Abstract
Intraoral local anesthesia is essential for delivering dental care. However, it is often perceived by some patients as the most painful and in some instances as the only painful part of the treatment, leading in extreme cases to avoidance of dental care. The present study measured the variables of pain, pressure, and discomfort caused by 4 commonly used local anesthesia injections: local infiltration, mental nerve block, inferior alveolar nerve block, and periodontal ligament injections. Patients were asked to grade pain, discomfort, and pressure on a visual analog scale as associated with needle insertion, operator finger position in the mouth, and pressure at injection. The inferior alveolar injection was graded to be the most painful followed by periodontal ligament and then mental nerve block injections. The periodontal ligament injections yielded the highest pressure scores. The inferior alveolar block injection yielded significantly more discomfort than local infiltration and mental nerve block injections when comparing finger and needle position. Local infiltration in the anterior maxillary region yielded the highest needle insertion and finger position discomfort scores. The present study suggests that the dental operator should be aware of local anesthesia injection pain, pressure, and discomfort together with efficacy of technique.
Keywords: Local anesthesia, Oral anesthesia, Injection pain
Local anesthetics (LAs) are the most widely used drugs in medicine and dentistry.1 They prevent nociception generated during surgical and dental procedures, and without LAs, many medical and dental procedures could not be performed. The injection of LAs is often the only perceived painful part of the medical or dental procedure, and fear associated with LA injection has been reported to be a factor in avoiding dental treatment.2 Numerous studies have examined possible variables that lead to this phenomenon. The purpose of this study was to assess the pain, pressure, and discomfort associated with commonly used traditional intraoral injections in a private office in an open, longitudinal study. The study attempted to establish baseline data on patient subjective responses to needle insertion sensation and pressure experienced with 4 oral LA injection procedures (infiltration, mental nerve block, inferior alveolar nerve block, and periodontal ligament [PDL] injection).
Previous studies have examined variables that might be involved in painful LA injections and tested possible ways of minimizing the discomforts perceived at the time of injection. Variables included tissue distensibility,1 speed of injection,3 and patient characteristics.4 The effects of temperature have also been examined. Rogers et al5 studied the effect of warming LA solutions injected into the buccal mucosa and found that this was no less painful than room temperature solution. Oikarinen et al6 injected prilocaine at 37°C and 21°C into the oral submucosa in 17 subjects and found that pain was experienced regardless of whether the solution was warmed or not. These researchers also noted that lower pH and addition of vasoconstrictor to the injection solution yielded more postoperative pain after anesthesia dissipated.
In a review article that examined the possible significance of the needle gauge in dental injections, Farsakian and Weine7 noted that the studies performed by Fuller et al,8 Mollen et al,9 and Brownbill et al10 all concluded that the “degree of pain was not related to needle gauge size.” Instead, Farsakian and Weine7 and other researchers11,12 promoted the hypothesis that the sharpness of the bevel, not the gauge, is important in pain avoidance. Pashley et al13 assessed the pressure created during dental LA procedures and revealed high values, ranging from 17,061–34,122 mm Hg. They stated that PDL injection created the second highest pressure after intraosseous injection and had similar values to an incisive papilla injection.
Another recent study examined the order effect of LA injections on pain and discomfort perception in children.14 Subjects were randomly given either maxillary infiltration or mandibular block on the first visit and vice versa on the second visit. It was found that the patients responded positively to both injections regardless of which was given initially. Preemptive topical anesthesia and electronic anesthesia were examined as a means of preventing or reducing pain during initial needle penetration and during the injection of LA.15 It was found that electronic anesthesia was more effective than topical anesthetics applied to the oral mucosa. Within the last few years, computerized syringes have been introduced with the promise of offering a reduction in pain and discomfort in intraoral injections.16–19 However, Grace et al20 and Ram and Peretz21 reported equal acceptance by both dentists and patients, with no difference in pain behavior to traditional and computer-controlled dental anesthetic injections.
