Mice were then randomly divided into three different diet groups—namely, high ω-6 LA, high ω-3 stearidonic acid (SDA), and no fat—and examined the effects of ω-6 and ω-3 fatty acids in diet on LAPC-4 tumor recurrence by monitoring for PSA. Mice in these diet groups were monitored for food consumption, body weight, and serum PSA indicative of the presence of LAPC-4 cells. Fatty acid methyl esters from erythrocyte membranes were examined for ω-6 and ω-3 levels to reflect long-term dietary intake. Our results provide evidence that prostate tumors can be modulated by the manipulation of ω-6:ω-3 ratios through diet and that the ω-3 fatty acid SDA [precursor of eicosapentaenoic acid (EPA)] promotes apoptosis and decreases proliferation in cancer cells, causing decreased PSA doubling time, compared to ω-6 LA fatty acid, likely by competing with the enzymes of LA and AA pathways, namely, 15-LO-1 and cyclooxygenases (COXs). Thus, EPA and DHA (major components of fish oil) could potentially be promising dietary intervention agents in PCa prevention aimed at 15-LO-1 and COX-2 as molecular targets. These observations also provide clues as to its mechanisms of action.
Keywords: Polyunsaturated fatty acids, cancer prevention, radical prostatectomy, 15-lipoxygenase-1, prostate cancer
Introduction
Prostate cancer (PCa) remains one of the leading causes of cancer deaths among men in the United States. Current therapies for PCa include watchful waiting, radical prostatectomy, hormonal therapy, and targeted radiation. Unfortunately, all available therapies have associated risks and limitations, and new therapeutic strategies are critically needed [1]. One promising strategy involves the use of dietary intervention. International incidence patterns and migrations studies, epidemiological data, and animal and in vitro studies indicate that consuming a diet rich in fat increases the risk for developing PCa [2–7]. In a mouse xenograft model for PCa, an isocaloric low-fat diet slowed prostate tumor growth, further corroborating a role for fat in PCa development [8,9]. Dietary fat includes omega (ω) 3 and ω-6 polyunsaturated fatty acids (PUFAs), both of which play important roles in many human biologic processes. As humans cannot synthesize ω-3 and ω-6 PUFAs, they are considered essential fatty acids. Although all mammalian cells can interconvert PUFAs within each series by elongation, desaturation, and retroconversion, the two series are not interchangeable due to lack of the Fat-1 gene [10], which encodes ω-3 desaturase enzyme [11,12].
Linoleic acid (LA; 18:2ω-6) represents an ω-6 PUFA commonly found in high-fat Western diets [13]. Terrestrial plants synthesize LA and, once ingested by mammals, LA is either metabolized to 13-(S)-hydroxyoctadecadienoic acid [13-(S)-HODE] or converted further to arachidonic acid (AA; 20:4ω-6). Three fatty acids, found primarily in fish oils, comprise the ω-3 family: alpha linolenic acid (ALA or α-LNA; 18:3ω-3), eicosapentaenoic acid (EPA; 20:5ω-3), and docosahexaenoic acid (DHA; 22:6ω-3). ALA, synthesized by cold water vegetation, is converted by fish to EPA and DHA. Of note, through the same series of enzymes used to convert LA to AA, humans can synthesize EPA and DHA from ingested ALA. The conversion of dietary ALA to EPA and DHA is also dependent on the dietary ω-6:ω-3 ratio [13]. Importantly, US diets provide excessive LA [14], which competes with ALA for desaturase and elongase enzymes, impeding the formation of EPA and DHA. Studies have suggested that the high incidence of PCa in Americans may, in part, result from an imbalance in the ratio of ω-3 to ω-6 fatty acids because the typical American diet is low in ω-3 and high in ω-6.
The negative effects of fatty acids may be direct or indirect [15–21], and the preponderance of evidence indicates that ω-3 and ω-6 fatty acids modulate PCa tumorigenesis. Yet, how these fatty acids affect disease development remains unclear. Work from our laboratory [17,18,22,23] and that of others [24–28] suggest that metabolites of PUFAs directly impact PCa and that the ability to do so depends on both diet and metabolic enzyme expression. Recently, we demonstrated an increased expression of an ω-6 LA-metabolizing enzyme, 15-lipoxygenase-1 (15-LO-1, ALOX15), in prostate tumor tissue compared with normal adjacent tissue [17]. Although AA can also act as a substrate for 15-LO-1, yielding the anti-inflammatory and proapoptotic metabolite 15-(S)-hydroxyeicosatetraenoic acid (15-(S)-HETE), the 15-LO-1 enzyme greatly prefers LA. 15-LO-1 metabolizes LA to 13-(S)-HODE, which can regulate cell growth, differentiation, and vascular homeostasis [17,18,24,29]. Although an increase in 15-LO-1 in colon cancer has previously been reported [30], this observation remains controversial [31]. TRansgenic Adenocarcinoma of Mouse Prostate (TRAMP) mice fed a highly saturated fat diet developed higher prostate tumor incidence compared with those fed a low-fat diet [32] and displayed high 12/15-LO (orthologue of human 15-LO-1) with PCa progression [33]. Human and mouse studies indicate that a high-LA diet may be a major risk factor for developing PCa, especially in those individuals with high 15-LO-1 concentrations in the prostate epithelium.
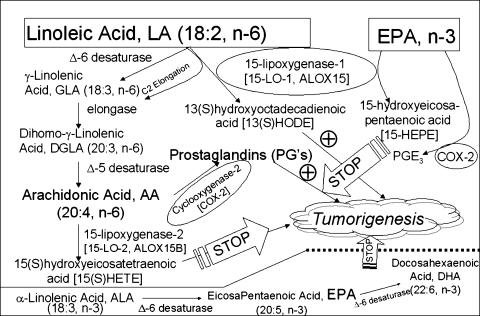
In addition, AA also acts as a substrate for cyclooxygenases (COX) 1 and 2 [34]. Most tissues constitutively express low protein levels of COX-1 and no COX-2. Growth factors or inflammatory agents rapidly induce COX-2 expression in prostate [35], and studies show overexpression of COX-2 in PCa [36,37]. COX-2 overexpression, leading to the production of proinflammatory prostaglandins (e.g., PGE2), possibly contributes to PCa pathobiology. Recently, a study has shown that the combination of DHA and celecoxib (a COX-2-specific inhibitor) prevents PCa cell growth in vitro [38]. This inhibition of disease development likely results, in part, from the ability of the ω-3 PUFA EPA to successfully compete with LA and AA for 15-LO-1 and COX-2, respectively. 15-LO-1 metabolizes EPA to 15-hydroxyeicosapentaenoic acid (15-HEPE) [39], a metabolite shown to have antitumorigenic properties, whereas COX-2 metabolizes EPA to the anti-inflammatory and antitumorigenic prostaglandin PGE3 [40,41]. The ω-3 PUFA EPA also serves as a substrate for 15-LO-1 and COX-2, but the metabolism of EPA by these enzymes results in the formation of antitumorgenic products. Therefore, ω-3 fatty acids may not only decrease the production of protumorigenic metabolites derived from the ω-6 fatty acid pathway, but may also result in increased production of antitumorigenic metabolites.
Based on these studies, we hypothesized that a diet rich in ω-6 PUFAs would cause rapid prostate tumor progression through the 15-LO-1 and COX metabolic pathways, whereas increased consumption of ω-3 PUFAs would antagonize this effect. Our study suggests two mechanisms for slowing PCa progression: 1) EPA and LA both compete as substrates for the enzyme 15-LO-1, which may result in a decrease in the protumorigenic metabolite of LA, 13-(S)-HODE, and an increase in the antitumorigenic metabolite of EPA, 15-HEPE; and 2) EPA and AA both compete as substrates for the enzyme COX-2, which may result in a decrease in the proinflammatory metabolite of AA, PGE2, and an increase in the anti-inflammatory metabolite of EPA, PGE3. Thus, EPA alone or EPA-derived fatty acids such as DHA could be promising dietary intervention agents in PCa aimed at 15-LO-1 and COX-2 as molecular targets.
Materials and Methods
Cell Culture
Los Angeles Prostate Cancer-4 (LAPC-4) PCa cells were kindly provided by Dr. Robert Reiter (University of California-Los Angeles, Los Angeles, CA) and maintained in phenol red-free Dulbecco's modified Eagle's medium (DMEM; Invitrogen, Carlsbad, CA) containing 5% heat-inactivated fetal calf serum (Sigma, St. Louis, MO) with streptomycin-penicillin antibiotics [designated DMEM/fetal bovine serum (FBS)] in a 5% CO2 incubator at 37°C. The PC3-15LOS (15-LO-1-overexpressing) PCa cells were grown in RPMI/FBS medium containing 50 µg/ml Zeocin (Invitrogen).
RNA Isolation and Real-Time Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) Analysis
Total RNA was isolated using RNeasy kit (Qiagen, Inc., Valencia, CA), and its concentration was determined using RiboGreen fluorescent dye (Molecular Probes, Inc., Eugene, OR) with VersaFluor Fluorometer System (BioRad, Hercules, CA). The quality and integrity of total RNA were assessed on 1% formaldehyde agarose gels. First-strand cDNA was synthesized using 1 µg of total RNA (DNase-treated) in a 20-µl RT reaction mixture. A 120-bp region of β-actin using primers 5′-CCTGGCACCCAGCACAAT-3′ and 5′-GCCGAT-CCACACGGAGTACT-3′ and a 140-bp region of 15-LO-1 using primers 15-LO-1 5′-CCAACCACCAAGGATGCAA-3′ and 5′-GGAGAGAAGCCTGGTGGAAGT-3′ were amplified. Separately, PCR-amplified cDNA products were also electrophoresed in a 2% agarose gel. In parallel, all real-time PCR reactions were performed in a 25-µl mixture containing 1/20 vol of cDNA preparation (1 µl), 1 x SYBR Green buffer (PE Applied Biosystems, Foster City, CA), 4 mM MgCl2, 0.2 µM of each primer (β-actin and 15-LO-1), 0.2 mM deoxynucleoside triphosphate mix, and 0.025 U of AmpliTaq Gold thermostable DNA polymerase (Applied Biosystems). Real-time quantitations were performed using iQ5 Real-Time PCR Detection System (BioRad). Fluorescence threshold value was calculated using system software. Optimization experiments showed that PCR for β-actin in triplicate was highly reproducible with a low intra-assay coefficient of variation (0.5%).
