Abstract
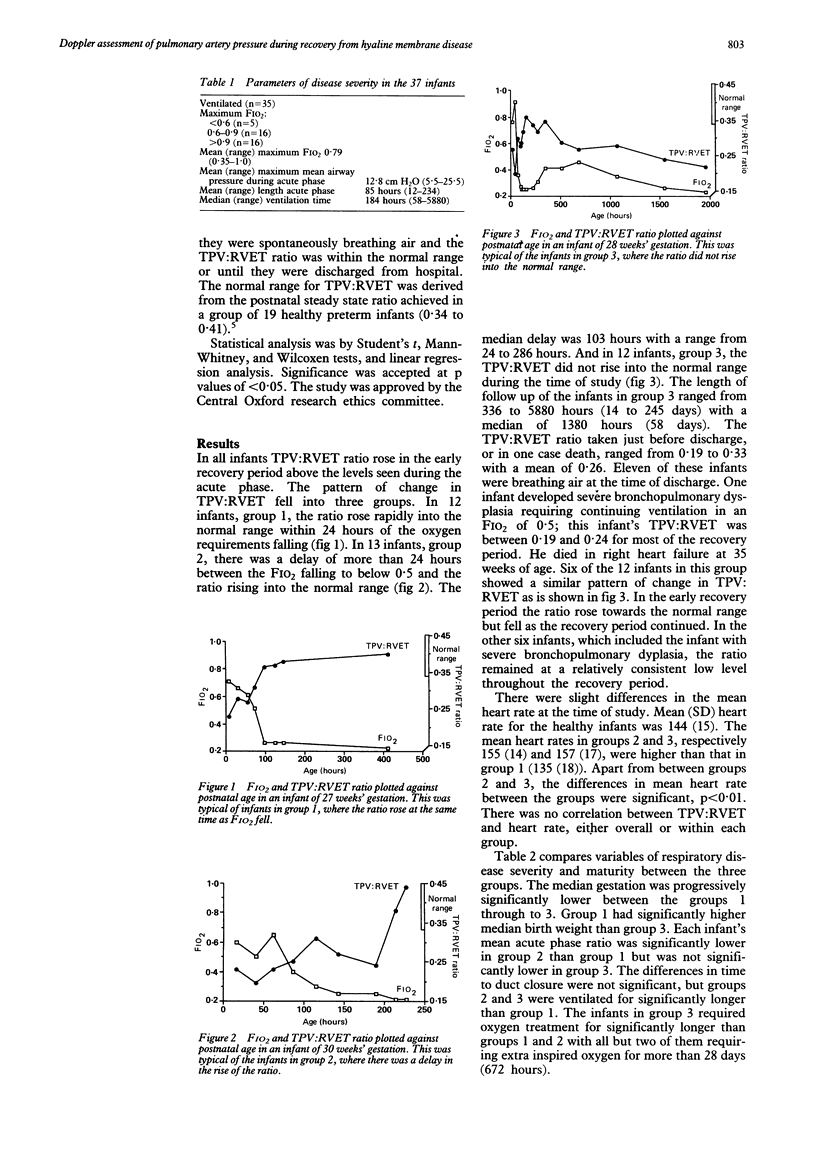
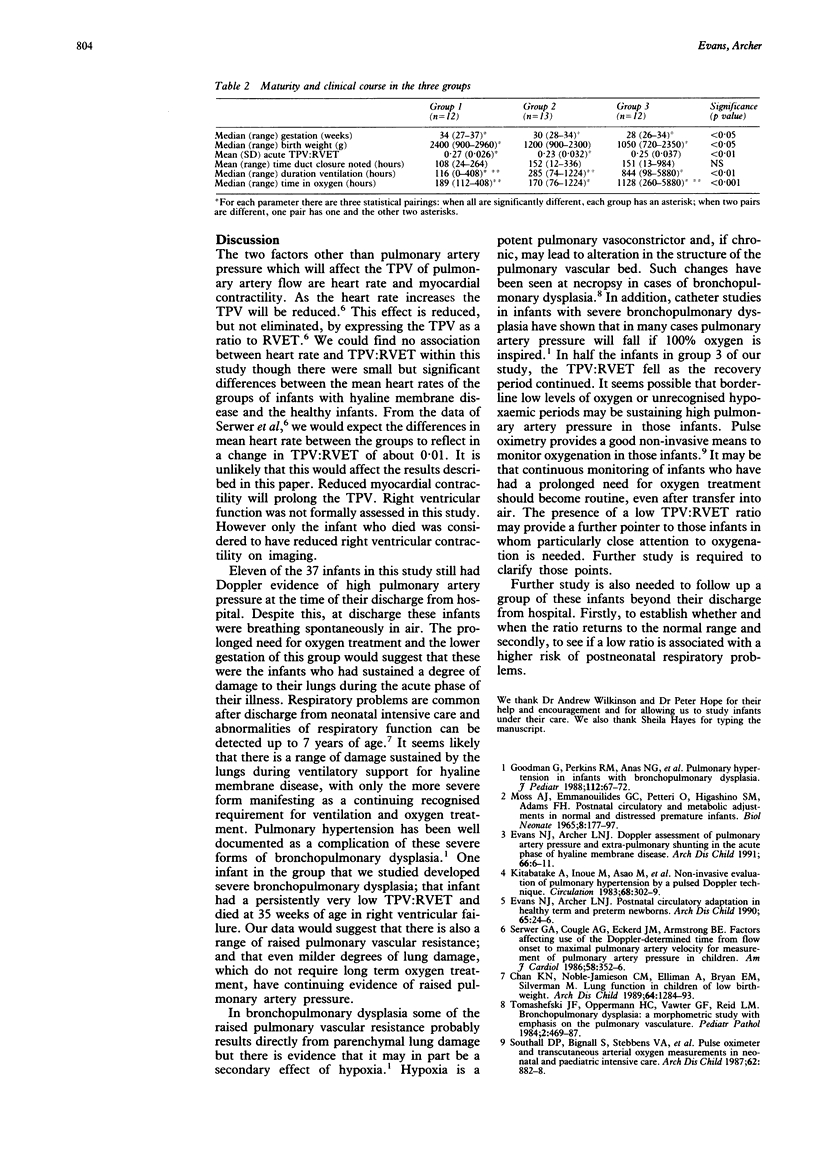
The changes in pulmonary artery pressure during recovery from hyaline membrane disease were studied by serial Doppler echocardiography on 37 preterm infants. Pulmonary artery pressure was assessed noninvasively by its inverse relationship with the ratio of pulmonary artery Doppler time to peak velocity and right ventricular ejection time. The pattern of rise in ratio after the acute phase of hyaline membrane disease divided into three types. In 25 infants the ratio returned to the normal range: in 12 (group 1) at the same time as the fractional inspired oxygen fell below 0.5 and in 13 (group 2) after a delay of at least 24 hours. In 12 infants (group 3) the ratio remained below the normal range during their hospital stay, suggesting pulmonary artery pressure remained high. Infants in group 3 were of significantly lower gestation and required oxygen treatment for significantly longer than infants in groups 1 and 2. Persistently raised pulmonary pressures in group 3 may reflect lung damage either directly affecting pulmonary vasculature or exerting a secondary effect on pulmonary vascular resistance through hypoxaemia.
