Abstract
In 1988, the National Vietnam Veterans Readjustment Study (NVVRS) of a representative sample of 1200 veterans estimated that 30.9% had developed posttraumatic stress disorder (PTSD) during their lifetimes and that 15.2% were currently suffering from PTSD. The study also found a strong dose-response relationship: As retrospective reports of combat exposure increased, PTSD occurrence increased. Skeptics have argued that these results are inflated by recall bias and other flaws. We used military records to construct a new exposure measure and to cross-check exposure reports in diagnoses of 260 NVVRS veterans. We found little evidence of falsification, an even stronger dose-response relationship, and psychological costs that were lower than previously estimated but still substantial. According to our fully adjusted PTSD rates, 18.7% of the veterans had developed war-related PTSD during their lifetimes and 9.1% were currently suffering from PTSD 11 to 12 years after the war; current PTSD was typically associated with moderate impairment.
On 16 December 2004, The New York Times reported that, ‘‘What was planned as a short and decisive intervention in Iraq has become a grueling counterinsurgency that has put American troops into sustained close-quarters combat on a scale not seen since the Vietnam War’’ (1). These similarities to Vietnam and findings from the congressionally mandated NVVRS (2, 3) that ‘‘one in three’’ Vietnam veterans developed PTSD have led some military and Department of Veterans Affairs’ experts to expect a ‘‘deluge of troubled soldiers’’ from the war in Iraq (1). A recent report that 35% of Army and Marine veterans of the Iraq war accessed mental health services within a year of returning home seems broadly consistent with this expectation, although it is unclear what proportion of the 35% involved PTSD (4).
The high PTSD rates identified in the NVVRS have been controversial. As measured by rates of combat stress breakdowns, killed in action, or wounded in action, Vietnam has been described as a ‘‘low-intensity’’ war for U.S. forces (5). Because rates of combat stress breakdowns, killed in action, and wounded in action have historically predicted the development of PTSD and other psychiatric disorders (5, 6), the psychiatric casualty rates in Vietnam were expected to be low (7). Consistent with this, in 1988, the Centers for Disease Control (CDC) reported rates of 14.7% lifetime PTSD and 2.2% current PTSD 11 to 12 years after the Vietnam war ended (8). The NVVRS rates of 30.9% lifetime PTSD and 15.2% current PTSD, which were reported at about the same time (2, 3), were inconsistent with expectations.
PTSD diagnoses require antecedent traumatic events, defined at the time of the NVVRS as events that are markedly distressing and ‘‘out-side the range of usual human experience’’—especially events that threaten the life or physical integrity of the individual or someone close to him. The definition also includes witnessing death or serious injury to others (9). Critics have argued that the NVVRS 30.9% lifetime rate of PTSD is twice as high as the proportion of veterans (15%) who served in combat roles (10–15). This anomaly has raised questions about the accuracy of the retrospective reports of PTSD symptoms and war-zone stressors that qualify as traumatic [supporting online material (SOM) text] (10–13, 16, 17) We used military records, historical accounts, diagnostic histories of PTSD by experienced clinicians, Minnesota Multiphasic Personality Inventory validity scales, and data on compensation-seeking to address these concerns about the NVVRS.
The estimated percentage of veterans involved in combat [15%, according to McNally (12)] probably includes 10.5% who were infantrymen [(18), p. 238] and their combat counterparts in the Marines, Navy, and Air Force. However, the 15% does not include 14% who were regularly exposed to combat hazards while serving in support roles, such as combat engineers and artillery personnel [(18), p. 238]. Moreover, estimates of the percentage of veterans exposed to combat dangers increase when Vietnam is recognized as a ‘‘war without fronts’’ rather than a conventional war (19). Kolko, for example, reports that 50% of soldiers were considered ‘‘combat forces’’ [(20), p. 361], and Baskir and Strauss conclude that about 1.6 million of the 2.15 million men that they estimate were assigned to tours in Vietnam itself ‘‘served in combat’’ [(21), p. 53] (SOM text).
We used data from military personnel files (201 files) extracted by the NVVRS investigators (2, 3) together with data that we obtained from military archival sources and historical accounts to develop a record-based military historical measure (MHM) of probable severity of exposure to war-zone stressors that would capture this complexity. We constructed this MHM of exposure for all 1200 veterans in the NVVRS’s representative sample of men who served in Vietnam or surrounding areas (Theater veterans) (22) (SOM text). The first three components of the MHM are the veteran’s military occupational specialty, the monthly killed-in-action rate during his Vietnam service, and the killed-in-action rate in his larger military unit (e.g., division) (23). We have combined (23), validated (table S1), and refined these three measures with important previously unused data from the military records of the approximately 58,000 U.S. servicemen killed in action in Vietnam (24) (SOM text).