Cell Proliferation and Viability Analyses
LAPC-4 cells (5000 cells/well) were plated in each well of 96-well plates (Costar Cat. No. 3595) in 100 µl of DMEM/FBS. Twenty-four hours after plating, cells were further grown in serum-free medium containing appropriate concentrations of eicosanoids and/or fatty acids in 0.1 % ethanol (experimental) vs 0.1% ethanol in PBS only (control; day 0) and 3-(4,5-dimethylthiazolyl-2)-2,5-diphenyltetrazolium bromide (MTT) assays (ATCC, Manassas, VA) performed on cells grown for 96 hours. The concentrations of EPA, DHA, and 15-HEPE were as described in the text and figure legends. At indicated time periods, the medium was aspirated from the wells, and 200 µl of MTT reagent (1 mg/ml) was added to each well. The cells were then incubated for 1 hour at 37°C and lysed by the addition of 200 µl of isoamyl alcohol and by shaking for 20 minutes. A 200-µl aliquot of each sample was then transferred to 96-well plates and read in an enzyme-linked immunosorbent assay reader at 570 to 690 nm. The percent increase or decrease (corrected absorbance) in cell proliferation is measured and reported as x100 OD at 570 nm. Doubling times were calculated by solutions of the equations derived by unweighed linear regression analysis of semi-logarithmic plots of the formazan data derived from the MTT assay. To examine the dose response of EPA, DHA, EPA + DHA, and 15-HEPE on growth, concentrations ranging from 10 to 300 µM were added in serum-free medium on day 0 and MTT assay was performed after 96 hours of incubation. LAPC-4 cells were harvested, and survival was estimated from those that excluded 0.2% trypan blue. Total and viable cell contents were determined by counting in a hemocytometer.
15-LO-1 and COX Enzyme Activities in LAPC-4 Cells
To establish that 15-LO-1 and COX-2 enzymes are active in LAPC-4 cells, cell homogenates (total protein, 800 µg) from LAPC-4 cells were incubated with 25 µM [1-14C]AA or [1-14C]LA (1 x 106 cpm; 15 nmol) in ethanol (2.5% of final volume) in the presence or absence of stearidonic acid (SDA) (10 µM) or EPA (10 µM) at 30°C for 15 minutes. The SDA was an ethyl ester obtained from K.D. Pharma Bexbach GmbH (Am Kraftwerk 6, Bexbach D-66450, Germany). The particular batch was 60% SDA and was verified by gas chromatography analysis [stearic acid, 0.95; oleic acid, 3.7%; LA, 2.2%; γ-linolenic acid (GLA), 5.3%; ALA, 5.8%; EPA, 1.6%; DHA, <0.1%]. The reaction mixture (600 µl) contained 50 mM Tris-HCl (pH 7.4) and 5 mM CaCl2. In all buffers, protease inhibitors were added just before use: phenylmethylsulfonyl fluoride and benzamidine at 1 mM each, aprotinin and leupeptin at 10 µg/ml, and pepstatin A at 1 µg/ml. After incubation, 0.3 mg of sodium borohydride was added, and the mixture was kept on ice for 15 minutes. This mixture was then acidified with HCl (pH 3.0). Appropriate unlabeled eicosanoids were used as internal standards. The sample was extracted in 2 ml of ethyl ether, the solvent was evaporated, and the dried material was dissolved in 50 µl of methanol:water (3:1) solvent. Reverse-phase high-performance liquid chromatography (HPLC) analyses were conducted with a C18 ultrasphere column (5 µm; 4.6 x 250 mm; Altex Scientific/Beckman Instruments, Fullerton, CA) equipped with a Waters model 6000A pump and a Waters (Milford, MA) model 717 autosampler injector. Metabolite separation was achieved using a 55% to 100% methanol stepwise gradient at 1.1 ml/min. Eluted radioactivity was monitored using Flo-One/Beta detector (Radiomatic Instruments, Tampa, FL) linked with an IBM Pentium 4 computer for data processing. UV analysis was also performed (for nonradioactive detection of SDA, EPA, and 15-HEPE) by monitoring absorbance at 234 nm with a Waters 486 detector. [1-14C]AA and [1-14C]LA (40–60 mCi/mmol) were from DuPont-New England Nuclear (Boston, MA). Unlabeled eicosanoids such as 13-hydroxyoctadecadienoic acid (13-HODE), 15-HETE, and 15-HEPE, and prostaglandins such as PGE2 and PGE3 were from Cayman Chemical (Ann Arbor, MI). All solvents were HPLC-grade and were from Baker (Phillipsburg, NJ). 15-LO-1 and COX enzyme activities were expressed as percent conversion of substrate(s) to product(s).
Enzyme Activity Calculation for Eicosanoid Pathway Analysis
The activities of enzymes (Table 2) involved in fatty acid biosynthesis were estimated as product-to-precursor ratios of the percentages of individual fatty acids [42]. Estimated enzyme activities included those of elongase, calculated as stearic acid (18:0):palmitic acid (16:0) ratio; Δ-5 desaturase, calculated as the AA (20:4, ω-6):dihomo-γ-linolenic acid (DGLA; 20:3, ω-6) ratio; Δ-6 desaturase, calculated as the DGLA (20:3, ω-6):LA (18:2, ω-6) ratio (assuming that Δ-6 desaturase, and not elongase, is rate-limiting); and Δ-9 desaturase, calculated as the oleic acid (18:1, ω-9):stearic acid (18:0, ω-9) ratio.
Table 2.
Phospholipid Analyses of Unsaturated and Saturated Fatty Acids, PUFA Ratios, and LA, AA, EPA, and DHA Compositions from Untreated Control Versus LA (100 µM)-, AA (100 µM)-, EPA (50 µM)-, LA + EPA-, and AA + EPA-Treated LAPC-4 Cells.
| Total Phospholipids | ω-6/ω-3 | Elongase | Δ-5-Desaturase | Δ-6-Desaturase | Δ-9-Desaturase | |||
| % Unsaturated | % Saturated | |||||||
| LAPC-4 | Control | 50.3 ± 1.3 | 40.6 ± 1.1 | 3.4 ± 0.6 | 118.0 ± 4.4 | 7.0 ± 0.4 | 3.6 ± 0.6 | 17.7 ± 0.4 |
| LA* | 51.4 ± 1.4 | 43.8 ± 1.4 | 9.1 ± 0.2 | 112.4 ± 5.4 | 15.4 ± 0.3 | 6.1 ± 1.4 | 7.8 ± 0.7 | |
| AA* | 49.7 ± 0.9 | 45.9 ± 1.2 | 6.1 ± 0.1 | 123.9 ± 3.7 | 12.3 ±0.7 | 7.0 ± 0.5 | 9.3 ± 0.5 | |
| LAPC-4 | EPA* | 50.1 ± 1.1 | 42.4 ± 1.4 | 0.9 ± 0.04 | 38.0 ± 1.3 | 0.5 ± 0.04 | 11.6 ±2.6 | 28.4 ± 0.6 |
| LA + EPA* | 52.8 ± 1.2 | 39.8 ± 1.2 | 2.1 ± 0.4 | 33.6 ± 1.5 | 0.9 ± 0.05 | 16.9 ±1.7 | 18.2 ± 0.4 | |
| AA + EPA* | 49.0 ± 1.4 | 45.4 ± 1.5 | 1.4 ± 0.5 | 35.1 ± 1.7 | 0.6 ± 0.05 | 12.4 ± 2.1 | 20.1 ± 0.3 | |
Fatty acid methyl esters were analyzed by temperature-programmed microcapillary gas liquid chromatography, as described in Materials and Methods section. The activities of key enzymes involved in fatty acid biosynthesis were estimated as the product-to-precursor ratios of the percentages of individual fatty acids. The estimated enzyme activities included those of elongase, calculated as the stearic acid (18:0):palmitic acid (16:0) ratio; Δ-5-desaturase, calculated as the AA (20:4, ω-6):dihomo-γ-linolenic acid (20:3, ω-6) ratio; Δ-6-desaturase, calculated as the dihomo-γ-linolenic acid (20:3, ω-6):LA (18:2, ω-6) ratio (assuming that ω-6-desaturase, and not elongase, is rate-limiting); and Δ-9-desaturase, calculated as the oleic acid (18:1, ω-9):stearic acid (18:0,ω-9) ratio. Data represent the mean ± SD of triplicate determinations from two separate experiments.
Concentrations added: LA (100 µM), AA (100 MM), and EPA (50 µM).
Animal, Feeding Protocol, LAPC-4 Injection, and Mouse Model to Simulate Radical Prostatectomy (MSRP)
Seventy-two athymic male BALB/C nude (nu/nu) mice (6–8 weeks old) were obtained from Charles River (Wilmington, MA) and started on a no-fat diet. The mice were housed in single sterile animal cages to allow for the maintenance of isocaloric intake between diet groups. Cages, bedding, and water were autoclaved before use. Specially designed feeding receptacles were placed in the cages so that food intake could be carefully monitored. Sterile techniques were used during the handling of cages, mice, and food. The Pittsburgh Animal Research Committee approved the experiments, and animals were cared for in accordance with institutional guidelines.
We used three different diets for our study: two diets were isocaloric and contained the same percent fat whereas one contained no fat (Table 3). These custom-made semipurified diets were prepared and irradiated by Purina Test Diet, Inc. (Richmond, IN). The high ω-6 diet contained 15 wt.% safflower oil (70% LA), which provided 10.5 wt.% LA in the diet, whereas the high ω-3 fat diet contained 15 wt.% SDA oil (SDA, 60% a precursor of EPA). Thus, the SDA diet provided 9 wt.% SDA (see Table 3 for composition). Use of pure EPA is cost-prohibitive; therefore, SDA, an immediate precursor of EPA, served as a legitimate substitute. Furthermore, because of concerns with mercury and polychlorinated biphenyl contamination of fish and fish oils, which currently provide the major sources of long-chain ω-3 in the human diet, land-based sources of functional ω-3 fatty acids such as SDA are currently being developed [43]. The caloric density of each of the fat-containing diets was 4.4 kcal/g. Note that the no-fat diet was not isocaloric to the fat diets because our study does not evaluate the role of the no-fat diet but specifically examines the individual roles of PUFAs in PCa. All the mice (n = 72) were kept on a no-fat diet for 2 weeks before the start of the experiment, so that tumor transplantation and the outcome of this study would not be confounded by variations in fatty acid levels from regular/normal diets.
Table 3.
Composition of Isocaloric Diets.
| Ingredient*,† | No Fat | SDA (ω-3) | LA (ω-6) |
| Sucrose | 35.0 | 35.0 | 35.0 |
| Casein (vitamin-free) | 21.0 | 21.0 | 21.0 |
| RP mineral mix no. 10 (adds 1.29% fiber) | 5.0 | 5.0 | 5.0 |
| Powdered cellulose | 3.0 | 3.0 | 3.0 |
| RP vitamin mix (adds 1.9% sucrose) | 2.0 | 2.0 | 2.0 |
| Choline chloride | 0.2 | 0.2 | 0.2 |
| DL-methionine | 0.2 | 0.2 | 0.2 |
| SDA | 0.0 | 15.0 | 0.0 |
| Safflower oil | 0.0 | 0.0 | 15.0 |
| Dextrin | 33.6 | 18.6 | 18.6 |
Three synthetic diets [namely, no fat (nonisocaloric), high ω-3 SDA, and high ω-6 LA] were designed with constant fat levels. The caloric density of each of the fat-containing diets was 4.4 kcal/g.
g Ingredient/100 g diet.
