Abstract
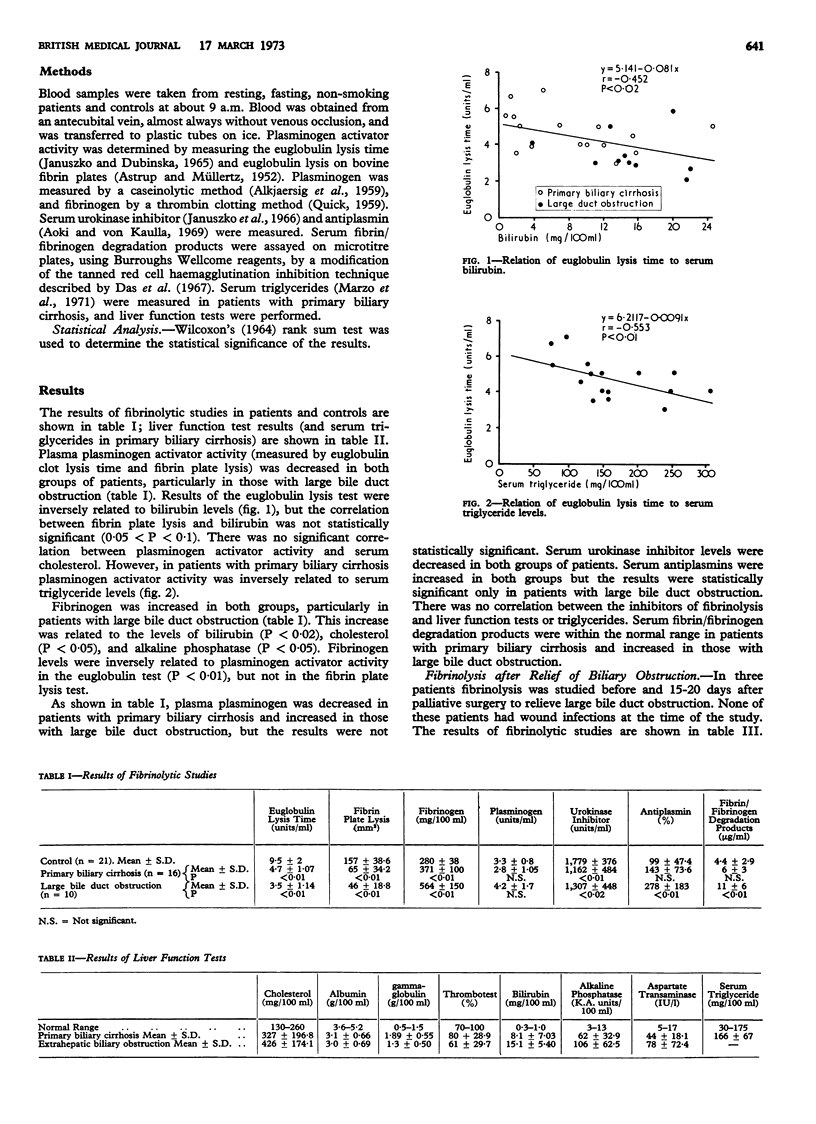
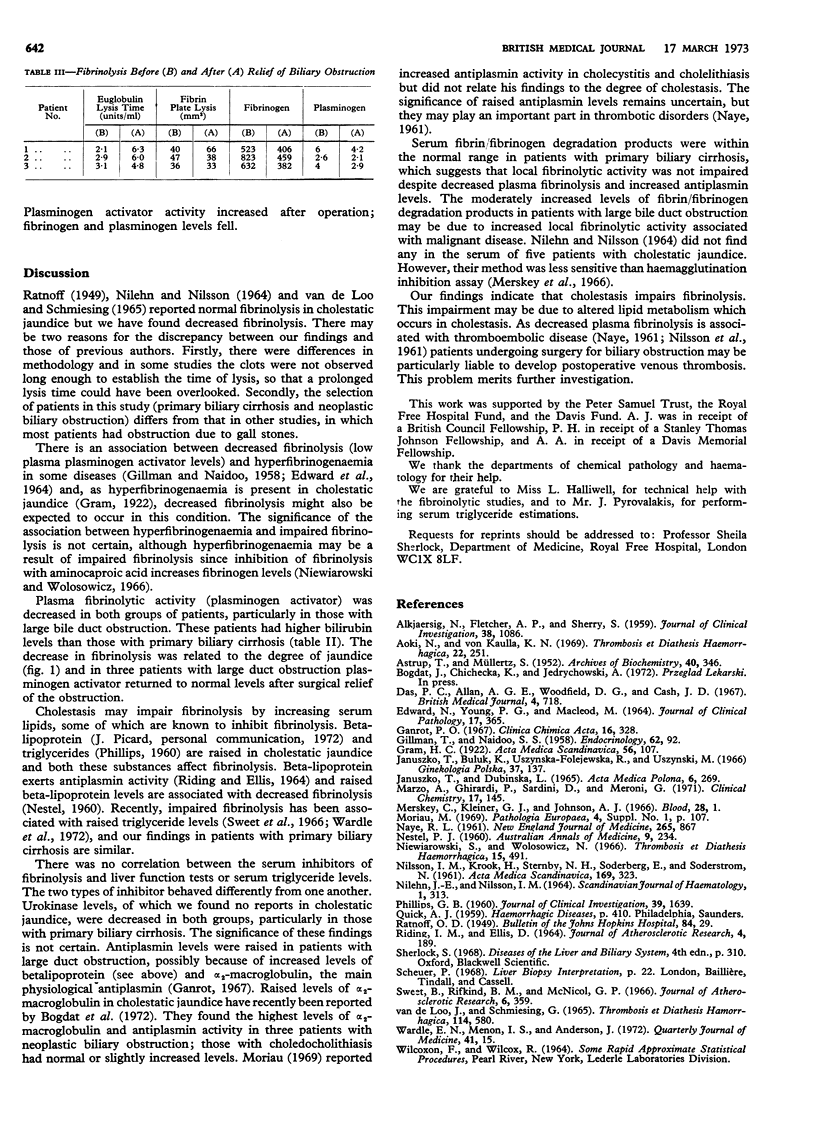
The fibrinolytic system was studied in primary biliary cirrhosis (16 patients) and large bile duct obstruction (10 patients, nine of whom had carcinoma). Plasma fibrinolysis (plasminogen activator activity) was decreased and fibrinogen increased in both groups of patients, particularly in those with large duct obstruction. These changes were related to the degree of cholestasis. Plasminogen activator activity was inversely related to serum triglyceride levels in patients with primary biliary cirrhosis. Urokinase inhibitors were decreased in both groups and antiplasmins increased in patients with large duct obstruction; fibrin/fibrinogen degradation products were normal in primary biliary cirrhosis and moderately increased in large duct obstruction. None of these fibrinolytic indices was related to the degree of cholestasis. Fibrinolytic activity and fibrinogen returned almost to normal levels after palliative surgery in the three patients with large duct obstruction who were studied. The decreased plasma fibrinolysis and increased fibrinogen may be due to altered lipid metabolism in cholestatic jaundice. In patients undergoing surgery for large duct obstruction there may be an increased risk of thrombosis.
Full text
PDF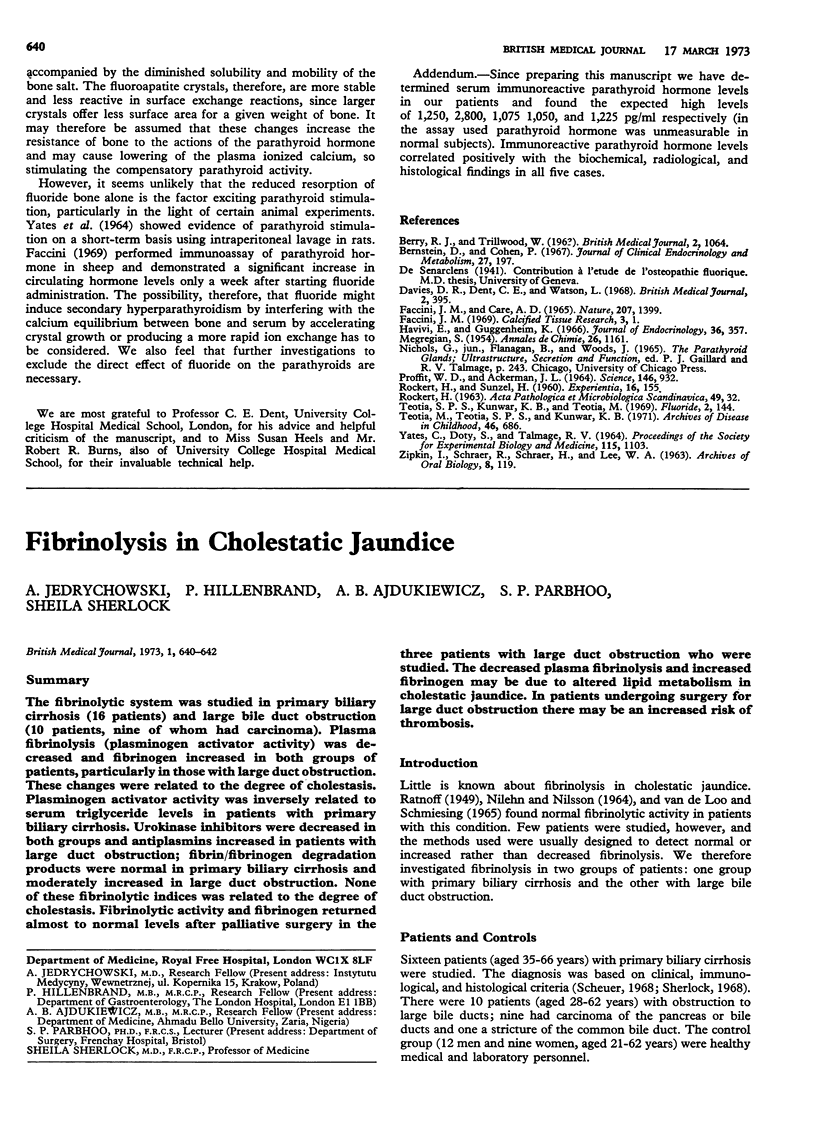
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ALKJAERSIG N., FLETCHER A. P., SHERRY S. The mechanism of clot dissolution by plasmin. J Clin Invest. 1959 Jul;38(7):1086–1095. doi: 10.1172/JCI103885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ASTRUP T., MULLERTZ S. The fibrin plate method for estimating fibrinolytic activity. Arch Biochem Biophys. 1952 Oct;40(2):346–351. doi: 10.1016/0003-9861(52)90121-5. [DOI] [PubMed] [Google Scholar]
