Meningococcal disease produces a considerable global burden of disease. In this clinical review we focus mainly on meningococcal disease in the United Kingdom, but we also acknowledge the wider issues across the world. Meningococcal disease, which may present clinically as septicaemia, as meningitis, or with a mixed picture, is caused by infection with Neisseria meningitidis or meningococcus.
Recent advances include greater knowledge about the pathogenesis of meningococcal disease, work to facilitate its early diagnosis, and some evidence of improved outcomes after meningococcal disease. Despite these advances, valid evidence from large controlled studies is scarce, so most recommendations are based on consensus or tradition rather than on firm scientific evidence.
Description of the disease only as “meningitis” is inaccurate and misleading to patients and professionals. Septicaemia is the more dangerous clinical syndrome,1 which needs urgent treatment; meningitis also needs rapid treatment but is more likely to lead to neurodevelopmental sequelae. In the meningitis belt of sub-Saharan Africa, meningococcal disease presents predominantly as meningitis alone.2
Meningococcal infection
What causes it
The meningococcus is solely a human pathogen, and up to 50% of the population may carry meningococci in the nasopharynx.3 w1 Factors that lead to invasion and production of disease include complex inter-relationships of genetic predisposition, host status, environmental conditions, and virulence of the organism.4 w2
Literature searches
We searched Medline in May 2006 (PubMed, since 1966, except where stated) with the terms meningococcus, meningococcal infection, meningococcal disease, meningococcal disease and predisposition (English, reviews, past 5 years), meningococcal disease and carriage (English, reviews, past 5 years), meningococcal disease and symptoms, meningococcal disease and signs, meningococcal disease and treatment, meningococcal disease and outcome, and meningococcal disease and prevention. We also did a Google search, which found about 2.5 million references on meningococcal disease
Summary points
Meningococcal disease is the most common infectious cause of death in childhood in developed countries
Meningococcal disease presents as septicaemia, meningitis, or a combination
Septicaemia is the more dangerous presentation, especially with septic shock; meningitis is more likely to lead to neurodevelopmental sequelae
Correct terminology informs correct management and communication between professionals and with patients
Classic features of septicaemia are a non-blanching rash in a feverish, ill child
Most children with meningococcal disease survive; 15% have sequelae, including deafness and major and minor neurodevelopmental impairments
Amputations and abnormal bone growth resulting from necrosis have recently appeared as sequelae of meningococcal disease
Meningococci are assigned to at least 13 serogroups according to the antigenic nature of their capsules. Group A meningococci predominate in the African meningitis belt and groups B and C elsewhere, but other serogroups (W135, X, Y) are becoming increasingly important. Antibodies to the capsule provide protection against infection, as shown by the successful MenC vaccine. However, the group B capsule is a self antigen and is not readily useable as a vaccine.
Who gets it?
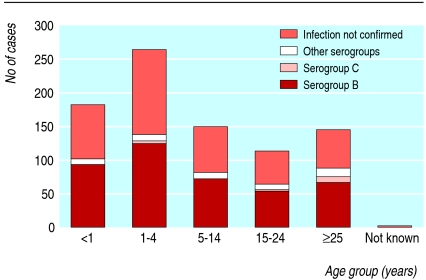
About 50% of meningococcal disease in the UK occurs in children aged under 4 years.5 Small increases in age related incidence occur in the late teenage years and above 65 years (fig 1). Incidence in the UK is around 5 per 100 000 population. In 2004, 1314 cases were notified—a significant drop from five years earlier.5 Meningococcal vaccine against type C disease was introduced in 1999 and may be responsible for some of this reduction.6 w3 Surveillance with enhanced methods suggests that actual cases total 50-80% more than laboratory confirmed cases.
Fig 1.
Serogroups of Neisseria meningitidis identified in cases in England and Wales by age: January to March 20057
How does it present?
As the organism spreads from the nasopharynx into the bloodstream, various infectious syndromes may be caused. In order of increasing duration of prodromal symptoms, children with meningococcal disease present with septicaemia, features of both septicaemia and meningitis, or meningitis; other rare presentations exist (box 1). In the UK, most children (more than 80%) with meningococcal disease present with some evidence of septicaemia. Other early symptoms include vomiting, diarrhoea, and myalgia. Some children (about 5%) present with features of septic shock but no rash. The clinical picture at presentation can be complicated still further by antecedent viral infection.
