Abstract
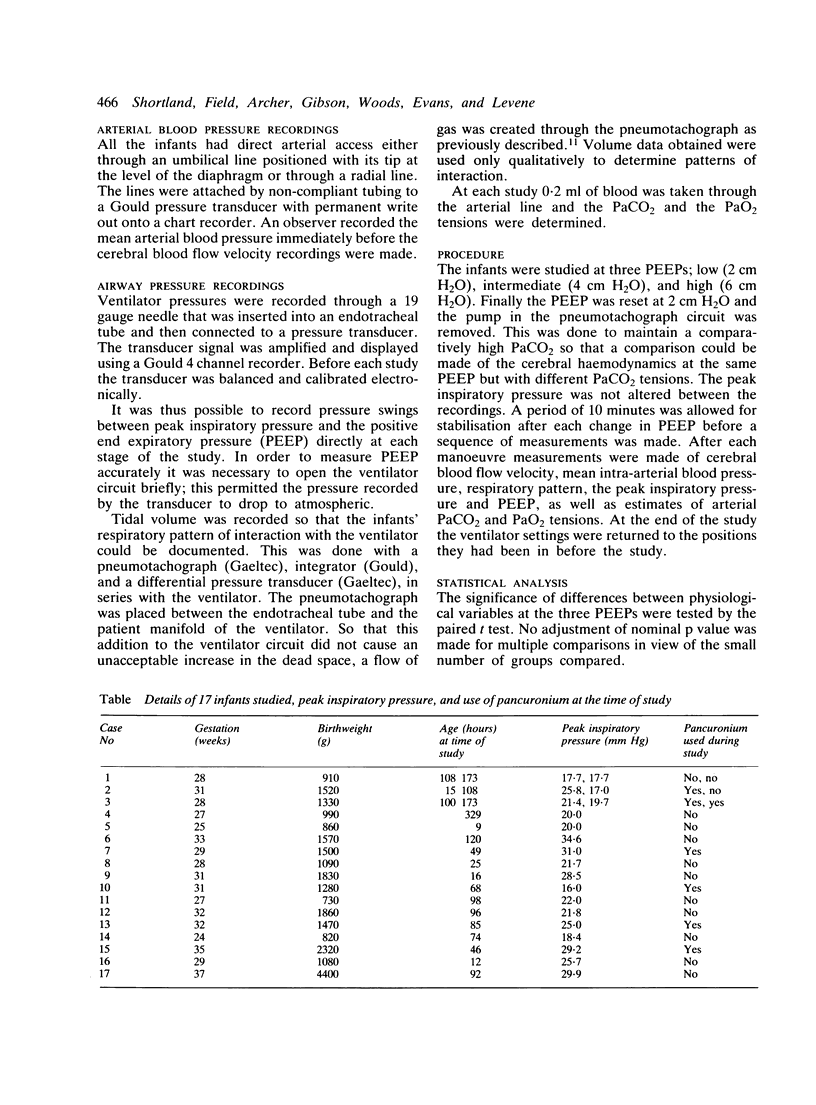
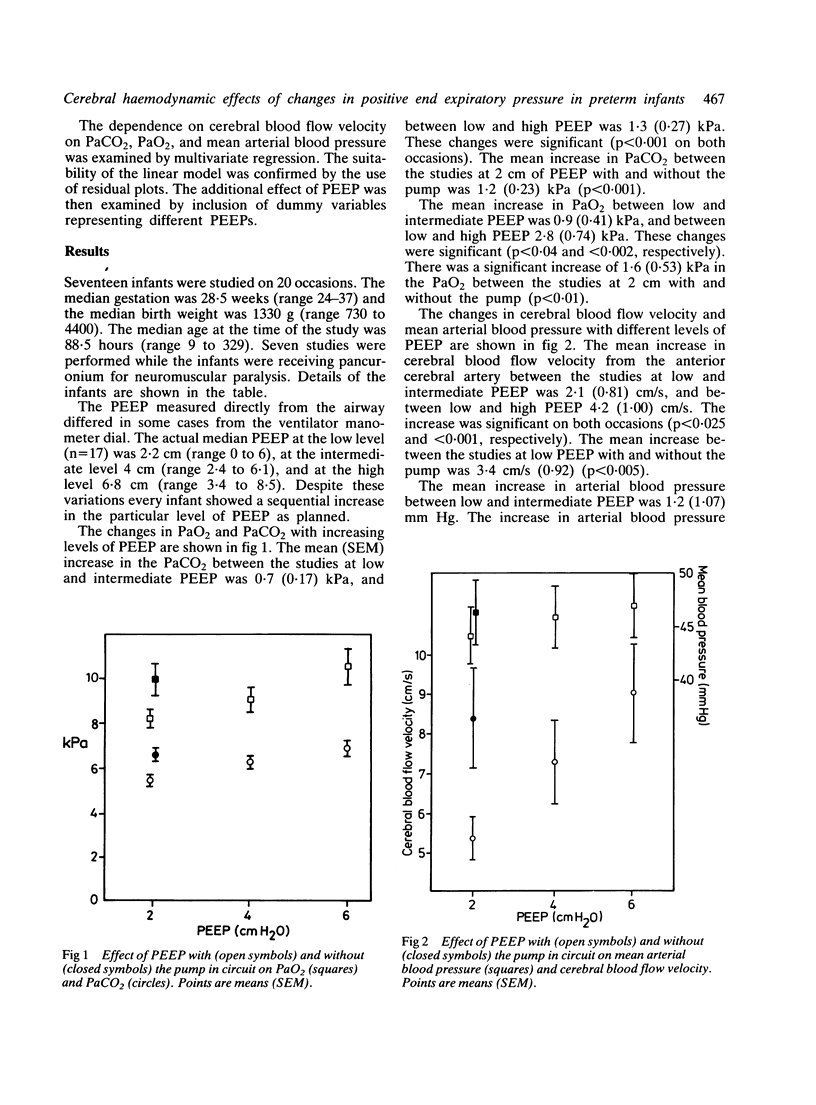
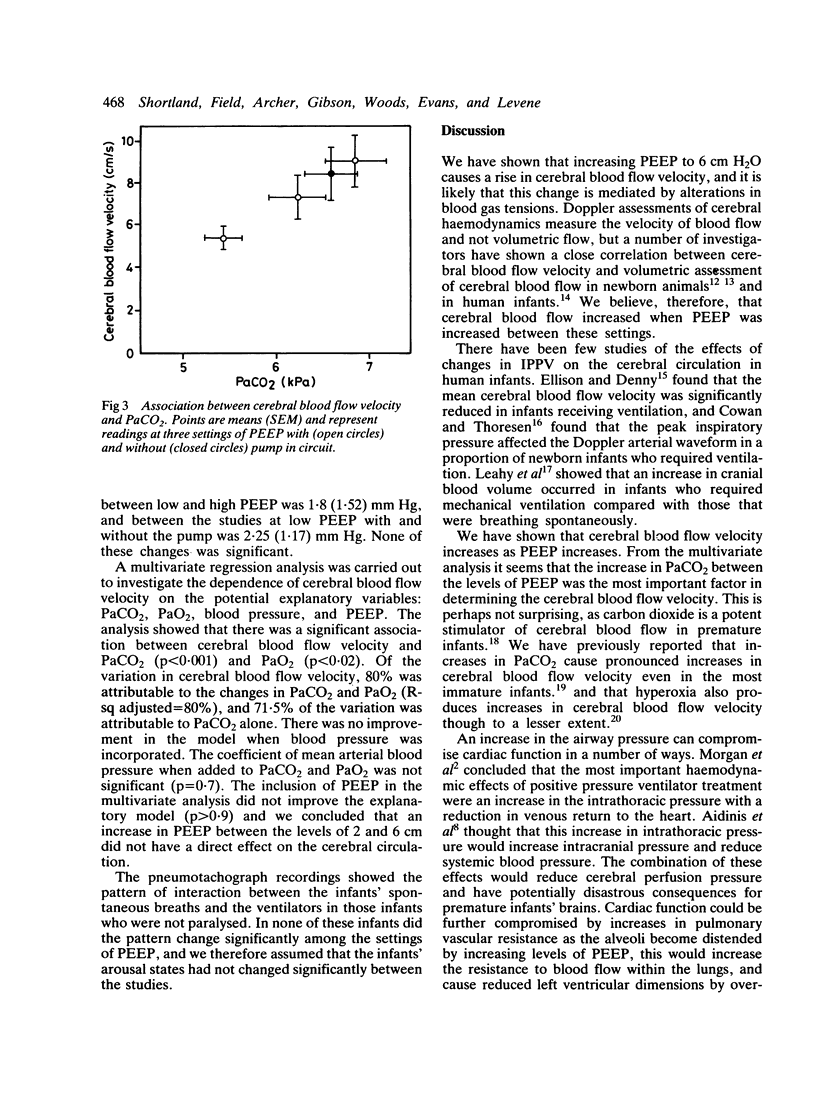
The effects of changes in positive end expiratory pressure (PEEP) on cerebral blood flow velocity, arterial blood gases, and mean arterial pressure were studied in newborn infants. In mechanically ventilated premature infants with severe respiratory disease, an increase in PEEP from 2 to 6 cm H2O was associated with an increase in cerebral blood flow velocity. There was no significant change in mean arterial blood pressure. There was a significant increase in PaO2 and PaCO2 for every stepwise rise in PEEP. Multivariate regression analysis showed that 72% of the effect on cerebral blood flow velocity was attributable to PaCO2 alone and that any change in blood pressure was not likely to contribute to these changes. There was no evidence that changes in PEEP within the commonly used range adversely affected the neonatal cardiovascular or cerebral circulations.
