Abstract
This study was conducted on 72 American Society of Anesthesiologists class 1 patients scheduled for extraction of a mandibular third molar after inferior alveolar nerve block. Each patient was randomly administered one of the following ropivacaine concentrations: 0.75%, 0.5%, 0.375%, or 0.25% (18 patients per group). Onset of block (mean ± SD) was rapid for both 0.75% (1.4 ± 0.4 minutes) and 0.5% (1.7 ± 0.5 minutes) ropivacaine but significantly slower for the 0.375% (4.2 ± 2.5 minutes) and 0.25% (10.7 ± 3.0 minutes) concentrations. Tooth extraction was performed successfully with the 0.5% and 0.75% concentrations, and supplemental injections were not required. Second injections, however, were required with 0.375% ropivacaine. Anesthesia was unsuccessful in 13 patients given 0.25% ropivacaine even after 3 injections. The mean durations of soft tissue anesthesia were 3.3 ± 0.3 hours and 3.0 ± 0.3 hours for the 0.75% and 0.5% concentrations, but significantly shorter with more dilute concentrations. The duration of analgesia showed a similar pattern, with the 0.75% and 0.5% concentrations producing prolonged analgesia of 6.0 ± 0.4 hours and 5.6 ± 0.4 hours. These results indicate that 0.5% and 0.75% concentrations were effective for intraoral nerve blockade, with both a rapid onset and prolonged duration of pain control.
Keywords: Ropivacaine, Local anesthesia, Local anesthetics, Dentistry, Oral surgery
Ropivacaine is a long-acting aminoamide local anesthetic structurally related to bupivacaine and mepivacaine.1 Its clinical profile is similar to that of bupivacaine but with fewer cardiac and central nervous system adverse effects.2 Various controlled clinical studies have demonstrated that ropivacaine is a suitable choice for peripheral nerve block.3,4 Axillary brachial plexus block with ropivacaine provides adequate anesthesia for hand surgery3; interscalene brachial plexus block with ropivacaine produces rapid onset of anesthesia and prolonged postoperative analgesia nearly twofold longer than with mepivacaine.5 Limited data are available concerning the use of ropivacaine in dental practice. It has been demonstrated that ropivacaine is equivalent in potency and efficacy to bupivacaine (both with 1 : 200,000 epinephrine) for maxillary anterior filtration.6 Although ropivacaine was not as effective as lidocaine with epinephrine in obtaining pulpal anesthesia after intraligamentary injection, adverse effects were minor and reversible.7 Two recent experimental trials indicate that ropivacaine may be suitable for intraoral nerve block anesthesia.8,9 This study was designed to determine an effective ropivacaine concentration that can be used in clinical dental practice for nerve blockade.
METHODS
After obtaining approval from the ethical committee of Tanta University and written informed consent of the participants, the study was conducted on 72 American Society of Anesthesiologists class 1 patients who required extraction of a mandibular third molar with inferior alveolar nerve blockade. No clinical or radiological evidence of infection or inflammation was permitted around the proposed surgical site. Also, patients could have no history of acute periodontal disease, trauma, or sensitivity. Patients received no analgesic drugs before the surgical procedure.
The anesthetic solutions were prepared by filling standard 1.8-mL local anesthetic cartridges with various concentrations of ropivacaine hydrochloride (Naropin, AstraZeneca Egypt, Cairo, Egypt) prepared by dilution of the 0.75% concentration with isotonic sodium chloride solution. Concentrations of 0.5%, 0.375%, and 0.25% were also used. Patients were randomly allocated to receive one of these concentrations by a standard inferior alveolar-lingual nerve block (with buccal infiltration).
The onset of mandibular anesthesia was assessed by asking the patient if altered sensation in the lower lip was present. An electric pulp tester (Analytic Technology, Redmond, Wash) was used to evaluate the depth of anesthesia. The experimental tooth and the contra-lateral mandibular canine (control tooth) were isolated with cotton rolls and dried with gauze. Toothpaste was applied to the probe tip that was placed midway between the gingival margin and the incisal edge of the tested tooth. By adjusting the rate control wheel to 1, the current was set to increase from no output (0) to the maximum output (80) over a 25-second period. No response from the patient to the maximum output of the pulp tester on 2 consecutive readings was used to indicate anesthesia.
