Abstract
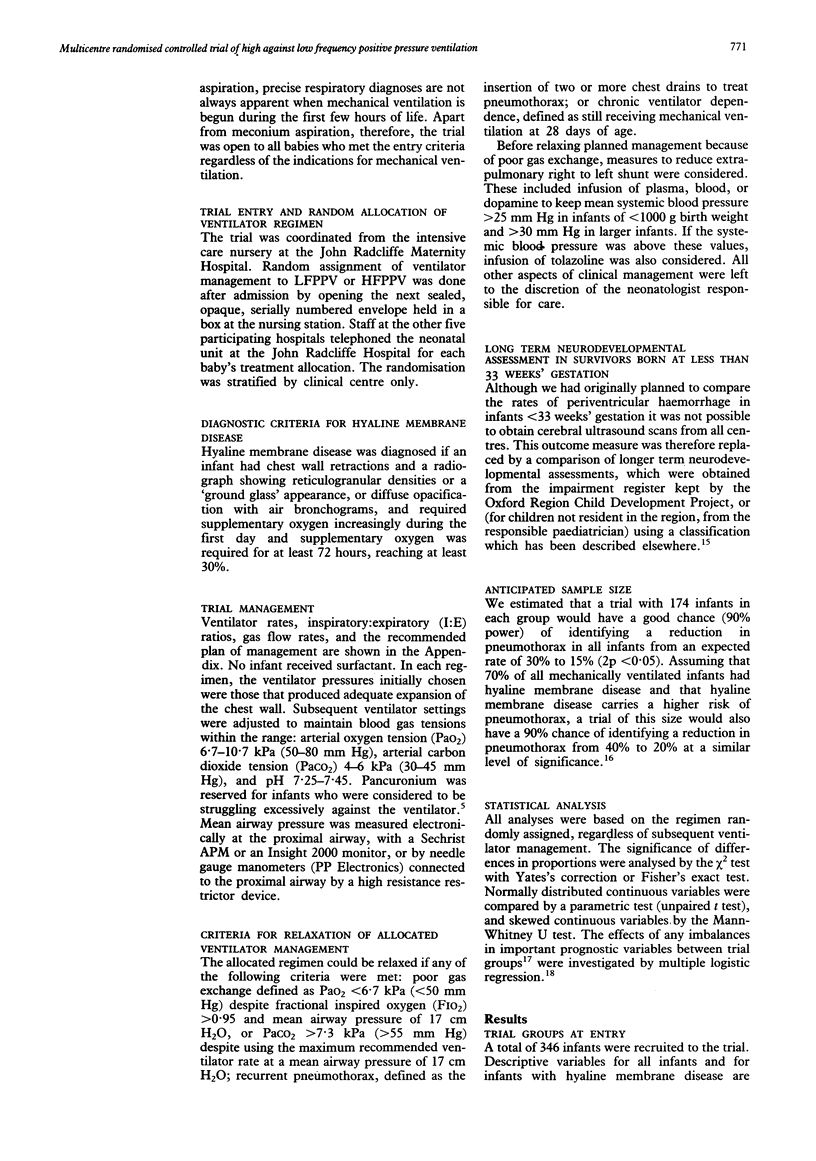
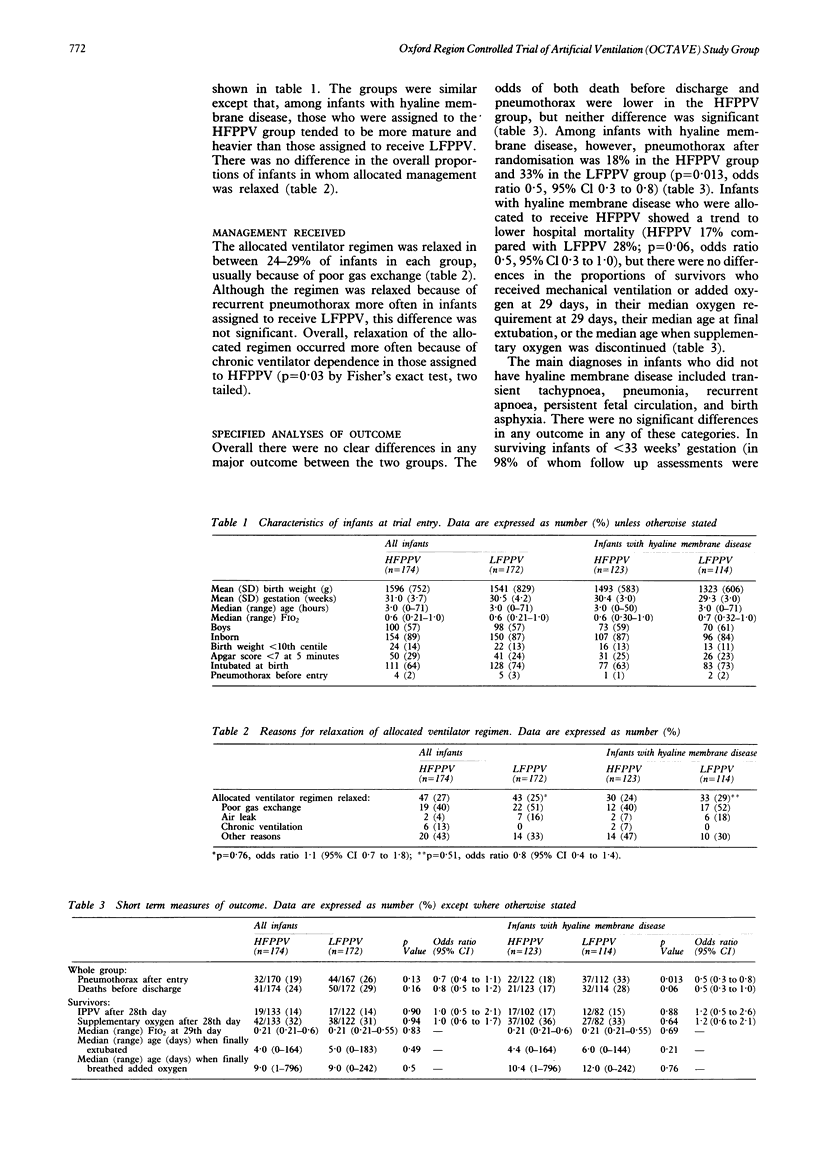
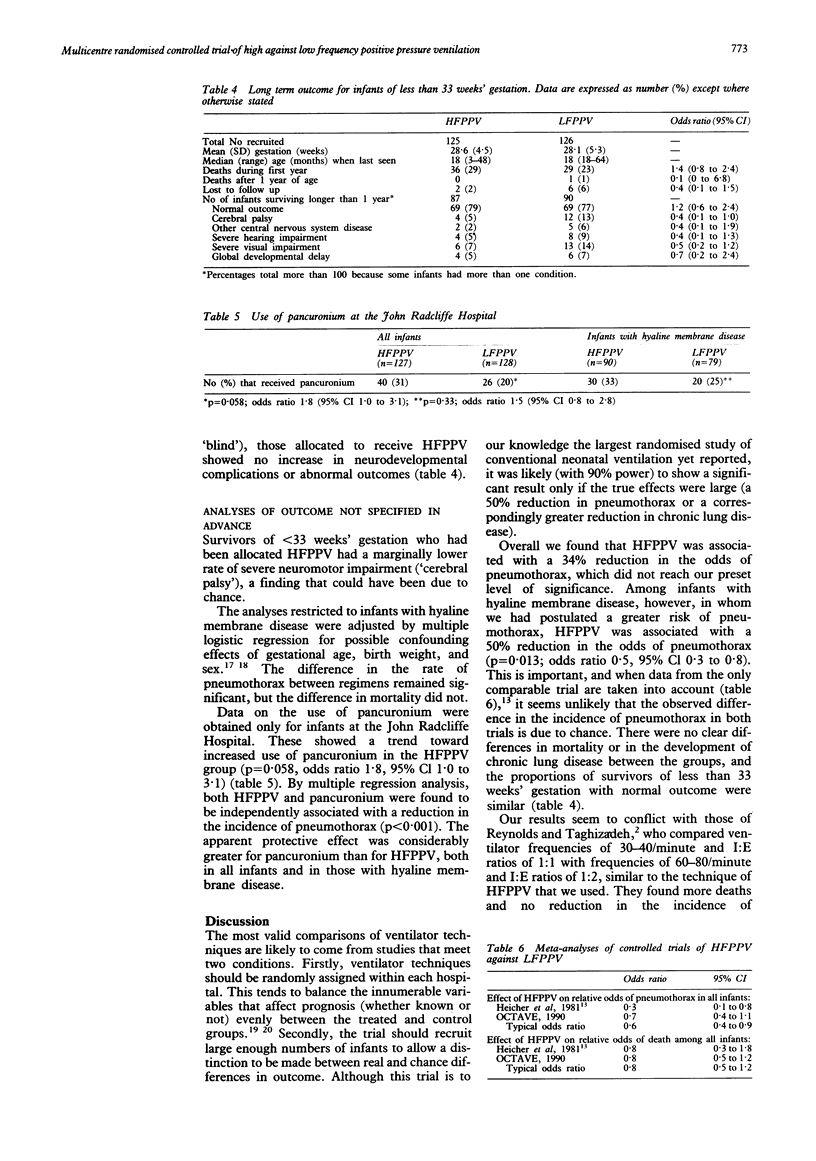
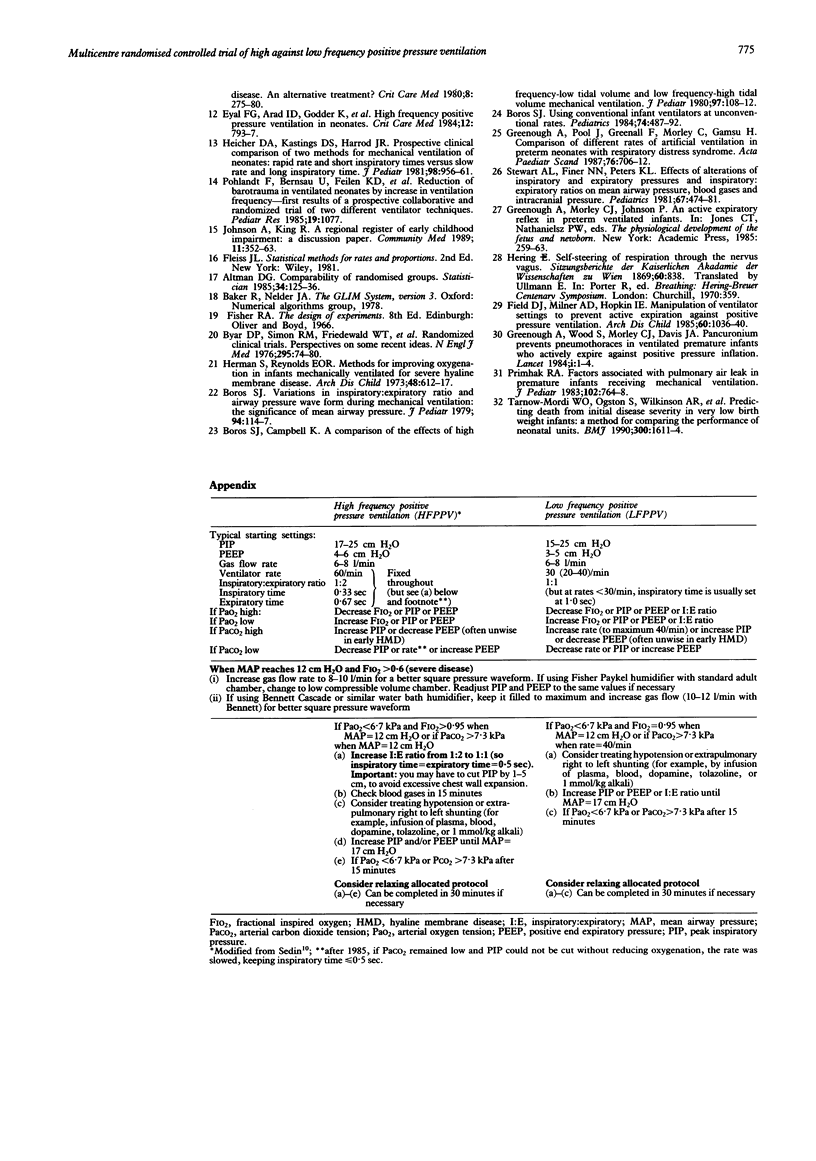
A total of 346 infants aged less than 72 hours were randomly allocated to be treated either by high frequency positive pressure ventilation (HFPPV; rate fixed at 60/minute throughout treatment and initial inspiratory:expiratory (I:E) ratio 1:2, increased to 1:1 if necessary) or by low frequency positive pressure ventilation (LFPPV; rate less than or equal to 40/minute and initial I:E ratio usually 1:1, both decreasing during weaning). The main hypotheses were that HFPPV reduces pneumothorax, chronic lung disease and death before discharge in all infants, as well as those with hyaline membrane disease, and that it reduces the incidence of later neurodevelopmental complications in infants of less than 33 weeks' gestation. Among all the infants the rate of pneumothorax was 19% in the HFPPV group and 26% in the LFPPV group (p = 0.13; odds ratio 0.7, 95% confidence intervals (CI) 0.4 to 1.1); there was no difference in mortality or the incidence of chronic lung disease. In infants of less than 33 weeks' gestation there were no differences in adverse neurodevelopmental outcomes. Among the subgroup of 237 infants with hyaline membrane disease, median fractional inspired oxygen at the time of entry to the trial was 0.6 in the HFPPV group and 0.7 in the LFPPV group, indicating that many had