Box 1: Presentations of meningococcal disease
Septicaemia
Septicaemia and meningitis
Meningitis
Arthritis
Osteomyelitis
Conjunctivitis
Endophthalmitis
Chronic meningococcaemia
Course of meningococcal disease
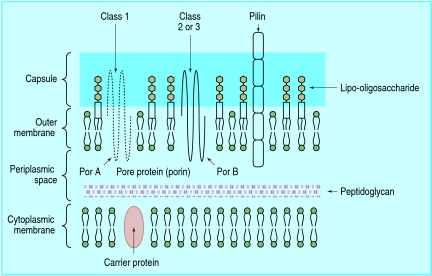
Children with meningococcal disease may become ill very rapidly. Blood bacterial loads quickly rise to very high levels (> 106/ml)8; most of the bacteria are dead, but they release blebs of outer membrane. This results in activation of the inflammatory cascade by meningococcal lipo-oligosaccharide from the wall of the organism (figs 2 and 3).9 This causes myocardial depression,10 endothelial dysfunction with extravasation of the circulating volume, and disseminated intravascular coagulation. Clinical signs of shock develop, with cool peripheries, poor capillary refill, a widening central-peripheral temperature gradient, tachycardia, and oliguria. Hypotension is a late sign in infants and young children, and its occurrence is ominous. Leaking of pulmonary fluid leads to pulmonary oedema, which may be heralded by tachypnoea and oxygen desaturation. Evolution of disease may proceed so fast that it outstrips any treatment that can be given (fig 4).
Fig 2.
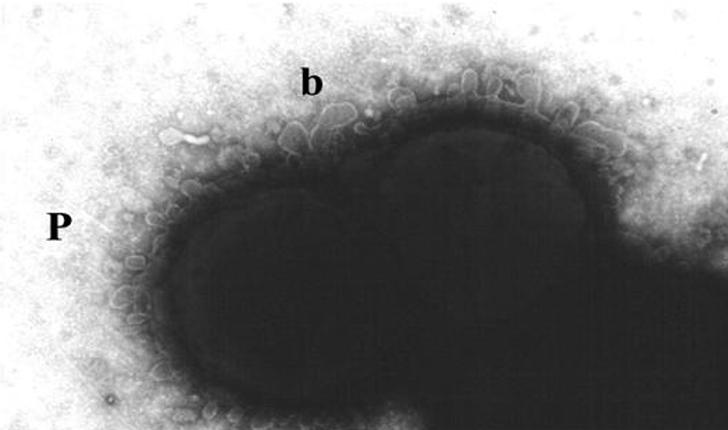
Electronmicrograph showing blebbing (b) of the outer membrane of Neisseria meningitides
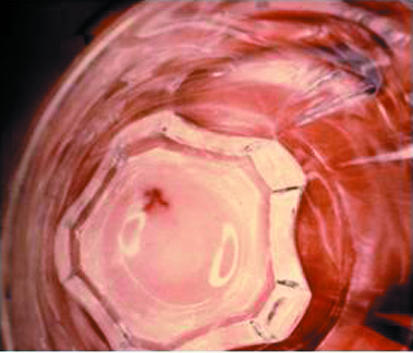
Fig 3.
Structure of cell wall of Neisseria meningitidis: 50% of the lipid in the outer leaflet of the outer membrane is lipo-oligosaccharide or endotoxin
Fig 4.


Evolution of non-blanching rash in meningococcal disease. Petechial, purpuric, and vasculitic elements are appearing. The pictures were taken 30 minutes apart. (Reproduced with permission from: Riordan FAI. Factors associated with mortality from meningococcal disease in Merseyside children (MD thesis). Liverpool University, 1995.)
How is it diagnosed?
The classic features of meningococcal sepsis are fever and a non-blanching rash in an ill child.11 Support literature promotes the “tumbler test” to parents as a way of confirming the non-blanching nature of the rash (fig 5). If the non-blanching rash is purpuric (more than 2 mm diameter) in an ill, febrile child then meningococcal disease is very likely. Up to 11% of children with an exclusively petechial rash will have meningococcal disease12; most of the rest have viral infections. The classic features may be preceded by viral infection-like non-specific symptoms. Up to 30% of children with meningococcal disease may present with a non-specific maculopapular rash (fig 6), although most will have non-blanching elements.13 Differentiating the nonblanching rash of meningococcal disease from viral rashes is almost impossible. (Most general practitioners will see thousands of children with non-specific, non-blanching rashes for every child presenting with meningococcal disease.)
