Abstract
The Centers for Disease Control and Prevention (CDC) and 35 partner organizations have engaged in developing an agenda for Preconception Health. A summit was held in June 2005 to discuss the current state of knowledge regarding preconception care and convene a select panel to develop recommendations and action steps for improving the health of women, children, and families through advances in clinical care, public health, and community action. A Select Panel on Preconception Care, convened by CDC, deliberated critical related issues and created refined definition of preconception care. The panel also developed a strategic plan with goals, recommendations, and action steps for improving preconception health. The recommendations and action steps are specific to the implementation of health behavior, access, consumer demand, research, and surveillance activities for monitoring and improving the health of women, children and families. The outcome of the deliberations is the CDC publication of detailed recommendations and action steps in the Morbidity and Mortality Weekly Report series, Recommendations and Reports.
Keywords: Preconception care, Maternal health, Health behavior, Research and surviellance, Access to care
Introduction
In June 2005 the Centers for Disease Control and Prevention (CDC) and the March of Dimes, in collaboration with 35 professional and governmental organizations, convened a 3-day summit to discuss an agenda for preconception care programs, research, and policy. The summit was the result of internal workgroup discussions at CDC and an initial meeting with external stakeholders in November 2004. Prior to the November meeting, subject matter experts in 19 programs from 8 centers throughout CDC conducted a detailed review of the relevant literature. The 3-day summit was divided evenly into two components: a presentation series from preconception care practitioners, followed by a select panel meeting. More than 60 presentations on preconception care research and programs were made and subsequently discussed by the select panel to generate recommendations for improving maternal and child health outcomes through better preconception care. The goals of the select panel discussions were to define current scientific knowledge, to identify best practices, and to highlight key issues needing further attention that could be used as the basis for formulating recommendations and action steps.
Deliberations of the select panel
The select panel consisted of nationally recognized experts from a variety of disciplines representing different perspectives on preconception care services designed to promote women's health and reduce adverse pregnancy and perinatal outcomes. The panel included experts in the fields of obstetrics, family practice, pediatrics, public health, nursing, reproductive health, toxic exposures, and chronic and infectious disease. The initial conceptual framework for deliberations and discussions was based on the acronym “ACT” (Accessible health care, Comprehensive care, and Timely provision of care) proposed by Dr. Jennifer Howse, president of the March of Dimes. It was then expanded to include six “A’s”: access, availability, affordability, acceptability, accuracy, and appropriateness. Five organizing themes (clinical practice, social marketing and health promotion, public health and community, public policy and finance, data and research) served as the basis for discussion.
One key topic of debate was the potential conflict in characterizing preconception care as preparation for pregnancy, as opposed to the broader promotion of women's health. Some panelists believed strongly that the focus must be on both women and infant health outcomes. In moving forward, the panel was conscientious not to carve preconception care out separately from good routine primary care; however, panel members also asserted that even though the focus should be on preconception care, providers should also recognize that the scope of care should include comprehensive women's health services. As one panel member said, “Preconception care should be happening at every interaction with a woman or man of reproductive age…. It's part of what we’re already doing in primary care. We’re just trying to get providers to reframe their thinking so we’re achieving preconception health.” Some, while agreeing, argued that the ultimate goal was to improve perinatal outcomes, making this a part of, but distinct from, all well-woman's health care.
The status of current research emerged as a central issue. Discussions often centered around the concern that insufficient scientific evidence currently exists for many preconception care interventions, for the best methods of integrating them into primary care, and for effectively delivering interventions as a package—or even if they work. Many panelists cited the need for intervention trials. In contrast, other members believed that existing research findings were sufficient, and that moving in the direction of translation and action should be the next step. This theme was captured in one member's comment, “Research is important; there's no doubt about it. But instead of just creating more new knowledge, let's ask ourselves: Why is it that the knowledge we created before isn't getting translated into action?” Ultimately, the panel's recommendations reflected both areas where sufficient evidence exists and those where more research is needed.
Many panel members supported recommendations that would advocate provider assistance for a woman and her partner in developing a reproductive life plan and in communicating her/their intentions through the implementation of that plan. As one panel member described it, “[Primary care providers can] develop the ability to help a woman write her reproductive health plan and facilitate her ability to carry this out, including the upgrading of this plan throughout her reproductive years.” Some participants suggested that the recommendations should strongly encourage all providers not only to ask a woman about her reproductive intentions, but to ask in a manner that conveyed to the woman that her decisions should be based on her personal preferences. This would allow the provider to help her choose the best contraceptive for meeting her life goals and to provide appropriate preconception awareness information.
