Abstract
The postprandial concentrations of free and conjugated bile acids were measured in total content and micellar phase of jejunal aspirates from nine patients with steatorrhoea due to the stagnant loop syndrome and from 11 normal controls. Aspirates from the stagnant loop syndrome patients, but not from the normal controls, had a high concentration of free (unconjugated) bile acids. There was a reciprocal decrease in the concentration of conjugated bile acids, but total bile acid concentration in the whole aspirate remained normal. Total bile acid concentration in the micellar phase of intestinal content was reduced, indicating precipitation of bile acids. These findings suggest that precipitation of unconjugated bile acids, rather than passive absorption, leads to a reduced postprandial concentration of bile acids in the micellar phase of jejunal content, and are consistent with the hypothesis that fat malabsorption in the stagnant loop syndrome results from decreased micellar dispersion of lipolytic products.
Full text
PDF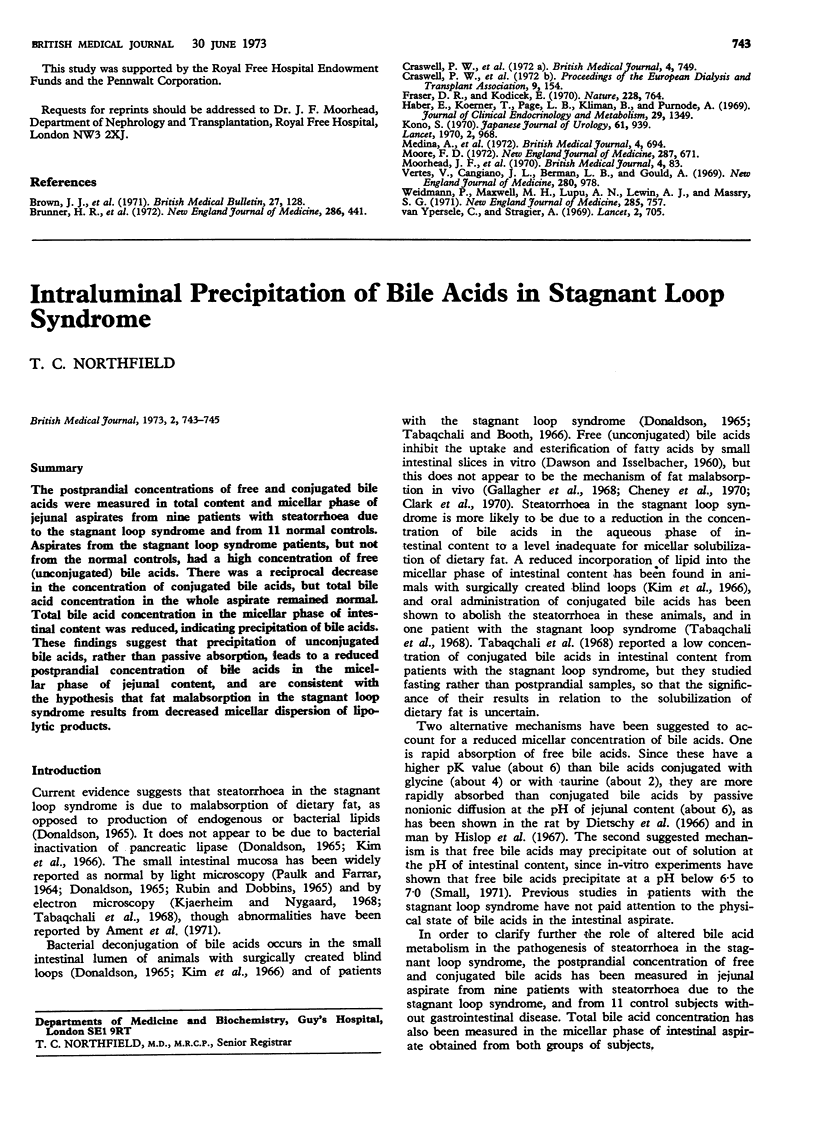
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson I. G., Haslewood G. A. Comparative studies of bile salts. 5 alpha-Chimaerol, a new bile alcohol from the white sucker Catostomus commersoni Lacépède. Biochem J. 1970 Feb;116(4):581–585. doi: 10.1042/bj1160581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badley B. W., Murphy G. M., Bouchier I. A. Intraluminal bile-salt deficiency in the pathogenesis of steatorrhoea. Lancet. 1969 Aug 23;2(7617):400–402. doi: 10.1016/s0140-6736(69)90111-1. [DOI] [PubMed] [Google Scholar]
- Cheney F. E., Burke V., Clark M. L., Senior J. R. Intestinal fatty acid absorption and esterification from luminal micellar solutions containing deoxycholic acid. Proc Soc Exp Biol Med. 1970 Jan;133(1):212–215. doi: 10.3181/00379727-133-34442. [DOI] [PubMed] [Google Scholar]
- Clark M. L., Lanz H. C., Senior J. R. Bile salt regulation of fatty acid absorption and esterification in rat everted jejunal sacs in vitro and into thoracic duct lymph in vivo. J Clin Invest. 1969 Sep;48(9):1587–1599. doi: 10.1172/JCI106124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DAWSON A. M., ISSELBACHER K. J. Studies on lipid metabolism in the small intestine with observations on the role of bile salts. J Clin Invest. 1960 May;39:730–740. doi: 10.1172/JCI104090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietschy J. M., Salomon H. S., Siperstein M. D. Bile acid metabolism. I. Studies on the mechanisms of intestinal transport. J Clin Invest. 