Fig 5.

The “tumbler test” is a way of confirming the non-blanching nature of the rash
Fig 6.
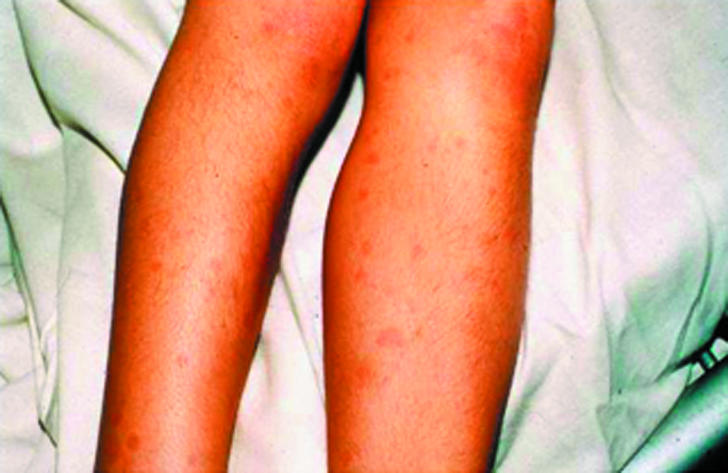
The maculopapular rash of meningococcal disease, indistinguishable from maculopapular rashes in viral infections. (Reproduced with permission from: Marzouk O. Clinical and laboratory aspects of childhood meningococcal disease (MD thesis). Liverpool, 1993.)
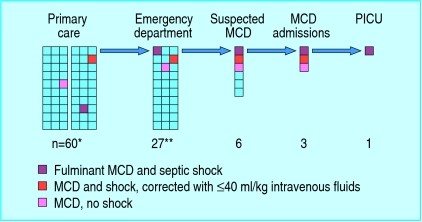
Some children present later in the course of the disease with features of meningitis (fever, headache, anorexia, vomiting, drowsiness, photophobia, stiff neck, positive Kernig's sign), as well as fever and a non-blanching rash; a small group present with classic features of meningitis but no rash and have the diagnosis confirmed at lumbar puncture. Recent evidence suggests that children who are subsequently admitted to paediatric intensive care units with septic shock have cold hands and feet and mottled skin early in their clinical course14; whether these features detected in primary care have a high positive predictive value for meningococcal disease is not clear (figs 7 and 8).
Fig 7.
Diagnostic and management pathway from primary care to paediatric intensive care unit (PICU): petechiae in children and meningococcal disease (MCD). (Each square represents one child.) *Range 30-180, but incidence of petechiae in primary care consultations for illness unknown. **Range 27-147, but incidence of petechiae in emergency department varies (Medline search May 2006)
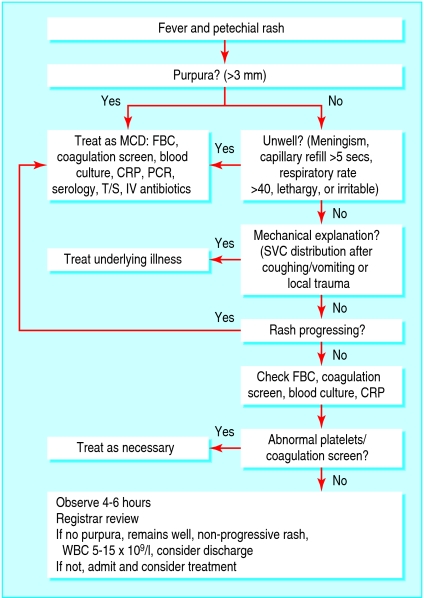
Fig 8.
Diagnosis of petechiae in children and meningococcal disease.15 CRP=C reactive protein; FBC=full blood count; IV=intravenous; MCD=meningococcal disease; PCR=meningococcal polymerase chain reaction; SVC=superior vena cava; T/S=throat swab for meningococci; WBC=white blood cells
Who suspects meningococcal disease?
Meningococcal disease presents as an emergency. With improving public information and media publicity, many parents recognise the significance of a nonblanching rash in an ill child and bring their child straight to the emergency department of a hospital. Some children who have been brought for an emergency consultation because they are nonspecifically unwell will be found to have a nonblanching rash on thorough examination or will develop it while under observation. Although their concerns should be respected, parents are not always accurate in their interpretation of symptoms and signs, and healthcare staff must examine children carefully and verify facts for themselves.
