Abstract
The aim of this study is to assess the difference in duration of action after infiltration anesthesia when elevation of a periosteal flap (EPF) was accomplished with water or saline irrigation versus nonelevation of a periosteal flap (NEPF). The 57 patients in this study were under conscious sedation. A long treatment time of more than 1 hour was used. Instances where peripheral nerve block or opioids were administered and infiltration anesthesia over 2 fields were excluded before the study. Patients were included in either an EPF group (n = 29) or an NEPF group (n = 28). Statistically significant differences were detected in the initial dose of anesthetic (EPF: 4.3 ± 1.4 mL, NEPF: 1.8 ± 0.9 mL), the time until initial supplemental anesthesia (EPF: 38 ± 26 minutes, NEPF: 65 ± 27 minutes), and the frequency of anesthesia administration (EPF: 2.5 ± 1.2 times, NEPF: 1.3 ± 0.7 times). These results suggest that the duration of anesthesia action in EPF decreases to half compared with NEPF, even if the anesthetic was infiltrated in double the amount. Although supplemental anesthesia is required frequently in EPF, it is not efficacious. We speculated that the residual anesthetics in tissue were washed out by irrigation and hemorrhage and that supplemental anesthesia became ineffective because of leakage from the opened flap. Elevation of a periosteal flap reduces the effect of infiltration anesthetics.
Keywords: Infiltration anesthesia, Local anesthesia, Lidocaine, Epinephrine, Oral surgery, Periosteal flap
Success of conscious sedation for minor oral surgery depends on effective local anesthesia. However, in clinical situations we occasionally experience cases where conscious sedation becomes difficult because of insufficient local anesthesia effect. We found insufficient local anesthesia more often during elevation of a periosteal flap (EPF) with water or saline irrigation to the bone during minor oral surgery. In these cases there was a reduction in the duration of action of infiltration anesthesia. Therefore, we assessed the difference in the duration of action of infiltration anesthesia for dental procedures with EPF with water or saline irrigation versus nonelevation of periosteal flap (NEPF), retrospectively.
METHODS
During 2002 we managed 165 cases with conscious sedation and local anesthesia. Hemodynamic monitoring was performed for all dental procedures. We performed conscious sedation for patients who reported dental phobia or a gagging or vomiting response to dental therapy and for those with cardiopulmonary disease. Fifty-seven patients who required long procedures of more than 1 hour were enrolled in the study. The use of peripheral nerve block or opioids and infiltration anesthesia over 2 fields were excluded from the study. These patients were included in either an EPF group (n = 29: 15 cases of impacted tooth extraction, 10 cases of api-coectomy and cystectomy, 2 cases of periodontal flap procedures, and 2 cases of implant surgery) or an NEPF group (n = 28: 12 cases of tooth preparation, 11 cases of pulp extirpation, and 5 cases of tooth extraction). The initial dose of infiltration anesthesia, the time until supplementation of anesthesia, and the frequency of infiltration anesthesia were compared within these 2 groups. If there was no supplementation, the time until the completion of procedure was used. The data were analyzed from the intraoperative management records. Statistical analysis was performed by Mann-Whitney U test and 2 × 2 chi-square test. Significance was considered at P < .05.