Values supplied by the supplier.
The day the mice were injected with LAPC-4 cells was counted as week 1. The mice were injected subcutaneously, in duplicate, in the right and left lateral flanks with 1 x 106 LAPC-4 tumor cells in 0.1 ml of Matrigel (Collaborative Biomedical Products, Bedford, MA). After LAPC-4 cell implantation, the mice (n = 72) continued on a no-fat diet for the first 9 weeks. On week 9, the tumors from the mice were surgically removed, skin was sutured, and mice were allowed to recover overnight. The mice were then randomly assigned (n = 24 per diet group) to LA, SDA, and no-fat diet groups and continued feeding over a 15-week time period (end point of the study). Throughout the experiment, mice were weighed and tumors were examined weekly. When tumors became palpable, tumor dimensions were measured using a caliper. Tumor volumes were calculated using the formula: length x width x height x 0.5236 [22].
Serum and Tumor Studies
The animals were euthanized when they had met institutional guidelines. Blood (100 µl) was collected from the dorsal metatarsal saphenous vein, and the serum was separated [44]. Serum was collected on weeks 1, 7, 9, 12, and 15, respectively (Figure 4), and assayed for prostate-specific antigen (PSA) using an enzyme-linked immunosorbent assay (ELISA) specific for human serum PSA (Diagnostic Systems Laboratories, Inc., Webster, TX).
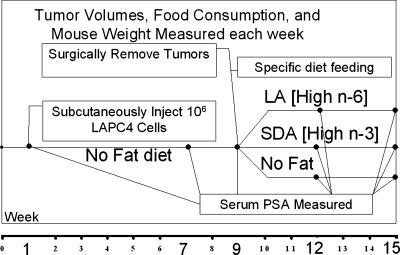
Figure 4.
MSRP. Male athymic male BALB/C nude (nu/nu) mice (6–8 weeks old) fed for 9 weeks. LAPC-4 cells were injected subcutaneously on week 1, and tumor growth was monitored for 9 weeks. On week 9, tumors were surgically removed and mice were randomly assigned to high ω-6 LA, high ω-3 SDA, and no-fat diet groups and fed accordingly until the termination of the experiment on week 15. Serum PSA was measured on weeks 1, 7, 9, 12, and 15, respectively. Tumor volume, food consumption, and mouse weight were measured every week.
Fatty Acid Composition from Erythrocyte Membranes and LAPC-4 Cells
Washed erythrocyte membranes (from serum-separated samples) or LAPC-4 cells (1 x 106) were extracted with chloroform/methanol and fatty acid methyl esters prepared by BF3 transmethylation. Fatty acid methyl esters were analyzed by temperature-programmed microcapillary gas liquid chromatography using an IDSP-2380 column (30 cm x 0.25 mm; Supelco, Supelco Park, PA) by reference to known standards (NuCheck Prep, Elysian, MN). The fatty acids are expressed as a percentage from total phospholipids measured (C14/C22). The relative amount of each fatty acid was quantified by integrating the area under the peak and dividing the result by the total area for all fatty acids. The total percentage of long-chain PUFA with ≥20 carbon units (C20–C22 PUFA), the sum of n-3 PUFA (18:3 n-3, 20:5 n-3, 22:5 n-3, and 22:6 n-3), and the sum of n-6 PUFA (18:2 n-6, 20:3 n-6, and 20:4 n-6) were calculated from primary data. The interassay coefficient of variation for determination of different fatty acids by this method ranged between 2.6% and 9.1%, reflecting the high reproducibility of the assay.
Assessment of 15-LO-1, Apoptotic Index, and Proliferation Index by Immunohistochemistry
Sections of formalin-fixed paraffin-embedded LAPC-4 tumor tissues (5 µm) were tested for the presence of 15-LO-1 (1:1600), Ki-67, and caspase-3 (1:50), using an avidin-biotin complex technique and steam heat-induced antigen retrieval. Cells were defined as apoptotic if the whole nuclear area of the cell was labeled positively for caspase-3. Apoptotic bodies were defined as small positively labeled globular bodies in the cytoplasm of tumor cells (singly or in groups). To estimate apoptotic index (the percentage of apoptotic events in a given area), apoptotic cells and bodies were counted in 10 high-power fields, and this figure was divided by the number of tumor cells in the same high-power fields. We also estimated the apoptotic index by light microscopy using hematoxylin-stained slides from the same tumor sections as those of caspase-3. The intensity of staining in 10 high-power fields was scored descriptively or semiquantitatively by a pathologist as: 1+, 0% to 25% positive cells; 2+, 25% to 50 % positive cells; 3+, 50% to 75% positive cells; and ≥4+, 75% to 100% positive cells) in a blinded manner. Proliferation was similarly examined, and the index was estimated as total Ki-67-labeled cells/total cells counted.
Statistical Analyses
Statistical analyses (SAS ver 5.0) were performed by Student's t test or analysis of variance. Correlations between outcome variables were computed using the Spearman correlation coefficient. P ≤ .05 was considered significant. Data are expressed as mean ± standard deviation (SD).
Results
Effect of Eicosanoids and Fatty Acids on the Growth of LAPC-4 Cells In Vitro
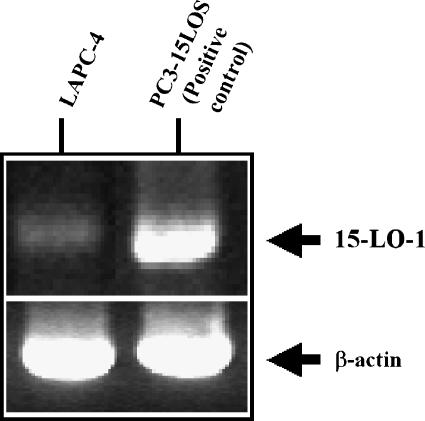
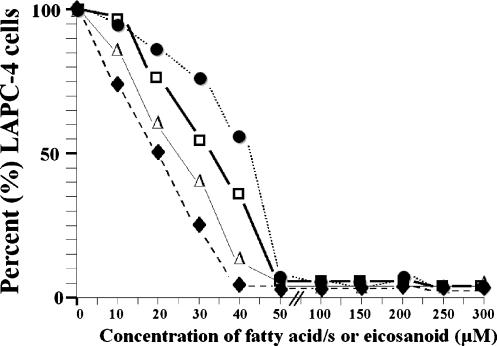
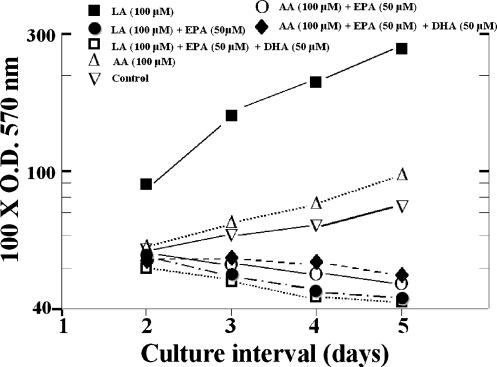
As shown in Figure 1, 15-LO-1 mRNA is expressed in LAPC-4 cells as determined using a PC-3 cell line overexpressing 15-LO-1 (PC3-15LOS) as standard. This observation was further confirmed by quantitative PCR analysis (data not shown). As shown in Figure 2, a dose-dependent inhibition in growth (at 96 hours) from initially plated 1 x 106 (considered as 100% for growth assay) LAPC-4 cells was observed when supplemented with EPA, DHA, EPA + DHA, and 15-HEPE in a growth medium (replaced by fresh media every 12 hours). The effective growth-inhibitory concentration of 15-HEPE, DHA, and EPA was 50 µM. Overall, the inhibition was EPA + DHA > EPA > 15-HEPE > DHA, respectively. The inhibition data also point to an important observation. No difference in cell numbers was observed on day 1 from those seeded on day 0, indicating that none of the eicosanoids or fatty acids exerted any cytotoxicity effects. Moreover, neither the ω-3 EPA and DHA nor the eicosanoid EPA causes toxicity at higher concentrations (i.e., from 100 to 300 µM). This dose-dependent inhibition was not observed in the benign prostatic hyperplasia-1 cell line containing undetectable levels of 15-LO-1 (data not shown). Similarly, as shown in Figure 3, there was increase in the growth/proliferation of LAPC-4 cells when supplemented with 100 µM LA and AA in the growth medium (replaced by fresh media every 12 hours), although LA showed a two-fold- to three-fold-higher proliferation rate when compared with AA over a 96-hour time period. However, 50 µM EPA or DHA (alone or in combination) caused inhibition in LAPC-4 growth when added with either 100 µM LA or AA in the growth medium over the same time period (i.e., 96 hours). This result suggests that the inhibition of LAPC-4 cell growth by EPA and DHA is caused by competition with LA and AA as substrates for 15-LO-1 and/or COX enzyme.
Figure 1.
RT-PCR of 15-LO-1 and β-actin expression in LAPC-4 and PC3-15LOS cells (control).
Figure 2.
PUFA modulation of LAPC-4 proliferation. Cells were propagated on medium containing 10% FBS. Monolayers were harvested, and cells were plated (5 x 103 cells/well and considered as 100% cells) in 96-well plates on a medium either containing different concentrations (0–300 µM) or lacking (control) EPA (△-△), DHA (●-●), EPA + DHA (◆-◆), and 15-HEPE (□-□). Viable cell content was determined by quantification of formazan production. For clarity, SD error bars from the mean of quadruplicate wells (SD ≤ 10% of the mean) have been omitted.
Figure 3.
Effect of LA (100 µM; ■-■), AA (100 µM; △-△), LA + EPA (50 µM; ●-●), LA + EPA + DHA (50 µM; □-□), AA + EPA (○-○), and AA + EPA + DHA (◆-◆) on the growth of 5 x 103 cells/well LAPC-4 in vitro. The untreated cells were used as control (▽-▽). Each point represents the mean ± SD of triplicate determinations from two separate experiments. For clarity, SD error bars from mean of triplicate wells (SD ≤ 10% of the mean) have been omitted. Values are half times for either population doubling (positive values) or viable cell loss (negative values). Half times were obtained by the solution of regression equations.
