Obesity can be assessed in several ways. Each method has advantages and disadvantages, and the appropriateness and scientific acceptability of each method will depend on the situation.
Figure 1.
For weight measurement subjects should ideally be in light clothing and bare feet, fasting, and with empty bladder; repeat measures are best made at same time of day
Table 1.
Levels of health risks associated with waist circumference (cm), defined by waist circumference action levels in white men and women
| Level | Men | Women | Health risk* |
|---|---|---|---|
| Below action level 1 |
< 94 |
< 80 |
Low |
| Action levels 1 to 2 |
≥ 94-101.9 |
≥ 80-87.9 |
Increased |
| Above action level 2 | ≥ 102 | ≥ 88 | High |
Risk for type 2 diabetes, coronary heart disease, or hypertension.
The assessment methods often measure different aspects of obesity—for example, total or regional adiposity. They also produce different results when they are used to estimate morbidity and mortality. When there is increased body fat, there will also be necessary increases in some lean tissue, including the fibrous and vascular tissues in adipose tissue, heart muscle, bone mass, and truncal or postural musculature. All these non-fat tissues have a higher density (1.0 g/ml) than fat (0.7 g/ml). The density of non-fat tissues is also increased by physical activity, which of course tends to reduce body fat.
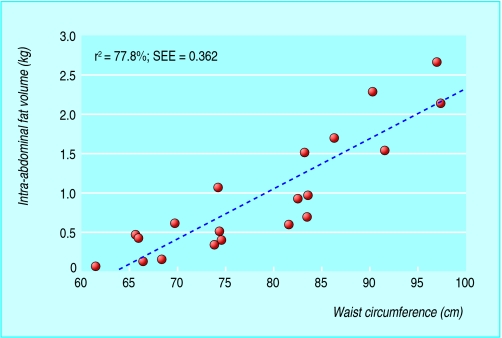
Figure 2.
The correlation of visceral fat with waist circumference is strong. Adapted from Han TS et al. Int J Obes Relat Metab Disord 1997;21: 587-93
In general, measurements of body weight and body dimensions (anthropometry) are used to reflect body fat in large (epidemiological) studies or in clinic settings as such measurements provide a rapid and cheap way to estimate body fatness and fat distribution. Densitometry or imaging techniques are used in smaller scale studies such as clinical trials.
Table 2.
Classification of body fatness based on body mass index according to World Health Organization
| BMI | Classification |
|---|---|
| < 18.5 |
Underweight |
| 18.5-24.9 |
Healthy |
| 25-29.9 |
Overweight |
| 30-39.9 |
Obese |
| ≥ 40 | Morbidly obese |
Anthropometry
Body mass index (BMI) has traditionally been used to identify individuals who are the most likely to be overweight or obese. It is calculated by dividing the weight (in kilograms) by the height (in metres) squared. Generally, a high value indicates excessive body fat and consistently relates to increased health risks and mortality. Unusually large muscle mass, as in trained athletes, can increase BMI to 30, but rarely above 32. BMI categories and cut-offs are commonly used to guide patient management. BMI reference ranges assume health in other aspects—healthy weight may be lower with major muscle wasting.
Waist circumference was developed initially as a simpler measure—and a potentially better indicator of health risk than BMI—to use in health promotion. Waist circumference is at least as good an indicator of total body fat as BMI or skinfold thicknesses, and is also the best anthropometric predictor of visceral fat.
People with increased fat around the abdomen or wasting of large muscle groups, or both, tend to have a large waist circumference relative to that of the hips (high waist to hip ratio). Waist circumference alone, however, gives a better prediction of visceral and total fat and of disease risks than waist to hip ratio. Waist circumference is minimally related to height, so correction for height (as in waist to height ratio) does not improve its relation with intra-abdominal fat or ill health.