METHODS
During a 3-month period, patients scheduled for routine dental restorative treatment in a private practice were asked to participate in the study. Treatment involved one or more teeth in the same quadrant, and none of the patients reported acute pain. Two hundred forty-seven patients classified by the American Society of Anesthesiologists (ASA) as healthy patients with localized pathological process (ASA I), patients with mild to moderate systemic disease (ASA II), or patients with severe systemic disease limiting activity but not incapacitating (ASA III) (confirmed by medical history) complied and signed an informed consent form. Sequential and longitudinal enrollment was performed by either of 2 operators, depending on who was in the office. One of 4 commonly used LA injection techniques was selected by the dentist according to accepted guidelines.1 Exclusion criteria were patients taking anti-inflammatory drugs; patients who abused drugs or alcohol; patients with a history of personality disorders; medically compromised patients with a status greater than ASA III; patients who did not demonstrate subjective signs of anesthesia or required a secondary injection; and patients who required sedative measures to deliver dental treatment. In all injection techniques, except PDL injection, a standard dental aspirating-type syringe (Pluraject 3M, Espe AG Dental Products, Seefeld, Germany) and 25-mm, 27-gauge needles were used. Intraoral injections in this study were used only as primary injections. If patients required a secondary or supplementary injection, they were excluded from the study.
Five basic techniques were used: local infiltration, mental nerve block, traditional inferior alveolar nerve block, palatal injection, and PDL injection. The PDL injections were administered with Citojet (Heraeus Kultzer Ltd., Hanau, Germany). However, since only 4 patients received a palatal injection, this technique was omitted from analysis, and only the remaining 4 groups were evaluated. All injection procedures followed the recommendations as described in The Handbook of Local Anesthesia.1 Before injection, a topical anesthetic gel (20% benzocaine, Beutlich Pharmaceuticals LP, Waukegan, Ill) was placed on the buccal mucosa. One minute later, LA was administered by the operator using room temperature 2% lidocaine plus epinephrine 1 : 100,000 (Lidocadren, Teva Pharmaceuticals, Petach Tikva, Israel) injected slowly (60 seconds), after aspiration (excluding PDL).
Before starting the dental procedure, patients completed a paper visual analog scale (VAS) questionnaire that reported their subjective response to the injection technique after receiving the injection. On the 100-mm VAS, 0 represented no pain, pressure, or discomfort, whereas 100 marked the highest score.22 Responses were measured for injection techniques, specifying pain, needle insertion, pressure, and finger position discomfort as marked on the VAS. A global evaluation of the entire injection procedure was recorded by the patients while the operator evaluated the patient’s response to injection. Global evaluation was recorded on a numerical scale, where 0 represented no pain, pressure, or discomfort and 10 represented the maximum possible score of these variables.23 The χ2 test was used to compare the 4 techniques for category variables (age, sex, tooth, and operator). The F test was used to compare the 4 groups of techniques for the continuous variables, and the Duncan multiple range test was used to compare group pairs.8 Tests were performed using SAS statistical software, version 6.12 (SAS Institute Inc, Cary, NC).
RESULTS
Two hundred forty-seven patients with uncomplicated medical histories (less than ASA III) participated in the study, including 90 males and 157 females. However, because of missing data, the final number of responses does not total 247 (VAS pain = 195, VAS needle = 246, VAS pressure = 235, VAS pressure discomfort = 245, VAS finger and needle position = 243) The average age was 31 years, ranging from 13 to 68.
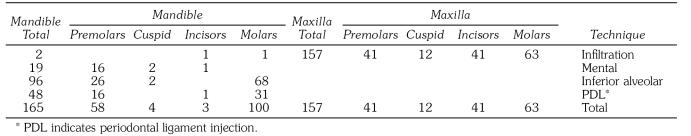
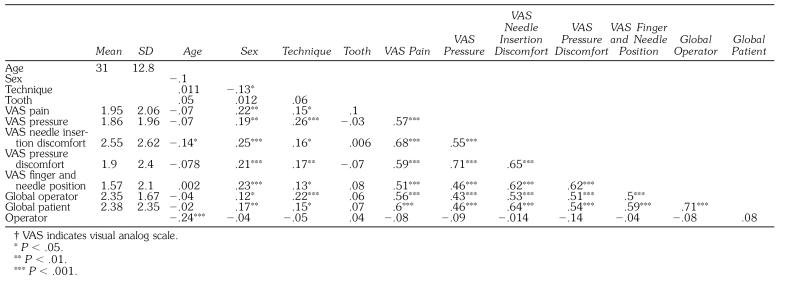
The distribution of LA techniques evaluated in the study is presented in Table 1. The variable means, SDs, and correlations are given in Table 2. The higher correlations (0.7) were found between VAS pain and VAS needle insertion discomfort, VAS pressure discomfort and VAS pressure, VAS pressure discomfort and VAS needle insertion discomfort, and global operator and global patient evaluation. However, they were not correlated with each other at a level higher than 0.80, which raises concern about serial correlation.24 Both operators treated groups that were age and sex homogenous (χ2 = 3). No statistically significant differences were found between patient age (P = .13) and sex (P = .11) in the 4 different technique groups. There were also no significant differences when incisors, bicuspids, cuspids, or molars were compared. The statistical elimination of the significance of age, sex, tooth location, or operator group made testing for differences in LA techniques alone possible.