1966 Jun;45(6):832–846. doi: 10.1172/JCI105399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson R. M., Jr Studies on the pathogenesis of steatorrhea in the blind loop syndrome. J Clin Invest. 1965 Nov;44(11):1815–1825. doi: 10.1172/JCI105289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ENEROTH P. THIN-LAYER CHROMATOGRAPHY OF BILE ACIDS. J Lipid Res. 1963 Jan;4:11–16. [PubMed] [Google Scholar]
- Gallagher N. D., Webb J. P., Dawson A. M. Effect of sodium desoxycholate on the intestinal absorption and lymphatic transport of oleic acid in the bile fistula rat. Gut. 1968 Oct;9(5):561–563. doi: 10.1136/gut.9.5.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HOFMANN A. F., BORGSTROEM B. THE INTRALUMINAL PHASE OF FAT DIGESTION IN MAN: THE LIPID CONTENT OF THE MICELLAR AND OIL PHASES OF INTESTINAL CONTENT OBTAINED DURING FAT DIGESTION AND ABSORPTION. J Clin Invest. 1964 Feb;43:247–257. doi: 10.1172/JCI104909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IWATA T., YAMASAKI K. ENZYMATIC DETERMINATION AND THIN-LAYER CHROMATOGRAPHY OF BILE ACIDS IN BLOOD. J Biochem. 1964 Nov;56:424–431. doi: 10.1093/oxfordjournals.jbchem.a128013. [DOI] [PubMed] [Google Scholar]
- Kim Y. S., Spritz N., Blum M., Terz J., Sherlock P. The role of altered bile acid metabolism in the steatorrhea of experimental blind loop. J Clin Invest. 1966 Jun;45(6):956–962. doi: 10.1172/JCI105411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northfield T. C., Condillac E., McColl I. Bile salt metabolism in the normal human small intestine. Gut. 1970 Dec;11(12):1063–1063. [PubMed] [Google Scholar]
- Northfield T. C., Drasar B. S., Wright J. T. Value of small intestinal bile acid analysis in the diagnosis of the stagnant loop syndrome. Gut. 1973 May;14(5):341–347. [PMC free article] [PubMed] [Google Scholar]
- PAULK E. A., Jr, FARRAR W. E., Jr DIVERTICULOSIS OF THE SMALL INTESTINE AND MEGALOBLASTIC ANEMIA: INTESTINAL MICROFLORA AND ABSORPTION BEFORE AND AFTER TETRACYCLINE ADMINISTRATION. Am J Med. 1964 Sep;37:473–480. doi: 10.1016/0002-9343(64)90202-5. [DOI] [PubMed] [Google Scholar]
- Rubin C. E., Dobbins W. O., 3rd Peroral biopsy of the small intestine. A review of its diagnostic usefulness. Gastroenterology. 1965 Dec;49(6):676–697. [PubMed] [Google Scholar]
- Tabaqchali S., Booth C. C. Jejunal bacteriology and bile-salt metabolism in patients with intestinal malabsorption. Lancet. 1966 Jul 2;2(7453):12–15. doi: 10.1016/s0140-6736(66)91744-2. [DOI] [PubMed] [Google Scholar]