moderately severe disease. In patients with hyaline membrane disease HFPPV was associated with a lower rate of pneumothorax (18% in the HFPPV group compared with 33% in the LFPPV group, p = 0.013, odds ratio 0.5, 95% CI 0.3 to 0.8, with no differences in mortality, or in duration of intubation or supplementary oxygen in survivors. As used in this study, HFPPV was the preferred ventilator regimen for infants with hyaline membrane disease.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Avery M. E., Tooley W. H., Keller J. B., Hurd S. S., Bryan M. H., Cotton R. B., Epstein M. F., Fitzhardinge P. M., Hansen C. B., Hansen T. N. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics. 1987 Jan;79(1):26–30. [PubMed] [Google Scholar]
- Bland R. D., Kim M. H., Light M. J., Woodson J. L. High frequency mechanical ventilation in severe hyaline membrane disease an alternative treatment? Crit Care Med. 1980 May;8(5):275–280. doi: 10.1097/00003246-198005000-00001. [DOI] [PubMed] [Google Scholar]
- Boros S. J., Bing D. R., Mammel M. C., Hagen E., Gordon M. J. Using conventional infant ventilators at unconventional rates. Pediatrics. 1984 Oct;74(4):487–492. [PubMed] [Google Scholar]
- Boros S. J., Campbell K. A comparison of the effects of high frequency--low tidal volume and low frequency--high tidal volume mechanical ventilation. J Pediatr. 1980 Jul;97(1):108–112. doi: 10.1016/s0022-3476(80)80146-6. [DOI] [PubMed] [Google Scholar]
