The Case: A 63-year-old woman presented to the emergency department after experiencing uncontrollable, irregular jerking movements of her right arm for 1 week. The movements were increasingly painful and were making it difficult for her to sleep; however, they disappeared during sleep. She reported no other symptoms.
The patient had type 2 diabetes mellitus for 23 years, hypertension and arthritis. Cancer of the right breast had been treated with radiation and mastectomy 2 years before the current presentation. Her medications included tamoxifen, oxycodone, fentanyl, triazolam, enalapril, ranitidine, lasix, amitriptyline and indomethacin. She started taking insulin 10 years ago, with poor glycemic control. She checked her glucose infrequently and followed up with her family physician rarely. Blood glucose levels on test strips ranged from 20–30 mmol/L.
On examination the patient's vital signs were stable. Results of language testing, and cranial nerve and motor examinations were normal. There were continuous and irregular jerking movements of her right arm and hand and, to a lesser extent, her right leg. She could not willfully suppress the movements nor appreciably minimize them forcibly with the other hand. There was infrequent grimacing of the right side of her face (see video clip, available at www.cmaj.ca/cgi/content/full/175/8/871/DC1). Deep-tendon reflexes were absent in all limbs, and there was no Babinski sign. Vibratory sense was bilaterally diminished to the ankles. There was dysmetria in the right arm and leg and an unsteady gait, in keeping with the degree of involuntary movements.
The complete blood count and electrolyte, blood urea nitrogen, creatinine and calcium levels were normal. The random glucose level was elevated, at 17.2 (normal 3.3–11.0) mmol/L. Also elevated were the hemoglobin A1c concentration (13.8% [normal 4.3%– 6.1%]), creatine kinase level (668 [normal < 200] U/L) and cholesterol and triglyceride levels. A CT scan of the head showed hyperdensity of the left lentiform nucleus of the basal ganglia (Fig. 1).

Fig. 1: CT scan, showing hyperdensity of left lentiform nucleus of basal ganglia.
The preliminary impression of the emergency staff was of a functional disorder, and the patient was discharged to the referring hospital. The patient was called back for a formal neurologic assessment after the emergency department physician subsequently reviewed the history and CT scan with the neurology team. A diagnosis of hemichorea– hemiballismus as a complication of nonketotic hyperglycemia was made.
Multiple medications in different combinations were tried, including haloperidol, olanzapine, quetiapine, clonazepam and tetrabenazine, with minimal immediate benefit. Severe pain from the continuous right arm jerking was treated with morphine. Long-term tetrabenazine therapy for the hemichorea was continued, to which the patient had a satisfactory response. Subsequent testing for Wilson's and thyroid disease yielded negative results. An endocrinologist was consulted to optimize diabetic control.
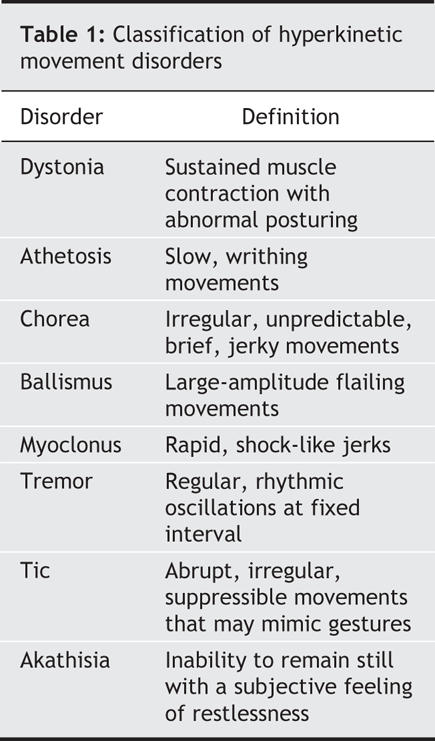
Hemichorea–hemiballismus (HC–HB) is a spectrum of involuntary, continuous, nonpatterned movements of one side of the body. It can be caused by a focal lesion of the contralateral basal ganglia or a diffuse systemic process (Box 1). Other abnormal movements must be distinguished from HC–HB (Table 1). Also, the possibility of continuous focal seizures (epilepsia partialis continua [EPC]) causing unilateral movements must be considered. EPC can occur secondary to hyperglycemia; however, the movements are usually regular and rhythmic and often have corresponding electroencephalogram abnormalities. EPC is often associated with cortical lesions rather than subcortical (basal ganglia) lesions. As a result, electroencephalography and brain MRI scanning are helpful in distinguishing these 2 entities, when history and examination do not provide sufficient information.1
Box 1.
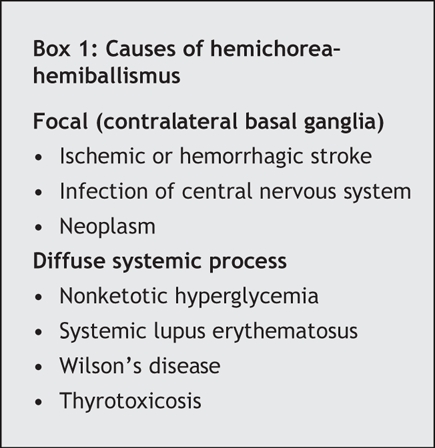
Table 1
Our patient had poorly controlled diabetes, and her HC–HB was a rare complication of nonketotic hyperglycemia. Between 1985 and 2001, only 53 case reports of this condition were published.2 The underlying pathophysiology leading to basal ganglia dysfunction is multifactorial. Recent imaging studies have shown reduced cerebral glucose metabolism on positron emission tomography (PET) scans, with concomitant hyperperfusion in the affected basal ganglia seen on single photon emission computed tomography (SPECT). These findings may suggest a local failure in vascular autoregulation in the setting of pre-existing microangiopathic disease and recurrent metabolic derangements.3
The basal ganglia in HC–HB appears hyperdense without mass effect on CT scans and hyperintense on T1-weighted MRI scans. In most cases, these imaging features completely reverse after therapy.2
The prognosis of HC–HB as a complication of nonketotic hyperglycemia is excellent.2 In a meta-analysis, 97% of patients had resolution of the abnormal movements within 6 months.3 Tight blood glucose control is sometimes sufficient to treat the hemichorea. More often, targeted monotherapy or combination therapy with neuroleptics is also required.2 Rarely surgical interventions, such as thalamotomy and deep brain stimulation, are considered.
Our case illustrates the diagnostic challenges of movement disorders and an association of one with a common medical condition. Unfamiliarity with these disabling conditions may result in their attribution to psychological or psychiatric disturbances. A high index of suspicion is warranted for neurologic consultation and investigation of patients with abnormal movements.
Haley Block James Scozzafava S. Nizam Ahmed Sanjay Kalra Division of Neurology Department of Medicine University of Alberta Edmonton, Alta.
Supplementary Material
Footnotes
Competing interests: None declared.
REFERENCES
- 1.Zumsteg D, Wennberg RA. A 61-year-old man with continuous clonic jerks of his right leg. CMAJ 2005;173(7):754-5. [DOI] [PMC free article] [PubMed]
- 2.Oh SH, Lee KY, Im JH, et al. Chorea associated with non-ketotic hyperglycemia and hyperintensity basal ganglia lesion on T1-weighted brain MRI study: a meta-analysis of 53 cases including four present cases. J Neurol Sci 2002;200:57-62. [DOI] [PubMed]
- 3.Hsu JL, Wang HC, Hsu WC. Hyperglycemia-induced unilateral basal ganglion lesions with and without hemichorea. A PET study. J Neurol 2004;251:1486-90. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