15-LO-1 and COX Enzyme Activities in LAPC-4 Cells
To study whether ω-3 EPA and SDA inhibited LAPC-4 cell growth by substrate competition with LA and AA for 15-LO-1 and COX enzymes, we incubated these substrates (i.e., LA, AA, SDA, LA + SDA, AA + SDA, EPA, LA + EPA, and AA + EPA) with proteins extracted from untreated LAPC-4 cells and analyzed for metabolites by HPLC analysis (Table 1). No substrate incubations served as controls. The ability of LAPC-4 cells to form 13-HODE from exogenous LA (the preferred substrate of 15-LO-1) and 15-HEPE from exogenous EPA or SDA was used to confirm 15-LO-1 activity in the LAPC-4 cells. Similarly, the formation of prostaglandins from LA, AA, SDA, and EPA confirmed COX activity (Table 1). This result also demonstrated the ability of the LAPC-4 cells to convert LA to AA through the desaturase/elongase pathway (Tables 1 and 2). The absence or undetectable amount of 15-HETE indicated either a deficiency in 15-LO-2 enzyme or poor 15-LO-1/AA metabolism. Note that, although 15-LO-1 can also convert AA to 15-(S)-HETE, AA remains to be a poor substrate. Importantly, these results also suggest that the ω-3 fatty acids SDA and EPA did not inhibit either 15-LO-1 or COX activities. On addition of SDA or EPA to the protein extracts containing LA, we observed an approximately 0.5-fold decrease in the formation of 13-HODE metabolite (1.98 ± 0.11 vs 0.92 ± 0.06, P < .01; or 1.98 ± 0.11 vs 0.87 ± 0.03, P < .01). We did not observe a statistically significant difference in the formation of 15-HEPE metabolite with SDA alone versus LA + SDA and AA + SDA (P = .4). A similar observation (P = .07) was noted with EPA alone versus LA + EPA and AA + EPA, although we observed a 1.5-fold increase in the 15-HEPE metabolite with EPA, suggesting that, among EPA and SDA, EPA is the preferred substrate and that both EPA and SDA competed equally with LA for 15-LO-1 enzyme activity. Lastly, we did not observe dramatic differences in prostaglandin formation. These observations provided evidence that ω-3 EPA and SDA inhibited LAPC-4 cell growth by substrate competition with LA and AA for 15-LO-1 and COX enzymes and are both comparable in their actions. Although the levels of prostaglandins remained significantly unaltered, we did not analyze the spectrum of prostaglandins formed because it is reasonable to assume that the composition of individual prostaglandins might very well be different (e.g., a shift from PGE2 to PGE3,).
Table 1.
Enzyme (15-LO-1 and COX) Activity Profiles of LA, AA, SDA, LA + SDA, AA + SDA, EPA, LA + EPA, and AA + EPA Metabolite Products from LAPC-4 Cells Are Measured as Described in the Materials and Methods Section.
| Substrates | Products* | |||
| 13-HODE | 15-HETE | 15-HEPE | Total prostaglandins | |
| LA | 1.98 ± 0.11 | ND | 0 | 6.15 ± 0.32 |
| AA | ND | ND | 0 | 9.23 ± 0.77 |
| SDA | ND | ND | 0.82 ± 0.04 | 4.74 ± 0.14 |
| LA + SDA | 0.92 ± 0.06 | ND | 0.76 ± 0.03 | 5.15 ± 0.12 |
| AA + SDA | ND | ND | 0.80 ± 0.01 | 7.90 ± 0.19 |
| EPA | ND | ND | 1.77 ± 0.05 | 5.34 ± 0.14 |
| LA + EPA | 0.87 ± 0.03 | ND | 1.21 ± 0.03 | 4.75 ± 0.12 |
| AA + EPA | ND | ND | 1.43 ± 0.01 | 7.61 ± 0.23 |
ND, not detectable.
Percent conversion (products) data represent the mean ± SD of triplicate determinations from two separate experiments.
Estimated Enzyme Activities of the LA and AA Pathways and Modulation by EPA in LAPC-4 Cells
To obtain additional evidence to support the hypothesis of EPA modulation in tumorigenesis, we examined percent unsaturated or percent saturated fatty acids in total phospholipids for PUFA ω-6:ω-3 ratios and for the major enzymes of the ω-6 catabolic pathway (by estimating product-to-precursor ratios of the percentages of individual fatty acids) (namely, elongase, Δ-5-desaturase, and Δ-6-desaturase) and the ω-9 anabolic fatty acid pathway enzyme Δ-9 desaturase in LAPC-4 cells grown in vitro with and without LA, AA, or EPA (Table 2). There were no apparent differences observed in either the percent unsaturated or the percent saturated fatty acids in the total phospholipids, suggesting that the cells maintained the membrane fluidity and functionality of proteins in the membrane. As shown in Table 2, we observed a 2.6-fold increase in ω-6:ω-3 ratio with LA, a 1.7-fold increase with AA, and a 3.7-fold decrease with EPA, compared to untreated control. Furthermore, EPA addition caused a 4.3-fold decrease in ω-6:ω-3 ratio when the cells were grown in the presence of LA compared to only LA-treated LAPC-4 cells. Similarly, we also observed a 4.3-fold decrease in ω-6:ω-3 ratio in the presence of AA + EPA compared to AA-treated LAPC-4 cells. In view of the assumed significance of lipid metabolism in PCa in connection with enzymes of the ω-6 and ω-3 metabolic pathways, the increased estimated activity of Δ-6-desaturase enzyme in the LAPC-4 cells treated with EPA alone or in the presence of LA or AA compared to untreated control, LA-treated, or AA-treated LAPC-4 cells may be associated with accumulation of antiproliferative GLA and DGLA. Similarly, a reduced estimated Δ-5-desaturase activity suggested that EPA may be inhibiting Δ-5-desaturase enzyme activity, which can then further limit the formation of DHA as well as cause accumulation of GLA and DGLA. Interestingly, the estimated activity of the anabolic ω-9 monounsaturated fatty acid pathway enzyme Δ-9-desaturase decreased with LA and AA supplemented in the growth medium, but remained unaltered in the presence of EPA, suggesting that EPA may favor the conversion of stearic acid (18:0, ω-9) to oleic acid (18:1, ω-9); this conversion is otherwise inhibited by either LA and/or AA. These observations provide additional support for the role of EPA in slowing PCa growth.
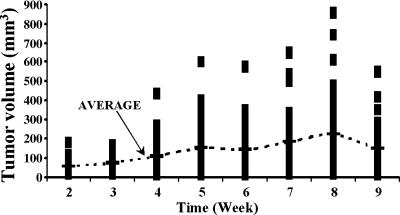
MSRP and the Effect of Isocaloric Diets on Mice Weight and Tumor Development
To confirm the observed in vitro effects of ω-3 fatty acids, these experiments focused on the in vivo effects of ω-6 and ω-3 diets on tumor formation and tumor characteristics using the MSRP (Figure 4). This model relies on athymic mice injected with a PCa cell line, LAPC-4, to induce prostate tumors and tests the efficacy of EPA in slowing prostate tumor progression and recurrence. LAPC-4 cells produce PSA, possess a wild-type androgen receptor, and show features of hormone-dependent growth and metastasis, thus closely resembling proliferating (neoplastic) epithelial cells of a prostate. We are aware that this mouse model may not be an adequate model of clinical cancer, especially with regard to metastasis. However, considering the ease of mimicking radical prostatectomy by surgically removing the tumors from mice and then randomly assigning to the different diet groups, we were assured of an outcome on tumor recurrence based specifically on different diets (Figure 4 and Table 3). After LAPC-4 cell implantation, the mice (n = 72) continued on a no-fat diet for the first 9 weeks (Figure 4). Note that only LA and SDA diets (not the no-fat diet) were isocaloric. The average kilocalories consumed during that time period were 100 kcal/week (data not shown). The feeding method used in the present study successfully maintained equivalent mouse weights throughout the study, although isocaloric intakes among the different diet groups varied, particularly in LA diet-fed mice. Ten- to 20-kcal variations in isocaloric intakes (SDA versus LA, and SDA versus no-fat) were not statistically significant (data not shown). This was a critical element, given that animal studies with consumption of a calorie-dense diet are reported to promote weight gain and prostate tumor growth, and caloric restriction results in decreased tumor growth. All mice developed tumors from weeks 2 to 8 and plateaued on week 9; the average tumor size grew four-fold (Figure 5). On week 9, the tumors from the mice were surgically removed, the skin was sutured, and the mice were allowed to recover overnight. The mice were then randomly assigned (n = 24 per diet group) to LA, SDA, and no-fat diet groups and monitored for PSA recurrence, if any.
Figure 5.
Average tumor volume per week in experimental mice. Average tumor volume (mm3; dotted line) per mouse was examined every week up to week 9 (before tumor resection) in the no-fat diet group (n = 72).
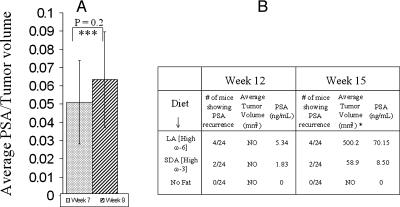
Effect of Diet on PSA, Tumor Size, and Tumor Recurrence
To examine the effects of specific diets on tumor size and recurrence after tumor removal, serum from mice was collected on week 1 (PSA undetectable and data not shown), weeks 7 and 9 (Figure 6A), and weeks 12 and 15 (Figure 6B), and assayed using an ELISA specific for human serum PSA. We observed that the average PSA per tumor volume in mice on week 9 vs week 7 was not significantly different (Figure 6A; P = .2), suggesting that the PSA level in tumors of no-fat diet-fed mice remains unaffected during that time period. Next, we observed 5.34 ng/ml PSA in 4 of 24 (?16% recurred) mice on week 12 in LA (high ω-6) diet-fed mice and 1.83 ng/ml PSA in 2 of 24 (?8.3% recurred) in SDA (high ω-3) diet-fed mice; neither tumor nor PSA was observed/detected in the no-fat diet-fed group (Figure 6B). These observations suggested that, although no palpable tumors were observed in either of the groups on week 12, rapid tumor recurrence had occurred in LA diet-fed mice compared to the SDA diet-fed mice. However, on week 15, palpable tumors were detected. Although the number of mice with tumors and those that were positive for PSA remained the same as in week 12, strikingly, the size of the tumors in the SDA diet-fed mice was eight-fold smaller in size compared with those in the LA diet-fed mice, and the levels of PSA examined corresponded to tumor size (70.15 ng/ml PSA in LA diet-fed mice vs 8.50 ng/ml PSA in SDA diet-fed mice) accordingly (Figure 6B). These results suggested that tumor recurrence was 50% reduced in SDA diet-fed mice than in LA diet-fed mice (from 16% to 8%). Although PSA velocity could not be determined, interestingly, PSA doubling time decreased by ≈ 1.5-fold in recurrent tumors of SDA diet-fed mice versus LA diet-fed mice.