- Boros S. J. Variations in inspiratory:expiratory ratio and airway pressure wave form during mechanical ventilation: the significance of mean airway pressure. J Pediatr. 1979 Jan;94(1):114–117. doi: 10.1016/s0022-3476(79)80372-8. [DOI] [PubMed] [Google Scholar]
- Byar D. P., Simon R. M., Friedewald W. T., Schlesselman J. J., DeMets D. L., Ellenberg J. H., Gail M. H., Ware J. H. Randomized clinical trials. Perspectives on some recent ideas. N Engl J Med. 1976 Jul 8;295(2):74–80. doi: 10.1056/NEJM197607082950204. [DOI] [PubMed] [Google Scholar]
- Eyal F. G., Arad I. D., Godder K., Robinson M. J. High-frequency positive-pressure ventilation in neonates. Crit Care Med. 1984 Sep;12(9):793–797. doi: 10.1097/00003246-198409000-00025. [DOI] [PubMed] [Google Scholar]
- Field D., Milner A. D., Hopkin I. E. Manipulation of ventilator settings to prevent active expiration against positive pressure inflation. Arch Dis Child. 1985 Nov;60(11):1036–1040. doi: 10.1136/adc.60.11.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenough A., Pool J., Greenall F., Morley C., Gamsu H. Comparison of different rates of artificial ventilation in preterm neonates with respiratory distress syndrome. Acta Paediatr Scand. 1987 Sep;76(5):706–712. doi: 10.1111/j.1651-2227.1987.tb10553.x. [DOI] [PubMed] [Google Scholar]
