Abstract
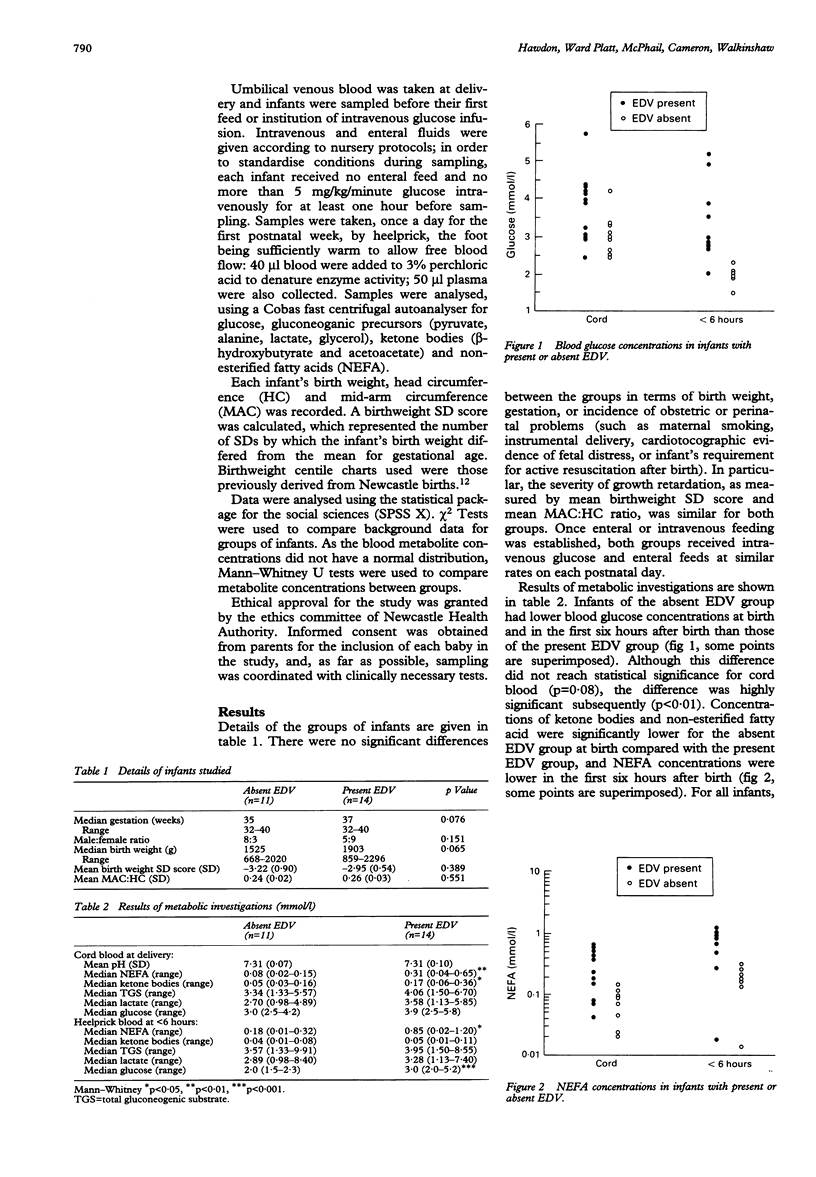
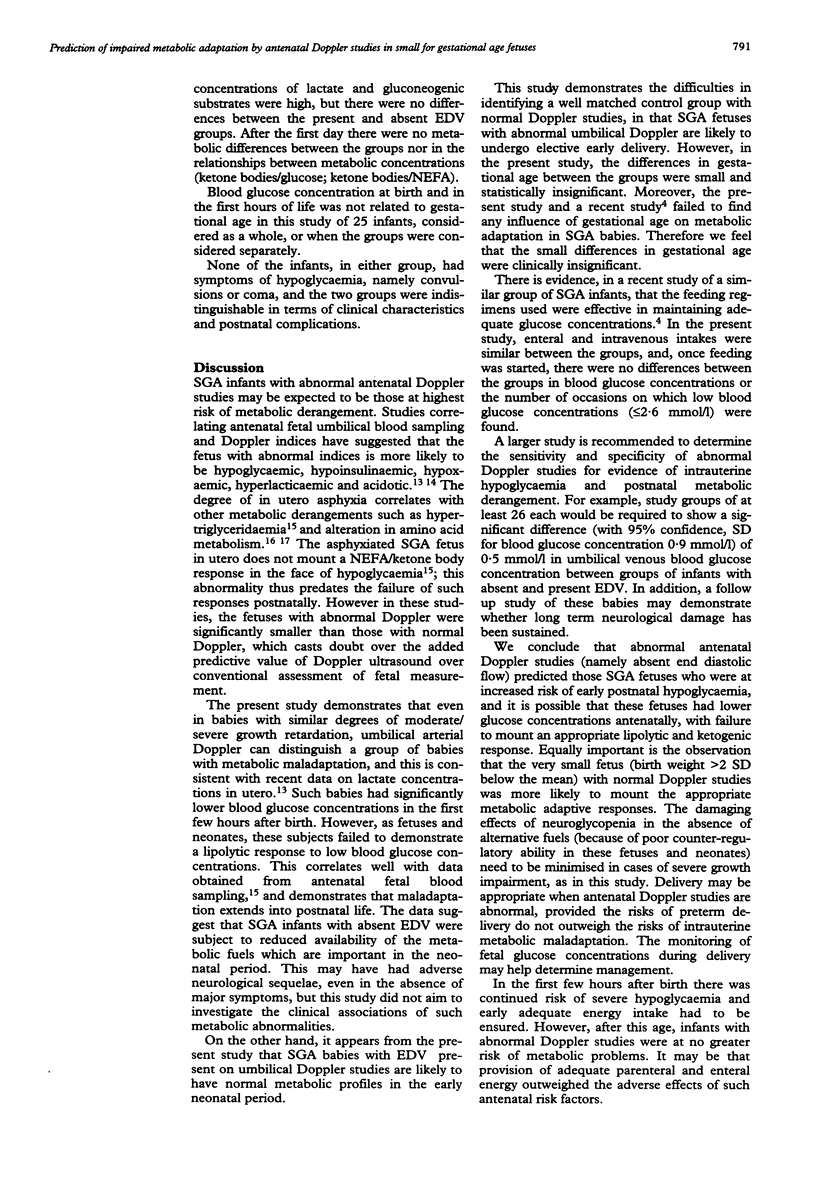
The increased risk of hypoglycaemia for infants who are small for gestational age (SGA) is well known, and further information regarding metabolic adaptation can be gained by examining the profiles of glucose and other metabolic fuels in such infants. Not all SGA infants experience hypoglycaemia, however, and the ability to identify, antenatally, those at most risk would be helpful for obstetric and neonatal management. This study investigated metabolic differences between two groups of SGA infants who had antenatal umbilical artery Doppler studies. Fourteen had end diastolic velocities (EDV) present and 11 had absent EDV. The absent EDV group had significantly lower non-esterified fatty acid (NEFA) concentrations at birth, and lower blood glucose and NEFA concentrations in the first six hours after birth. After the first day, few metabolic differences were found between the two groups. Antenatal Doppler studies may identify those SGA infants who fail to achieve neonatal metabolic adaptation and are most at risk of early neonatal hypoglycaemia.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Burke G., Stuart B., Crowley P., Scanaill S. N., Drumm J. Is intrauterine growth retardation with normal umbilical artery blood flow a benign condition? BMJ. 1990 Apr 21;300(6731):1044–1045. doi: 10.1136/bmj.300.6731.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CORNBLATH M., ODELL G. B., LEVIN E. Y. Symptomatic neonatal hypoglycemia associated with toxemia of pregnancy. J Pediatr. 1959 Nov;55:545–562. doi: 10.1016/s0022-3476(59)80239-0. [DOI] [PubMed] [Google Scholar]