Figure 6.
(A) Average PSA per tumor volume in the no-fat diet-fed mice on week 7 vs week 9 (n = 72). ***P = .2. (B) Number of mice showing tumor recurrence, average tumor volume, and PSA, after tumor resection, in mice fed no-fat, high ω-3 SDA, and high ω-6 LA diets on week 12 vs week 15. NO, not observed. *Estimated value.
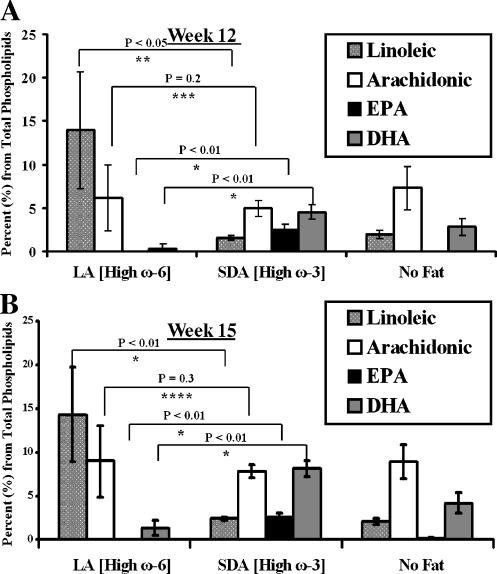
Effect of Diet on Total Red Blood Cell (RBC) Phospholipids
In order for the in vivo experiments to accurately assess the effects of diet on PCa, the ω-6:ω-3 fatty acids ratios normally found in individuals must be recapitulated in the mice. We chose to examine whether the LA, SDA, and no-fat diets modulated ω-6:ω-3 ratios by evaluating mouse RBC phospholipids because RBCs are responsive to diet and appear to accurately reflect long-term dietary intake for many of the fatty acids, particularly the n-3 long-chain PUFA [45,46]. Furthermore, the distribution of fatty acids in RBC membranes has been validated as an accurate estimate of the distribution of fatty acids in the diet [47–52]. An additional theoretical advantage is that phospholipid fatty acids probably represent the most pertinent cell membrane component in tissues (i.e., prostate), and there appears to be a continuous exchange of dietary fats among various blood compartments [46–49]. As shown in Figure 7, A and B, there were statistically significant differences in the composition of LA, EPA, and DHA in the RBC phospholipids measured (AA was not statistically different) in ω-6 LA and ω-3-SDA diet groups on weeks 12 and 15, respectively. Drastic differences were not observed in the total LA, AA, EPA, and DHA composition in phospholipids from reticulocytes harvested on week 12 vs week 15. Similarly, the LA, AA, EPA, and DHA compositions in tumor phospholipids on week 15 (from LA diet- and SDA diet-fed mice) were comparable to those observed from reticulocytes (data not shown). Furthermore, the ω-6 (LA and AA):ω-3 (EPA and DHA) ratios were 17–20:1 in LA diet-fed, 1:1 in SDA diet-fed, and 5:1 in no-fat diet-fed mice, respectively. These data suggest that the phospholipids in RBCs are responsive to diet, represent phospholipids in tumor tissues, and remain practically constant by week 12.
Figure 7.
Composition of LA, AA, EPA, and DHA in erythrocyte phospholipids (n = 3) from mice fed no-fat, high ω-3 SDA, and high ω-6 LA diets on (A) week 12 vs (B) week 15. Fatty acid methyl esters from erythrocytes were analyzed by gas liquid chromatography, as described in Materials and Methods section. The fatty acids are expressed as percentages of total phospholipids. *P < .01, **P < .05, ***P = .2, ****P = .3.
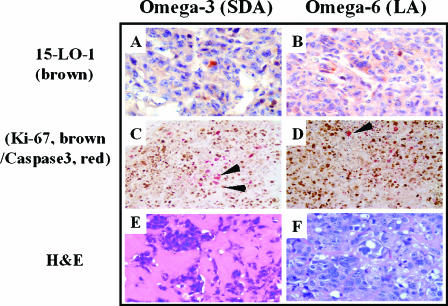
Effect of Diet on Proliferation and Apoptotic Indices in Recurrent Tumors
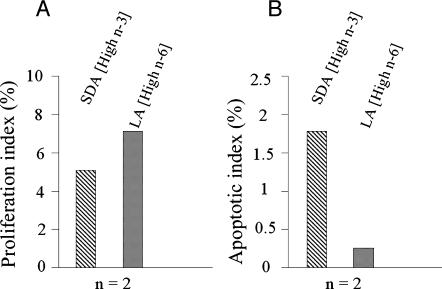
To examine the in vivo effects of ω-3 and ω-6 fat diets on the rate of tumor recurrence (slow versus fast tumor growth), we next evaluated, by immunohistochemistry, proliferation status (Ki-67) and apoptosis (Caspase-3) in tumors from mice fed LA and SDA diets (n = 2). As depicted in Figures 8 and 9, although 15-LO-1 protein levels remained similar, Ki-67 expression and the calculated percent proliferation index increased in tumors from mice fed the ω-6 diet when compared to tumors from mice fed the ω-3 SDA diet. Furthermore, increased apoptosis was observed in tumors of ω-3 SDA diet-fed mice versus tumors from ω-6 diet-fed mice. These results suggest that, although differences in percent proliferation index were observed in both diet groups, ω-3 EPA dramatically modulated the percent apoptotic index in tumor cells (Figure 9).
Figure 8.
Representative immunostaining (A–D) and hematoxylin and eosin (H&E) staining (E and F) of tumors from mice fed high ω-3 SDA and high ω-6 LA diets on week 15 with polyclonal antibody for 15-LO-1 (brown), dual staining with Ki-67 (brown) as a proliferation marker, and caspase-3 (red; arrowheads) as an apoptosis marker (x40). ω-3 SDA (A, C, and E) and ω-3 SDA (B, D, and F). (A and B) 15-LO-1; (C and D) dual Ki-67/caspase-3; (E and F) H&E staining.
Figure 9.
Assessment of (A) proliferation index and (B) apoptotic index in recurrent tumors on week 15 from mice fed high ω-3 SDA (n = 2) and high ω-6 LA diets (n = 2). Sections of formalin-fixed paraffin-embedded LAPC-4 tumor tissues were tested for the presence of 15-LO-1, Ki-67, and caspase-3. Proliferation and apoptotic indices (%) were estimated as described in Materials and Methods section.
Discussion
International incidence patterns and migrations studies, epidemiological data, and animal and in vitro studies indicate that consuming a diet rich in fat increases the risk for developing PCa. For example, a wide variation in international PCa mortality rates exists; rates are particularly high in Northern Europe and North America, whereas they are much lower in Japan and other Asian countries [2]. In contrast, the frequency of latent carcinoma of the prostate diagnosed at autopsy is as common in Japanese males as in the male population of the United States, Canada, and UK [3]. These findings implicate environmental variables, such as diet, as a significant contributing factor. Indeed, immigrants from Poland and Japan, where the incidence of PCa is low, exhibit a significant increase in the risk for developing PCa after moving to the United States [4–7]. Shennen and Bishop [5] reported a positive relationship between the consumption of dietary fats, including PUFAs, and the development of PCa in 32 countries. Moreover, regional consumption of high-fat foods in the United States parallels that of mortality from PCa [3–6]. Although all mammalian cells can interconvert ω-6 and ω-3 PUFAs within each series by elongation, desaturation, and retroconversion, the two series are not interchangeable.
Our previous in vitro and in vivo studies demonstrating the presence of ω-6 LA-metabolizing enzyme 15-LO-1 at higher levels in PCa compared to that in the normal epithelium, and the correlation between expression and Gleason grade suggested that 15-LO-1 is a key enzyme that contributes to the initiation and development of the neoplastic phenotype in PCa [17,18,22,23]. Based on the current study and other reports supporting our observations, we propose a mechanistic approach as to how the metabolites of antitumorigenic ω-3 fatty acids can modulate the protumorigenic ω-6 LA and AA enzymatic pathways (Figure 10). An important finding in the present study using the mouse xenograft model mimicking prostatectomy for studying recurrence (biochemical failure) is that the ω-3 diet-fed mice demonstrated slower LAPC-4 tumor recurrence and PSA doubling time, relative to mice fed an ω-6 diet. This study attempts to clarify the roles of ω-3 fatty acids that promote apoptosis and decrease proliferation in cancer cells likely by competing with the enzymes of the LA and AA pathways (15-LO-1 and COX). Therefore, the use of dietary ω-3 PUFAs as agents for cancer prevention can prove to be a valuable strategy in the fight against PCa [53–62] and recurrence. Our observations confirmed that LAPC-4 cells expressed active 15-LO-1 and COX enzymes and that LA and AA fatty acids were pro-proliferative in their actions in vitro. A mixture of DHA + EPA mimicking fish oil was the most effective nontoxic in vitro growth inhibitor, compared to EPA alone, toward LAPC-4 proliferation even in the presence of LA or AA. This result supports a previous observation on the effects of ω-3 and ω-6 fatty acids on the growth of PCa cells [63] and provides explanations for the previously conducted studies evaluating fish oils as well as flaxseeds in PCa intervention trials that have yielded confounding results (reviewed in Ref. [64]).
Figure 10.
Modulation of the enzymes of the LA and AA pathways by ω-3 and ω-6 fatty acids.
In addition to 15-LO-1, evidence also suggests that other metabolic enzymes play important roles in PCa pathobiology. AA obtained through diet or LA metabolic conversion is the preferred substrate for 15-lipoxygenase-2 (15-LO-2). 15-LO-2 converts AA to 15-(S)-HETE, a metabolite shown to both enhance apoptosis and act as a negative cell cycle regulator [65]. Furthermore, 15-(S)-HETE has anti-inflammatory properties [66,67], and studies support an association between inflammation and PCa [68,69]. However, PCa tissue or LAPC-4 cells (this study) express very little 15-LO-2 [70]. Similarly, AA also acts as a substrate for COX-2, leading to the production of prostaglandins, such as PGE2, that have proinflammatory effects and thus possibly contribute to PCa pathobiology. Although the present study did not specifically evaluate both COX-1 and COX-2 levels for prostaglandins such as PGE2 versus PGE3, previous studies have demonstrated overexpression of COX-2 [36,37] and an antitumorigenic role of PGE3 in PCa [39]. Therefore, due to the abundance of COX-2 in PCa tissues, it was reasonable to assume that the vast majority of AA in LAPC-4 cells would be converted to PGE2 if ω-3 were low or absent.