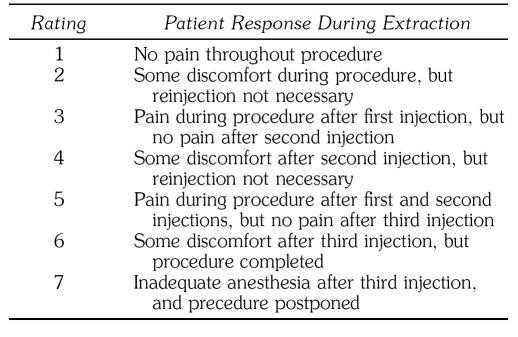
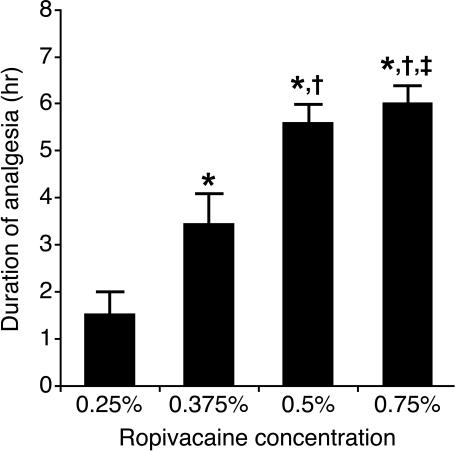
The quality of anesthesia during extraction was rated on a 7-point scale (Table 1). If adequate surgical anesthesia was not obtained, a second cartridge of test anesthetic solution was given; a third test cartridge was administered if the anesthesia was still incomplete. Patients not adequately anesthetized with the third cartridge were reappointed at a later time for extraction with a standard local anesthetic.
Table 1.
Quality of Anesthesia Rating Scale
The duration of anesthesia was determined by the time at which numbness was completely gone from the lower lip. The duration of analgesia was determined by the time when pain began at the mandibular extraction site.
Analysis of the data was performed with the Statistical Package for the Social Sciences. The Kruskal-Wallis test was used to detect the effect of each concentration, and post hoc testing was used to compare groups together. P values of ≤.05 and ≤.001 were used to indicate significant and highly significant differences, respectively.
RESULTS
Demographic details of the patients in the 4 groups are summarized in Table 2. The onset of anesthesia was rapid for both the 0.5% and 0.75% concentrations (Figure 1). There was a marginal statistical difference (P = .04) between the 2 concentrations, with the higher concentration slightly faster in onset (1.4 ± 0.4 minutes vs 1.7 ± 0.5 minutes). The 0.375% and 0.25% concentrations were much slower in onset (4.2 ± 2.5 minutes and 10.7 ± 3.0 minutes), and these differences were highly significant (P < .001) with respect to the higher concentrations and between each other.
Table 2.
Demographics of Patients
Figure 1. Mean onset time of anesthesia after ropivacaine nerve block (18 patients per group; each bracket indicates the standard deviation). *P < .001 compared with 0.25% ropivacaine; †P < .001 compared with 0.375% ropivacaine; and ‡ P < .05 compared with 0.5% ropivacaine.
The quality of anesthesia (Figure 2) revealed adequate (ratings 1 or 2) and similar (P = .20) surgical anesthesia with the 0.75% and 0.5% concentrations. Each tooth extraction was performed successfully, and there was no need for supplemental injections of local anesthetic intraoperatively. On the other hand, all patients in the 0.375% group required a second injection for adequate pain control. Individual quality of anesthesia ratings ranged from 3 to 5. There were highly significant differences (P < .001) between 0.375% ropivacaine and both higher concentrations and the 0.25% concentration, the last of which yielded quality ratings of 6 or 7, uniformly required a supplemental third injection and even then was unsuccessful in providing adequate pain control in 72% of patients.
Figure 2. Mean quality of anesthesia during surgery (18 patients per group; each bracket indicates the standard deviation). Rating scores are defined in Table 1. *P < .001 compared with 0.25% ropivacaine; †P < .001 compared with 0.375% ropivacaine.