Our study revealed a strong positive relationship between our record-based MHM exposure measure and the dichotomous measure of high versus low or moderate war-zone stress constructed by the NVVRS investigators [(2), Appendix C] on the basis of the veterans’ retrospective reports of their experiences (Fig. 1). For example, 96.5% of the veterans classified as probable low exposure on the MHM were in the combined low or moderate category of the NVVRS self-report measure, and 72.1% of those classified as very high on the MHM were high by self-report.
Fig. 1.
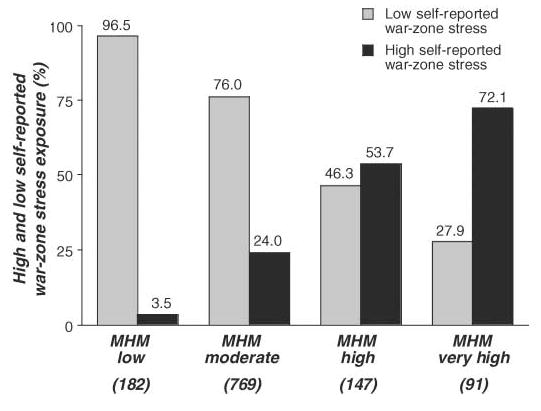
Self-reports of war-zone stress exposure correlated well with records-based MHM war-zone stress exposure. A high percentage of veterans categorized as low exposure on the basis of records-based MHM evidence had self-reported low exposure. Veterans who self-reported high exposure were the large majority of the MHM very high exposure category. Full sample n = 1189, excluding 11 veterans with missing data on self-reported war-zone exposure. Low and moderate self-reports of exposure were grouped together as ‘‘Low self-reported war-zone stress’’ [(2), Appendix C].
The NVVRS employed experienced, doctoral level clinicians to give diagnostic examinations to a representative subsample (n = 260) of the veterans who resided in 28 standard metropolitan regions (SMRs) (22). These diagnoses were used in the NVVRS to calibrate more economical PTSD symptom scales in the full 1200-member Theater sample [(2), Appendix D]. The resulting algorithm was the basis for the NVVRS 15.2% rate of current PTSD in Theater veterans. Although not representative of the entire sample of Theater veterans, the sample from the 28 SMRs had a similar rate of current PTSD (15.4%). Because the NVVRS algorithm for PTSD focused solely on current symptoms, the often quoted but rarely analyzed lifetime rate, 30.9%, was extrapolated from the results of the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) (SCID) diagnoses in the subsample [(2), Appendix E].
The subsample diagnostic examinations themselves have received relatively little attention or analysis in the main reports of the NVVRS (2, 3) or in the wider literature, even though the diagnoses contain by far the most detailed data on PTSD and the only data on the history of this disorder. We conducted further analyses of these data because they shed light on the nature of PTSD and its prevalence in Vietnam veterans. Most important, on the basis of information contained in the written records and tape recordings of these diagnoses, we were able to distinguish (i) between war-related first onsets of PTSD and first onsets that occurred before or after service in Vietnam in calculations of lifetime rates and (ii) between past PTSD that remitted and current PTSD that was present in the six months before the diagnostic examinations (22). We were also able to identify the types of criterion traumatic events that were reported by the veterans. The majority (86.6%) of the veterans with war-related onsets described events that our raters, blind to diagnostic status, judged to be personally life threatening. Events that involved witnessing death or physical harm to others were also frequently reported.
Unlike the current DSM-IV, the diagnosis of PTSD in DSM-III-R did not require impairment by either disability in social roles or elevated psychological distress. However, because the examiners assessed each veteran’s present functioning on the Global Assessment of Functioning (GAF) rating scale as part of the examination with the SCID (25), we were able to check whether the high NVVRS rates included substantial numbers of veterans with only mild, unimpairing PTSD.
We found that the majority (84.8%) of the veterans with current war-related PTSD (‘‘current group’’) were rated as having more than slight impairment at the time of the examination (Table 1). However, only 28.5% had more than moderate difficulty. Moreover, current impairment in veterans with past war-related PTSD (‘‘past group’’) differed little from impairment in the group with no war-related onsets of PTSD.
Table 1.