Full text
PDF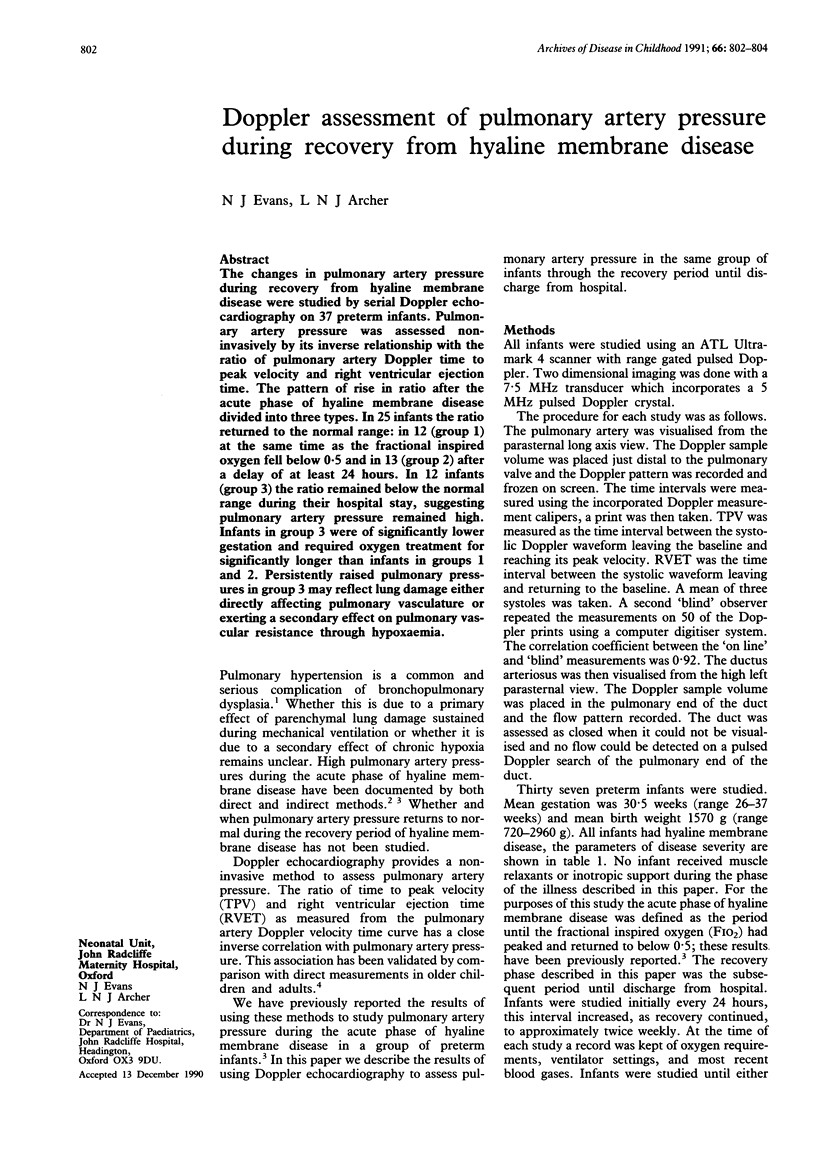
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chan K. N., Noble-Jamieson C. M., Elliman A., Bryan E. M., Silverman M. Lung function in children of low birth weight. Arch Dis Child. 1989 Sep;64(9):1284–1293. doi: 10.1136/adc.64.9.1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans N. J., Archer L. N. Doppler assessment of pulmonary artery pressure and extrapulmonary shunting in the acute phase of hyaline membrane disease. Arch Dis Child. 1991 Jan;66(1 Spec No):6–11. doi: 10.1136/adc.66.1_spec_no.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans N. J., Archer L. N. Postnatal circulatory adaptation in healthy term and preterm neonates. Arch Dis Child. 1990 Jan;65(1 Spec No):24–26. doi: 10.1136/adc.65.1_spec_no.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman G., Perkin R. M., Anas N. G., Sperling D. R., Hicks D. A., Rowen M. Pulmonary hypertension in infants with bronchopulmonary dysplasia. J Pediatr. 1988 Jan;112(1):67–72. doi: 10.1016/s0022-3476(88)80125-2. [DOI] [PubMed] [Google Scholar]
