Abstract
The care of patients now almost inevitably seems to involve many different individuals, all needing to share patient information and discuss their management. As a consequence there is increasing interest in, and use of, information and communication technologies to support health services. Yet, while there is significant discussion of, and investment in, information technologies, communication systems receive much less attention and the clinical adoption of even simpler services like voice-mail or electronic mail is still not commonplace in many health services. There remain enormous gaps in our broad understanding of the role of communication services in health care delivery. Laboratory medicine is perhaps even more poorly studied than many other areas, such as the interface between primary care and hospital services. Given this lack of specific information about laboratory communication services, this paper will step back and generally review the components of a communication system, including the basic concepts of a communication channel, service, device and interaction mode. The review will then try and summarise some of what is known about specific communication problems that arise across health services in the main, including the community and hospital service delivery.
Introduction
The care of patients now almost inevitably seems to involve many different individuals, all needing to share patient information and discuss their management. As a consequence there is increasing interest in, and use of, information and communication technologies to support health services. Indeed, if information is the lifeblood of healthcare then communication systems are the heart that pumps it.1 Yet, while there is significant discussion of, and investment in, information technologies, communication systems receive much less attention. Whilst there is some significant advanced research in highly specific areas like telemedicine, the clinical adoption of even simpler services like voice-mail or electronic mail is still not commonplace in many health services. Much of this would change if it were more widely realised that the biggest information repository in healthcare sits in the heads of the people working within it, and the biggest information network is the complex web of conversations that link the actions of these individuals.
There remain enormous gaps in our broad understanding of the role of communication services in health care delivery. Laboratory medicine is perhaps even more poorly studied than many other areas, such as the interface between primary care and hospital services. Yet clinical laboratories in many ways are message-processing enterprises, receiving messages containing information requests, and generating results that are sent as messages back to clinical services. While there is much current focus on improving laboratory turn around times and internal efficiencies, little is really known about the broader communication processes within the healthcare system, of which clinical laboratories are but one link in the chain. Yet without this broader view, there is an ever-present risk that local systems within laboratories are optimised and over-engineered, but that the global performance of health services remain relatively unchanged.
Given this lack of specific information about laboratory communication services, this paper will step back and generally review the components of a communication system, including the basic concepts of a communication channel, service, device and interaction mode. The review will then try and summarise some of what is known about specific communication problems that arise across health services in the main, including the community and hospital service delivery.
The Communication Space Accounts for the Bulk of Information Transactions in Healthcare
We can conceive of all the information that gets exchanged in health care as forming a ‘space’.2 The communication space is that portion of the total number of information transactions that involves interpersonal interaction. For example, face-to-face conversations, telephone calls, letters and e-mail all generate transactions that would fall into the communication space.
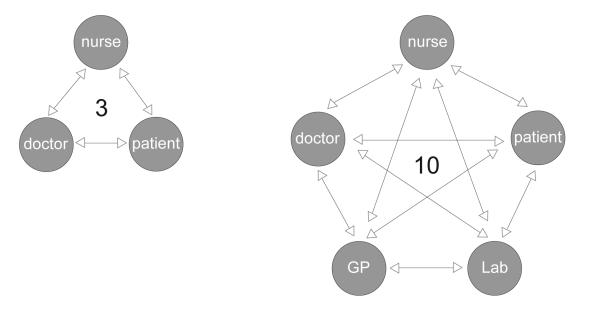
Even small clinical teams have the capacity to generate large and complex communication spaces. Theoretically, the number of different conversations that could take place at any one time is determined by the number of individuals who may have a need to communicate.3 With three members in a clinical team, three separate conversations could take place between any two individuals. If we increase the size of the team to five individuals, the number of possible conversations increases to 10, and for a team of 10 the number of possible conversations blows out to 45 (Figure 1). This is because the number of possible conversations is determined by a combinatorial formula:
Figure 1.
The number of possible conversations increases combinatorially with the number of individuals who need to communicate (after Lang and Dickie, 1978).3
| number of conversations = n!/(r!(n−r)! |
where n is the number of individuals, and r is the number of individuals involved in a single conversation.