- Aoki N., von Kaulla K. N. Inactivation of human serum plasminogen antiactivator by synthetic fibrinolysis inducers. Thromb Diath Haemorrh. 1969 Nov 15;22(2):251–262. [PubMed] [Google Scholar]
- Das P. C., Allan A. G., Woodfield D. G., Cash J. D. Fibrin degradation products in sera of normal subjects. Br Med J. 1967 Dec 23;4(5581):718–720. doi: 10.1136/bmj.4.5581.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EDWARD N., YOUNG D. P., MACLEOD M. FIBRINOLYTIC ACTIVITY IN PLASMA AND URINE IN CHRONIC RENAL DISEASE. J Clin Pathol. 1964 May;17:365–368. doi: 10.1136/jcp.17.3.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GILLMAN T., NAIDOO S. S. Gonadal influences on plasma fibrin and fibrinolytic activity: a possible basis for the further analysis of some forms of coronary thrombosis. Endocrinology. 1958 Jan;62(1):92–97. doi: 10.1210/endo-62-1-92. [DOI] [PubMed] [Google Scholar]
- Ganrot P. O. Inhibition of plasmin activity by alpha-2-macroglobulin. Clin Chim Acta. 1967 May;16(2):328–329. doi: 10.1016/0009-8981(67)90201-x. [DOI] [PubMed] [Google Scholar]
- Januszko T., Buluk K., Uszyńska-Folejewska R., Uszyński M. Pomiar inhibitora aktywacji plazminogenu w teście euglobulinowym. Ginekol Pol. 1966 Feb;37(2):137–141. [PubMed] [Google Scholar]
- Januszko T., Dubińska L. Estimation of the activator of fibrinolysis by means of the euglobulin test. Acta Med Pol. 1965;6(2):269–276. [PubMed] [Google Scholar]
- Marzo A., Ghirardi P., Sardini D., Meroni G. Simplified measurement of monoglycerides, diglycerides, triglycerides, and free fatty acids in biological samples. Clin Chem. 1971 Mar;17(3):145–147. [PubMed] [Google Scholar]