At the current incidence of the disease, and with the reduced exposure to ill children out of hours in primary care, an average general practitioner will see one case in his or her career in primary care and thus needs knowledge beyond experience.
How is meningococcal disease managed?
What should doctors do when they suspect meningococcal disease?
Box 2 summarises the management of meningococcal septicaemia. Doctors in primary care who suspect meningococcal disease, either septicaemia or meningitis, should give benzylpenicillin, intravenously if possible or intramuscularly if not, as recommended by the chief medical officer since 1988.16 Evidence favours pre-hospital antibiotic treatment.17 w4 (Recent UK data might be taken to contradict this, because they show that children who were given parenteral penicillin by a general practitioner had more severe disease on arrival at hospital than those who were not given parenteral penicillin.18 These children had a worse outcome, probably because their disease was worse to start with.w5)
Box 2: Management of meningococcal septicaemia
Prompt recognition by parents and primary and secondary care staff
Cefotaxime/penicillin within half an hour of recognition
Assessment of disease severity (Glasgow meningococcal septicaemia prognostic score)
Early recognition and vigorous treatment of shock (fluid and inotropes)
Early transfer of illest children for care in paediatric intensive care unit
Confirmation of the diagnosis (cultures, polymerase chain reaction)
Disease notification for infection control and prophylaxis
Full, accurate information to parents
Follow-up with hearing test
Delaying antibiotic treatment to assist with microbiological diagnosis is not appropriate, as newer methods of laboratory diagnosis (such as polymerase chain reaction for meningococcal DNA) are more sensitive than microbial culture and do not depend on live organisms.19 Box 3 describes the investigations available.
Hospital doctors who suspect meningococcal disease in a child should call for an experienced paediatrician.20 Assessment of children with suspected meningococcal disease is an urgent need. Hospital staff have validated diagnostic algorithms to follow, which focus attention on children with meningococcal disease. If diagnosis or management is delayed, the risk of death is increased.
Box 3: Investigations for meningococcal disease
Blood should be taken for full blood count, blood culture, and detection of meningococci by polymerase chain reaction. Patients who have been pretreated with antibiotics will still have a positive result on polymerase chain reaction for some time afterwards. Aspirates, smears, or punch biopsy may yield meningococci on microscopy, culture, serology, or polymerase chain reaction but are not routinely used.
Other investigations will include urea and electrolytes, glucose, clotting studies, fibrin degradation products (for septicaemia), and lumbar puncture with microscopy and culture (for meningitis) of cerebrospinal fluid as indicated by clinical circumstances. Lumbar puncture is not recommended in the acute phase of septicaemia but should be considered around 48 hours after physiological stabilisation, as confirmation of meningitis would alter the length of antibiotic course
What treatment is given in hospital?
Antibiotic treatment is needed urgently and ideally should be given within half an hour of arrival. Antibiotics should be continued in high doses if already given in primary care. Children with septicaemia, especially those with septic shock, will need intravenous fluid given promptly to correct shock and maintain the extracellular volume. Initial resuscitation with 20 ml/kg fluid may need to be repeated, but if more than 40 ml/kg has been given most children will need transfer to a paediatric intensive care unit. Inotropic support—dopamine, dobutamine, adrenaline (epinephrine)—may be started and then given in combination if response is suboptimal. Eventual infusion of fluid up to several times the circulating blood volume may be needed. Many articles and guidelines exist.11,6 w6
Children who have a Glasgow meningococcal septicaemia prognostic score of 8 or more out of 15 have an increased risk of death21; they should generally be transferred to a paediatric intensive care unit after elective intubation and placement of central line, arterial line, and catheter. Intermittent positive pressure ventilation, sedation, and restoration and maintenance of the central circulation are the mainstays of care in the paediatric intensive care unit. Anticytokine treatment with plasma exchange, haemofiltration, and other anti-inflammatory agents are variably offered to the sickest children: none has been proved to be effective.
Whether dexamethasone should be part of routine treatment of meningococcal meningitis in industrialised countries is not clear. It probably has a benefit in meningococcal meningitis if given before antibiotics. No advantage has been shown in meningococcal septicaemia.17 Cases of meningitis in paediatric intensive care units often need paediatric neurologist input.