There are few studies that have attempted to directly quantify the actual size of the communication space in health settings. Those studies that do exist all paint a similar picture. Covell et al. reported that colleagues rather than document sources met about 50% of information requests by clinicians in clinic.4 In a similar study, Tang et al. found that about 60% of clinician time in clinic is devoted to talk.5 Safran et al. reviewed the information transactions in a hospital with a mature computer-based record system, and still found about 50% of information transactions occurred face-to-face between colleagues, with e-mail and voice-mail accounting for about another quarter of the total.6 Only about 10% of the information transactions occurred through the electronic medical record. In some specialised clinical units like the emergency room, where a large number of staff are physically co-located and engage in teamwork, the communication space can account for almost all information transactions. In one study, communication between staff represented almost 90% of all the information transactions that were measured in two emergency rooms.7
The sheer scale and complexity of these interactions within the healthcare system puts a heavy burden on the process of communication, and miscommunication can have terrible consequences. Not only is the communication space huge in terms of the total information transactions and clinician time, it is also a source of significant morbidity and mortality. Communication failures are a large contributor to adverse clinical events and outcomes. In a retrospective review of 14,000 in-hospital deaths, communication errors were found to be the lead cause, twice as frequent as errors due to inadequate clinical skill.8 Further, about 50% of all adverse events detected in a study of primary care physicians were associated with communication difficulties.9 If we look beyond the raw numbers, the clinical communication space is interruption-driven, has poor communication systems and poor practices.10 At the administrative level, the poor communication of information can have substantial economic consequences. It is now clear, for example, that the healthcare system suffers enormous inefficiencies because of the poor quality of communication systems that are often in place.
So, in summary, the communication space is apparently the largest part of the health system’s information space. It contains a substantial proportion of the health system information ‘pathology’, but is still usually ignored in our thinking. Yet it seems to be where most of the information in the clinical workplace is acquired and presented.
A Communication System Includes People, Messages, Mediating Technologies, and Organisational Structures
Communication systems are the formal or informal structures organisations use to support their communication needs. A communication system involves people, the messages they wish to convey, the technologies that mediate conversations, and the organisational structures that define and constrain the conversations that are allowed to occur. Elements of communication systems include:
Communication channel: The channel is the ‘pipe’ along which a message is conveyed, and there are a wide variety of different communication channels available, from basic face-to-face conversation, through to telecommunication channels like the telephone or e-mail, and computational channels like the medical record. Channels have attributes like capacity and noise, which determine their suitability for different tasks. When two parties exchange messages across a channel at the same time, this is known as synchronous communication. Telephones are one of the commonest two-way synchronous channels. It is the nature of synchronous communication that it is interruptive, and these interruptions may have a negative impact on individuals who have high cognitive loads. For example, a busy clinician may forget to carry out a clinical task because they have been interrupted while they are busy. In contrast, when individuals can be separated in time, they may use an asynchronous channel to support their interaction. Since there can be no simultaneous discussion, conversations occur through a series of message exchanges. This can range from Post-it™ notes left on a colleague’s desk, to sophisticated electronic messaging systems. One of the benefits of asynchronous communication is that it is not inherently interruptive, and if a communication is not urgent, asynchronous channels may be a preferred way of communicating with otherwise busy individuals.
Types of message: Messages are structured to achieve a specific task using available resources to suit the needs of the receiver. Informal messages, which have variable structures, include voice and e-mail messages. Structured or formal messages include hospital discharge summaries, computer-generated alerts and laboratory results. When these messages are computer generated, they typically will be in a format that complies with a standard, and the HL7 standard is now arguably the international de facto messaging standard within healthcare.
Communication policies: A communication system can be bounded by formal procedure rather than technology, e.g. clinical handover. A hospital may have many different policies that shape their communication system performance, independent of the specific technologies used. For example, it might be a policy to prohibit general practitioners to obtain a medical record directly from the records department without the permission of a hospital clinician.
Agents: A communication system can be specifically constructed around the agents involved in the different information transactions. For example, in a busy clinical unit, one could devise a system where a ward clerk can be tasked to field all incoming telephone calls. The clerk’s specific communication role is thus an organisational structure created in support of a policy to minimise interruption to clinical staff, who might otherwise have to answer the phone. Agents have attributes like their understanding of specific tasks and language.
Communication services: Just as computer systems can run a number of different software applications, we can think of a communication system providing a number of different communication services. Thus voice communication is only one of the many services available across a telephone line. Fax transmission of documents is an entirely different kind of service that uses the same underlying channel. For example, a mobile phone may provide voice-mail, text messaging.
Communication device: Communication services can run on different communication devices. Examples of devices include the telephone, fax machine, and personal digital assistant (PDA). Different devices are suited to handle different situations and tasks. Communication devices are a source of continuing innovation, and will continue to evolve. One area of recent interest has been the area of wearable computing, where devices are small enough to become personal accessories like wristwatches or earrings.
Interaction mode: The way an interaction is designed determines much of the utility of different information systems, and this is just as true for communication systems. Some modes of interaction for example, demand that the message receiver pays attention immediately, such as the ringing tone of a phone, while others can be designed to not interrupt. An asynchronous service that is inherently not interruptive, like e-mail, may still be designed with an interruptive interaction mode, such as the ringing of a computer tone when a message arrives, altering the impact of the service on the message receiver.