Table 1.
Distribution of Teeth Tested According to Injection Technique Used
Table 2.
Means, SDs, and Correlations†
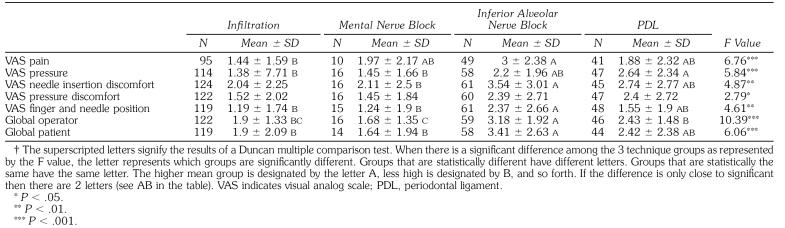
In all variables presented in Table 3, statistically significant differences occurred among the 4 techniques. In most of the variables, the technique of inferior alveolar nerve block had the highest values. Infiltration and mental nerve block techniques had the same results in most of the variables, which were significantly lower than the values of the inferior alveolar nerve block technique. The PDL injection technique yielded VAS values that fell between those of the infiltration and mental nerve block techniques and those of the inferior alveolar nerve block technique except for the pressure value.
Table 3.
Comparison Among the 4 Different Techniques and Dependent Variables†
The operators’ perception of patient response to various techniques suggested that inferior alveolar nerve block injection was significantly more painful than the other 3 techniques (P < .001). Similarly, patient global rating of inferior alveolar nerve block was significantly higher than the other 3, indicating more pain, pressure, and discomfort. The Duncan test did not differentiate among these techniques in VAS pressure discomfort. However, the F test result is significant, indicating that there is a significant difference between the techniques (F = 2.79 and P < .05). Similar findings were seen in inferior alveolar and PDL injections with greater discomfort reported. Pain response was generally higher in the inferior alveolar injection than in other techniques. The values in the PDL injection technique were similar to the inferior alveolar injection technique, with lower values for the mental nerve block and infiltration. Additionally, significantly higher pain values were found in maxillary incisors for verbal pain (P = .0001), VAS needle insertion discomfort (P = .0001), VAS finger and needle position (P = .01), global operator (P = .003), and global patient pain scores (P = .0001).
DISCUSSION
The present study evaluated and compared the pain, pressure, and discomfort induced by 4 commonly used intraoral LA injections. The results indicated that inferior alveolar nerve block was more painful than local infiltration or mental nerve block and PDL injection more painful than local infiltration and mental nerve block (for finger and needle position, operator scoring of patient perception, and patient global rating). These data suggest that for single tooth procedures in the mandible, the dental operator might seriously consider a less painful injection alternative to the inferior alveolar nerve block. Mansour and Adawy25 found that 96% of the patients claimed PDL injection was less painful than other techniques. Marin26 stated that patients reported hardly being aware of pain with PDL injection. Another study, which assessed pain scores during local infiltration and PDL injection, found no difference between the 2 injection techniques.21
The PDL injection is an option, but the practitioner must also take into account that VAS pressure is slightly higher with the PDL injection when compared with the other 3 techniques. Low-pressure, slow-delivery appa-ratuses, such as computerized syringes, should be evaluated as a possible means to minimize this variable. Also, if needle gauge has a minimum effect on pain perception on injection, then larger-diameter needles may be tested as an alternative for pressure reduction with PDL injection. When multiple tooth procedures are required, the Gow-Gates27 and Akinosi28 procedures, which were not tested in the present study, could be considered as an alternative to the inferior alveolar nerve block, and we suggest that future controlled studies test these 2 techniques for pain pressure and aversive perception at injection.