Previous studies suggest that the high incidence of PCa in Americans may, in part, result from an imbalance in the ω-3:ω-6 PUFA ratio [3,4]. Ideally, the ω-3:ω-6 PUFA ratio in the human body should be 1:4 to 1:1 [71]. The typical US diet is low in ω-3 and high in ω-6, and many individuals contain 10 to 20 times more ω-6 PUFAs than ω-3 PUFAs [72–74]. Although an increase in the ω-6:ω-3 ratio with LA and AA compared to untreated control was evident, the addition of EPA to LAPC-4 cells in the presence of LA or AA in vitro or in mice fed the SDA diet was able to maintain the desirable ω-6:ω-3 ratio of ≈1 and 2. Therefore, for PCa intervention, it is reasonable to consume excess nontoxic EPA and to facilitate the production of antitumorigenic metabolites to counteract the production of protumorigenic metabolites derived from ω-6 fatty acid pathways. In the present study, we used isocaloric fats, providing diets with 4.4 kcal/g. Short-term human trials using 5.4 to 15 g/day ω-3 PUFA, to balance 13 g/day ω-6 [72–74], were harmless [75,76].
Consequently, 15-LO-1 metabolizes EPA to 15-HEPE [39], a metabolite shown to have antitumorigenic properties, whereas COX-2 metabolizes EPA to the anti-inflammatory as well as antitumorigenic prostaglandin PGE3 [39–41]. Therefore, based on the substrates (i.e., dietary ω-6 or ω-3 in concert with the activities of 15-LO-1 and COXs), cells can be predisposed to either a proliferative or an antiproliferative outcome. This effect seemed to be independent of percent unsaturated or percent saturated fatty acids in the total phospholipids, as observed in LAPC-4 cells treated with either ω-6 or ω-3 fatty acids, because the cells are able to maintain the fluidity and functionality of proteins in the membrane. Thus, the present study suggests that there is a link between PUFA lipid metabolism in the PCa and the fate of carcinogenesis, which is based on the balance between ω-6 and ω-3 PUFAs and their respective metabolic pathways.
The first and rate-limiting step in the shared ω-3 and ω-6 metabolic pathways, besides 15-LO-1, is also catalyzed by Δ-6-desaturase (Figure 10). On one hand, the increased estimated activity of Δ-6-desaturase enzyme in the LAPC-4 cells treated with EPA alone or in the presence of LA or AA, compared to untreated control, indicated an accumulation of antiproliferative GLA and DGLA. However, a reduced estimated Δ-5-desaturase activity suggested that EPA could inhibit Δ-5-desaturase enzyme activity, which eventually limits the formation of DHA and also causes accumulation of antitumorigenic DGLA and GLA. Interestingly, the estimated activity of ω-9 monounsaturated fatty acid pathway enzyme Δ-9-desaturase decreased with LA and AA supplemented in the growth medium, but was not affected in the presence of EPA, suggesting that EPA may favor the conversion of stearic acid (18:0, ω-9) to oleic acid (18:1, ω-9), which is otherwise inhibited by either LA and/or AA.
Based on the current study, we propose that, due to low Δ-6 desaturase in cancer cells, their ability to convert either ω-6 LA to GLA or to convert ω-3 α-linolenic acid (ALA) to SDA, EPA, and DHA is severely limited. Cancer cells thus have very low levels of GLA, DGLA, SDA, DHA, and EPA, and, although ALA may accumulate, it is not converted to SDA [77–84]; therefore, 15-LO-1 activity leading to pro-proliferative actions probably through IGF-1 supports carcinogenesis [85]. Consequently, it is conceivable that, without examining for 15-LO-1, studies evaluating a mixture of ω-3 PUFAs, as found in fish oils in PCa intervention trials, can yield confounding results (reviewed in Ref. [64]). Of note is that an age-related decrease in Δ-6 desaturase activity corresponded with both low EPA and high ALA and LA concentrations in rats [78], suggesting the possibility that similar effects are possible in aged humans, causing diseased prostate tissues that are unable to convert sufficient quantities of antiproliferative ω-3 ALA to EPA. Importantly, US diets provide excessive LA [14], and LA competes with ALA for the desaturase and elongase enzymes, thus inhibiting the conversion of ALA to EPA and DHA.
Epigenetic effects of high-fat PUFAs on gene expressions of enzymes from the ω-3 and ω-6 pathways are unknown, and possible mechanisms may involve DNA methylation of promoters or the presence of transcriptional inhibitors—studies that may require more research in the future. Using LAPC-4 cells, an isocaloric low-fat diet slowed LAPC-4 tumor growth, further corroborating a role for fats in PCa development [8,9]. Although this observation and our current study both suggest that a no-fat diet may be the most beneficial diet to radical prostatectomy patients, compliance with a no-fat diet would likely not be feasible in long-term clinical trials. Combining a reduction of dietary ω-6 fat with an intake of essential ω-3 fatty acids likely would be more attainable and, thus, more beneficial.
PSA doubling time is the most powerful predictor of progression, stratifying patients with biochemical failure into high- and low-risk groups for clinical failure [86,87]. Our study suggests that ω-3 SDA caused a reduction in PSA doubling time that was exacerbated by ω-6 LA. Although a clinical trial will demonstrate its usefulness, the use of natural dietary ω-3 supplementation after radical prostatectomy could potentially be useful in improving biochemical progression-free survival and local control in patients with a high risk of progression. In conclusion, due to the probable impact of ω-3 and ω-6 PUFAs on PCa development, our results strongly support a dietary intervention role for ω-3 PUFAs as adjunct therapy in the prevention and treatment of PCa.
Acknowledgements
We thank Brian Philips and Malabika Sen for critically reading the manuscript.
Abbreviations
- 5-LO-1
15-lipoxygenase-1
- AA
arachidonic acid
- COX
cyclooxygenase
- HETE
hydroxyeicosatetraenoic acid
- HODE
hydroxyoctadecadienoic acid
- LO
lipoxygenase
- LA
linoleic acid
- MSRP
mouse model to simulate radical prostatectomy
- LAPC-4
Los Angeles Prostate Cancer-4
- PUFA
polyunsaturated fatty acid
- PSA
prostate-specific antigen
Footnotes
This work was supported, in part, by American Cancer Society grant RSG-03-022-01 to U.P.K.
References
- 1.Shappell SB, Thomas GV, Roberts RL, Herbert R, Ittmann MM, Rubin MA, Humphrey PA, Sundberg JP, Rozengurt N, Barrios R, et al. Prostate pathology of genetically engineered mice: definitions and classification. The consensus report from the Bar Harbor meeting of the Mouse Models of Human Cancer Consortium Prostate Pathology Committee. Cancer Res. 2004;64:2270–2305. doi: 10.1158/0008-5472.can-03-0946. [DOI] [PubMed] [Google Scholar]
- 2.Breslow N, Chan CW, Dhom G, Drury RA, Franks LM, Gellei B, Lee YS, Lundberg S, Sparke B, Sternby NH, et al. Latent carcinoma of prostate at autopsy in seven areas. The International Agency for Research on Cancer, Lyons, France. Int J Cancer. 1977;20:680–688. doi: 10.1002/ijc.2910200506. [DOI] [PubMed] [Google Scholar]
- 3.Dunn JE. Cancer epidemiology in populations of the United States—with emphasis on Hawaii and California—and Japan. Cancer Res. 1975;35:3240–3245. [PubMed] [Google Scholar]
- 4.Haenszel W, Kurihara M. Studies of Japanese migrants: I. Mortality from cancer and other diseases among Japanese in the United States. J Natl Cancer Inst. 1968;40:43–68. [PubMed] [Google Scholar]
- 5.Shennen DH, Bishop OS. Diet and mortality from malignant disease in 32 countries. West Indian Med J. 1974;23:44. [PubMed] [Google Scholar]
- 6.Blair A, Fraumeni JF. Geographic patterns of prostate cancer in the United States. J Natl Cancer Inst. 1978;61:1379–1384. [PubMed] [Google Scholar]
- 7.Armstrong B, Doll R. Environmental factors and cancer incidence and mortality in different countries, with special reference to dietary practices. Int J Cancer. 1975;15:617–631. doi: 10.1002/ijc.2910150411. [DOI] [PubMed] [Google Scholar]
- 8.Ngo TH, Barnard RJ, Cohen P, Freedland S, Tran C, deGregorio F, Elshimali YI, Heber D, Aronson WJ. Effect of isocaloric low-fat diet on human LAPC-4 prostate cancer xenografts in severe combined immunodeficient mice and the insulin-like growth factor axis. Clin Cancer Res. 2003;9:2734–2743. [PubMed] [Google Scholar]
- 9.Ngo TH, Barnard RJ, Anton T, Tran C, Elashoff D, Heber D, Freedland SJ, Aronson WJ. Effect of isocaloric low-fat diet on prostate cancer xenograft progression to androgen independence. Cancer Res. 2004;64:1252–1254. doi: 10.1158/0008-5472.can-03-3830. [DOI] [PubMed] [Google Scholar]
- 10.Kang JX, Wang J, Wu L, Kang ZB. Transgenic mice: fat-1 mice convert n-6 to n-3 fatty acids. Nature. 2004;427:504. doi: 10.1038/427504a. [DOI] [PubMed] [Google Scholar]
- 11.Crawford MA. The role of dietary fatty acids in biology: their place in the evolution of the human brain. Nutr Rev. 1992;50:3–11. doi: 10.1111/j.1753-4887.1992.tb01283.x. [DOI] [PubMed] [Google Scholar]