Security protocol: In health care, patient privacy concerns make it important that unauthorised individuals do not access clinical records. To protect privacy, messages can be scrambled or ‘encoded’ as a means to prevent unauthorised individuals intercepting and interpreting them. For example, mobile phone conversations can be scrambled to protect unauthorised eavesdropping, and reports of medical investigations sent by e-mail can similarly have their contents encrypted. Only those with access to systems that understand the encoding, for example, through the possession of a ‘key’, should be able to read them. A widely available public method for encoding messages is through use of the Public Key Infrastructure. As is now widely known, there are always individuals with the time and capacity to try and ‘hack’ security protocols and read privileged information. Fortunately, most important communications typically have extremely strong security protocols that are exceedingly hard to be cracked. For example, internet banking systems are only possible because customers have faith that system security is for practical purposes impenetrable. The use of similar encryption methods in healthcare will typically afford the same degree of protection, and confidence in the system. The choice of security protocol used will reflect the degree of risk associated with unauthorised access to message content.
A communication system is thus a bundle of different components and the utility of the overall system is determined by the appropriateness of all the components together. If even one element of the system bundle is inappropriate to the setting, the communication system can under perform. For example, sending an X-ray to a small PDA is unlikely to be useful, both because the size of the device may limit the view of the image, as well as the size of the image may exceed the capacity of the wireless channel used by the PDA.
Services Vary in the Media they Employ
Communication systems can also be understood in terms of the different media they employ. Some for example, are designed only for voice, whilst others may carry images or data (Table 1). The value of one medium over another is usually context dependent.11 The nature of a particular task, the setting in which it occurs, and the amount of information that a medium can bear all seem to have effects on human performance on a communication task.12 For example, relatively information-lean media like electronic mail12 and voice-mail11 can be used for routine, simple communications. In contrast, it seems that for non-routine and difficult communications, a richer medium like video, and preferably face-to-face conversation, should be used.
Table 1.
Communication needs can be characterised by the separation of participants over time or distance (after Johansen et al.13)
| Sound | Image | Data | |
|---|---|---|---|
| synchronous | telephony | video-conferencing | shared electronic white boards, shared documents |
| asynchronous | voice-mail | letters and notes, computer image store and forward | paging, fax, e-mail |
This may be because in routine situations, individuals share a common model of the task and so need to communicate less during an exchange. In contrast, in novel situations a significant portion of the communication may need to be devoted to establishing common ground.14 In simple terms, since the participants do not share a common model of the task at hand, they are unable to interpret all the data passing over the channel. This means that during the conversation, there are additional demands upon the channel to also support the transmission of task models. Since this is a complex communication task, individuals may need to check with each other repeatedly throughout the conversation that they indeed understand each other.
Communication Needs in Healthcare Vary Widely
Communication tasks vary widely across the healthcare system and it is helpful to separate communication needs into the intra-organisational needs within particular groups, such as hospitals or primary care centres, and the inter-organisational needs that occur at the interfaces between different organisations. The communication boundary between primary care givers in the community and hospital based health services, for example, are characterised by the widely differing task styles and organisational structures of individuals within the two groups. In the following sections, current work devoted to supporting communication within the areas of community and hospitals will be reviewed.
Communication and Primary Care
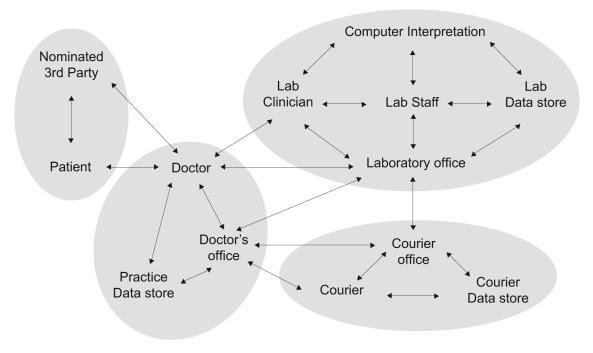
There are significant organisational and communication challenges facing those delivering healthcare in the community. The model of shared care often adopted means that many different healthcare professionals may be involved in the management of an individual patient. Even apparently simple activities such as ordering a laboratory test in general practice, and receiving the report, can involve many individuals, and many opportunities for inefficiency and error (Figure 2).
Figure 2.
Possible communication pathways for a laboratory test, ordered by a general practitioner.
Primary care in many nations is under pressure with diminishing resources being applied to growing consumer demands for access to care. Telephone services can be used to both provide information to patients who believe they need to visit a general practitioner, as well as actively triage the patient. For example, it may be possible to counsel a patient that no visit is required, direct them instead to a more appropriate service like a hospital emergency room, or assist them by making an appointment with their GP when this appears necessary.