Despite the fact that local infiltration was found to be in general the least painful procedure with the least discomfort, our study points to significantly higher pain values for infiltration in maxillary incisors. These findings indicate that an alternative technique should be considered to minimize the pain at injection in maxillary incisors. The PDL injection again may possibly be a solution, as well as the palatal approach to anterior superior alveolar nerve.29 Devices such as needleless or jet syringes might also be considered, evaluated, and improved within this context.1
As this study indicates, the area being injected in the oral cavity has direct relation to pain and discomfort perception. Oral mucosa and periodontal ligament have an abundant number of free nerve endings, whereas the submucosa area has fewer.7 We suggest that further studies on nociception of needle contact with various oral tissues (attached gingival oral mucosa) and its relation to depth of penetration be designed. Finger and needle positioning during injection should also be further investigated to test possible patient preference for devices with a different design of needle control, such as pen grip syringes (such as Wand and Citojet, which claim to minimize digit interference in the oral cavity).
Relatively new computerized injection devices have claimed a reduction in pain and discomfort in intraoral injections. However, the dental community has been slow in adopting this technology. This has been attributed to a number of possible reasons. The high expense in buying the new syringes and disposable attachments, the length of injection time, the need for changing work routines, and the additional space needed for the device remain limiting factors.16,21 The accompanying new injection technique anterior and middle superior alveolar anesthesia or palatal-anterior superior alveolar injection, although on one hand offer an alternative way of controlling pain, on the other hand may also deter dentists who are hesitant in learning another injection skill and influence the decision in whether to use computerized local anesthesia administration.16,21,30,31 Therefore, although there is no doubt that computerized syringes will find their place in the armamentarium of pain control in dentistry, the present study concentrated on comparing the pain, pressure, and discomfort caused by traditional commonly used LA injections.
CONCLUSIONS
This study examined 4 traditional intraoral LA injection techniques in a longitudinal noncontrolled study that scaled their influence on patient perception of pain, pressure, and discomfort. The inferior alveolar injection was graded to be the most painful and produced the highest rates of discomfort. These findings suggest that whenever LAs are involved, dentists should consider not only efficacy of antinociception but also the perception of pain, pressure, and discomfort produced by the injection itself. There is a need for further research into the latest LA devices and techniques, computerized constant pressure devises, and jet syringes, which may yield lower pain, pressure, and discomfort scores. It is hoped that the findings of this present study can serve as baseline data of pain, pressure, and discomfort reactions for further comparative studies.
REFERENCES
- Malamed SF. St Louis, Mo: CV Mosby; 1997. Handbook of Local Anesthesia. 4th ed. [Google Scholar]
- Milgrom P. Four dimensions of fear of dental injections. J Am Dent Assoc. 1997;128:756–762. doi: 10.14219/jada.archive.1997.0301. [DOI] [PubMed] [Google Scholar]
- Rood JP. The pressures created by inferior alveolar injections. Br Dent J. 1978;144:280–282. doi: 10.1038/sj.bdj.4804079. [DOI] [PubMed] [Google Scholar]
- Dworkin SF. Psychological considerations for facilitating anesthesia and sedation in dentistry. In: Dionne RA, Laskin DM, editors. Anesthesia and Sedation in the Dental Office. New York, NY: Elsevier; 1986. pp. 15–28. [Google Scholar]
- Rogers KB, Allen FF, Markiewicz SW. The effect of warming local anesthetic solutions prior to injection. Gen Dent. 1989;37:496–499. [PubMed] [Google Scholar]
- Oikarinen VJ, Ylipaavalniemi P, Evers H. Pain and temperature sensations related to local anesthesia. Int J Oral Surg. 1975;4:151–156. doi: 10.1016/s0300-9785(75)80063-9. [DOI] [PubMed] [Google Scholar]
