Abstract
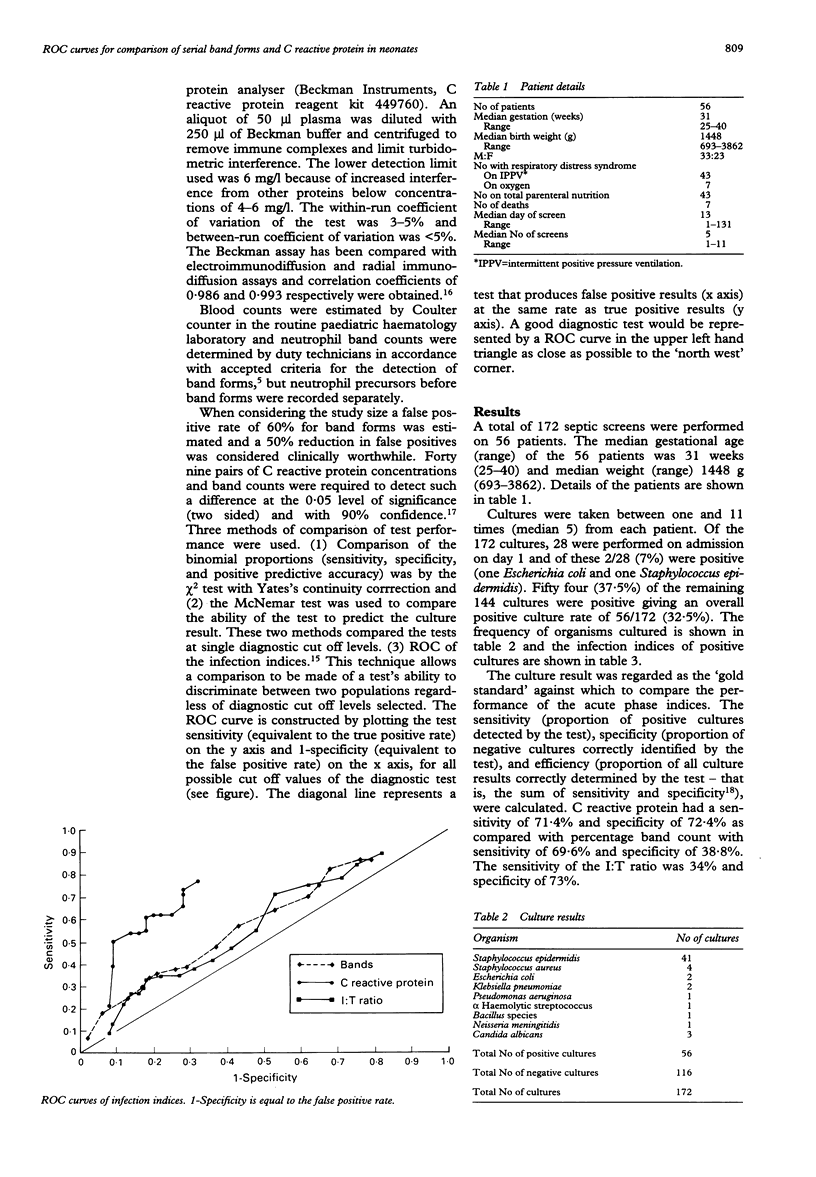
The performance of indirect indices of infection in the newborn vary because of differences in techniques, including diagnostic cut off levels. We have compared serial neutrophil band cell counts with C reactive protein measured by rate nephelometry. The 'gold standard' was a positive culture and the performance of the tests was compared by the technique of receiver operating characteristics (ROC) as well as sensitivity and specificity. A total of 172 septic screens were performed in 56 patients. The operational diagnostic cut off values were: C reactive protein greater than 8 mg/l, immature:total neutrophil ratio (I:T ratio) greater than 0.2, and band count greater than 5%. Compared with the sensitivity of C reactive protein (71%), I:T ratio (34%) was significantly different but band count (69%) was not. The specificity of C reactive protein (72%) was better than band count (39%) but no better than I:T ratio (73%). ROC curves were constructed for all possible diagnostic cut off values of the tests and superior performance was demonstrated for C reactive protein compared with band count and I:T ratio. We conclude that C reactive protein is a useful early indicator of infection in neonates and that ROC curves permit comprehensive and graphic comparison between tests and the calculation of optimal diagnostic cut off values.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beck J. R., Shultz E. K. The use of relative operating characteristic (ROC) curves in test performance evaluation. Arch Pathol Lab Med. 1986 Jan;110(1):13–20. [PubMed] [Google Scholar]
- Gill C. W., Bush W. S., Burleigh W. M., FIscher C. L. An evaluation of a C-reactive protein assay using a rate immunonephelometric procedure. Am J Clin Pathol. 1981 Jan;75(1):50–55. doi: 10.1093/ajcp/75.1.50. [DOI] [PubMed] [Google Scholar]
- Gregory J., Hey E. Blood neutrophil response to bacterial infection in the first month of life. Arch Dis Child. 1972 Oct;47(255):747–753. doi: 10.1136/adc.47.255.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindocha P., Campbell C. A., Gould J. D., Wojciechowski A., Wood C. B. Serial study of C reactive protein in neonatal septicaemia. Arch Dis Child. 1984 May;59(5):435–438. doi: 10.1136/adc.59.5.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kite P., Millar M. R., Gorham P., Congdon P. Comparison of five tests used in diagnosis of neonatal bacteraemia. Arch Dis Child. 1988 Jun;63(6):639–643. doi: 10.1136/adc.63.6.