This is the second article in the series
Adolphe Quételet was a 19th century Belgian scientist who established the body mass index to classify people's ideal weight for their height
BMI is still a useful guide to obesity related health risks, but waist circumference is a simple alternative with additional value for predicting metabolic and vascular complications
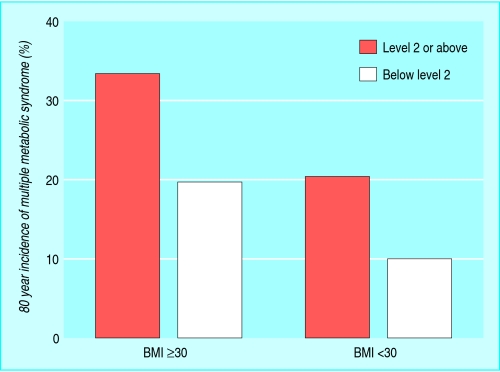
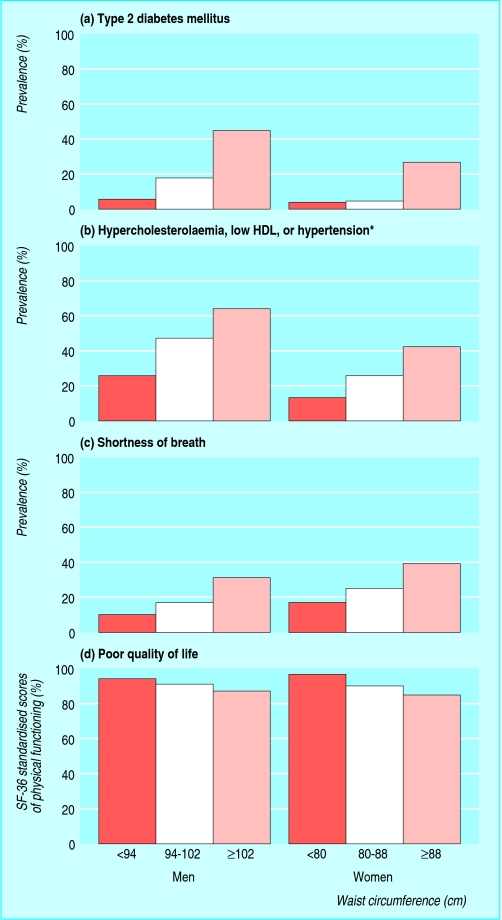
People with a large waist are many times more at risk of ill health, including features of metabolic syndrome (such as diabetes, hypertension, and dyslipidaemia) as well as shortness of breath and poor quality of life. These increased risks also apply in people whose BMI is normal but who have a large waist. However, BMI and waist circumference are colinear, so combining the two measures adds relatively little to risk predicton.
Figure 3.
Incidence of metabolic syndrome in people with different categories of body mass index and of waist circumference action levels (action level 1=94 cm in men and 80 cm in women, action level 2=102 cm in men and 88 cm in women). Adapted from Han TS et al. Obes Res 2002;10: 923-31
During weight loss, each kilogram of weight loss is equivalent to a reduction of 1 cm in waist circumference. However, there is greater measurement error for waist circumference, so body weight is the best measure for monitoring change.
Figure 4.
Prevalence of diabetes (a); hypercholesterolaemia, low HDL (high density lipoprotein), or hypertension (b); shortness of breath (c); and poor quality of life (d) in people with large waist. Adapted from Lean ME et al. Lancet 1998;351: 853-6
Waist to hip ratio was introduced—mainly as a result of Swedish research—on the assumption that it would predict fat distribution better than waist circumference alone. Subsequent research, however, showed that it did not.
Table 3.
Classification of overweight and obesity by body mass index, waist circumference, and associated disease risk* (adapted from data from National institutes of Health)
|
Risk relative to normal weight and waist circumference |
|||
|---|---|---|---|
| BMI | Men <102 cm, women <88 cm | Men ≥102 cm, women ≥cm | |
| Underweight |
18.5 |
Not increased |
Not increased |
| Normal |
18.5-24.9 |
Not increased |
Increased |
| Overweight |
25.0-29.9 |
Increased |
High |
| Obesity (class I) |
30.0-34.9 |
High |
Very high |
| Obesity (class II) |
35.0-39.9 |
Very high |
Extremely high |
| Extreme obesity (class III) | ≥ 40.0 | Extremely high | Extremely high |
Most of the relevant information in relation to risk can be derived from measurement of waist alone.
Disease risk for type 2 diabetes, hypertension, and cardiovascular disease.
Hip circumference does have a relation to health and disease, but in an inverse way, such that a relatively large hip circumference is associated with lower risks of diabetes and coronary heart disease. This is probably because hip circumference reflects muscle mass, which is reduced in type 2 diabetes and inactivity.
Table 4.