Panelists generally agreed that the recommendations should focus on feasible actions that could have the greatest positive impact on health outcomes. This resulted in much discussion of fundamental issues, including 1) who gets preconception care—women at high risk for adverse pregnancy outcomes or all women; 2) what would yield the greatest return on investment (e.g., focus on the preconception period or the interconception period; focus on all women or high-risk women); 3) whether interventions could be packaged and targeted to reach specific populations or address specific needs of women; and 4) how finance case and services, as well as the potential cost effectiveness and cost benefit of the proposed interventions?
Defining preconception care
The select panel worked to refine the definition of preconception care. The participants agreed that it is important to recognize what preconception care is and what it is not. Preconception care is not a single visit but a continuum of care designed to meet the needs of a woman throughout the various stages of her reproductive life. The goal of the preconception care process is to make sure that the woman is healthy as she attempts to become pregnant [1–6], and to promote her health and the health of her children throughout her reproductive lifespan. Based on the Select Panel deliberations and its subsequently published recommendations, preconception care is defined here as a set of interventions that aim to identify and modify biomedical, behavioral, and social risks to a woman's health or pregnancy outcome through prevention and management, emphasizing those factors that must be acted on before conception or early in pregnancy to have maximal impact. Thus, it is more than a single visit and less than all well-woman care. It includes care before a first pregnancy or between pregnancies (commonly known as interconception care) [7].
Preconception care and interventions are designed to reduce perinatal risk factors and, for optimal effectiveness, must be successfully implemented before the start of pregnancy [4]. The components of preconception care, including an array of interventions to address medical, psychosocial, and environmental risks associated with childbearing, augment routine well-woman care. Current Guidelines for Perinatal Care (jointly issued by the American Academy of Pediatrics and American College of Obstetricians and Gynecologists) recommend that “All health encounters during a woman's reproductive years, particularly those that are a part of preconception care, should include counseling on appropriate medical care and behavior to optimize pregnancy outcomes” [8, 9]. There is scientific evidence that certain preconception interventions are effective, yet at present they are not routinely and systematically applied.
The framework for preconception care recommendations
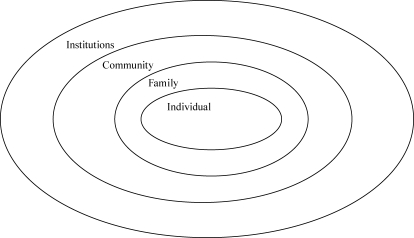
The framework for the recommendations and action steps to improve preconception health is based on two well-established models for community health and behavior change, the ecological and the lifespan models. The ecological model for medical care is constructed with the woman being the central player, while recognizing the significant roles of the larger community, the providers, and the institutions in ensuring the best outcomes for her (Fig. 1). The four levels of this model interact and are not distinct. Each level has primary responsibility for different aspects of health and well-being; however, all levels are integrated and each plays a supportive role in the success of the other levels and the system as a whole. If one level is not fully engaged, the system will weaken, and the result may be poor health for the individual woman. In many regards the community and institution levels overlap; institutions operate within the community, just as the community determines what services the institutions provide. Using this framework, the proposed recommendations outline actions and responsibilities at each level and demonstrate the role that all sectors have in improving preconception care and ultimately the health of women and their families. The recommendations and action steps described here aim to address needs and gaps at each level.
Fig. 1.
Ecological model
The second model influencing the framework for preconception care is the lifespan perspective [10]. This framework recognizes that health is determined by factors across the lifespan and is intergenerational. Improving preconception health will require, first, that the woman herself is achieving optimal health throughout her life. With women living in a healthy state, healthy children are more likely to result. As one panel member said, “We should build on the pediatric model of anticipatory guidance… [and] have consistent messages and care for women through the lifespan that will address women's and preconception health before, between and beyond.” Furthermore, good health in infancy is likely to carry through to childhood, adolescence, young adulthood and older adulthood so that healthy infants become healthy adults and achieve their reproductive goals. This lifespan framework extends beyond the individual to promote health in the family and community. Thus, the recommendations and action steps both address health needs across the lifespan and recognize that the individual, family, community, and institutions each have roles in ensuring that all women have lifelong optimal health.