- Kitabatake A., Inoue M., Asao M., Masuyama T., Tanouchi J., Morita T., Mishima M., Uematsu M., Shimazu T., Hori M. Noninvasive evaluation of pulmonary hypertension by a pulsed Doppler technique. Circulation. 1983 Aug;68(2):302–309. doi: 10.1161/01.cir.68.2.302. [DOI] [PubMed] [Google Scholar]
- Serwer G. A., Cougle A. G., Eckerd J. M., Armstrong B. E. Factors affecting use of the Doppler-determined time from flow onset to maximal pulmonary artery velocity for measurement of pulmonary artery pressure in children. Am J Cardiol. 1986 Aug 1;58(3):352–356. doi: 10.1016/0002-9149(86)90076-7. [DOI] [PubMed] [Google Scholar]
- Southall D. P., Bignall S., Stebbens V. A., Alexander J. R., Rivers R. P., Lissauer T. Pulse oximeter and transcutaneous arterial oxygen measurements in neonatal and paediatric intensive care. Arch Dis Child. 1987 Sep;62(9):882–888. doi: 10.1136/adc.62.9.882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomashefski J. F., Jr, Oppermann H. C., Vawter G. F., Reid L. M. Bronchopulmonary dysplasia: a morphometric study with emphasis on the pulmonary vasculature. Pediatr Pathol. 1984;2(4):469–487. doi: 10.3109/15513818409025895. [DOI] [PubMed] [Google Scholar]