- Greenough A., Roberton N. R. Morbidity and survival in neonates ventilated for the respiratory distress syndrome. Br Med J (Clin Res Ed) 1985 Feb 23;290(6468):597–600. doi: 10.1136/bmj.290.6468.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman S., Reynolds E. O. Methods for improving oxygenation in infants mechanically ventilated for severe hyaline membrane disease. Arch Dis Child. 1973 Aug;48(8):612–617. doi: 10.1136/adc.48.8.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwood S. P., Boyle M. H., Torrance G. W., Sinclair J. C. Mortality and morbidity of 500- to 1,499-gram birth weight infants live-born to residents of a defined geographic region before and after neonatal intensive care. Pediatrics. 1982 May;69(5):613–620. [PubMed] [Google Scholar]
- Johnson A., King R. A regional register of early childhood impairments: a discussion paper. The Steering Committee of the Oxford Region Child Development Project. Community Med. 1989 Nov;11(4):352–363. [PubMed] [Google Scholar]
- Primhak R. A. Factors associated with pulmonary air leak in premature infants receiving mechanical ventilation. J Pediatr. 1983 May;102(5):764–768. doi: 10.1016/s0022-3476(83)80254-6. [DOI] [PubMed] [Google Scholar]
- Ramsden C. A., Reynolds E. O. Ventilator settings for newborn infants. Arch Dis Child. 1987 May;62(5):529–538. doi: 10.1136/adc.62.5.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid D. H., Tunstall M. E., Mitchell R. G. A controlled trial of artificial respiration in the respiratory-distress syndrome of the newborn. Lancet. 1967 Mar 11;1(7489):532–533. doi: 10.1016/s0140-6736(67)92112-5. [DOI] [PubMed] [Google Scholar]