Ongoing research
This falls into several main areas:
Why children acquire meningococcal disease and what protects others
How children with meningococcal disease can be diagnosed earlier
Identification of the components of the pathophysiology of the various presentations of meningococcal disease
Treatments in primary care, secondary care, and paediatric intensive care that will improve intact survival
Candidate vaccines for meningococcal serogroup B disease
What new treatments can we expect?
Elucidation of the pathophysiology of meningococcal septic shock has underpinned developments in treatment. Septic shock is mediated peripherally and centrally, the second of these through myocardial depression.22 This improved understanding has led to more rational inotropic prescribing and fluid management for the macrocirculation. Better support for the microcirculation may also be beneficial.
Unanswered questions
How prevalent are petechiae in children?
Can meningococcal disease be recognised earlier in primary care, before the classic non-blanching rash develops?
Do cold hands and feet and mottled extremities predict meningococcal disease in primary care?
How should children with petechiae who are relatively well and feverish (or fever-free) be managed?
How do bloodstream bacterial loads (> 106 bacteria/ml) reach such high levels so rapidly?
To what extent and until what point in the course of the disease does prompt treatment with antibiotics improve the outcome in meningococcal septicaemia?
Do corticosteroids benefit children with meningococcal septicaemia?
Can Neisseria lactamica be used to colonise the pharynx and prevent meningococcal disease?
Additional educational resources
Health Protection Agency. Meningococcal disease. (www.hpa.org.uk/infections/topics_az/meningo/menu.htm)
Communicable Disease Report. Laboratory reports of invasive meningococcal infections. (www.hpa.org.uk/cdr/archives/2005/cdr1605.pdf)
RCPCH/Meningitis Research Foundation project on meningococcal disease. Lessons from research for junior doctors. (www.meningitis.org)
Centers for Disease Control. Meningococcal disease. (www.cdc.gov/ncidod/dbmd/diseaseinfo/meningococcal_g.htm)
Centers for Disease Control. Health information for international travel. www2.ncid.cdc.gov/travel/yb/utils/ybGet.asp?section=dis&obj=menin.htm)
World Health Organization. Epidemic and pandemic alert and response: meningococcal disease.(www.who.int/csr/disease/meningococcal/en/index.html)
Correia JB, Hart CA. Meningococcal disease. Clin Evid 2004;12:1164-81. (www.clinicalevidence.com/ceweb/conditions/ind/0907/0907_contribdetails.jsp)
Information resources for patients
Meningitis Research Foundation (www.meningitis.org)—UK charity that funds research, promotes education and awareness, and gives support to people affected
Meningitis Trust (www.meningitis-trust.org)—International charity that provides support and education, raises awareness, and funds research
Meningococcal Education (www.meningococcal.com.au/)—Produces written information and educational videos and DVDs for the public and health professionals
GP tips
Do not think of meningococcal disease as only meningitis—septicaemia is more common and more dangerous
Suspect meningococcal disease in any child with a non-blanching rash, especially if ill and febrile
Give antibiotics in suspected meningococcal disease, as recommended by the chief medical officer
Immune modulation is the target for new treatments but has so far been disappointing.23 Trials of antiendotoxin treatment with monoclonal antibody or bactericidal permeability increasing protein have shown no benefit.24,25 Trials of treatment with activated protein C, which has shown a benefit in adult septic shock, are inconclusive in childhood meningococcal septicaemia; in meningococcal meningitis an increased risk of intracranial haemorrhage exists.
What other actions should be taken in hospital?
Meningococcal disease is a notifiable disease in the UK. Once the diagnosis has been established as clinically probable—or after laboratory confirmation—the consultant for communicable disease control should be notified. Chemoprophylaxis is indicated for household contacts.17 Usually, the hospital will be responsible for treating first degree relatives and chemoprophylaxis for other contacts will be arranged by the consultant for communicable disease control through primary care.
Information to parents
Full and accurate information for parents is especially necessary in meningococcal disease. This disease may evolve with frightening rapidity, and information given in the flurry of clinical activity may be confusing or misunderstood. A debriefing meeting before discharge and further discussion at follow-up may avert potential misinterpretation of events.
What are the outcomes of meningococcal disease?
Most children with meningococcal disease survive, although 8% die from septic shock and its complications. Improvements in outcome are likely to have resulted from multiple factors.26 w7 Among survivors, 10% have deafness, 10% have neurodevelopmental sequelae such as cerebral palsy, and 5% have more subtle neurodevelopmental abnormalities.27 Over the past 15 years, improved recognition and earlier treatment may have led to a higher survival rate, although data need to be examined carefully,w8 but with the emergence of “survival at a cost” peripheral amputations especially have increased.