Challenges for implementing the proposed frameworks
Maximizing the potential impact of preconception interventions will require integration across the various levels of care and areas of expertise [5, 11–13]. Changes in individual behavior, clinical practice, community programs, and public policies are recommended.
In the context of clinical care, much can be done by primary care providers, but evidence suggests that many women have two primary care providers—one with expertise in obstetrics and gynecology and one with general medical training. In addition, the U.S. health-care system is fragmented into highly specialized components. Nevertheless, bundling the various preconception interventions has the potential to improve perinatal outcomes and reduce costs associated with adverse outcomes. These recommendations call for more integrated delivery of health promotion and care services for women rather than for greater fragmentation of the health-care system. Integration is critical to moving forward, In consideration of competing priorities and limited resources, integration may achieve health-care economies of scale that produce more efficient delivery of services and more effective results in improving preconception health. For example, primary care providers potentially could routinely and efficiently use the tools available to screen for smoking, alcohol abuse, genetic risks, and occupational hazards; endocrinologists, geneticists, and nutritionists could become an integral part of a preconception care strategy. Moreover, settings such as family planning or sexually transmitted disease clinics must become part of an integrated approach in order to reach many women at high risk for adverse pregnancy outcomes. New models of care and well-designed quality-improvement efforts could foster the integration of preconception interventions.
At the same time, preconception care must be tailored to meet the needs of the individual woman. Given that preconception care is a process, not a visit, some recommendations will be more relevant to women at specific stages in their lives or those with varying levels of health risks. Health promotion efforts, risk screening, and interventions would be different for a young woman who has never experienced pregnancy than for a 35-year-old woman who has had three children. Women with chronic diseases, prior pregnancy complications, or behavioral risk factors may need more intensive interventions [5, 6, 11, 12]. At the clinical level, it is especially important that individual interventions be tailored to the specific needs of the woman. Such variations in interventions also place constraints on how interventions can and should be bundled or prepackaged.
This special issue of the Maternal and Child Health Journal, as well as the MMWR Recommendations and Reports, emphasizes components of preconception care supported by research and an evidence base that documents the efficacy of specific interventions [7]. For example, that increasing pre-pregnancy intake of folic acid reduces neural tube defects, and controlling diabetes prior to pregnancy yields better outcomes for mothers and babies [14, 15]. As with prenatal care or well-child care, however, evidence may not be forthcoming that one regimented process of preconception care significantly improves outcomes. Rather, the process of providing individualized screening, health education, and necessary interventions that can yield better outcomes.
Finally, implementing these recommendations to improve preconception health will take time. Diffusion of innovation theory demonstrates how concepts and best practices tend to be disseminated and adopted [16]. The innovators who lead current efforts to advance preconception care and the early adopters who run model programs are making only the first steps toward larger societal change. Whereas the select panel's action steps were designed to be short-term efforts, better implementing professional standards of care, modifying physician behaviors, developing effective health promotion messages, and adjusting payment mechanisms all will take time.
A strategic plan for improving women's health and pregnancy outcomes
Based on the June summit presentations and subsequent expert panel deliberations, 10 recommendations were developed (Table 1). These recommendations were based on four overarching goals that were identified as critical to help women reach optimal health and realize their reproductive goals. These four broad goals are 1) to improve both men's and women's knowledge, attitudes, and behaviors related to preconception health; 2) to ensure that all U.S. women of childbearing age receive preconception care services—screening, health promotion, and interventions—that will enable them to begin a pregnancy in optimal health; 3) to reduce risks indicated by a prior adverse pregnancy outcome through interventions during the interconception (inter-pregnancy) period that can prevent or minimize health problems for a mother and her future children; and 4) to reduce the health disparities in adverse pregnancy outcomes.
Table 1.
