Abstract
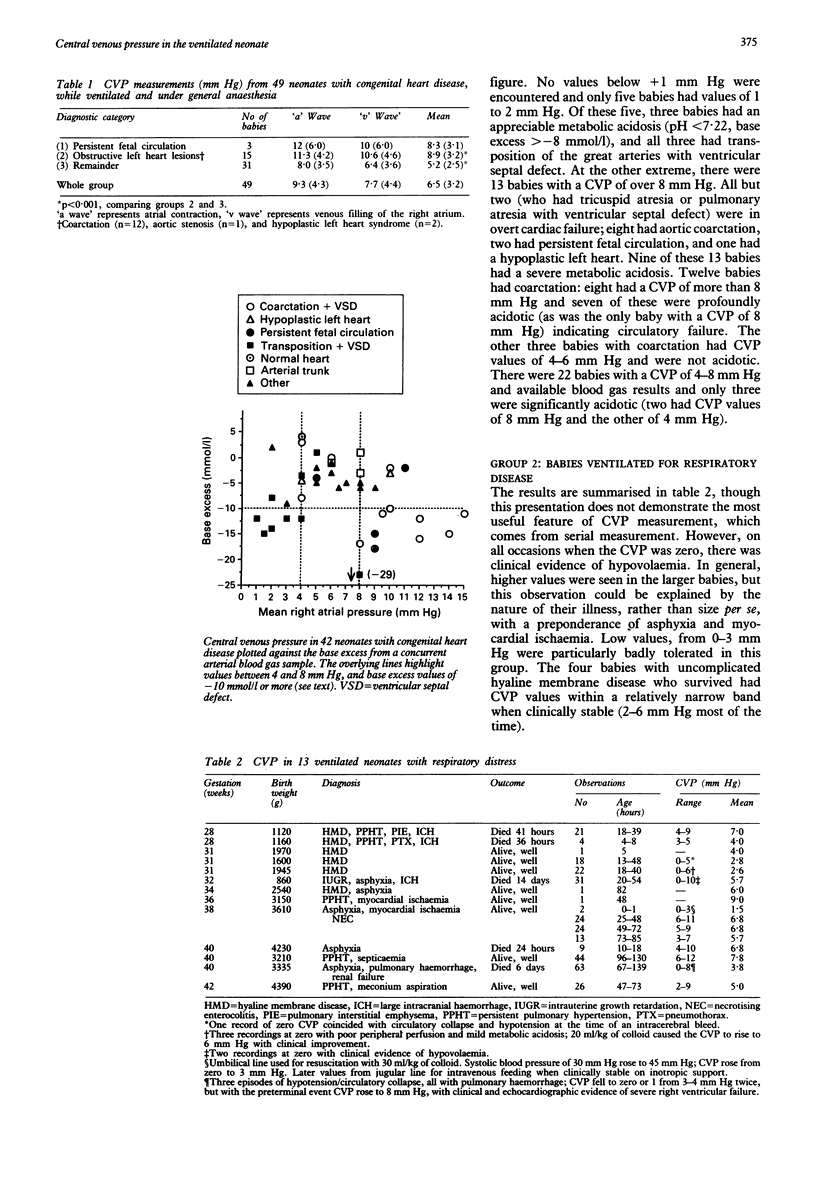
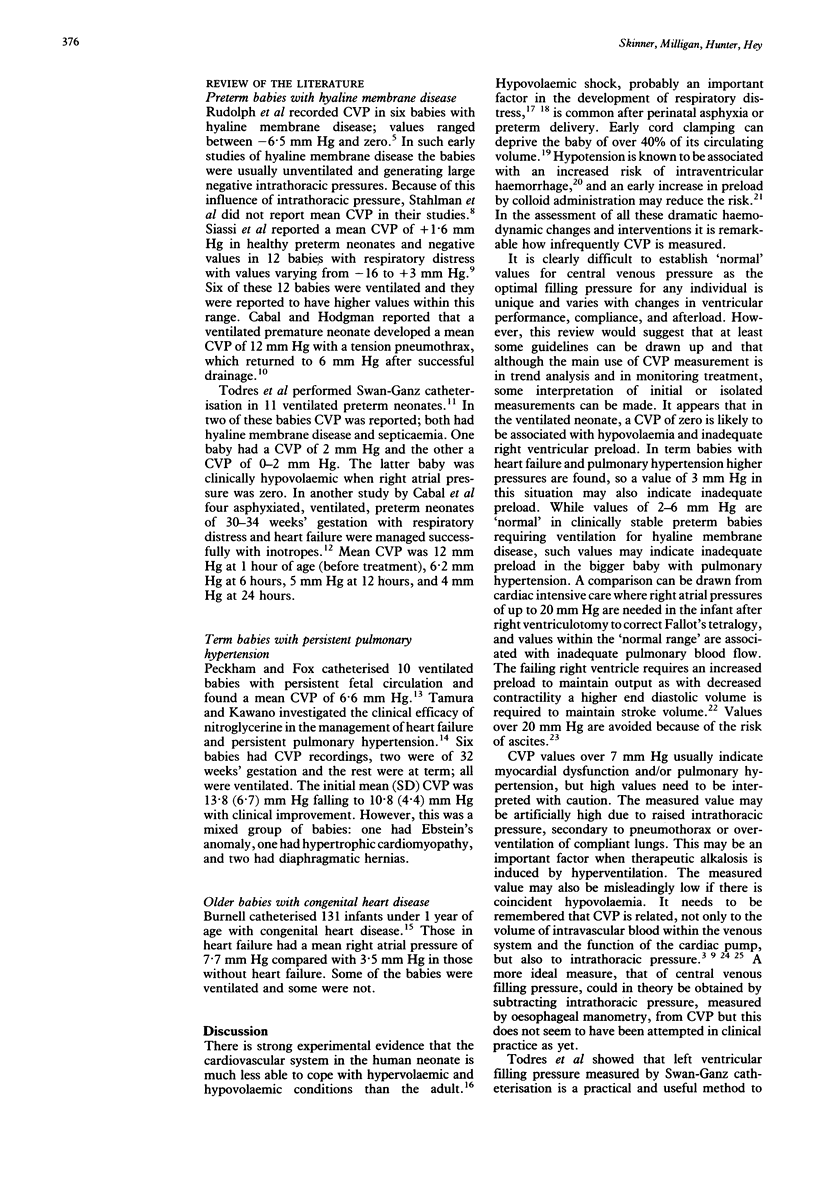
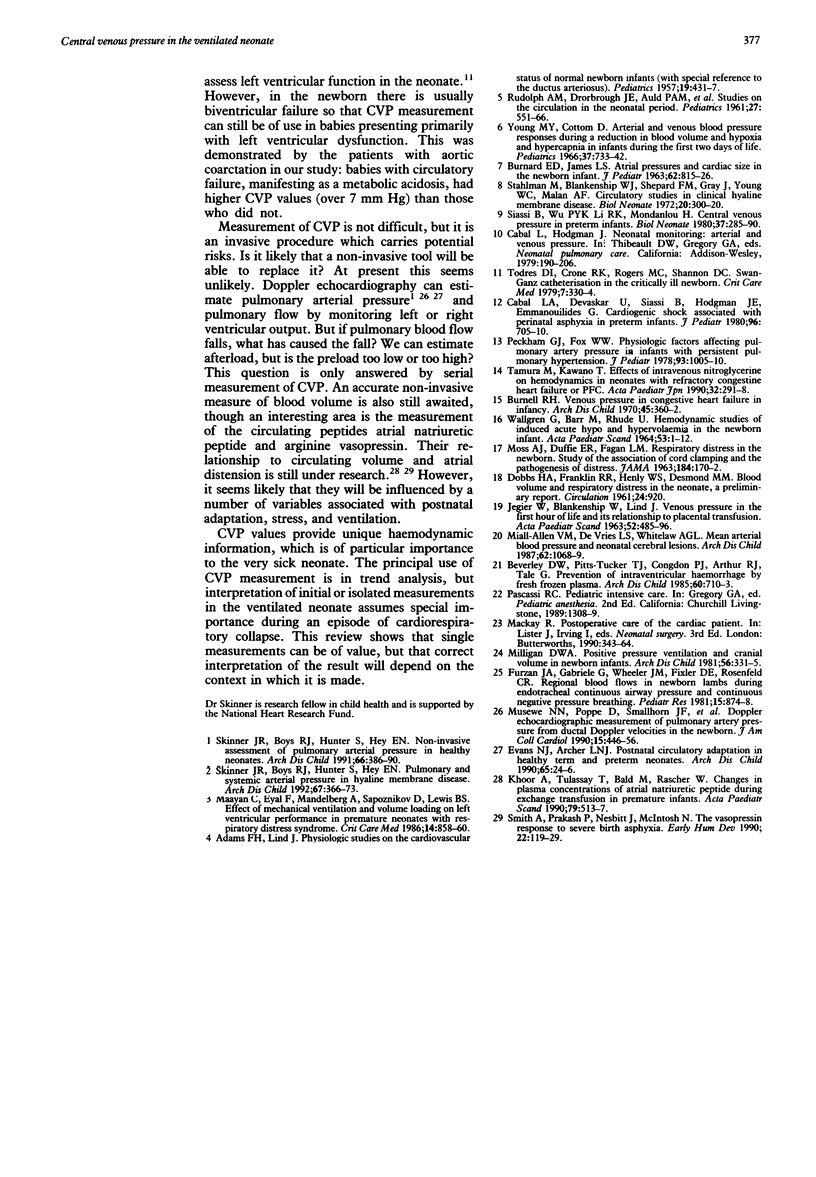
As there is no other measurement of right ventricular preload, central venous pressure (CVP) measurement provides unique and important haemodynamic information. CVP is not measured routinely in neonatology and there is a shortage of data in the ventilated neonate. CVP was measured in 62 ventilated neonates. Thirteen had respiratory disorders (28-42 weeks' gestation, birth weight 860-4390 g) and 49 had congenital heart disease (birth weight 1600-4500 g, age 0.5-30 days). Data from other case reports are also presented. In the babies with respiratory distress, a value of zero was associated with clinical evidence of hypovolaemia and negative values, common in the unventilated neonate, did not occur in those who were ventilated. Values over 7 mm Hg were found in babies with evidence of myocardial dysfunction or persistent fetal circulation but were also found with transmitted high intrathoracic pressure, such as with pneumothorax. In the babies with congenital heart disease, values mostly lay between 4 and 8 mm Hg. Values outside this range, particularly above 8 mm Hg, were usually associated with profound metabolic acidosis, suggesting circulatory failure. While the main use of CVP measurement is in trend analysis, this report suggests that single measurements can be of value, though correct interpretation will depend on the context in which they are made.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ADAMS F. H., LIND J. Physiologic studies on the cardiovascular status of normal newborn infants (with special reference to the ductus arteriosus). Pediatrics. 1957 Mar;19(3):431–437. [PubMed] [Google Scholar]