How can meningococcal disease be prevented?
Capsular polysaccharide vaccines for serogroups A, C, Y, and W135 exist, and the conjugate MenC vaccine has been successfully introduced into the schedule of routine immunisation in the UK and has resulted in a dramatic decrease in serogroup C disease. Most meningococcal infection in the “meningitis belt” is with serogroup A organisms. Travellers to this area and pilgrims on the annual Hajj to Mecca are advised to be immunised against serogroup A disease. Vaccines for group B disease suitable for routine use in young children have not so far been developed. The possibility of protection against meningococcal disease by blocking pharyngeal binding with Neisseria lactamica is intriguing,w9 but it only tackles one aspect of the predisposing conditions for meningococcal infection.
A patient's story
J, aged 2 years and 6 months, became unwell over 12 hours with fever and vomiting. His parents found two petechial spots. They recognised these as non-blanching and brought him to the emergency department at midnight. On arrival, he was irritable and unwell but afebrile. He was tachycardic (150/minute) and normotensive, with a prolonged capillary refill time (more than 4 seconds). He had oxygen saturations of 100% in air and was breathing normally. Over the next hour a petechial and purpuric rash evolved all over his body. Venous access was established, and he was given intravenous cefotaxime within half an hour of arrival, followed by two boluses each of 20 ml/kg saline. An arterial line was sited, and he was transferred to the high dependency unit. His C reactive protein was moderately raised (58 mg/l) and his white cell count and differential were normal, but clotting studies were abnormal (platelets 146×109/l, international normalised ratio 1.5, prothrombin time ratio 2.3, with raised fibrinogen resulting from disseminated intravascular coagulation). His condition stabilised but then deteriorated steadily four hours later; he was ventilated and admitted to a paediatric intensive care unit 11 hours after the original admission. Before transfer, he needed resuscitation with 350 ml/kg fluid intravenously (normal saline, albumen 4.2%, fresh frozen plasma, and blood because of supervening anaemia, totalling more than four times his circulating blood volume since admission). Inotropes (dopamine, then dobutamine and adrenaline) were started. He was treated with haemofiltration for several days in intensive care. Blood culture was positive, and polymerase chain reaction confirmed Meningococcus serogroup B, serotype 15, subtype P1.4. He needed treatment for extensive skin scarring later, but he recovered fully and had no neurological detriment two years afterwards.
Supplementary Material
 Extra references w1-w9 are on bmj.com
Extra references w1-w9 are on bmj.com
Competing interests: Both authors have received research grants from the Meningitis Research Foundation. APJT acts as an expert witness (for claimants and defendants) on cases of meningococcal disease and meningitis.
References
- 1.Thomson APJ, Riordan FAI. The management of meningococcal disease. Current Paediatrics 2000;10: 104-9. [Google Scholar]
- 2.Molesworth AM, Thomson MC, Connor SJ, Creswell MP, Morse AP, Shears P, et al. Where is the meningitis belt? Defining an area at risk of epidemic meningitis in Africa. Epidemiol Infect 2002;96: 242-9. [DOI] [PubMed] [Google Scholar]
- 3.Yazdankhah SP, Caugant DA. Neisseria meningitidis: an overview of the carriage state. J Med Microbiol 2004;53: 821-32. [DOI] [PubMed] [Google Scholar]
- 4.Kvalsvig AJ, Unsworth DJ. The immunopathogenesis of meningococcal disease. J Clin Pathol 2003;6: 417-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Health Protection Agency. Laboratory reports of invasive meningococcal infections, England and Wales: weeks 50-53/2004. CDR Wkly (Online) 2005;15(16).
- 6.Gray SJ, Trotter CL, Ramsay ME, Guiver M, Fox AJ, Borrow R, et al. Epidemiology of meningococcal disease in England and Wales 1993/94 to 2003/04: contribution and experiences of the Meningococcal Reference Unit. J Med Microbiol 2006;55: 887-96. [DOI] [PubMed] [Google Scholar]
- 7.Health Protection Agency. Laboratory reports of invasive meningococcal infections, England and Wales: weeks 01-05/2005, 06-10/2005. CDR Wkly (Online) 2005;15(25).