RESULTS
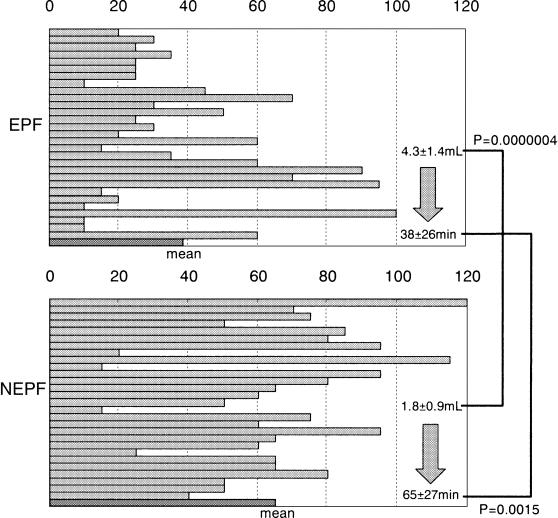
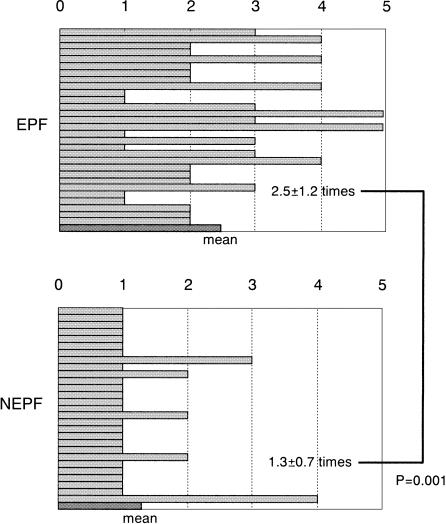
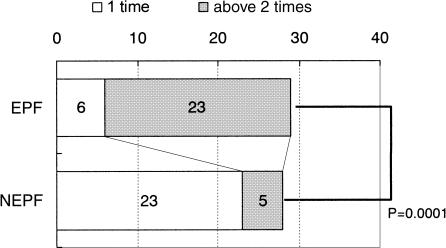
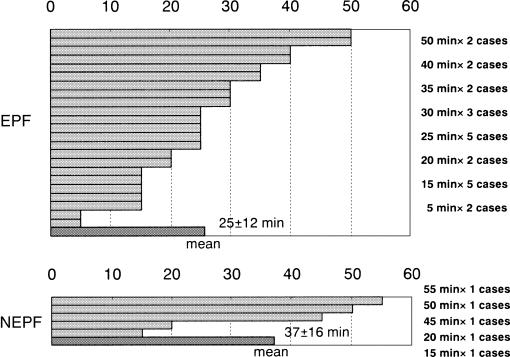
Regarding age and gender, there was no statistically significant difference (P = .0801, P = .42) between EPF (43 ± 17 years, M : F = 14 : 15) and NEPF (45 ± 18 years, M : F = 17 : 11). Each patient received 2% lidocaine with 1 : 80,000 epinephrine infiltrated as the local anesthetic and was sedated with propofol or midazolam. For the initial dose of anesthesia, there was a statistically significant difference (P = .0000004) between EPF (4.3 ± 1.4 mL, 2–7.2 mL) and NEPF (1.8 ± 0.9 mL, 0.3–4.4 mL). There was also a statistically significant difference (P = .0015) between EPF (38 ± 26 minutes, 10–100 minutes) and NEPF (65 ± 27 minutes, 15–120 minutes) (Figure 1) for the time until initial supplemental infiltration anesthesia and a statistically significant difference (P = .0001) between EPF (2.5 ± 1.2 times, 1–5 times) and NEPF (1.3 ± 0.7 times, 1–4 times) (Figure 2) when evaluating the frequency of infiltration anesthesia. Furthermore, in the ratio of a single infiltration versus multiple infiltrations, there was a statistically significant difference (P = .00001) between EPF (6 : 23) and NEPF (23 : 5) (Figure 3). The mean interval of multiple anesthetic infiltrations was 25 ± 12 minutes (range 5–50 minutes) in the 23 cases of EPF and 37 ± 16 minutes (range 15–55 minutes) in the 5 cases of NEPF (Figure 4). However, no statistically significant difference was detected, possibly because of the small sample size (NEPF n = 5).
Figure 1. The time (minutes) until initial supplemental infiltration anesthesia. During the period of the initial dose of infiltration anesthetics, there was a significant difference (P = .0000004) between elevation of a periosteal flap (EPF) (4.3 ± 1.4 mL, 2–7.2 mL) and nonelevation of a periosteal flap (NEPF) (1.8 ± 0.9 mL, 0.3–4.4 mL). During the period before initial supplemental infiltration anesthesia, there was a significant difference (P = .0015) between EPF (38 ± 26 minutes, 10–100 minutes) and NEPF (65 ± 27 minutes, 15–120 minutes).