Estimated impairment on the GAF scale in the 260-member subsample of veterans diagnosed by experienced clinicians using the SCID (25) as having no lifetime war-related first onsets of PTSD (past or current) (n = 158), past war-related first onsets of PTSD (n = 30), and war-related first onsets of PTSD that remained current (n = 59). Percentages are based on data weighted to reflect the complex sampling design (22). (Omitted from the analysis are four veterans with prewar onsets, two missing onset information, one missing sampling weight, and six missing impairment scores.) A chi-square test shows that the overall difference in the percentages of male veterans with more than slight impairment is statistically significant at the 0.01 level. Individual tests show that the percentage impaired in veterans with current war-related PTSD is significantly greater at the 0.01 level than the percentage of impaired in veterans with past PTSD and the percentage impaired in veterans with no PTSD.
| GAF score | Description of impairment | None (%) | Past (%) | Current (%) |
|---|---|---|---|---|
| 09 | Good functioning in all areas | 46.6 | 43.6 | 0.0 |
| 08 | No more than slight impairment | 29.9 | 24.0 | 15.1 |
| 07 | Some difficulty in social, occupational, or school functioning | 18.3 | 23.9 | 40.5 |
| 06 | Moderate difficulty | 2.7 | 8.2 | 15.6 |
| 05 | Any serious impairment | 1.7 | 0.3 | 21.1 |
| 04 | Major serious impairment in several areas | 0.1 | 0.0 | 7.0 |
| 03 | Inability to function | 0.0 | 0.0 | 0.0 |
| 02 | Some danger to self or others | 0.0 | 0.0 | 0.0 |
| 01 | Persistent danger to self or others | 0.0 | 0.0 | 0.4 |
The clinicians made ratings of the severity of PTSD at its worst in addition to the severity at the time of the examination. These severity ratings, which are strongly related to the GAF impairment ratings, suggest that the results in Table 1 underestimate impairment when the disorder was at its worst. For example, 36.1% of veterans in the current group were rated mild, 43.1% moderate, and 20.8% severe at the time of diagnosis. When PTSD was at its worst, 3.7% of veterans were rated mild, 31.8% moderate, and 66.5% severe. The results also suggest that at least 85% of veterans in the past group had more than slight impairment when their PTSD was at its most severe (SOM text).
To investigate questions about the possible falsification of symptom reporting, we reasoned that if some NVVRS veterans exaggerated their PTSD symptoms by outright lying or more subtle retrospective distortions (26), these veterans should be overrepresented among veterans who reported experiencing high war-zone stress despite having record-based MHMs indicating low or moderate severity of exposure. Using questionnaire measures of dissembling (27–31) and self-reported symptoms, we found no indication of dissembling and little evidence of exaggeration (SOM text).
The possibility of receiving disability compensation might motivate falsification of symptoms and exposure reports (16). Compensation-seeking for psychiatric disability was reported by 9.3% of the veterans. However, there was no elevation of compensation-seeking among veterans discordant on the exposure measures; for example, only 3.0% of those who reported high exposure in the context of low MHM exposure sought compensation compared with 15.6% who were high on both exposure measures.
Veterans’ 201 files do not systematically record information about specific war-zone experiences (32). However, these files routinely contain, or make it possible to access from historical accounts, other valuable indicators of the likelihood of experiencing traumatic stressors. These indicators include high-exposure military occupational specialty; receipt of a Purple Heart, combat medal, or Combat Infantryman Badge; service in a company with one or more killed in action during the veteran’s tour; attachment to a high casualty division; and being in Vietnam during the nationwide Tet offensive of 1968. More than one of these indicators was present for all 30 subsample veterans in our high and very high MHM exposure groups. One or more of these indicators was also present in the 201 files of 47 of the 60 subsample veterans diagnosed with war-related PTSD in the low and moderate MHM exposure groups (SOM text).
To investigate the validity of the reports of the remaining 13 of the 60 veterans with onsets of PTSD but none of the record-based indicators of probable exposure, we compared their narratives of traumatic events with information from military histories (33, 34) and from newspaper accounts of events in Vietnam published contemporaneously in The New York Times and the Los Angeles Times. These independent sources confirmed the narratives of traumatic events of five veterans: Three veterans reported attacks on air bases, which were reported in detail in a military history of Air Force actions (33); one veteran who served in a submarine described a harrowing rescue of U.S. personnel in a downed aircraft, which was corroborated in a newspaper account, as was a typhoon that occurred during a series of attacks on another veteran’s base. This left only eight subsample veterans whose accounts were not confirmed by any of our independent checks (SOM text).