Full text
PDF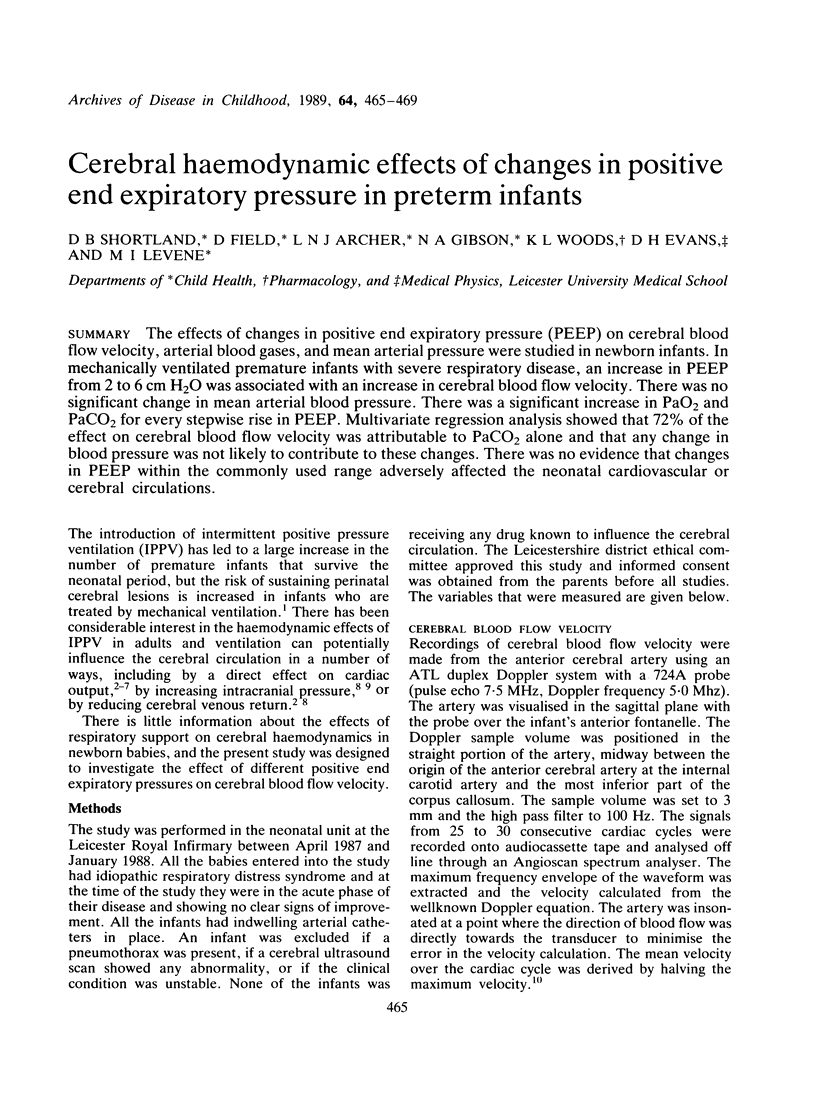
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aidinis S. J., Lafferty J., Shapiro H. M. Intracranial responses to PEEP. Anesthesiology. 1976 Sep;45(3):275–286. doi: 10.1097/00000542-197609000-00004. [DOI] [PubMed] [Google Scholar]
- Batton D. G., Hellmann J., Hernandez M. J., Maisels M. J. Regional cerebral blood flow, cerebral blood velocity, and pulsatility index in newborn dogs. Pediatr Res. 1983 Nov;17(11):908–912. doi: 10.1203/00006450-198311000-00014. [DOI] [PubMed] [Google Scholar]
- Cowan F., Thoresen M. The effects of intermittent positive pressure ventilation on cerebral arterial and venous blood velocities in the newborn infant. Acta Paediatr Scand. 1987 Mar;76(2):239–247. doi: 10.1111/j.1651-2227.1987.tb10454.x. [DOI] [PubMed] [Google Scholar]
- Evans D. H. On the measurement of the mean velocity of blood flow over the cardiac cycle using Doppler ultrasound. Ultrasound Med Biol. 1985 Sep-Oct;11(5):735–741. doi: 10.1016/0301-5629(85)90107-3. [DOI] [PubMed] [Google Scholar]
- Field D., Milner A. D., Hopkin I. E. High and conventional rates of positive pressure ventilation. Arch Dis Child. 1984 Dec;59(12):1151–1154. doi: 10.1136/adc.59.12.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greisen G., Johansen K., Ellison P. H., Fredriksen P. S., Mali J., Friis-Hansen B. Cerebral blood flow in the newborn infant: comparison of Doppler ultrasound and 133xenon clearance. J Pediatr. 1984 Mar;104(3):411–418. doi: 10.1016/s0022-3476(84)81108-7. [DOI] [PubMed] [Google Scholar]
- Greisen G., Trojaborg W. Cerebral blood flow, PaCO2 changes, and visual evoked potentials in mechanically ventilated, preterm infants. Acta Paediatr Scand. 1987 May;76(3):394–400. doi: 10.1111/j.1651-2227.1987.tb10488.x. [DOI] [PubMed] [Google Scholar]
- Hansen N. B., Stonestreet B. S., Rosenkrantz T. S., Oh W. Validity of Doppler measurements of anterior cerebral artery blood flow velocity: correlation with brain blood flow in piglets. Pediatrics. 1983 Oct;72(4):526–531. [PubMed] [Google Scholar]
- Hausdorf G., Hellwege H. H. Influence of positive end-expiratory pressure on cardiac performance in premature infants: a Doppler-echocardiographic study. Crit Care Med. 1987 Jul;15(7):661–664. doi: 10.1097/00003246-198707000-00007. [DOI] [PubMed] [Google Scholar]
- Huseby J. S., Pavlin E. G., Butler J. Effect of positive end-expiratory pressure on intracranial pressure in dogs. J Appl Physiol Respir Environ Exerc Physiol. 1978 Jan;44(1):25–27. doi: 10.1152/jappl.1978.44.1.25. [DOI] [PubMed] [Google Scholar]