Nurse operated telephone triage has been shown to be both safe and effective as an out of hours service in primary care. One large-scale controlled study compared the impact of 7184 calls to a nurse triage point versus 7308 calls in the control group.15 No increase in adverse events were noted during the trial, and the service resulted in a 69% reduction in telephone advice from the general practices, a 38% reduction in patient attendances to the practices, and a 23% reduction in home visits.
In the UK, a service called NHS Direct has been set up to provide both information to consumers as well as acting as a triage point for the National Health Service (NHS). The system interacts with patients using multiple different channels and media, including a web presence, a call centre, and information kiosks located in public areas. Even simple communication services are actually a complex bundle of components, often making evaluation difficult. With such a heterogeneous service as NHS Direct, one would expect no single metric to be available to determine effectiveness, nor would one expect benefits to be spread uniformly across the service.
Indeed, the evaluation of NHS Direct has proven to be difficult, given the complexity of the service.16 Some evidence suggests it has reduced the demand on emergency rooms, which have received fewer telephone enquiries since the service came into operation.17 However, little evidence exists that NHS Direct has significantly reduced demand on the NHS18 and therefore it is argued it is unlikely to be cheaper to run.19 Lack of patient awareness of the service has confounded the analysis, as measures like cost-effectiveness for services with national reach are predicated on high levels of national awareness. Cost effectiveness has proven to be an issue in other settings as well. A study of 32 paediatric call centres in the United States showed that all were losing on average $500 000 a year.20
The Interface between Primary Care and Specialist Services There has been a great emphasis in telemedicine on the interface between primary care and specialist services. There is a clear need for patient information to be exchanged between hospitals and primary care physicians upon admission to and discharge from hospital. The use of existing processes like the postal system to deliver such information is often criticised for tardiness and unreliability. In contrast, rapid communication of hospital discharge information using electronic data transfer mechanisms has been shown to be beneficial for general practitioners.21
Hospital discharge summaries have long been identified as a weak point between primary care and hospitals, both because of the tardiness of their arrival, and the quality of the information they contain. Discharge summaries arrive by a variety of means including the post, fax and e-mail. A randomised clinical trial in Canada compared discharge summaries created automatically from medical records against summaries created by voice dictation and demonstrated that the automated service can result in speedier completion of the summaries at no reduction in quality.22
Criticism is also often made of communications that originate in primary care, especially referral letters accompanying patients to the emergency room, or specialists. Simple interventions such as structured forms may improve the quality of such communication,23 but the wide variation in the types of message such letters might contain may require more complex, computer assisted methods.
There has been significant recent effort in promoting methods that permit primary care practitioners to manage patients whom they would normally have referred to specialist centres, by supporting them with access to remote specialist advice. In one study, direct telephone access to a hospital-based cardiac monitoring centre was provided to primary care practitioners. They were able to consult with a cardiologist as needed, as well as transmit a 12-lead ECG.24 The centre in this study provided a 24 hour continuous service. Possible outcomes of the discussion were that the practitioner continued to manage the patient, that the patient was referred to a cardiology clinic, or in the case of suspected myocardial infarction, rapid hospital admission was arranged with pre-warning of hospital medical teams. A trial of 2563 patients over 18 months indicated that the service was perceived to be valuable, but no comparative cost-benefit analysis was performed.
In a pilot of video-based consultation for dermatological problems, the primary care practitioner was able to discuss patient cases interactively with a dermatologist, with the patient present. Over half of the patients could then be dealt with by the general practitioner immediately after consultation.25 Common wisdom sees this type of service as a useful means of screening patients prior to being seen by specialists, especially if travel is involved. However, in this study the patients suggested that they preferred an initial face-to-face consultation with the specialist dermatologist, and that the teleconsultation would have been better used for subsequent review of their progress.
Similar studies in Norway have identified other benefits to this type of remote telemedical consultation. The skill level of isolated practitioners was raised through repeated interactions with remote specialists and through having to manage cases that were previously referred.26 This may arise through the dynamics of the relationship between remote practitioner and specialist. Unlike most educational settings, both are motivated to form a coach and apprentice relationship for the immediate management of a patient.
It is still unclear in what precise circumstances video-based consultations are most appropriate. While there are some benefits in accessing remote expertise, there are limitations to the current technologies. It is well known for example, that during a clinical encounter, a significant component of the information conveyed between practitioner and patient is non-verbal.27 Tone of voice, facial expression and posture all convey subtle information cues that are interpreted by the patient. Technology can act either to distort these cues, or to filter them out. In some cases this might be beneficial. A patient may be less distressed if they are unable to pick up cues that the practitioner is worried about a situation. Equally, a patient’s distress might increase if cues are misinterpreted because they are unfamiliar with the dynamics of the video consultation. These effects will vary with the type of communication channel used, and the practitioner’s skills at using the channel. Having a good ‘video manner’ may well soon be as important as having a good telephone manner.