Thus, we were able to confirm as plausible the exposure to traumatic stressors of most of the subsample veterans with war-related onsets of PTSD, and most but not all of these war-related PTSD onsets, as we reported earlier, were associated with more than slight impairment. Nevertheless, removing subsample veterans without independent documentation of traumatic exposure and/or with no more than slight impairment somewhat reduces lifetime rates of war-related onsets of PTSD and rates of war-related onsets that remained current (Table 2).
Table 2.
Percentages of lifetime first onsets (past plus current) (n = 90) and percentages of current first onsets (n = 60) of war-related PTSD in the 260-member SCID-diagnosed subsample of veterans with and without adjustments for the requirements of impairment and/or independent documentation of traumatic exposure. Sample n values are in parentheses and percentages are based on data weighted to reflect the complex sampling design (22). (Omitted from the analysis are four veterans with prewar onsets, two missing onset information, and one missing a sampling weight.)
| Adjustments | Lifetime (%) | Current (%) |
|---|---|---|
| Unadjusted | 22.5 | 12.2 |
| Adjusted for impairment of functioning | 21.0 | 10.4 |
| Adjusted for documentation of exposure | 20.3 | 11.1 |
| Adjusted for both impairment and documentation | 18.7 | 9.1 |
We next investigated whether, as with the NVVRS retrospective measure of exposure and the PTSD algorithm, there is a dose-response relationship between the record-based MHM exposure and clinically diagnosed PTSD (Fig. 2). Our results show that there is. The relationship is especially strong for current PTSD, with less than 1% of the low-exposed veterans receiving this diagnosis, compared with 28.1% of the veterans in the very high exposure category. Omission of the veterans with unconfirmed traumatic exposure and/or those with no more than slight impairment had little effect (SOM text).
Fig. 2.
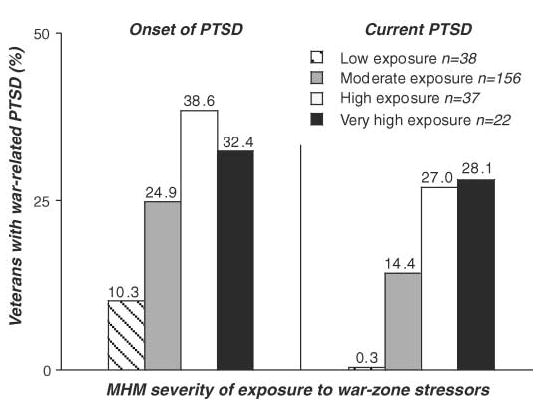
The percentages of veterans who had suffered from war-related PTSD during their lifetime (Onset of PTSD) and the percentages of those who still suffered from PTSD at the time of the study (Current PTSD) increase with increases in MHM probable severity of exposure to war-zone stressors. Subsample n = 253, omitting four veterans with prewar onset, two missing onset information, and one missing sampling weight.
The conundrum posed by critics of the NVVRS involves two figures: a 15% rate of combat exposure and a 30.9% lifetime rate of PTSD in Vietnam veterans. Our analyses show that neither figure represents the reality of the psychological risks and their consequences for U.S. forces in Vietnam. First, consistent with estimates from military histories of this war without fronts, at least half of the Theater veterans were involved in combat (20, 21). Second, even the least conservative rates of SCID-diagnosed PTSD from Table 2 (22.5% war-related onsets, 12.2% war-related current) are lower than the previously published NVVRS rates (30.9% lifetime and 15.2% current). These latter rates are based on an algorithm that calibrates self-reports of symptoms to SCID diagnoses in the subsample [(2), Appendix E]. This algorithm does not distinguish between war-related PTSD and PTSD with other origins, and scores do not depend crucially on the presence of DSM-III-R traumatic events. These differences probably contribute to the higher rates found with the algorithm.
In contrast, the SCID-based rates, even those fully adjusted for impairment and verification of exposure (18.7% onset and 9.1% current), are higher than the rates in the CDC study (8, 35). The CDC used about half of the items (36) from a newly developed module from the Diagnostic Interview Schedule (DIS) (37) to diagnose lifetime and current PTSD on the basis of responses to closed questions asked by lay interviewers. This version of the DIS PTSD module has been found to diagnose much lower rates of PTSD in the general population than the other diagnostic instrument that is most widely used by lay interviewers (38). Against this background, it is not surprising that the abbreviated CDC adaptation of the DIS PTSD module was found in the NVVRS to miss 78% of veterans who had diagnosable PTSD, according to the SCID clinicians [(2), Appendix E]. These results suggest that PTSD is under-diagnosed in both military and civilian samples when this version of DIS PTSD is used.