Waist to hip ratio and myocardial infarction
| • A recent report from the international Interheart study proposed waist to hip ratio as the best adiposity risk marker for acute myocardial infarction |
| • The study was a case-control study, however, rather than prospective |
| • Lower hip circumference may have reflected lower muscle mass in cases, whereas the value of waist circumference may have been diminished in this study because a non-standard method was used |
| • These factors might have exaggerated the association between waist to hip ratio and myocardial infarction |
Weight gain leads to greater adverse metabolic changes in certain ethnic groups. As a result, Asians should be considered overweight if BMI ≥23 and obese if BMI ≥27.5. Waist levels associated with risk are also lower in Asian men (≥90 cm v ≥94 cm in Europoids)
Perceptions of anthropometry
The main difficulty with anthropometric measures is that doctors, scientists, and the public are not aware of the value of these measures. People often assume that technological devices—such as fat analysers—are better at measuring body fat, despite evidence to the contrary. This assumption often arises from better marketing of technology, yet no portable body fat analysers (including those that measure bioelectrical impedance, which is highly dependent of body hydration status) are better than waist circumference for measuring body fat in adults.
Figure 5.
Accuracy in measuring waist circumference can be improved with use of a specially designed tape measure, although a change in body fat may not be detected by waist circumference in very fat people, when the abdominal fat mass is pendulous. During waist measurement, patients should be asked not to hold in their stomach, and a constant-tension, spring-loaded tape device reduces errors from over-enthusiastic tightening during measurement
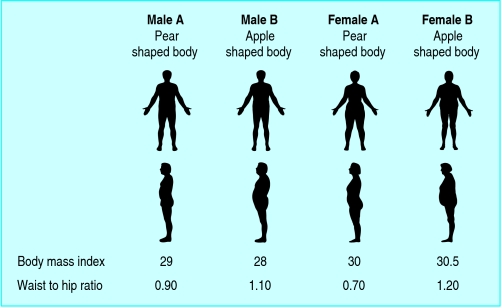
Cut-off levels of waist circumference relating to increased health risks have not been fully defined for different ethnic groups, although some African and Asian groups clearly have a greater risk of coronary heart disease than Europoids at the same cut-off levels. Two people of the same BMI may have very distinct body shapes, depending on the distribution of body fat and skeletal muscle. A change in single measures, such as the amount of weight loss or reduction in waist circumference, is easily understood by lay people, whereas a ratio (such as waist to hip ratio or BMI) is more difficult to conceptualise. BMI charts can help.
Figure 6.
Variation in human body fat distribution in men and women. In each pair of men and pair of women (subjects A and B), the body mass indices are similar. However, the waist circumference and waist to hip ratios of subjects B are much higher, indicating a greater distribution of body fat around the abdomen as well as a decreased amount of muscle mass around the hips
Anthropometric methods
Weight should be measured by digital scales or a beam balance to the nearest 100 g. Equipment should be calibrated regularly by standard weights (4×10 kg and 8×10 kg), and the results of test weighing recorded in a book. Patients should ideally be weighed in light clothing and bare feet, ideally fasting and with an empty bladder.
Figure 7.

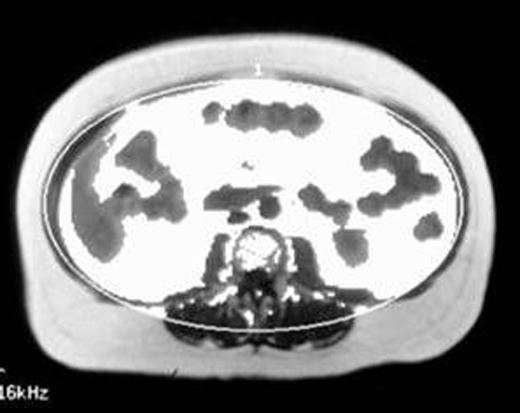
Images of different fat compartments by computed tomography. The inner elliptic ring shows intra-abdominal fat
Height is measured with a regularly calibrated stadiometer. Patients stand in bare feet that are kept together. The head is level with a horizontal Frankfort plane (an imaginary line from lower border of the eye orbit to the auditory meatus).
If a patient cannot stand—for example, is confined to a chair or bed—BMI can still be derived from special equations using arm span or lower leg length instead of height.
Waist circumference should be measured midway between the lower rib margin and iliac crest, with a horizontal tape at the end of gentle expiration. Waist circumference measurement at the umbilical level is not reliable because sagging of abdominal skin occurs in very obese subjects or those who have lost weight previously.
Densitometry
Total body fat was classically measured by densitometry based on the Archimedes principles of water displacement, assuming just two body compartments: fat (density about 0.7 g/ml) and fat-free tissue (about 1.0 g/ml). Under this principle, if two individuals of the same weight on land have different proportions of body fat and lean tissue, the one with more body fat and less lean tissue would weigh less under water.