Figure 2. The frequency of infiltration anesthesia. There was significant difference (P = .0001) between elevation of a periosteal flap (2.5 ± 1.2 times, 1–5 times) and nonelevation of a periosteal flap (1.3 ± 0.7 times, 1–4 times).
Figure 3. Ratio differences in the frequency of anesthesia infiltration. There was a significant difference (P = .00001) between elevation of a periosteal flap (6 : 23) and nonelevation of a periosteal flap (23 : 5).
Figure 4. The mean interval of multiple anesthetic infiltration was 25 ± 12 minutes (5–50 minutes) in 23 cases of elevation of a periosteal flap and 37 ± 16 minutes (15–55 minutes) in the 5 cases of nonelevation of a periosteal flap (NEPF). However, the small sample size in the NEPF group prevented a significant difference from being detected.
DISCUSSION
In our intraoperative management records, supplemental infiltration anesthesia was required because of discomfort reported by the patient. This tells us that infiltration anesthesia became ineffective during the short procedure. In fact, conscious sedation began to fail when the infiltration anesthesia became ineffective. Therefore, our results suggest that the duration of infiltration anesthesia action in EPF decreased to half in comparison with NEPF, even if the anesthetic amount in EPF was doubled that of NEPF. In cases where EPF was used, supplemental infiltration anesthesia was required frequently, and even then it proved to be less than efficacious. We speculate that the residual anesthetic that was retained in the bone and subperiosteal space was washed out, for the bone surface and tissue were directly sprayed and irrigated with water or saline. Furthermore, there is the possibility that hemorrhage from the bone surface also washed out the residual anesthetic. In that case, supplemental infiltration anesthesia does not prove efficacious because it leaks easily from the opened flap. Further research is suggested in an attempt to duplicate our findings. Specifically, we will have to compare the residual anesthetic concentration in the bone in both EPF and NEPF procedures after infiltration anesthesia. Another way to obtain these data may be to measure the anesthetic concentration in the blood and irrigation water or saline that is aspirated from the operative field of the patient.
Our hospital uses cartridges of 2% lidocaine with 1 : 80,000 epinephrine as our anesthetic of choice. 2% Lidocaine with 1 : 80,000–1 : 100,000 epinephrine is the gold standard as an infiltration anesthetic in many dental procedures.1–11 One advantage of 2% lidocaine with 1 : 80,000 epinephrine is that it reduces hemorrhage from the operative field better than many other drugs.1,2 The duration of action of infiltration anesthesia with 2% lidocaine with 1 : 80,000–1 : 100,000 epinephrine is 120–180 minutes,1–10 which is almost the same as 3% mepivacaine, 4% prilocaine, 4% articaine with 1 : 200,000 epinephrine, and 3% prilocaine with 0.3 U felypressin.3–5 However, the duration of anesthesia in our study (EPF: 38 ± 26 minutes, NEPF: 65 ± 27 minutes) was shorter than previous research demonstrated. We used the time until completion of the procedure if there was no supplemental infiltration. Most previous publications used the time until complete disappearance of anesthesia. Another difference between our study and most other data is that most previous studies focused on noninvasive procedures whereas our data included invasive dental therapy. Some studies have found that 1.5% etidocaine with 1 : 200,000 epinephrine and 0.5% bupivacaine with 1 : 200,000 epinephrine has a clinical duration of action of 1.75–2.16 times longer than 2% lidocaine with 1 : 80,000–1 : 100,000 epinephrine.1,2,6–10 Patients sometimes consider unnecessarily long duration of action of anesthesia to be uncomfortable,3 but long-acting anesthetics should be considered for the cases such as EPF in our study. One problem is that neither etidocaine nor bupivacaine is packaged in an anesthetic cartridge in Japan.