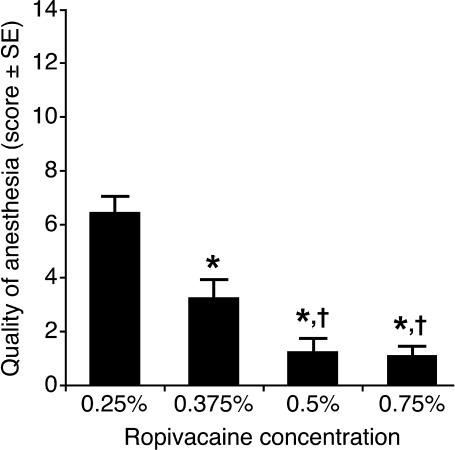
The duration of anesthesia is presented in Figure 3. There was a statistically (if not clinically) significant difference between the 0.75% concentration (3.3 ± 0.3 hours) and the 0.5% concentration (3.0 ± 0.3 hours, P = .006). Highly significant differences were recorded with both of these concentrations in comparison with the more dilute concentrations, which yielded mean durations of 2.3 ± 0.3 hours and 1.4 ± 0.4 hours for the 3.75% and 0.25% concentrations. The duration of analgesia (Figure 4) for the 0.25% concentration was essentially the same (1.5 ± 0.5 hours) as the duration of anesthesia; it was about 50% longer for the 0.375% concentration (3.5 ± 0.6 hours) and approximately 85% longer for the 0.5% (5.6 ± 0.4 hours) and 0.75% (6.0 ± 0.4) concentrations.
Figure 3. Mean duration of lip tissue anesthesia after ropivacaine nerve block (18 patients per group; each bracket indicates the standard deviation). *P < .001 compared with 0.25% ropivacaine; †P < .001 compared with 0.375% ropivacaine; and ‡P < .01 compared with 0.5% ropivacaine.
Figure 4. Mean duration of analgesia after ropivacaine nerve block (18 patients per group; each bracket indicates the standard deviation). *P < .001 compared with 0.25% ropivacaine; †P < .001 compared with 0.375% ropivacaine; and ‡P < .01 compared with 0.5% ropivacaine.
DISCUSSION
The speed with which neural block begins is proportional to the concentration of the local anesthetic solution.10 This study demonstrated that the onset of anesthesia was rapid for 0.75% and 0.50% ropivacaine, ranging from 1 to 2.2 minutes. Similar onset times (1 to 3.2 minutes) were recorded with 0.5% ropivacaine injected supraperiosteally for maxillary anesthesia.6 Some investigators5,11,12 have confirmed that increasing the concentration of ropivacaine reduces the onset time of peripheral nerve block, presumably because more local anesthetic molecules are available to penetrate the nerve per unit time. Akerman and associates1 attributed ropivacaine's tendency toward a more rapid onset of action in comparison with bupivacaine to its weaker binding to extraneural fat and tissues and to its greater availability for transfer to the site of action in the nerve. Conversely, the long duration of action of ropivacaine may be related partially to its vasoactivity, as a broad range of ropivacaine concentrations can cause vasoconstriction.1
The anesthetic potency of a local anesthetic depends, at least in part, on its physicochemical properties, which include the drug's lipid solubility expressed in terms of a lipid–water partition coefficient. As the partition coefficient increases, there is greater lipid solubility and higher local anesthetic potency. Among the injectable amides, unncharged ropivacaine is second only to uncharged bupivacaine in lipid solubility.13 Both the 0.75% and 0.5% concentrations produced adequate surgical anesthesia in this study. Tooth extraction was performed successfully, and no patient required supplemental injections of local anesthetic intraoperatively. Lower concentrations could not reliably produce adequate surgical anesthesia.
It has been reported that ropivacaine provides a concentration-dependent separation of sensory and motor effects.13 Several studies have found that sensory blockade is obtained with lower concentrations.14,15 Lower concentrations of ropivacaine may also have a selective analgesic effect because clinically they block thin Aδ and C nerve fibers more readily than large Aβ fibers.15 Although ropivacaine at low concentrations may be suitable for providing postoperative analgesia, as shown for outpatient hernia surgery performed under spinal anesthesia,4 higher concentrations are required for effective surgical anesthesia.1,16,17 The high concentrations used in this study provided both surgical anesthesia and postoperative analgesia, with pain relief significantly outlasting soft tissue numbness.
In conclusion, ropivacaine at concentrations of 0.5% and 0.75% was an effective local anesthetic for inferior nerve block, providing a rapid onset and prolonged duration. It may be a suitable local anesthetic without vasoconstrictor for nerve block anesthesia in dental practice.