Communication and Hospitals
Telemedical systems, as we have seen, have been actively explored at the interface between hospital-based specialist services and primary care. Similar problems exist between small hospitals, which may not have access to the highly specialised personnel that can be found in larger institutions like teaching hospitals. Indeed, with the growing number of sub-specialities in clinical medicine, it is now unlikely that any one institution has a representative from every feasible medical sub-speciality within their institution. For this reason, there is a need to share highly specialised expertise across different hospitals, sometimes involving large distances.
Inter-hospital Communication
There is now some evidence that remote consultation, using telemedical facilities like video-conferencing, is able to assist with this problem of distribution of expertise.28 It has been shown for example, that when a general radiologist is able to consult with a remote specialist, sharing views of X-ray images using low resolution video, then the general radiologist’s diagnostic accuracy improved.29 It now seems accepted that with appropriate technology, digitally transmitted images can in principle match existing imaging methods.30,31 The cost of achieving such results varies with the type of imaging task being attempted.
Triage models, similar to those explored in primary care, can limit the number of patients who need to be seen by limited sub-speciality resources. For example, in one study, general pathologists reviewed and reported on cases, and referred difficult cases to remote specialists by sending them high-resolution images.32
In another study, patients were offered access to specialist medical practitioners in a different country. Patients were able to travel there or to have a consultation by video-link. Choosing the video-conferencing option changed patients’ desires to travel overseas. Of those seeking consultation, 20% initially wished to travel for treatment, but after the teleconsultation only 6% chose this option.33
Most of these studies throw up evidence that advanced communication systems and services are valuable. What remains unclear is whether there is any real cost-benefit from this approach. Indeed, it is becoming clear that the application of such technologies is only beneficial in particular sets of circumstances.
For example, comparing the costs of providing a rural population with radiology services from a small community-based unit, against a teleradiology system, the communication option fared poorly in one study.34 The study showed that the existing community-based system was the most cost-efficient, and the telemedical option the most expensive. The inconvenience caused when patients had to travel for specialist investigations was not factored into the study, nor was the possibility that some communities might not have access to local expertise.
Overall, the cost savings from installing any communication system must vary for different communities. The amount of resource saved, however measured, depends upon many variables. These include:
the size of population served
the utilisation rates of the services that are being augmented by the communication option
the distances workers or patients might otherwise need to travel
the effectiveness of local services in comparison to the telemedical options.
There is also evidence that some types of task are not entirely suited to the remote consultation model. Microbiologists, for example, probably need 3 dimensional image information, as well as non-visual data like smell, before remote interpretation of microbiology specimens becomes feasible.35
As always, it is important to not overlook simpler solutions to communication problems, if they exist. It is not always appropriate or necessary, for example, to use video-based consultation. In many cases, the communication needs of a specialist consultation may be met by use of the telephone alone.36 Rather than purchasing systems permitting real-time video conferencing, images can be sent across computer networks. Standard e-mail systems are capable of transmitting text and image, and are more than able to manage the task of sending still images, such as pathology slides or X-ray images.37 Once images have been received remotely, they can be viewed simultaneously and discussed over the telephone. Simple methods now exist to enhance this further, so that viewers can mark or point to sections of an image, and have these markings appear at the remote site.
Intra-hospital Communication
Almost all of the current telemedical research is focused on the interfaces between hospitals and community services or the home. Very little work has been done to understand the internal communication dynamics and requirements of hospitals. Yet it should be apparent that any hospital is a complex organisation, and that good communication processes must be fundamental to its operation.
Thus, while much effort has been devoted to developing the electronic patient record, there has been minimal exploration of what communication systems can be developed to support hospital operation. However, a critical examination of the characteristics of the hospital as a workplace can identify clear areas in which there is significant potential for improvement. Two areas in particular deserve discussion; the need to support mobility, and the need for asynchronous messaging.
Mobility.
In contrast to other populations such as office workers or clinic-based healthcare workers, hospital workers are highly mobile during their working day. Nursing staff are perhaps least mobile, spending most of their day moving around their home ward. Medical staff may have to move widely across a hospital campus. Senior medical staff may also have to move off campus, to attend other hospitals or clinics. Nevertheless, it is important that staff remain within reach during the working day.