- Farsakian LR, Weine FS. The significance of needle gauge in dental injections. Compend Contin Educ Dent. 1991;12:262–268. [PubMed] [Google Scholar]
- Fuller NP, Menke RA, Meyers WJ. Perception of pain to three different intraoral penetrations of needles. J Am Dent Assoc. 1979;99:822–824. doi: 10.14219/jada.archive.1979.0384. [DOI] [PubMed] [Google Scholar]
- Mollen AJ, Ficara AJ, Provant DR. Needles −25 gauge versus 27 gauge—can patients really tell? Gen Dent. 1981;29:417–418. [PubMed] [Google Scholar]
- Brownbill JW, Walker PO, Bouncy BD, Keenan KM. Comparison of inferior dental nerve block injection in child patients using 30-gauge and 25 gauge short needles. Anesth Prog. 1987;34:215. [PMC free article] [PubMed] [Google Scholar]
- Forrest JO. A survey of the equipment of local anesthesia. Br Dent J. 1968;124:303. [PubMed] [Google Scholar]
- Lehtinen R. Penetration of 27-and 30-gauge dental needles. Int J Oral Surg. 1983;12:444–445. doi: 10.1016/s0300-9785(83)80036-2. [DOI] [PubMed] [Google Scholar]
- Pashley EL, Nelson R, Pashley DH. Pressure created by dental injections. J Dent Res. 1981;60:1742–1748. doi: 10.1177/00220345810600100301. [DOI] [PubMed] [Google Scholar]
- Ram D, Peretz B. Reactions of children to maxillary infiltration and mandibular block injections. Pediatr Dent. 2001;23:343–346. [PubMed] [Google Scholar]
- Quarnstrom F, Libed NE. Electronic anesthesia versus topical anesthesia for the control of injections pain. Quintessence Intl. 1994;25:713–716. [PubMed] [Google Scholar]
- Hochman M, Chiarello D, Hochman CB, Lopatkin R, Pergola S. Computerized local anesthetic delivery vs. traditional syringe technique. N Y State Dent J. 1997;63:24–29. [PubMed] [Google Scholar]
- Grace EG, Barnes DM, Macek MD, Tatum N. Patient and dentist satisfaction with a computerized local anesthetic injection system. Compend Cont Educ Dent. 2000;21:746–748. 750, 782. [PubMed] [Google Scholar]
- Ran D, Peretz B. Assessing the pain reaction of children receiving periodontal ligament anesthesia using a computerized device (Wand) J Clin Pediatr Dent. 2003;27:247–250. [PubMed] [Google Scholar]
- Allen KD, Kotil D, Larzelere RE, Hutfiess S, Beiraghi S. Comparison of a computerized anesthesia device with a traditional syringe in preschool children. Pediatr Dent. 2002;24:315–320. [PubMed] [Google Scholar]
- Grace EG, Barnes DM, Reid BC, Flores M, George D. Computerized local dental anesthetic systems: patient and dentist satisfaction. J Dent. 2003;31:9–12. doi: 10.1016/s0300-5712(02)00130-6. [DOI] [PubMed] [Google Scholar]
- Ram D, Peretz B. The assessment of pain sensation during local anesthesia using a computerized local anesthesia (Wand) and a conventional syringe. J Dent Child. 2003;70:130–133. [PubMed] [Google Scholar]
- Price DD, McGrath PA, Rafli A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17:45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- Heft MW, Parker SR. An experimental basis for revising the graphic rating scale of pain. Pain. 1984;19:153–161. doi: 10.1016/0304-3959(84)90835-2. [DOI] [PubMed] [Google Scholar]
- Kennedy P. Boston, Mass: MIT Press; 1984. A Guide to Econometrics. [Google Scholar]
- Mansour MS, Adawy AM. The periodontal ligament injection. Egyp Dent J. 1985;31:109–119. [PubMed] [Google Scholar]
- Marin MK. Intraseptal anesthesia in the general dental practice. Compend Contin Educ Dent. 1987;8:202–209. [PubMed] [Google Scholar]
- Gow-Gates GA. Mandibular conduction anesthesia. Oral Surg Oral Med Oral Pathol. 1973;36:321–328. doi: 10.1016/0030-4220(73)90208-9. [DOI] [PubMed] [Google Scholar]
- Akinosi JO. A new approach to the mandibular nerve block. Br J Oral Surg. 1977;15:83–87. doi: 10.1016/0007-117x(77)90011-7. [DOI] [PubMed] [Google Scholar]
- Allen KD, Kotil D, Larzelere RE, Hutfiess S, Beiraghi S. Comparison of a computerized anesthesia device with traditional syringe in preschool children. Pediatr Dent. 2002;24:315–320. [PubMed] [Google Scholar]
- Friedman JM, Hochman NM. A 21st century computerized injection system for local pain control. Compend Cont Educ Dent. 1997;18:995–1003. [PubMed] [Google Scholar]
- Hawkins JM, Moore PA. Local anesthesia: advances in agents and techniques. Dent Clin N Am. 2002;46:719–721. doi: 10.1016/s0011-8532(02)00020-4. [DOI] [PubMed] [Google Scholar]