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd B. W., Oto A. Normal values for mature and immature neutrophils in very preterm babies. Arch Dis Child. 1982 Mar;57(3):233–235. doi: 10.1136/adc.57.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manroe B. L., Weinberg A. G., Rosenfeld C. R., Browne R. The neonatal blood count in health and disease. I. Reference values for neutrophilic cells. J Pediatr. 1979 Jul;95(1):89–98. doi: 10.1016/s0022-3476(79)80096-7. [DOI] [PubMed] [Google Scholar]
- Philip A. G. Acute-phase proteins in neonatal infection. J Pediatr. 1984 Dec;105(6):940–942. doi: 10.1016/s0022-3476(84)80082-7. [DOI] [PubMed] [Google Scholar]
- Philip A. G. Detection of neonatal sepsis of late onset. JAMA. 1982 Jan 22;247(4):489–492. [PubMed] [Google Scholar]
- Philip A. G., Hewitt J. R. Early diagnosis of neonatal sepsis. Pediatrics. 1980 May;65(5):1036–1041. [PubMed] [Google Scholar]
- Rodwell R. L., Leslie A. L., Tudehope D. I. Early diagnosis of neonatal sepsis using a hematologic scoring system. J Pediatr. 1988 May;112(5):761–767. doi: 10.1016/s0022-3476(88)80699-1. [DOI] [PubMed] [Google Scholar]
- Sabel K. G., Wadsworth C. C-reactive protein (CRP) in early diagnosis of neonatal septicemia. Acta Paediatr Scand. 1979 Nov;68(6):825–831. doi: 10.1111/j.1651-2227.1979.tb08219.x. [DOI] [PubMed] [Google Scholar]
- Sann L., Bienvenu F., Bienvenu J., Bourgeois J., Bethenod M. Evolution of serum prealbumin, C-reactive protein, and orosomucoid in neonates with bacterial infection. J Pediatr. 1984 Dec;105(6):977–981. doi: 10.1016/s0022-3476(84)80094-3. [DOI] [PubMed] [Google Scholar]
- Speer C., Bruns A., Gahr M. Sequential determination of CRP, alpha 1-antitrypsin and haptoglobin in neonatal septicaemia. Acta Paediatr Scand. 1983 Sep;72(5):679–683. doi: 10.1111/j.1651-2227.1983.tb09793.x. [DOI] [PubMed] [Google Scholar]
- Wasunna A., Whitelaw A., Gallimore R., Hawkins P. N., Pepys M. B. C-reactive protein and bacterial infection in preterm infants. Eur J Pediatr. 1990 Mar;149(6):424–427. doi: 10.1007/BF02009664. [DOI] [PubMed] [Google Scholar]
- Xanthou M. Leucocyte blood picture in healthy full-term and premature babies during neonatal period. Arch Dis Child. 1970 Apr;45(240):242–249. doi: 10.1136/adc.45.240.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xanthou M. Leucocyte blood picture in ill newborn babies. Arch Dis Child. 1972 Oct;47(255):741–746. doi: 10.1136/adc.47.255.741. [DOI] [PMC free article] [PubMed] [Google Scholar]