The SCID diagnostic results in the NVVRS have proved robust to record checks, investigation of compensation-seeking, and measures designed to detect outright falsification. It was sometimes even possible to confirm in contemporary newspaper accounts or military histories the plausibility of the veterans’ reports of war-zone experiences for which there was no confirmatory evidence in their personnel files. These results suggest that reports of a high rate of unverified trauma in some subgroups of compensation-seeking veterans (16) should not be generalized to the population of Vietnam veterans as a whole.
The message from the NVVRS has been that the Vietnam War took a severe psychological toll on U.S. veterans. Our results provide compelling reasons to take this message seriously. The nature of this toll is suggested by the substantial rates of war-related onset and current PTSD and their strong dose-response relationship with severity of exposure—a relationship that cannot be due to biases in self-reports of exposure because it holds for our new prospective, record-based MHM (SOM text). It is especially notable that, conservatively, almost 10% suffered from and were impaired by current PTSD more than a decade after the war. This finding points to the need for further research on the factors that contribute to chronicity (23, 39).
However, the majority of the veterans with high and very high MHM exposure did not develop war-related PTSD (Fig. 2). Even allowing for substantial heterogeneity of individual experiences within these high exposure categories, there appear to be protective factors that reduce vulnerability. Moreover, the trajectory for most veterans with war-related PTSD that causes substantial impairment is toward amelioration or complete remission. This tendency toward improvement is present even for ~10% of veterans who still had impairing current PTSD at follow-up; the impairment most of them showed by this time was not severe. The functioning of the veterans who had developed war-related PTSD but who no longer met criteria for the disorder at follow-up differed little from that of veterans who did not develop war-related PTSD.
These trends toward recovery over time cannot be explained entirely by treatment administered by mental health professionals because less than half the veterans with past war-related PTSD (44.9%) received such treatment. Investigations of other factors that may contribute to initial resilience and psychological readjustment after traumatic war experiences are needed (23).
Substantial similarities exist between Vietnam then and Iraq now. Both have been wars without fronts, in which it is often difficult to tell peaceful civilians from enemy combatants. What has been, and can still be, learned about PTSD and Vietnam veterans should be applicable to understanding the psychological risks to U.S. veterans of the war in Iraq.
Supplementary Material
Footnotes
Supporting Online Material
www.sciencemag.org/cgi/content/full/313/5789/979/DC1
Materials and Methods
SOM Text
Table S1
References
References
- 1.Shane S. The New York Times; 16 December, 2004. ‘‘A deluge of troubled soldiers is in the offing, experts predict,’’; p. A1. [Google Scholar]
- 2.Kulka RA, et al. I. Veterans Administration; Washington, DC: 7 November, 1988. Contractual Report of Findings from the National Vietnam Veterans Readjustment Study. [Google Scholar]
- 3.Kulka RA . Brunner/Mazel; New York: 1990. Trauma and the Vietnam War Generation. [Google Scholar]
- 4.Hoge C, Auchterlonie J, Milliken C. JAMA. 2006;295:1023. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- 5.Jones E, Wessely S. Br J Psychiatry. 2001;178:242. doi: 10.1192/bjp.178.3.242. [DOI] [PubMed] [Google Scholar]
- 6.Solomon Z, Weisenberg M, Schwarzwald J, Mikulincer M. Am J Psychiatry. 1987;144:448. doi: 10.1176/ajp.144.4.448. [DOI] [PubMed] [Google Scholar]
- 7.Wessely S. Br J Psychiatry. 2005;186:459. doi: 10.1192/bjp.186.6.459. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control. JAMA. 1988;259:2701. [Google Scholar]