- Cetin I., Corbetta C., Sereni L. P., Marconi A. M., Bozzetti P., Pardi G., Battaglia F. C. Umbilical amino acid concentrations in normal and growth-retarded fetuses sampled in utero by cordocentesis. Am J Obstet Gynecol. 1990 Jan;162(1):253–261. doi: 10.1016/0002-9378(90)90860-a. [DOI] [PubMed] [Google Scholar]
- Economides D. L., Crook D., Nicolaides K. H. Hypertriglyceridemia and hypoxemia in small-for-gestational-age fetuses. Am J Obstet Gynecol. 1990 Feb;162(2):382–386. doi: 10.1016/0002-9378(90)90391-j. [DOI] [PubMed] [Google Scholar]
- Economides D. L., Nicolaides K. H., Gahl W. A., Bernardini I., Evans M. I. Plasma amino acids in appropriate- and small-for-gestational-age fetuses. Am J Obstet Gynecol. 1989 Nov;161(5):1219–1227. doi: 10.1016/0002-9378(89)90670-4. [DOI] [PubMed] [Google Scholar]
- Haworth J. C., Dilling L., Younoszai M. K. Relation of blood-glucose to haematocrit, birthweight, and other body measurements in normal and growth-retarded newborn infants. Lancet. 1967 Oct 28;2(7522):901–905. doi: 10.1016/s0140-6736(67)90228-0. [DOI] [PubMed] [Google Scholar]
- Járai I., Mestyán J., Schultz K., Lázár A., Halász M., Krassy I. Body size and neonatal hypoglycemia in intrauterine growth retardation. Early Hum Dev. 1977 Oct;1(1):25–38. doi: 10.1016/0378-3782(77)90027-5. [DOI] [PubMed] [Google Scholar]
- Koh T. H., Aynsley-Green A., Tarbit M., Eyre J. A. Neural dysfunction during hypoglycaemia. Arch Dis Child. 1988 Nov;63(11):1353–1358. doi: 10.1136/adc.63.11.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubchenco L. O., Bard H. Incidence of hypoglycemia in newborn infants classified by birth weight and gestational age. Pediatrics. 1971 May;47(5):831–838. [PubMed] [Google Scholar]