Panel Recommendations and Actions
| Recommendation 1. Individual responsibility across the lifespan. Each woman, man and couple should be encouraged to have a reproductive life plan. |
| Action Steps |
| • Develop, evaluate, and disseminate reproductive life planning tools for women and men in their childbearing years, respecting variations in age; literacy, including health literacy; and cultural/linguistic contexts |
| • Conduct research leading to development, dissemination, and evaluation of individual health education materials for women and men regarding preconception risk factors, including materials related to biomedical, behavioral, and social risks known to affect pregnancy outcomes |
| Recommendation 2. Consumer awareness. Increase public awareness of the importance of preconception health behaviors and preconception care services by using information and tools appropriate across various ages; literacy, including health literacy; and cultural/linguistic contexts |
| Action Steps |
| • Develop, evaluate, and disseminate age-appropriate educational curricula and modules for use in school health education programs |
| • Integrate reproductive health messages into existing health promotion campaigns (e.g., campaigns to reduce obesity and smoking) |
| • Conduct consumer-focused research necessary to develop messages and terms for promoting preconception health and reproductive awareness |
| • Design and conduct social marketing campaigns necessary to develop messages for promoting preconception health knowledge and attitudes, and behaviors among men and women of childbearing age |
| • Engage media partners to assist in depicting positive role models for lifestyles that promote reproductive health (e.g., delaying initiation of sexual activity, abstaining from unprotected sexual intercourse, and avoiding use of alcohol and drugs) |
| Recommendation 3. Preventive visits. As a part of primary care visits, provide risk assessment and educational and health promotion counseling to all women of childbearing age to reduce reproductive risks and improve pregnancy outcomes |
| Action Steps |
| • Increase health provider (including primary and specialty care providers) awareness regarding the importance of addressing preconception health among all women of childbearing age |
| • Develop and implement curricula on preconception care for use in clinical education at graduate, postgraduate, and continuing education levels |
| • Consolidate and disseminate existing professional guidelines to develop a recommended screening and health promotion package |
| • Develop, evaluate, and disseminate practical screening tools for primary care settings, with emphasis on the 10 areas for preconception risk assessment (e.g., reproductive history, genetic, environmental risk factors) |
| • Develop, evaluate, and disseminate evidence-based models for integrating components of preconception care to facilitate delivery of and demand for prevention and intervention services |
| • Apply quality improvement techniques (e.g., conduct rapid improvement cycles, establish benchmarks and brief provider training, use practice self-audits, and participate in quality improvement collaborative groups) to improve provider knowledge and attitudes, and practices and to reduce missed opportunities for screening and health promotion |
| • Use the federally funded collaboratives for community health centers and other FQHC to improve the quality of preconception risk assessment, health promotion, and interventions provided through primary care |
| • Develop fiscal incentives for screening and health promotion |
| Recommendation 4. Interventions for identified risks. Increase the proportion of women who receive interventions as follow-up to preconception risk screening, focusing on high priority interventions (i.e., those with evidence of effectiveness and greatest potential impact) |
| Action Steps |
| • Increase health provider (including primary and specialty care providers) awareness concerning the importance of ongoing care for chronic conditions and intervention for identified risk factors |
| • Develop and implement modules on preconception care for specific clinical conditions for use in clinical education at graduate, postgraduate, and continuing education levels |
| • Consolidate and disseminate existing professional guidelines related to evidence-based interventions for conditions and risk factors |
| • Disseminate existing evidence-based interventions that can be used in primary care settings (e.g., brief interventions for alcohol misuse and smoking) |
| • Develop fiscal incentives (e.g., pay for performance) for risk management, particularly in managed care settings |
| • Apply quality improvement techniques and tools (e.g., conduct rapid improvement cycles, establish benchmarks, use practice self-audits, and participate in quality improvement collaborative groups) |
| Recommendation 5. Interconception care. Use the interconception period to provide additional intensive interventions to women who have had a previous pregnancy which ended in adverse outcome (e.g., infant death, fetal loss, birth defects, low birthweight or preterm birth) |
| Action Steps |
| • Monitor the percentage of women who complete postpartum visits (e.g. using HEDIS measures for managed care plans and Title V Maternal Child Health Block Grant state measures), and use these data to identify communities of women at risk and opportunities to improve provider follow-up |
| • Develop, evaluate, and replicate intensive evidence-based interconception care and care coordination models for women at high social and medical risk |
| • Enhance the content of postpartum visits to promote interconception health |
| • Use existing public health programs serving women in the postpartum period to provide or link to interventions (e.g., family planning, home visiting, and WIC) |