- 8.Hackett SJ, Guiver M, Marsh J, Sills JA, Thomson APJ, Kaczmarski EB, et al. Meningococcal bacterial DNA load at presentation correlates with disease severity. Arch Dis Child 2002;86: 44-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hackett SJ, Thomson APJ, Hart CA. Cytokines, chemokines and other effector molecules involved in meningococcal disease. J Med Microbiol 2001;50: 847-59. [DOI] [PubMed] [Google Scholar]
- 10.Makwana N, Baines PB. Myocardial dysfunction in meningococcal septic shock. Curr Opin Crit Care 2005;11: 418-23. [DOI] [PubMed] [Google Scholar]
- 11.Riordan FAI, Thomson APJ, Sills JA, Hart CA. Who spots the spots? The diagnosis and treatment of early meningococcal disease in children. BMJ 1996;313: 1255-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wells LC, Smith JC, Weston VC, Collier J, Rutter N. The child with a nonblanching rash: how likely is meningococcal disease? Arch Dis Child 2001;85: 218-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marzouk O, Thomson APJ, Sills J, Hart CA, Harris F. Features and outcome in meningococcal disease presenting with maculopapular rash. Arch Dis Child 1991;66: 485-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson MJ, Ninis N, Perera R, Mayon-White R, Phillips C, Bailey L, et al. Clinical recognition of meningococcal disease in children and adolescents. Lancet 2006;367: 397-403. [DOI] [PubMed] [Google Scholar]
- 15.Richards C, Thimm A, Clark J, Thomson APJ, Newton T, Riordan FAI. The management of fever and petechiae: collaborative studies are needed. Arch Dis Child 2001;85: 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chief Medical Officer. Meningococcal infection. London: Department of Health, 1999. (PL/CMO/99/1).
- 17.Correia JB, Hart CA. Meningococcal disease. Clin Evid 2004;12: 1164-81. [PubMed] [Google Scholar]
- 18.Harnden A, Ninis N, Thompson M, Perera R, Levin M, Mant D, et al. Parenteral penicillin for children with meningococcal disease before hospital admission. BMJ 2006;332: 1295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hackett SJ, Carrol ED, Guiver M, Marsh J, Sills JA, Thomson APJ, et al. Improved case confirmation in meningococcal disease with whole blood Taqman PCR. Arch Dis Child 2002;86: 449-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ninis N, Phillips C, Bailey L, Pollock JI, Nadel S, Britto J, et al. The role of healthcare delivery in the outcome of meningococcal disease in children: case-control study of fatal and non-fatal cases. BMJ 2005;330: 1475-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riordan FAI, Marzouk O, Thomson APJ, Sills JA, Hart CA. Prospective validation of the Glasgow meningococcal septicaemia prognostic score: comparison with other scoring methods. Eur J Pediatr 2002;161: 531-7. [DOI] [PubMed] [Google Scholar]
- 22.Pathan N, Sandiford C, Harding SE, Levin M. Characterization of a myocardial depressant factor in meningococcal septicemia. Crit Care Med 2002;30: 2191-8. [DOI] [PubMed] [Google Scholar]
- 23.Carrol ED, Thomson APJ, Hart CA. New therapies and vaccines for meningococcal disease. Expert Opin Investig Drugs 2001;10: 1487-500. [DOI] [PubMed] [Google Scholar]
- 24.Derkx B, Wittes J, McCloskey RV, European Pediatric Meningococcal Septic Shock Trial Study Group. A randomised placebo-controlled trial of HA-1A, a human monoclonal anti-endotoxin antibody, in children with meningococcal septic shock. Clin Infect Dis 1999;28: 770-7. [DOI] [PubMed] [Google Scholar]
- 25.Levin M, Quint PA, Goldstein B, Barton P, Bradley JS, Shemie S, et al. Recombinant bactericidal/permeability-increasing protein (rBPI21) as adjunctive treatment for children with severe meningococcal sepsis: a randomised trial. Lancet 2000;356: 961-7. [DOI] [PubMed] [Google Scholar]
- 26.Thorburn K, Baines P, Thomson A, Hart CA. Mortality in severe meningococcal disease. Arch Dis Child 2001;85: 382-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fellick J, Sills JA, Marzouk O, Hart CA, Cooke RWI, Thomson APJ. Neurodevelopmental outcome in meningococcal disease: a case-control study. Arch Dis Child 2001;85: 6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.