- BURNARD E. D., JAMES L. S. Atrial pressures and cardiac size in the newborn infant. Relationships with degree of birth asphyxia and size of placental transfusion. J Pediatr. 1963 Jun;62:815–826. doi: 10.1016/s0022-3476(63)80095-5. [DOI] [PubMed] [Google Scholar]
- Beverley D. W., Pitts-Tucker T. J., Congdon P. J., Arthur R. J., Tate G. Prevention of intraventricular haemorrhage by fresh frozen plasma. Arch Dis Child. 1985 Aug;60(8):710–713. doi: 10.1136/adc.60.8.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnell R. H. Venous pressure in congestive heart failure in infancy. Arch Dis Child. 1970 Jun;45(241):360–362. doi: 10.1136/adc.45.241.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabal L. A., Devaskar U., Siassi B., Hodgman J. E., Emmanouilides G. Cardiogenic shock associated with perinatal asphyxia in preterm infants. J Pediatr. 1980 Apr;96(4):705–710. doi: 10.1016/s0022-3476(80)80750-5. [DOI] [PubMed] [Google Scholar]
- Evans N. J., Archer L. N. Postnatal circulatory adaptation in healthy term and preterm neonates. Arch Dis Child. 1990 Jan;65(1 Spec No):24–26. doi: 10.1136/adc.65.1_spec_no.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furzan J. A., Gabriele G., Wheeler J. M., Fixler D. E., Rosenfeld C. R. Regional blood flows in newborn lambs during endotracheal continuous airway pressure and continuous negative pressure breathing. Pediatr Res. 1981 May;15(5):874–878. doi: 10.1203/00006450-198105000-00010. [DOI] [PubMed] [Google Scholar]
- JEGIER W., BLANKENSHIP W., LIND J. VENOUS PRESSURE IN THE FIRST HOUR OF LIFE AND ITS RELATIONSHIP TO PLACENTAL TRANSFUSION. Acta Paediatr. 1963 Sep;52:485–496. doi: 10.1111/j.1651-2227.1963.tb03808.x. [DOI] [PubMed] [Google Scholar]