| • Encourage additional states to develop preconception health improvement projects with funds from the Title V Maternal Child Health Block Grant, Prevention Block Grant, and similar public health programs |
| Recommendation 6. Prepregnancy check up. Offer, as a component of maternity care, one prepregnancy visit for couples and individuals planning pregnancy |
| Action Steps |
| • Modify third party payer rules to permit payment for one prepregnancy visit per pregnancy, including development of billing and payment mechanisms |
| • Consolidate existing professional guidelines to develop the recommended content and approach for such a visit |
| • Educate women and couples regarding the value and availability of prepregnancy planning visits |
| Recommendation 7. Health insurance coverage for women with low incomes. Increase public and private health insurance coverage among women with low incomes to improve access to preventive women's health, preconception, and interconception care |
| Action Steps |
| • Improve the design of family planning waivers by permitting states (by federal waiver or by creating a new state option) to offer interconception risk assessment, counseling, and interventions along with family planning services. Such policy developments would create new opportunities to finance interconception care |
| • Increase health coverage among women who have low incomes and are of childbearing age by using federal options and waivers under public and private health insurance systems and the State Children's Health Insurance Program |
| • Increase access to health-care services through policies and reimbursement levels for public and private health insurance systems to include a full range of clinicians who care for women |
| Recommendation 8. Public health programs and strategies. Integrate components of preconception health into existing local public health and related programs, including emphasis on interconception interventions for women with previous adverse outcomes |
| Action Steps |
| • Use federal and state agency support to encourage more integrated preconception health practices in clinics and programs |
| • Provide support for CDC programs to develop, evaluate, and disseminate integrated approaches to promote preconception health |
| • Analyze and evaluate the preconception care activities used under the federal Healthy Start program and support replication projects |
| • Convene or use local task forces, coalitions, or committees to discuss opportunities for promotion and prevention in preconception health at the community level |
| • Develop and support public health practice collaborative groups to promote shared learning and dissemination of approaches for increasing preconception health |
| Recommendation 9. Research. Increase the evidence base and promote the use of the evidence to improve to preconception health |
| Action Steps |
| • Prepare an updated evidence-based systematic review of all published reports on science, programs, and policy (e.g., through the Agency for Healthcare Research and Quality) |
| • Encourage and support evaluation of model programs and projects, including integrated service delivery and community health promotion projects |
| • Conduct quantitative and qualitative studies to advance knowledge of preconception risks and clinical and public health interventions, including knowledge of more integrated practice strategies and interconception approaches |
| • Design and conduct analyses of cost-benefit and cost-effectiveness as part of the study of preconception interventions |
| • Conduct health services research to explore barriers to evidence-based and guidelines-based practice |
| • Conduct studies to examine the factors that results in variations in individual use of preconception care (i.e., barriers and motivators that affect health-care use) |
| • Support activities to translate research into clinical practice and public health action |
| Recommendation 10. Monitoring improvements. Maximize public health surveillance and related research mechanisms to monitor preconception health |
| Action Steps |
| • Apply public health surveillance strategies to monitor selected preconception health indicators (e.g., folic acid supplementation, smoking cessation, alcohol misuse, diabetes, and obesity) |
| • Expand data systems and surveys (e.g., PRAMS and NSFG) to monitor individual experiences related to preconception care |
| • Use geographic information system techniques to target preconception health programs and interventions to areas where high rates of poor health outcomes exist women of reproductive age and their infants |
| • Use analytic tools (e.g., PPOR) to measure and monitor the proportion of risk attributable to the health of women before pregnancy |
| • Include preconception, including interconception, health measures and population-based performance monitoring systems (e.g., in national and state Title V programs) |
| • Include a preconception measure in the Healthy People 2020 objectives |
| • Develop and implement indicator quality improvement measures for all aspects of preconception care. For example, use HEDIS measures to monitor the percentage of women who complete postpartum visits |
For each of the 10 recommendations, the panelists identified specific actions. For each action step, those persons primarily responsible for implementation as well as those who had supportive roles were listed. The action steps were designed as feasible and practical activities that could be undertaken in the near future and could result in change in the next 2 to 5 years.
These goals, recommendations, and action steps form a strategic plan for improving preconception health and pregnancy outcomes. This can be illustrated as a pyramid (Fig. 2), building from the smaller attainable actions steps to fulfilling a recommendation, to attainment of the four goals, and finally to the combination of the goals to reach the pinnacle of the pyramid—a vision for better women's health and improved pregnancy outcomes.