- Jardin F., Farcot J. C., Boisante L., Curien N., Margairaz A., Bourdarias J. P. Influence of positive end-expiratory pressure on left ventricular performance. N Engl J Med. 1981 Feb 12;304(7):387–392. doi: 10.1056/NEJM198102123040703. [DOI] [PubMed] [Google Scholar]
- Leahy F. A., Cates D., MacCallum M., Rigatto H. Effect of CO2 and 100% O2 on cerebral blood flow in preterm infants. J Appl Physiol Respir Environ Exerc Physiol. 1980 Mar;48(3):468–472. doi: 10.1152/jappl.1980.48.3.468. [DOI] [PubMed] [Google Scholar]
- Levene M. I., Fawer C. L., Lamont R. F. Risk factors in the development of intraventricular haemorrhage in the preterm neonate. Arch Dis Child. 1982 Jun;57(6):410–417. doi: 10.1136/adc.57.6.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levene M. I., Shortland D., Gibson N., Evans D. H. Carbon dioxide reactivity of the cerebral circulation in extremely premature infants: effects of postnatal age and indomethacin. Pediatr Res. 1988 Aug;24(2):175–179. doi: 10.1203/00006450-198808000-00007. [DOI] [PubMed] [Google Scholar]
- Mirro R., Busija D., Green R., Leffler C. Relationship between mean airway pressure, cardiac output, and organ blood flow with normal and decreased respiratory compliance. J Pediatr. 1987 Jul;111(1):101–106. doi: 10.1016/s0022-3476(87)80354-2. [DOI] [PubMed] [Google Scholar]
- Morgan B. C., Martin W. E., Hornbein T. F., Crawford E. W., Guntheroth W. G. Hemodynamic effects of intermittent positive pressure respiration. Anesthesiology. 1966 Sep-Oct;27(5):584–590. doi: 10.1097/00000542-196609000-00009. [DOI] [PubMed] [Google Scholar]
- Niijima S., Shortland D. B., Levene M. I., Evans D. H. Transient hyperoxia and cerebral blood flow velocity in infants born prematurely and at full term. Arch Dis Child. 1988 Oct;63(10 Spec No):1126–1130. doi: 10.1136/adc.63.10_spec_no.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qvist J., Pontoppidan H., Wilson R. S., Lowenstein E., Laver M. B. Hemodynamic responses to mechanical ventilation with PEEP: the effect of hypervolemia. Anesthesiology. 1975 Jan;42(1):45–55. doi: 10.1097/00000542-197501000-00009. [DOI] [PubMed] [Google Scholar]
- Santamore W. P., Heckman J. L., Bove A. A. Cardiovascular changes from expiration to inspiration during IPPV. Am J Physiol. 1983 Aug;245(2):H307–H312. doi: 10.1152/ajpheart.1983.245.2.H307. [DOI] [PubMed] [Google Scholar]