- 12.Norrish AE, Skeaff CM, Arribas GL, Sharpe SJ, Jackson RT. Prostate cancer risk and consumption of fish oils: a dietary biomarker-based case-control study. Br J Cancer. 1999;81:1238–1242. doi: 10.1038/sj.bjc.6690835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emken EA, Adlof RO, Gulley RM. Dietary linoleic acid influences desaturation and acylation of deuterium-labeled linoleic and ALAs in young adult males. Biochim Biophys Acta. 1994;1213:277–288. doi: 10.1016/0005-2760(94)00054-9. [DOI] [PubMed] [Google Scholar]
- 14.Willett WC. Specific fatty acids and risks of breast and prostate cancer: dietary intake. Am J Clin Nutr. 1997;66:1557S–1563S. doi: 10.1093/ajcn/66.6.1557S. [DOI] [PubMed] [Google Scholar]
- 15.Iynem AH, Alademir AZ, Obek C, Kural AR, Konukoglu D, Akcay T. The effect of prostate cancer and antiandrogenic therapy on lipid peroxidation and antioxidant systems. Int Urol Nephrol. 2004;36:57–62. doi: 10.1023/b:urol.0000032676.31470.b2. [DOI] [PubMed] [Google Scholar]
- 16.Gupta S, Srivastava M, Ahmad N, Sakamoto K, Bostwick DG, Mukhtar H. Lipoxygenase-5 is overexpressed in prostate adenocarcinoma. Cancer. 2001;91:737–743. doi: 10.1002/1097-0142(20010215)91:4<737::aid-cncr1059>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 17.Kelavkar UP, Cohen C, Kamitani H, Eling TE, Badr KF. Concordant induction of 15-lipoxygenase-1 and mutant p53 expression in human prostate adenocarcinoma: correlation with Gleason staging. Carcinogenesis. 2000;10:1777–1787. doi: 10.1093/carcin/21.10.1777. [DOI] [PubMed] [Google Scholar]
- 18.Kelavkar U, Glasgow W, Eling T. The effect of 15-lipoxygenase-1 (15-LO-1) expression on cancer cells. Curr Urol Rep. 2002;3:207–214. doi: 10.1007/s11934-002-0066-8. [DOI] [PubMed] [Google Scholar]
- 19.Donaldson MS. Nutrition and cancer: a review of the evidence for an anti-cancer diet. Nutr J. 2004;3:19–27. doi: 10.1186/1475-2891-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fukatsu T, et al. Genetic polymorphisms of hormone-related genes and prostate cancer risk in the Japanese population. Anticancer Res. 2004;24:2431–2437. [PubMed] [Google Scholar]
- 21.Kasper S. Survey of genetically engineered mouse models for prostate cancer: analyzing the molecular basis of prostate cancer development, progression, and metastasis. J Cell Biochem. 2005;94:279–297. doi: 10.1002/jcb.20339. [DOI] [PubMed] [Google Scholar]
- 22.Kelavkar U, Nixon J, Cohen C, Dillehay D, Eling T, Badr K. Overexpression of 15-lipoxygenase-1 (15-LO-1) in PC-3 human prostate cancer cells causes aggressive tumorigenesis. Carcinogenesis. 2001;22:1765–1773. doi: 10.1093/carcin/22.11.1765. [DOI] [PubMed] [Google Scholar]
- 23.Kelavkar UP, Cohen C. 15-Lipoxygenase-1 expression up-regulates and activates insulin-like growth factor-1 receptor in prostate cancer cells. Neoplasia. 2004;6:41–52. doi: 10.1016/s1476-5586(04)80052-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kamitani H, Geller M, Eling T. Expression of 15-lipoxygenase by human colorectal carcinoma Caco-2 cells during apoptosis and cell differentiation. J Biol Chem. 1998;273:21569–21577. doi: 10.1074/jbc.273.34.21569. [DOI] [PubMed] [Google Scholar]
- 25.Glasgow WC, Afshari CA, Barrett JC, Eling TE. Modulation of the epidermal growth factor mitogenic response by metabolites of linoleic and arachidonic acid in Syrian hamster embryo fibroblasts. Differential effects in tumor suppressor gene (+) and (-) phenotypes. J Biol Chem. 1992;267:10771–10779. [PubMed] [Google Scholar]
- 26.Sauer LA, Dauchy RT, Blask DE, Armstrong BJ, Scalici S. 13-Hydroxyoctadecadienoic acid is the mitogenic signal for linoleic acid-dependent growth in rat hepatoma 7288CTC in vivo. Cancer Res. 1999;59:4688–4692. [PubMed] [Google Scholar]
- 27.Blask DE, Sauer LA, Dauchy RT, Holowachuk EW, Ruhoff MS, Kopff HS. Melatonin inhibition of cancer growth in vivo involves suppression of tumor fatty acid metabolism via melatonin receptor-mediated signal transduction events. Cancer Res. 1999;59:4693–4701. [PubMed] [Google Scholar]
- 28.Blask DE, Dauchy RT, Sauer LA, Krause JA. Melatonin uptake and growth prevention in rat hepatoma 7288CTC in response to dietary melatonin: melatonin receptor-mediated inhibition of tumor linoleic acid metabolism to the growth signaling molecule 13-hydroxyoctadecadienoic acid and the potential role of phytomelatonin. Carcinogenesis. 2004;25:951–960. doi: 10.1093/carcin/bgh090. [DOI] [PubMed] [Google Scholar]
- 29.Coleman KE, Kelavkar UP, Lawson D, Haseman J, Cohen C. 15-Lipoxygenase-1 (15-LO-1) as a molecular marker in cancer: an immunohistochemical study. Mod Pathol. 2002;15:304A. [Google Scholar]
- 30.Shureiqi I, et al. Decreased 13-S-hydroxyoctadecadienoic acid levels and 15-lipoxygenase-1 expression in human colon cancers. Carcinogenesis. 1999;20:1985–1995. doi: 10.1093/carcin/20.10.1985. [DOI] [PubMed] [Google Scholar]
- 31.Hsi LC, Xi X, Lotan R, Shureiqi I, Lippman SM. The histone deacetylase inhibitor suberoylanilide hydroxamic acid induces apoptosis via induction of 15-lipoxygenase-1 in colorectal cancer cells. Cancer Res. 2004;64:8778–8781. doi: 10.1158/0008-5472.CAN-04-1867. [DOI] [PubMed] [Google Scholar]
- 32.Kelavkar UP, Glasgow W, Olson SJ, Foster BA, Shappell SB. Overexpression of 12/15-lipoxygenase, an ortholog of human 15-lipoxygenase-1, in the prostate tumors of TRAMP mice. Neoplasia. 2004;6:821–830. doi: 10.1593/neo.04286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wechter WJ, Leipold DD, Murray ED, Jr, Quiggle D, McCracken JD, Barrios RS, Greenberg NM. E-7869 (R-flurbiprofen) inhibits progression of prostate cancer in the TRAMP mouse. Cancer Res. 2000;60:2203–2208. [PubMed] [Google Scholar]
- 34.Brash AR. Lipoxygenases: occurrence, functions, catalysis, and acquisition of substrate. J Biol Chem. 1999;274:23679–23682. doi: 10.1074/jbc.274.34.23679. [DOI] [PubMed] [Google Scholar]
- 35.Wang W, Bergh A, Damber JE. Cyclooxygenase-2 expression correlates with local chronic inflammation and tumor neovascularization in human prostate cancer. Clin Cancer Res. 2005;11:3250–3256. doi: 10.1158/1078-0432.CCR-04-2405. [DOI] [PubMed] [Google Scholar]
- 36.O'Neill GP, Ford-Hutchinson AW. Expression of mRNA for cyclooxygenase-1 and cyclooxygenase-2 in human tissues. FEBS Lett. 1993;330:156–160. doi: 10.1016/0014-5793(93)80263-t. [DOI] [PubMed] [Google Scholar]
- 37.Hussain T, Gupta S, Mukhtar H. Cyclooxygenase-2 and prostate carcinogenesis. Cancer Lett. 2003;191:125–135. doi: 10.1016/s0304-3835(02)00524-4. [DOI] [PubMed] [Google Scholar]
- 38.Narayanan NK, Narayanan BA, Reddy BS. A combination of docosahexaenoic acid and celecoxib prevents prostate cancer cell growth in vitro and is associated with modulation of nuclear factor-kappaB, and steroid hormone receptors. Int J Oncol. 2005;26:785–792. [PubMed] [Google Scholar]
- 39.Hughes-Fulford M, Chen Y, Tjandrawinata RR. Fatty acid regulates gene expression and growth of human prostate cancer PC-3 cells. Carcinogenesis. 2001;22:701–707. doi: 10.1093/carcin/22.5.701. [DOI] [PubMed] [Google Scholar]
- 40.Bagga D, Wang L, Farias-Eisner R, Glaspy JA, Reddy ST. Differential effects of prostaglandin derived from omega-6 and omega-3 polyunsaturated fatty acids on COX-2 expression and IL-6 secretion. Proc Natl Acad Sci USA. 2003;100:1751–1756. doi: 10.1073/pnas.0334211100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Serhan CN, Clish CB, Brannon J, Colgan SP, Chiang N, Gronert K. Novel functional sets of lipid-derived mediators with antiinflammatory actions generated from omega-3 fatty acids via cyclooxygenase 2 nonsteroidal antiinflammatory drugs and transcellular processing. J Exp Med. 2000;192:1197–1204. doi: 10.1084/jem.192.8.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Andersson A, Sjödin A, Hedman A, Olsson R, Vessby B. Fatty acid profile of skeletal muscle phospholipids in trained and untrained young men. Am J Physiol Endocrinol Metab. 2000;279:E744–E751. doi: 10.1152/ajpendo.2000.279.4.E744. [DOI] [PubMed] [Google Scholar]
- 43.Ursin VM. Modification of plant lipids for human health: development of functional land-based omega-3 fatty acids. J Nutr. 2003;133:4271–4274. doi: 10.1093/jn/133.12.4271. [DOI] [PubMed] [Google Scholar]
- 44.Hem A, Smith AJ, Solberg P. Saphenous vein puncture for blood sampling of the mouse, rat, hamster, gerbil, guinea pig, ferret and mink. Lab Anim. 1998;32:364–368. doi: 10.1258/002367798780599866. [DOI] [PubMed] [Google Scholar]
- 45.Balas J, Pawlicka M, Jacorzynski B, Filipek A, Domina P, Mielniczuk E, Daniewski M. The fat and fatty acids content in selected sea fish. Rocz Panstw Zakl Hig. 2001;52:277–284. [PubMed] [Google Scholar]
- 46.Richardson AJ, Easton T, Puri BK. Red cell and plasma fatty acid changes accompanying symptom remission in a patient with schizophrenia treated with eicosapentaenoic acid. Eur Neuropsychopharmacol. 2000;10:189–193. doi: 10.1016/s0924-977x(00)00068-7. [DOI] [PubMed] [Google Scholar]
- 47.Farquhar JW, Ahrens EH. Effects of dietary fats on human erythrocyte fatty acid patterns. J Clin Invest. 1963;42:675–685. doi: 10.1172/JCI104759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yamori Y, Nara Y, Iritani N, Workman RJ, Inagami T. Comparison of serum phospholipid fatty acids among fishing and farming Japanese populations and American inlanders. J Nutr Sci Vitaminol (Tokyo) 1985;31:417–422. doi: 10.3177/jnsv.31.417. [DOI] [PubMed] [Google Scholar]