- Lucas A., Morley R., Cole T. J. Adverse neurodevelopmental outcome of moderate neonatal hypoglycaemia. BMJ. 1988 Nov 19;297(6659):1304–1308. doi: 10.1136/bmj.297.6659.1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marconi A. M., Cetin I., Ferrazzi E., Ferrari M. M., Pardi G., Battaglia F. C. Lactate metabolism in normal and growth-retarded human fetuses. Pediatr Res. 1990 Dec;28(6):652–656. doi: 10.1203/00006450-199012000-00022. [DOI] [PubMed] [Google Scholar]
- NELIGAN G. A., ROBSON E., WATSON J. Hypoglycaemia in the newborn. A sequel of intrauterine malnutrition. Lancet. 1963 Jun 15;1(7294):1282–1284. doi: 10.1016/s0140-6736(63)91982-2. [DOI] [PubMed] [Google Scholar]
- Nicolini U., Nicolaidis P., Fisk N. M., Vaughan J. I., Fusi L., Gleeson R., Rodeck C. H. Limited role of fetal blood sampling in prediction of outcome in intrauterine growth retardation. Lancet. 1990 Sep 29;336(8718):768–772. doi: 10.1016/0140-6736(90)93239-l. [DOI] [PubMed] [Google Scholar]
- Pardi G., Buscaglia M., Ferrazzi E., Bozzetti P., Marconi A. M., Cetin I., Battaglia F. C., Makowski E. L. Cord sampling for the evaluation of oxygenation and acid-base balance in growth-retarded human fetuses. Am J Obstet Gynecol. 1987 Nov;157(5):1221–1228. doi: 10.1016/s0002-9378(87)80298-3. [DOI] [PubMed] [Google Scholar]
- Soothill P. W., Nicolaides K. H., Campbell S. Prenatal asphyxia, hyperlacticaemia, hypoglycaemia, and erythroblastosis in growth retarded fetuses. Br Med J (Clin Res Ed) 1987 Apr 25;294(6579):1051–1053. doi: 10.1136/bmj.294.6579.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]