REFERENCES
- Akerman B, Hellberg IB, Trossvik C. Primary evaluation of the local anaesthetic properties of the amino amide agent ropivacaine (LEA 103) Acta Anaesthesiol Scand. 1988;32:571–578. doi: 10.1111/j.1399-6576.1988.tb02788.x. [DOI] [PubMed] [Google Scholar]
- Knudsen K, Beckman Suurkula M, Blomberg S, Sjovall J, Edvardsson N. Central nervous and cardiovascular effects of IV infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997;78:507–514. doi: 10.1093/bja/78.5.507. [DOI] [PubMed] [Google Scholar]
- Salonen MHA, Haasio J, Bachmann M, Xu M, Rosenberg PH. Evaluation of efficacy and plasma concentrations of ropivacaine in continuous axillary brachial plexus block: high dose for surgical anesthesia and low dose for postoperative analgesia. Reg Anesth Pain Med. 2000;25:47–51. doi: 10.1016/s1098-7339(00)80010-3. [DOI] [PubMed] [Google Scholar]
- Mulroy MF, Burgess FW, Emanuelsson BM. Ropivacaine 0.25% and 0.5%, but not 0.125%, provide effective wound infiltration analgesia after outpatient hernia repair, but with sustained plasma drug levels. Reg Anesth Pain Med. 1999;24:136–141. doi: 10.1016/s1098-7339(99)90074-3. [DOI] [PubMed] [Google Scholar]
- Casati A, Fanelli G, Aldegheri G, et al. Interscalene brachial plexus anaesthesia with 0.5%, 0.75% or 1% ropivacaine: a double-blind comparison with 2% mepivacaine. Br J Anaesth. 1999;83:872–875. doi: 10.1093/bja/83.6.872. [DOI] [PubMed] [Google Scholar]
- Kennedy M, Reader A, Beck M, Weaver J. Anesthetic efficacy of ropivacaine in maxillary anterior infiltration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:406–412. doi: 10.1067/moe.2001.114000. [DOI] [PubMed] [Google Scholar]
- Meechan JG. A comparison of ropivacaine and lidocaine with epinephrine for intraligamentary anesthesia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:469–473. doi: 10.1067/moe.2002.121390. [DOI] [PubMed] [Google Scholar]
- Axelsson S, Isacsson G. The efficacy of ropivacaine as a dental local anaesthetic. Swed Dent J. 2004;28:85–91. [PubMed] [Google Scholar]
- Ernberg M, Kopp S. Ropivacaine for dental anesthesia: a dose-finding study. J Oral Maxillofac Surg. 2002;60:1004–1010. doi: 10.1053/joms.2002.34409. [DOI] [PubMed] [Google Scholar]
- Denson DD, Mazoit JX. Physiology, pharmacology, and toxicity of local anesthetic: adult and pediatric concentrations. In: Raj PP, editor. Clinical Practice of Regional Anesthesia. New York, NY: Churchill Livingstone; 1991. [Google Scholar]
- Casati A, Fanelli G, Borghi B, Torri G. for the Study Group on Orthopedic Anesthesia of the Italian Society of Anesthesia, Analgesia and Intensive Care. Ropivacaine or 2% mepivacaine for lower limb peripheral nerve blocks. Anesthesiology. 1999;90:1047–1052. doi: 10.1097/00000542-199904000-00018. [DOI] [PubMed] [Google Scholar]
- Casati A, Fanelli G, Cedrati V, Berti M, Aldegheri G, Torri G. Pulmonary function changes after interscalene brachial plexus anesthesia with 0.5% and 0.75% ropivacaine: a double-blinded comparison with 2% mepivacaine. Anesth Analg. 1999;88:587–592. doi: 10.1097/00000539-199903000-00024. [DOI] [PubMed] [Google Scholar]
- Wildsmith JAW. Peripheral nerve block and ropivacaine. Am J Anesthesiol. 1997;24(suppl 5):14–17. [Google Scholar]
- Rosenberg PH, Heinonen E. Differential sensitivity of A and C nerve fibres to long-acting amide local anaesthetics. Br J Anaesth. 1983;55:163–167. doi: 10.1093/bja/55.2.163. [DOI] [PubMed] [Google Scholar]
- Wildsmith JAW, Brown DT, Paul D, Johnson S. Structure-activity relationships in differential nerve block at high and low frequency stimulation. Br J Anaesth. 1989;63:444–452. doi: 10.1093/bja/63.4.444. [DOI] [PubMed] [Google Scholar]
- Whitehead E, Arrigoni B, Bannister J. An open study of ropivacaine in extradural anaesthesia. Br J Anaesth. 1990;64:67–71. doi: 10.1093/bja/64.1.67. [DOI] [PubMed] [Google Scholar]
- Koinig H, Krenn CG, Glaser C, et al. The dose-response of caudal ropivacaine in children. Anesthesiology. 1999;90:1339–1344. doi: 10.1097/00000542-199905000-00018. [DOI] [PubMed] [Google Scholar]