- 49.Dyerberg J, Bang HO, Hjome N. Fatty acid composition of the plasma lipids in Greenland Eskimos. Am J Clin Nutr. 1975;28:958–966. doi: 10.1093/ajcn/28.9.958. [DOI] [PubMed] [Google Scholar]
- 50.Albert CM, Campos H, Stampfer MJ, Ridker PM, Manson JE, Willett WC, Ma J. Blood levels of long-chain n-3 fatty acids and the risk of sudden death. N Engl J Med. 2002;346:1113–1118. doi: 10.1056/NEJMoa012918. [DOI] [PubMed] [Google Scholar]
- 51.Shepherd IL. Resistance to changes in diet. Proc Nutr Soc. 2002;61:267–272. doi: 10.1079/PNS2002147. [DOI] [PubMed] [Google Scholar]
- 52.Farquhar JW, Ahrens EH. Effects of dietary fats on human erythrocyte fatty acid patterns. J Clin Invest. 1963;42:675–685. doi: 10.1172/JCI104759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee MM, Chang JS, Jacobs B, Wrensch MR. Complementary and alternative medicine use among men with prostate cancer in 4 ethnic populations. Am J Public Health. 2002;92:1606–1609. doi: 10.2105/ajph.92.10.1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sparber A, Bauer L, Curt G, Eisenberg D, Levin T, Parks S, Steinberg SM, Wootton J. Use of complementary medicine by adult patients participating in cancer clinical trials. Oncol Nurs Forum. 1999;27:623–630. [PubMed] [Google Scholar]
- 55.Patterson RE, Neuhouser ML, Hedderson MM, Schwartz SM, Standish LJ, Bowen DJ. Changes in diet, physical activity, and supplement use among adults diagnosed with cancer. J Am Diet Assoc. 2003;103:323–328. doi: 10.1053/jada.2003.50045. [DOI] [PubMed] [Google Scholar]
- 56.Downer SM, Cody MM, McCluskey P, Wilson PD, Arnott SJ, Lister TA, Slevin ML. Pursuit and practice of complementary therapies by cancer patients receiving conventional treatment. BMJ. 1994;309:86–89. doi: 10.1136/bmj.309.6947.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wynder EL, Mabuchi K, Whitmore WF., Jr Epidemiology of cancer of the prostate. Cancer. 1971;28:344–360. doi: 10.1002/1097-0142(197108)28:2<344::aid-cncr2820280214>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 58.Terry P, Lichtenstein P, Feychting M, Ahlbom A, Wolk A. Fatty fish consumption and risk of prostate cancer. Lancet. 2001;357:1764–1766. doi: 10.1016/S0140-6736(00)04889-3. [DOI] [PubMed] [Google Scholar]
- 59.Terry PD, Rohan TE, Wolk A. Intakes of fish and marine fatty acids and the risks of cancers of the breast and prostate and of other hormone-related cancers: a review of the epidemiologic evidence. Am J Clin Nutr. 2003;77:532–543. doi: 10.1093/ajcn/77.3.532. [DOI] [PubMed] [Google Scholar]
- 60.Yang YJ, Lee S Ho, Hong SJ, Chung BC. Comparison of fatty acid profiles in the serum of patients with prostate cancer and benign prostatic hyperplasia. Clin Biochem. 1999;32:405–409. doi: 10.1016/s0009-9120(99)00036-3. [DOI] [PubMed] [Google Scholar]
- 61.Freeman VL, Meydani M, Yong S, Pyle J, Flanigan RC, Waters WB, Wojcik EM. Prostatic levels of fatty acids and the histopathology of localized prostate cancer. J Urol. 2000;164:2168–2172. [PubMed] [Google Scholar]
- 62.Freeman VL, Meydani M, Hur K, Flanigan RC. Inverse association between prostatic polyunsaturated fatty acid and risk of locally advanced prostate carcinoma. Cancer. 2004;101:2744–2754. doi: 10.1002/cncr.20676. [DOI] [PubMed] [Google Scholar]
- 63.Pandalai PK, Pilat MJ, Yamazaki K, Naik H, Pienta KJ. The effects of omega-3 and omega-6 fatty acids on in vitro prostate cancer growth. Anticancer Res. 1996;16:815–820. [PubMed] [Google Scholar]
- 64.Fleshner N, Bagnell PS, Klotz L, Venkateswaran V. Dietary fat and prostate cancer. J Urol. 2004;171:S19–S24. doi: 10.1097/01.ju.0000107838.33623.19. [DOI] [PubMed] [Google Scholar]
- 65.Tang S, et al. Evidence that arachidonate 15-lipoxygenase 2 is a negative cell-cycle regulator in normal prostate epithelial cells. J Biol Chem. 2002;277:16189–16201. doi: 10.1074/jbc.M111936200. [DOI] [PubMed] [Google Scholar]
- 66.Coutant F, Agaugue S, Perrin-Cocon L, Andre P, Lotteau V. Sensing environmental lipids by dendritic cell modulates its function. J Immunol. 2004;172:54–60. doi: 10.4049/jimmunol.172.1.54. [DOI] [PubMed] [Google Scholar]
- 67.Serhan CN, et al. Reduced inflammation and tissue damage in transgenic rabbits overexpressing 15-lipoxygenase and endogenous anti-inflammatory lipid mediators. J Immunol. 2003;171:6856–6865. doi: 10.4049/jimmunol.171.12.6856. [DOI] [PubMed] [Google Scholar]
- 68.Nelson WG, De Marzo AM, DeWeese TL, Isaacs WB. The role of inflammation in the pathogenesis of prostate cancer. J Urol. 2004;172:S6–S11. doi: 10.1097/01.ju.0000142058.99614.ff. [DOI] [PubMed] [Google Scholar]
- 69.Donnell RF. Epidemiology of inflammation and prostate cancer. Curr Urol Rep. 2004;5:297. doi: 10.1007/s11934-004-0053-3. [DOI] [PubMed] [Google Scholar]
- 70.Shappell SB, Boeglin WE, Olson SJ, Kasper S, Brash AR. 15-Lipoxygenase-2 (15-LOX-2) is expressed in benign prostatic epithelium and reduced in prostate adenocarcinoma. Am J Pathol. 1999;155:235–245. doi: 10.1016/S0002-9440(10)65117-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Simopoulos AP, Leaf A, Salem N. Essentiality of and recommended dietary intakes for omega-6 and omega-3 fatty acids. Ann Nutr Metab. 1999;43:127–130. doi: 10.1159/000012777. [DOI] [PubMed] [Google Scholar]
- 72.Kris-Etherton PM, Taylor DS, Yu-Poth S, Huth P, Moriarty K, Fishell V, Hargrove RL, Zhao G, Etherton TD. Polyunsaturated fatty acids in the food chain in the United States. Am J Clin Nutr Suppl. 2000;71:179S–188S. doi: 10.1093/ajcn/71.1.179S. [DOI] [PubMed] [Google Scholar]
- 73.Jonnalagadda SS, Egan SK, Heimbach JT, Harris SS, Kris-Etherton PM. Fatty acid consumption patterns of Americans: 1987–1988 USDA Nationwide Food Consumption Survey. Nutr Res. 1995;15:1767–1781. [Google Scholar]
- 74.Allison DB, Egan SK, Barraj LM, Caughman C, Infante M, Heimbach JT. Estimated intake of trans fatty acids and other fatty acids in the US population. J Am Diet Assoc. 1999;99:166–174. doi: 10.1016/S0002-8223(99)00041-3. [DOI] [PubMed] [Google Scholar]
- 75.Knapp HR, Reilly IA, Alessandrini P, FitzGerald GA. In vivo indexes of platelet and vascular function during fish-oil administration in patients with atherosclerosis. N Engl J Med. 1986;314:937–942. doi: 10.1056/NEJM198604103141501. [DOI] [PubMed] [Google Scholar]
- 76.Knapp HR, FitzGerald GA. The antihypertensive effects of fish oil. A controlled study of polyunsaturated fatty acid supplements in essential hypertension. N Engl J Med. 1989;320:1037–1043. doi: 10.1056/NEJM198904203201603. [DOI] [PubMed] [Google Scholar]
- 77.Ip C. Review of the effects of trans fatty acids, oleic acid, n-3 polyunsaturated fatty acids, and conjugated linoleic acid on mammary carcinogenesis in animals. Am J Clin Nutr. 1997;66:1523–1529. doi: 10.1093/ajcn/66.6.1523S. [DOI] [PubMed] [Google Scholar]
- 78.Hrelia S, Bordoni A, Celadon M, Turchetto E, Biagi PL, Rossi CA. Age-related changes in linoleate and alpha-linoleate desaturation by rat liver microsomes. Biochem Biophys Res Commun. 1989;163:348–355. doi: 10.1016/0006-291x(89)92142-6. [DOI] [PubMed] [Google Scholar]
- 79.Newcomer LM, King IB, Wicklund KG, Stanford JL. The association of fatty acids with prostate cancer risk. Prostate. 2001;47:262–268. doi: 10.1002/pros.1070. [DOI] [PubMed] [Google Scholar]
- 80.De Stefani E, Deneo-Pellegrini H, Boffetta P, Ronco A, Mendilaharsu M. Alphalinolenic acid and risk of prostate cancer: a case-control study in Uruguay. Cancer Epidemiol Biomark Prev. 2000;9:335–338. [PubMed] [Google Scholar]
- 81.Blot WJ, Lanier A, Fraumeni JF, Bender TR. Cancer mortality among Alaska natives, 1960–1969. J Natl Cancer Inst. 1975;55:546–554. doi: 10.1093/jnci/55.3.547. [DOI] [PubMed] [Google Scholar]
- 82.Harvei S, Bjerve KS, Tretli S, Jellum E, Robsahm TE, Vatten L. Prediagnostic level of fatty acids in serum phospholipids: omega-3 and omega-6 fatty acids and the risk of prostate cancer. Int J Cancer. 1997;71:545–551. doi: 10.1002/(sici)1097-0215(19970516)71:4<545::aid-ijc7>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 83.Chung BH, Mitchell SH, Zhang JS, Young CYF. Effects of docosahexaenoic acid and eicosapentaenoic acid on androgen-mediated cell growth and gene expression in LNCaP prostate cancer cells. Carcinogenesis. 2001;22:1201–1206. doi: 10.1093/carcin/22.8.1201. [DOI] [PubMed] [Google Scholar]
- 84.Rose DP. The mechanistic rationale in support of dietary cancer prevention. Prev Med. 1996;25:34–37. doi: 10.1006/pmed.1996.0012. [DOI] [PubMed] [Google Scholar]
- 85.Kaplan PJ, Mohan S, Cohen P, Foster BA, Greenberg NM. The insulin-like growth factor axis and prostate cancer: lessons from the TRansgenic Adenocarcinoma of Mouse Prostate (TRAMP) model. Cancer Res. 1999;59:2203–2209. [PubMed] [Google Scholar]
- 86.Nelson JB, Lepor H. Prostate cancer: radical prostatectomy. Urol Clin North Am. 2003;30:703–723. doi: 10.1016/s0094-0143(03)00049-1. (viii) [DOI] [PubMed] [Google Scholar]
- 87.Ward JF, Blute ML, Slezak J, Bergstralh EJ, Zincke H. The long-term clinical impact of biochemical recurrence of prostate cancer 5 or more years after radical prostatectomy. J Urol. 2003;170:1872–1876. doi: 10.1097/01.ju.0000091876.13656.2e. [DOI] [PubMed] [Google Scholar]