However, concomitant use of a peripheral nerve block may be used to prolong the analgesic duration of the local anesthetic.11 We have to consider that a peripheral nerve block often includes increased discomfort, facial palsy, local anesthetic overdose, intoxication, hypertension, vagal reflex activation, trismus, infection, hematoma, and neuroparalysis, among other effects. In addition, peripheral nerve blocks do not reduce intraoperative blood loss because the vasoconstrictor does not act within the operative field.1,2 Peripheral nerve blocks also do not anesthetize the buccal nerve. Therefore, we often administer analgesics such as opioids during conscious sedation when local anesthesia becomes ineffective. There were many cases of ineffective local anesthesia that required removal of those cases from this study. We preferred to avoid the administration of opioids to ambulatory patients because opioids in Japan (fentanyl, pethidine [meperidine], morphine, butorphanol, pentazocine, buprenorphine) are too long acting.
Therefore, success of conscious sedation for minor oral surgery depends on the effective local anesthesia. We must consider both treatment time and whether sedation is indicated when minor oral surgery with EPF is planned. We may choose general anesthesia for cases where the surgical operating time may exceed 38 ± 26 minutes.
REFERENCES
- Sisk AL. Comparison of etidocaine and lidocaine for control of intra- and post-operative bleeding and pain. J Oral Maxillofac Surg. 1986;44:16–20. doi: 10.1016/0278-2391(86)90009-1. [DOI] [PubMed] [Google Scholar]
- Sisk AL, Dionne RA, Wirdzek PR. Evaluation of etidocaine hydrochloride for local anesthesia and postoperative pain control in oral surgery. J Oral Maxillofac Surg. 1984;42:84–88. doi: 10.1016/0278-2391(84)90316-1. [DOI] [PubMed] [Google Scholar]
- Hersh EV, Hermann DG, Lamp CJ, Johnson PD, MacAfee KA. Assessing the duration of mandibular soft tissue anesthesia. J Am Dent Assoc. 1995;126:1531–1536. doi: 10.14219/jada.archive.1995.0082. [DOI] [PubMed] [Google Scholar]
- Vahatalo K, Antila H, Lehtinen R. Articaine and lidocaine for maxillary infiltration anesthesia. Anesth Prog. 1993;40:114–116. [PMC free article] [PubMed] [Google Scholar]
- Nordenram A, Danielsson K. Local anaesthesia in elderly patients. An experimental study of oral infiltration anaesthesia. Swed Dent J. 1990;14:19–24. [PubMed] [Google Scholar]
- Crout RJ, Koraido G, Moore PA. A clinical trial of long-acting local anesthetics for periodontal surgery. Anesth Prog. 1990;37:194–198. [PMC free article] [PubMed] [Google Scholar]
- Giovannitti JA, Bennett CR. The effectiveness of 1.5% etidocaine HCl with epinephrine 1:200,000 and 2% lidocaine HCl with epinephrine 1:100,000 in oral surgery: a clinical comparison. J Am Dent Assoc. 1983;107:616–618. doi: 10.14219/jada.archive.1983.0299. [DOI] [PubMed] [Google Scholar]
- Laskin JL. Use of etidocaine hydrochloride in oral surgery: a clinical study. J Oral Surg. 1978;36:863–865. [PubMed] [Google Scholar]
- Laskin JL, Wallace WR, DeLeo B. Use of bupivacaine hydrochloride in oral surgery-a clinical study. J Oral Surg. 1977;35:25–29. [PubMed] [Google Scholar]
- Nespeca JA. Clinical trials with bupivacaine in oral surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1976;42:301–307. doi: 10.1016/0030-4220(76)90163-8. [DOI] [PubMed] [Google Scholar]
- Danielsson K, Evers H, Holmlund A, Kjellman O, Nordenram A, Persson NE. Long-acting local anaesthetics in oral surgery. Clinical evaluation of bupivacaine and etidocaine for mandibular nerve block. Int J Oral Maxillofac Surg. 1986;15:119–126. doi: 10.1016/s0300-9785(86)80131-4. [DOI] [PubMed] [Google Scholar]