- Khoór A., Tulassay T., Bald M., Rascher W. Changes in plasma concentrations of atrial natriuretic peptide during exchange transfusion in premature infants. Acta Paediatr Scand. 1990 May;79(5):513–517. doi: 10.1111/j.1651-2227.1990.tb11505.x. [DOI] [PubMed] [Google Scholar]
- Maayan C., Eyal F., Mandelberg A., Sapoznikov D., Lewis B. S. Effect of mechanical ventilation and volume loading on left ventricular performance in premature infants with respiratory distress syndrome. Crit Care Med. 1986 Oct;14(10):858–860. doi: 10.1097/00003246-198610000-00004. [DOI] [PubMed] [Google Scholar]
- Miall-Allen V. M., de Vries L. S., Whitelaw A. G. Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child. 1987 Oct;62(10):1068–1069. doi: 10.1136/adc.62.10.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milligan D. W. Positive pressure ventilation and cranial volume in newborn infants. Arch Dis Child. 1981 May;56(5):331–335. doi: 10.1136/adc.56.5.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musewe N. N., Poppe D., Smallhorn J. F., Hellman J., Whyte H., Smith B., Freedom R. M. Doppler echocardiographic measurement of pulmonary artery pressure from ductal Doppler velocities in the newborn. J Am Coll Cardiol. 1990 Feb;15(2):446–456. doi: 10.1016/s0735-1097(10)80076-2. [DOI] [PubMed] [Google Scholar]
- Peckham G. J., Fox W. W. Physiologic factors affecting pulmonary artery pressure in infants with persistent pulmonary hypertension. J Pediatr. 1978 Dec;93(6):1005–1010. doi: 10.1016/s0022-3476(78)81239-6. [DOI] [PubMed] [Google Scholar]
- Siassi B., Wu P. Y., Li R. K., Mondanlou H. Central venous pressure in preterm infants. Biol Neonate. 1980;37(5-6):285–290. doi: 10.1159/000241288. [DOI] [PubMed] [Google Scholar]