- Reynolds E. O., Taghizadeh A. Improved prognosis of infants mechanically ventilated for hyaline membrane disease. Arch Dis Child. 1974 Jul;49(7):505–515. doi: 10.1136/adc.49.7.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedin G. Positive-pressure ventilation at moderately high frequency in newborn infants with respiratory distress syndrome (IRDS). Acta Anaesthesiol Scand. 1986 Oct;30(7):515–520. doi: 10.1111/j.1399-6576.1986.tb02467.x. [DOI] [PubMed] [Google Scholar]
- Stewart A. R., Finer N. N., Peters K. L. Effects of alterations of inspiratory and expiratory pressures and inspiratory/expiratory ratios on mean airway pressure, blood gases, and intracranial pressure. Pediatrics. 1981 Apr;67(4):474–481. [PubMed] [Google Scholar]
- Tarnow-Mordi W. O., Narang A., Wilkinson A. R. Lack of association between barotrauma and air leak in hyaline membrane disease. Arch Dis Child. 1985 Jun;60(6):555–559. doi: 10.1136/adc.60.6.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarnow-Mordi W., Ogston S., Wilkinson A. R., Reid E., Gregory J., Saeed M., Wilkie R. Predicting death from initial disease severity in very low birthweight infants: a method for comparing the performance of neonatal units. BMJ. 1990 Jun 23;300(6740):1611–1614. doi: 10.1136/bmj.300.6740.1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tooley W. H. Epidemiology of bronchopulmonary dysplasia. J Pediatr. 1979 Nov;95(5 Pt 2):851–858. doi: 10.1016/s0022-3476(79)80451-5. [DOI] [PubMed] [Google Scholar]