At present the most common solution to this problem of contacting mobile staff is provided by radio-paging. Pagers are almost ubiquitous in modern hospitals, and staff may carry several of these. For example, a pager might be issued to each individual. Other pagers are issued to members of teams, for example a ‘crash’ team that needs to respond to critical emergencies like cardiac arrests within the hospital. Pagers thus serve to permit communication both with named individuals, and individuals occupying labelled roles like ‘surgeon on call’.38,39
Pagers have several drawbacks. Invariably in a busy work environment, people move about and telephones are a pooled resource that quickly become engaged. As someone is paged, they answer the call to find either that the number given is now engaged, or that the caller has moved on to another ward location. The end result is often a game of ‘telephone tag’. The provision of mobile telephones bypasses many of these problems. The call set-up delays inherent in paging are eliminated, and the number of communication access points is multiplied through personal handsets. The value of mobile communications in a clinical environment is starting to be appreciated, but at present remains an under-utilised option.40 As with any technology there are some drawbacks. At a practical level, some healthcare workers can choose to hide behind a paging system, effectively choosing which calls to answer based upon their current state. This form of call-screening may no longer be possible if individuals have personal mobile telephones. The reduced costs of contacting colleagues and increased benefits of being contactable may be at the cost of decreased control of communication and increased interruption. At present it appears that the benefits significantly outweigh the costs, but formal studies are needed to confirm this.
Asynchronous communications.
Hospitals are highly interrupt-driven environments.38 Interruptions to the normal flow of work are caused by the paging and telephone systems, as well as the result of impromptu face-to-face meeting by colleagues (e.g. being stopped in the corridor). The team-based nature of work also demands that subjects communicate frequently with team members throughout the working day.
For example, nearly a third of communication events in a study of emergency room practice were classified as interruptions, meaning that they were not initiated by the observed subject, and occurred using a synchronous communication channel such as face-to-face conversation. This gave a rate of 11.15 interruptions per hour for all subjects.7 Even higher interruption rates were identified for individual clinical roles. Medical registrars and nurse coordinators experienced rates of 23.5 and 24.9 interruptions per hour.41 In contrast, nurses and junior doctors had rates of 9.2 and 8.3 interruptions per hour.
The consequence of such frequent interruptions is that hospital workers have to repeatedly suspend active tasks to deal with the interruption, and then return to the previous task. Suspending tasks and then returning to them imposes a cognitive load, and may result in tasks being forgotten, or left incomplete.42 There thus is a cost in time and efficiency arising out of the interrupt-driven nature of the hospital work environment.
In part, the interruptive nature of hospitals is a result of the communication practices and systems in place in these organisations. For example, external telephone calls are one major source of interruption in emergency rooms, especially if clinical staff is expected to suspend their current tasks to handle the calls. A simple organisational change such as the introduction of a dedicated communications clerk, who fields all incoming calls, has the potential to significantly reduce the communication load on clinical staff.
More generally, many hospitals do not at present routinely offer asynchronous channels like voice-mail or e-mail. It is likely that some of the interruptions delivered through synchronous systems like the telephone and pager system could be handled by asynchronous channels. For example, updates on patient results or non-urgent requests to complete tasks could be sent by voice-mail or e-mail. As long as it is felt by those sending such messages that they definitely will be attended to, then some of the cause of interruption can be shifted onto these asynchronous systems. Thus there seems to be a need for a concomitant change in communication process as well as the technology for such changes to be effective. The evidence that such asynchronous systems are of genuine benefit is slowly accumulating.
One of the limitations to the introduction of e-mail systems is the lack of access points around a campus, for many of the same reasons that access to telephony is limited. The mobility of workers is perhaps one of the main issues. It is for this reason that mobile computers are being introduced into the hospital environment.43 Connected by wireless links, these small devices provide access to the hospital computer network.
The main driver for introducing such systems is to provide an easy way to capture clinical data and enter it into the hospital record system, or to retrieve data from it. One additional benefit of mobile computing will be mobile access to e-mail. However, more advanced systems will be able to provide even richer services. Integrating mobile telephony, paging, and access to the hospital network through lightweight portable devices, newer systems can combine the functionality of the telephone with that of the computer.
Conclusions
Information and communication technology offer powerful means for restructuring many health service processes, and there currently are an increasing array of communication channels, media, and devices from which communication services can be constructed. In health care, where we are constantly reminded of the need to make pragmatic improvements to the outcomes of health care delivery, empirical evidence is needed to guide the use of new technologies, and there is a now thankfully a growing literature on the value of communication systems in health service delivery. Nevertheless there remains a substantial imbalance in the attention that is given to communication support, compared to that paid to traditional information systems. Yet communication enhancements seem to be one of the cheapest and most cost effective interventions we have available to improve the quality and safety of clinical services, and deserve much greater attention than they currently receive.