- Skinner J. R., Boys R. J., Hunter S., Hey E. N. Non-invasive assessment of pulmonary arterial pressure in healthy neonates. Arch Dis Child. 1991 Apr;66(4 Spec No):386–390. doi: 10.1136/adc.66.4_spec_no.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner J. R., Boys R. J., Hunter S., Hey E. N. Pulmonary and systemic arterial pressure in hyaline membrane disease. Arch Dis Child. 1992 Apr;67(4 Spec No):366–373. doi: 10.1136/adc.67.4_spec_no.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A., Prakash P., Nesbitt J., McIntosh N. The vasopressin response to severe birth asphyxia. Early Hum Dev. 1990 Jun;22(3):119–129. doi: 10.1016/0378-3782(90)90178-l. [DOI] [PubMed] [Google Scholar]
- Stahlman M., Blankenship W. J., Shepard F. M., Gray J., Young W. C., Malan A. F. Circulatory studies in clinical hyaline membrane disease. Biol Neonate. 1972;20(3):300–320. doi: 10.1159/000240473. [DOI] [PubMed] [Google Scholar]
- Tamura M., Kawano T. Effects of intravenous nitroglycerin on hemodynamics in neonates with refractory congestive heart failure or PFC. Acta Paediatr Jpn. 1990 Jun;32(3):291–298. doi: 10.1111/j.1442-200x.1990.tb00827.x. [DOI] [PubMed] [Google Scholar]
- Todres I. D., Crone R. K., Rogers M. C., Shannon D. C. Swan-Ganz catheterization in the critically ill newborn. Crit Care Med. 1979 Aug;7(8):330–334. doi: 10.1097/00003246-197908000-00002. [DOI] [PubMed] [Google Scholar]
- WALLGREN G., BARR M., RUDHE U. HEMODYNAMIC STUDIES OF INDUCED ACUTE HYPO- AND HYPERVOLEMIA IN THE NEWBORN INFANT. Acta Paediatr. 1964 Jan;53:1–12. doi: 10.1111/j.1651-2227.1964.tb07200.x. [DOI] [PubMed] [Google Scholar]
- Young M., Cottom D. Arterial and venous blood pressure responses during a reduction in blood volume and hypoxia and hypercapnia in infants during the first two days of life. Pediatrics. 1966 May;37(5):733–742. [PubMed] [Google Scholar]