- 9.American Psychiatric Association. Third Edition. American Psychiatric Association; Washington, DC: 1987. Diagnostic and Statistical Manual of Mental Disorders. Revised (DSM-III-R) [Google Scholar]
- 10.Burkett BG, Whitely G. Verity; Dallas, TX: 1998. Stolen Valor. [Google Scholar]
- 11.Marlowe D. Rand Corporation; Santa Monica, CA: 2000. Psychological and Psychosocial Consequences of Combat and Deployment. [Google Scholar]
- 12.McNally RJ. Annu Rev Psychol. 2003;54:229. doi: 10.1146/annurev.psych.54.101601.145112. [DOI] [PubMed] [Google Scholar]
- 13.Satel S. The New York Times; 5 March, 2004. ‘‘Returning from Iraq, still fighting Vietnam,’’; p. A23. [Google Scholar]
- 14.Shephard B. Harvard Univ. Press; Cambridge, MA: 2001. A War of Nerves. [Google Scholar]
- 15.Wessely S. Br J Psychiatry. 2005;186:473. doi: 10.1192/bjp.186.6.459. [DOI] [PubMed] [Google Scholar]
- 16.Frueh BC. Br J Psychiatry. 2005;186:467. doi: 10.1192/bjp.186.6.467. [DOI] [PubMed] [Google Scholar]
- 17.Southwick SM, Morgan IIICA, Nicholaou AL, Charney DS. Am J Psychiatry. 1997;154:173. doi: 10.1176/ajp.154.2.173. [DOI] [PubMed] [Google Scholar]
- 18.Clodfelter M. McFarland; Jefferson, NC: Vietnam in Military Statistics. 1995. [Google Scholar]
- 19.Thayer T. Westview Press; Boulder, CO: War Without Fronts. 1985. [Google Scholar]
- 20.Kolko G. Pantheon Books; New York: 1985. Anatomy of a War. [Google Scholar]
- 21.Baskir LM, Strauss WA. Knopf; New York: 1978. Chance and Circumstance. [Google Scholar]
- 22.Materials and methods are available as supporting material on Science Online.
- 23.Dohrenwend BP, et al. J Consult Clin Psychol. 2004;72:417. doi: 10.1037/0022-006X.72.3.417. [DOI] [PubMed] [Google Scholar]
- 24.Coffelt RD, Arnold RJ, Argabright D. National Archives and Records Administration; Washington, DC: 2002. Electronic Database. [Google Scholar]
- 25.Spitzer R, Williams J, Gibbon M. New York State Psychiatric Institute, Biometrics Research Department; New York: 1987. Structured Clinical Interview for DSM-III-R, version NP-V. [Google Scholar]
- 26.Young A. Posttraumatic Stress Disorder. In: Rosen GM, editor. Wiley; West Sussex, England: 2004. pp. 127–146. [Google Scholar]
- 27.Gough HG. J Abnorm Soc Psychol. 1947;42:215. doi: 10.1037/h0062924. [DOI] [PubMed] [Google Scholar]
- 28.Gough HG. J Consult Psychol. 1950;14:408. doi: 10.1037/h0054506. [DOI] [PubMed] [Google Scholar]
- 29.Gough HG. Consulting Psychologists Press; Palo Alto, CA: 1957. California Psychological Inventory Manual. [Google Scholar]
- 30.Weiner DN. J Consult Psychol. 1948;12:164. doi: 10.1037/h0055594. [DOI] [PubMed] [Google Scholar]
- 31.Greene RL, editor. Grune & Stratton; New York: 1988. The MMPI: Use with Specific Populations. [Google Scholar]
- 32.U.S. National Archives & Records Administration. Military Service Records and Official Military Personnel Files. (obtained 8 February 2006 through www.archives.gov)
- 33.Fox RP. Office of Air Force History; Washington, DC: 1979. Air Base Defense in the Republic of Vietnam, 1961–1973. [Google Scholar]
- 34.Sigler DB. McFarland; Jefferson, NC: 1992. Vietnam Battle Chronology. [Google Scholar]
- 35.Roberts L. Science. 1988;241:788. doi: 10.1126/science.2841757. [DOI] [PubMed] [Google Scholar]
- 36.Thompson WW, Gottesman II, Zalewski C. BMC Psychiatry. 2006;6:19. doi: 10.1186/1471-244X-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Robins LN, Helzer JE, Croughan J, Ratcliff KS. Arch Gen Psychiatry. 1981;38:381. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 38.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson C. Arch Gen Psychiatry. 1995;52:1048. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 39.Marshall RD, et al. J Nerv Ment Dis. 2006;194:275. doi: 10.1097/01.nmd.0000207363.25750.56. [DOI] [PubMed] [Google Scholar]
- 40.We thank C. J. Douglass, D. W. King, L. A. King, Y. Neria, P. E. Shrout, W. E. Schlenger, and three anonymous referees for valuable comments and suggestions. Supported by the National Institute of Mental Health (NIMH) grant R01-MH059309 and grants from The Spunk Fund, Inc. (B.P.D.); also training grant 5T32MH13043 and NIMH K08 MH070627 (K.C.K.).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