Acknowledgments
This paper is an edited and updated version of material that originally appeared in the Guide to Health Informatics, published by Arnold Hodder, London, 2003.
Footnotes
Competing Interests: None declared.
References
- 1.Touissant PJ, Coiera E. Supporting communication in health care. Int J Med Inform. 2005;74:779–81. doi: 10.1016/j.ijmedinf.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Coiera E. When Conversation is better than Computation. J Am Med Inform Assoc. 2000;7:277–86. doi: 10.1136/jamia.2000.0070277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lang GS, Dickie KJ. The practice-oriented medical record, Aspen, MD, 1978.
- 4.Covell DG, Uman GC, Manning PR. Information needs in office practice: are they being met? Ann Intern Med. 1985;130:596–9. doi: 10.7326/0003-4819-103-4-596. [DOI] [PubMed] [Google Scholar]
- 5.Tang PC, Jaworski MA, Fellencer CA, Kreider N, LaRosa MP, Marquardt WC. Clinician information activities in diverse ambulatory care practices. Proc AMIA Annu Fall Symp 1996;:12–6. [PMC free article] [PubMed]
- 6.Safran C, Sands DZ, Rind DM. Online Medical Records: A decade of experience. Proceedings of EPRIMP 1998; October; Rotterdam; IMIA. p. 67–74.
- 7.Coiera E, Jayasuriya R, Hardy J, Bannan A, Thorpe M. Communication loads on clinicians in the Emergency Department. Med J Aust. 2002;176:415–8. doi: 10.5694/j.1326-5377.2002.tb04482.x. [DOI] [PubMed] [Google Scholar]
- 8.Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JC. The Quality in Australian Health Care Study. Med J Aust. 1995;163:458–71. doi: 10.5694/j.1326-5377.1995.tb124691.x. [DOI] [PubMed] [Google Scholar]
- 9.Bhasale AL, Miller GC, Reid SE, Britt HC. Analysing potential harm in Australian general practice: an incident-monitoring study. Med J Aust. 1998;169:73–6. doi: 10.5694/j.1326-5377.1998.tb140186.x. [DOI] [PubMed] [Google Scholar]
- 10.Coiera E, Tombs V. Communication behaviours in a hospital setting - an observational study. BMJ. 1998;316:673–7. doi: 10.1136/bmj.316.7132.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caldwell BS, Uang S, Taha LH. Appropriateness of communications media use in organizations: situation requirements and media characteristics. Behaviour and Information Technology. 1995;14:199–207. [Google Scholar]
- 12.Rice RE. Task analyzability, use of new media, and effectiveness: a multi-site exploration of media richness. Organizational Science. 1992;3:475–500. [Google Scholar]
- 13.Johansen R, et al. Leading business teams, Addison Wesley, 1991.
- 14.Clarke H, Brennan S. Grounding in Communication. In Resnick LB, Levine J, and Behreno S, editors. Perspectives on socially shared cognition. Washington: American Psychological Association;1991. p. 127–49.
- 15.Lattimer VL, George S, Thompson F, et al. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial. The South Wiltshire Out of Hours Project (SWOOP) Group. BMJ. 1998;317:1054–9. doi: 10.1136/bmj.317.7165.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.George S. NHS Direct Audited. BMJ. 2002;324:558–9. doi: 10.1136/bmj.324.7337.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones J, Playforth MJ. The effect of the introduction of NHS Direct on requests for telephone advice from an accident and emergency department. Emerg Med J. 2001;18:300–1. doi: 10.1136/emj.18.4.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munro J, Nicholl J, O’Cathain A, Knowles E. Impact of NHS Direct on demand for immediate care: observational study. BMJ. 2000;321:150–3. doi: 10.1136/bmj.321.7254.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wootton R. Recent advances:Telemedicine, BMJ. 2001;323:557–60. doi: 10.1136/bmj.323.7312.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Melzer SM, Poole SR. Computerized pediatric telephone triage and advice programs at children’s hospitals: operating and financial characteristics. Arch Pediatr Adolesc Med. 1999;153:858–63. doi: 10.1001/archpedi.153.8.858. [DOI] [PubMed] [Google Scholar]
- 21.Branger PJ, van der Wouden JC, Schudel BR, et al. Electronic communication between providers of primary and secondary care. BMJ. 1992;305:1068–70. doi: 10.1136/bmj.305.6861.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Walraven C, Laupacis A, Seth R, Wells G. Dictated versus database-generated discharge summaries: a randomized clinical trial. CMAJ. 1999;160:319–26. [PMC free article] [PubMed] [Google Scholar]
- 23.Harris MF, Giles A, O’Toole AB. Communication across the divide. A trial of structured communication between general practice and emergency departments. Aust Fam Physician. 2002;31:197–200. [PubMed] [Google Scholar]
- 24.Shanit D, Cheng A, Greenbaum RA. Telecardiology: supporting the decision-making process in general practice. J Telemed Telecare. 1996;2:7–13. doi: 10.1258/1357633961929105. [DOI] [PubMed] [Google Scholar]
- 25.Jones DH, Crichton C, Macdonald A, Potts S, Sime D, et al. Teledermatology in the Highlands of Scotland. J Telemed Telecare. 1996;2 (Suppl 1):7–9. doi: 10.1258/1357633961929402. [DOI] [PubMed] [Google Scholar]
- 26.Akselsen S, Lillehaug S. Teaching and learning aspects of remote medical consultation. Telektronikk. 1993;89:42–7. [Google Scholar]
- 27.Pendleton D, Schofield T, Tate P, Havelock P. The Consultation - an approach to learning and teaching Oxford:Oxford University Press;1984.