- Merskey C., Kleiner G. J., Johnson A. J. Quantitative estimation of split products of fibrinogen in human serum, relation to diagnosis and treatment. Blood. 1966 Jul;28(1):1–18. [PubMed] [Google Scholar]
- NESTEL P. J. The relationship between blood fibrinolytic activity, serum lipoproteins and serum cholesterol in atherosclerotic arterial disease. Australas Ann Med. 1960 Aug;9:234–236. doi: 10.1111/imj.1960.9.3.234. [DOI] [PubMed] [Google Scholar]
- NILEHN J. E., NILSSON I. M. DEMONSTRATION OF FIBRINOLYTIC SPLIT PRODUCTS IN HUMAN SERUM BY AN IMMUNOLOGICAL METHOD IN SPONTANEOUS AND INDUCED FIBRINOLYTIC STATES. Scand J Haematol. 1964;1:313–330. doi: 10.1111/j.1600-0609.1964.tb00029.x. [DOI] [PubMed] [Google Scholar]
- NILSSON I. M., KROOK H., STERNBY N. H., SODERBERG E., SODERSTROM N. Severe thrombotic disease in a young man with bone marrow and skeletal changes and with a high content of an inhibitor in the fibrinolytic system. Acta Med Scand. 1961 Mar;169:323–337. doi: 10.1111/j.0954-6820.1961.tb07838.x. [DOI] [PubMed] [Google Scholar]
- Niewiarowski S., Wolosowicz N. The in-vivo-effect of E-aminocaproic acid (EACA) on human plasma fibrinolytic system. Thromb Diath Haemorrh. 1966 May 15;15(3):491–500. [PubMed] [Google Scholar]
- PHILLIPS G. B. The lipid composition of serum in patients with liver disease. J Clin Invest. 1960 Nov;39:1639–1650. doi: 10.1172/JCI104187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RIDING I. M., ELLIS D. ANTIPLASMIN ACTIVITY OF BETA-LIPOPROTEIN. J Atheroscler Res. 1964 Mar-Apr;4:189–192. doi: 10.1016/s0368-1319(64)80039-9. [DOI] [PubMed] [Google Scholar]
- van de Loo J., Schmiesing G. Faktoren des fibrinolytischen Systems bei Leberkrankheiten. Thromb Diath Haemorrh. 1965 Nov 15;14(3-4):580–591. [PubMed] [Google Scholar]