Imaging
In the past decade, new imaging techniques such as computed tomography and magnetic resonance imaging allow discrete deposits of body fat to be imaged. Specific fat depots can be measured, including the visceral fat depots. These relate more strongly than subcutaneous fat to metabolic abnormalities. Fat in other structures, such as the liver, or muscle cannot be quantified easily. Imaging is very expensive and can be problematic for people who are claustrophobic.
Densitometry requires underwater weighing facilities and takes time, so it is expensive; furthermore, many people would not like to be submerged in water. Densitometry is therefore not used routinely. It also cannot indicate body fat distribution
Precise and accurate measurements of regional fat mass can be estimated from two dimensional, transverse, multiple slices. The fat volume estimated from a single slice based on regression equations can be used to reduce time, cost, and risk of radiation exposure for some purposes, such as repeated studies in the same patient.
Table 5.
Comparison of relative strengths and weaknesses of body mass index versus waist circumference
| BMI | Waist circumference |
|---|---|
| Predictor of total body fat and related health risks at a population level |
Predictor of total body fat and related health risks at a population level |
| Weak relation to visceral fat |
Best simple marker for visceral fat |
| Modest predictor of multiple health risks in individuals |
Stronger predictor of multiple health risks in individuals |
| Routinely collected in general practitioner contracts |
Not yet collected as part of general practitioner contracts |
| Large existing databases |
Databases accumulating rapidly |
| Less reliable in discriminating health risk when BMI < 30 |
Less reliable in discriminating health risks when BMI > 40 |
| Potentially confounded by differences in muscle mass |
Larger measurement error than BMI |
| Requires shoes off |
Requires upper clothing off |
| Sex differences ignored |
Cut-offs different for men and women |
| Needs calculation or chart for clinical use; is conceptually complex | Easy home monitoring (no calculation needed); is easily understood |
Other imaging techniques, including dual energy x ray examination, are good predictors of visceral fat but, like computed tomography, expose subjects to radiation which limits their use in repeated measurements. They were originally calibrated against densitometry.
Bioimpedance
Obese people have increased lean body mass as well as increased fat mass. Bioimpedance estimates total body water crudely, as a component of lean body mass. Therefore, estimation of fat mass by this technique is relatively weak.
Summary
Identifying people who are overweight, and particularly with accumulation of excessive visceral fat, is essential for directing future intervention. BMI and waist circumference are well validated and available to all health professionals. Waist circumference is arguably better, but both are simple, and change is best monitored by following body weight. “Black box” methods such as bioimpedance do not add greatly, and even more complex methods remain in the research domain.
The photo at the start of the article is published with permission from Simon Fraser/SPL. The computed tomograms were reproduced with permission from The American Diabetes Association (Kelly IE, Han TS, Walsh K, Lean ME. Diabetes Care 1999;22: 288-93).
The ABC of obesity is edited by Naveed Sattar (nsattar@clinmed.gla.ac.uk), professor of metabolic medicine, and Mike Lean, professor of nutrition, University of Glasgow. The series will be published as a book by Blackwell Publishing in early 2007.
Competing interests: For series editors' competing interests, see the first article in this series.
References
- • Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001;285: 2486-97. [DOI] [PubMed] [Google Scholar]
- • Han TS, Lean ME, Seidell JC. Waist circumference remains useful predictor of coronary heart disease. BMJ 1996;312: 1227-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- • Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ 1995;311: 158-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- • Lissner L, Bjorkelund C, Heitmann BL, Seidell JC, Bengtsson C. Larger hip circumference independently predicts health and longevity in a Swedish female cohort. Obes Res 2001;9: 644-6. [DOI] [PubMed] [Google Scholar]
- • Must A, Jaques PF, Dallal GE, Bajema CJ, Dietz WH. Long term morbidity and mortality of overweight adolescents: a follow-up of the Harvard growth study of 1922 to 1935. N Engl J Med 1992;327: 1350-5. [DOI] [PubMed] [Google Scholar]
- • World Health Organization. Global strategy on diet, physical activity and health. www.who.int/dietphysicalactivity/publications/facts/obesity/ (accessed 25 Jun 2006)
- • National Heart, Lung, and Blood Institute. The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. 2000. www.nhlbi.nih.gov/guidelines/obesity/practgde.htm (accessed 25 Jun 2006)
- • WHO Expert Consultation. Appropriate body mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363: 157-63. [DOI] [PubMed] [Google Scholar]