- 28.Doolittle GC, Allen A. From acute leukaemia to multiple myeloma: clarification of a diagnosis using tele-oncology. J Telemed Telecare. 1996;2:119–21. doi: 10.1177/1357633X9600200209. [DOI] [PubMed] [Google Scholar]
- 29.Franken EA, Jr, Berbaum KS. Subspecialty radiology consultation by interactive telemedicine. J Telemed Telecare. 1996;2:35–41. doi: 10.1258/1357633961929141. [DOI] [PubMed] [Google Scholar]
- 30.Martel J, Jimenez MD, Martin-Santos FJ, A Lopez-Alonso A. Accuracy of teleradiology in skeletal disorders: solitary bone lesions and fractures. J Telemed Telecare. 1995;1:13–8. doi: 10.1177/1357633X9500100103. [DOI] [PubMed] [Google Scholar]
- 31.Franken EA, Berbaum KS, Smith WL, Chang PJ, Owen DA, Bergus GR. Teleradiology for rural hospitals: analysis of a field study. J Telemed Telecare. 1995;1:202–8. doi: 10.1177/1357633X9500100403. [DOI] [PubMed] [Google Scholar]
- 32.Bhattacharyya AK, Davis JR, Halliday, et al. Case triage model for the practice of telepathology. Telemed J. 1995;1:9–17. doi: 10.1089/tmj.1.1995.1.9. [DOI] [PubMed] [Google Scholar]
- 33.Richardson RJ, Goldberg MA, Sharif HS, Matthew D. Implementing global telemedicine: experience with 1097 cases from the Middle East to the USA. J Telemed Telecare. 1995;2(Suppl 1):79–82. doi: 10.1258/1357633961929376. [DOI] [PubMed] [Google Scholar]
- 34.Halvorsen PA, Kristiansen IS. Radiology services for remote communities: cost minimisation study of telemedicine. BMJ. 1996;312:1333–6. doi: 10.1136/bmj.312.7042.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Akselsen S, Hartviksen G, Vorland L. Remote interpretation of microbiology specimens based on transmitted still images. J Telemed Telecare. 1995;1:229–33. doi: 10.1177/1357633X9500100407. [DOI] [PubMed] [Google Scholar]
- 36.McLaren P. Telepsychiatry in the USA. J Telemed Telecare. 1995;1:121–2. doi: 10.1177/1357633X9500100210. [DOI] [PubMed] [Google Scholar]
- 37.Della Mea V, Forti S, Puglisi F, et al. Telepathology using Internet multimedia electronic mail: remote consultation on gastrointestinal pathology. J Telemed Telecare. 1996;2:28–34. doi: 10.1258/1357633961929132. [DOI] [PubMed] [Google Scholar]
- 38.Coiera E. Clinical communication - a new informatics paradigm. Proc AMIA Annu Fall Symp. 1996:17–21. [PMC free article] [PubMed] [Google Scholar]
- 39.Smith HT, Hennessy PA, Lunt GA. An object-oriented framework for modelling organisational communication. In Bowers JM, Benford SD editors, Studies in computer supported cooperative work. Elsevier Science (North-Holland);1991. p. 145–57.
- 40.Fitzpatrick K, Vineski E. The role of cordless phones in improving patient care. Physician Assist. 1993;17:87–92. [PubMed] [Google Scholar]
- 41.Spencer R, Coiera E. Variation in communication loads on clinical staff in the emergency department. Ann Emerg Med. 2004;44:268–73. doi: 10.1016/j.annemergmed.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 42.Parker J, Coiera E. Improving clinical communication: a view from psychology. J Am Med Inform Assoc. 2000;7:453–61. doi: 10.1136/jamia.2000.0070453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Forman GH, Zahorjan J. The challenges of mobile computing, IEEE Computer 38–47, April, (1994).