Fig. 2.
Preconception care pyramid
The recommendations presented here focus on individual health knowledge and behavior, clinical care, public health programs, and health-care policies, improving preconception health will require the involvement of and changes in other sectors, including education, housing, urban planning, and environmental health. Moving forward, these sectors should be included as part of the comprehensive solution to improving women's health and, by extension, the health of families. In all of the action steps, women and their families have a critical role to play in engaging the system and developing the consumer demand and culture to normalize preconception care as part of women's health promotion and routine care.
The focus of the recommendations
The 10 recommendations outlined in Table 1 address individual, provider, system, and research needs that mirror the different levels described in the ecological model. Under each of the recommendations there are multiple actions steps that describe specific activities geared towards achieving the recommendations.
The first two recommendations focus on individual responsibility for preconception health. Under these recommendations, action steps are focused on the development, evaluation, and dissemination of tools to help women and their partners make decisions regarding their reproductive health across the lifespan. The action steps clearly highlight the need to ensure that these tools are age-appropriate and culturally relevant and cover both general health topics and specific risk behaviors. The action steps recognize the importance of being able to integrate preconception health-care messages with existing health promotion activities whenever possible. This is especially important in an environment with limited resources for health promotion activities. Both recommendations 1 and 2 call for action to be taken at both the individual and community level so that societal norms shift toward supporting optimal preconception health behaviors.
Recommendations 3, through 6 call for actions to improve health-care services and are particularly focused on changing provider knowledge, attitudes, and behaviors. Because the existing knowledge base has not been widely disseminated, the action steps call for new and continuing education activities to help all providers improve their skills and coverage of preconception care services. The use of quality improvement tools and techniques are suggested as a means of changing professional practices. In the current market-driven environment, it is clear that incentives such as pay for performance and risk management activities also must be developed to help encourage the provision of these services.
Recommendations 5 and 6 particularly focus more on improving preconception care and health for specific groups of women. Recommendation 5 focuses on interconception care and the opportunity for the prevention of adverse pregnancy outcomes among those who are at risk for or have previously had pregnancy complications. In addition to action steps aimed at modifying provider practices, others encourage public health programs to do more identification and follow-up of women at risk. Recommendation 6 suggests pre-pregnancy checkups or visits for couples to focus on their health and risks when they are trying to conceive. The action steps include consumer education and consolidated professional guidelines, as well as better third-party health insurance coverage of such visits as a part of prenatal and maternity coverage.
Action steps for recommendation 7 call for increased health-care coverage among uninsured, low-income women, specifically through Medicaid. Currently, most low-income women do not qualify for Medicaid unless they are pregnant; unfortunately, this is often too late for some health promotion and therapeutic interventions to have maximum impact on the health of the woman and her child.
Recommendation 8 describes a series of action steps that public health and community programs can take to improve preconception health by increasing the access to and use of preconception care services. These steps include using publicly funded women's and children's health programs to promote preconception health, to screen for health risks, and to refer women at risk to appropriate clinicians. For example, preconception health promotion messages are complementary to the purposes of family planning and HIV/STD clinics. However, the use of publicly funded women's and children's health programs for these purposes will require that federal and state public health agencies minimize the categorical restrictions that often prevent true integration at the community level. The second two action steps encourage the adaptation, implementation, and evaluation of community-based programs that provide preconception services. There are model programs currently being implemented that could be modified and used to meet the unique needs of specific populations. A key component of these actions is to engage the community to develop the best methods for development, implementation, and evaluation of local preconception care programs. Without community support and designs that truly represent the needs of the communities, programs will be ineffective.
Recommendations 9 and 10 include action steps focused on the continuous quality improvement and planning feedback loop that supports excellence in health-care systems. Research and evaluation are critical to examining progress toward achieving goals. Currently, a need exists for updating the systematic reviews of existing literature on preconception care interventions as well as increasing the knowledge base through qualitative and quantitative research projects. Economic analyses of preconception care interventions are not often conducted, and a great deal of work must be done to understand the impact of interventions. Limitations exist in many of the interventions currently available; and effective interventions have not been developed in some areas. Meeting the need for research and evaluation is a key factor in the ability to continue moving the field forward. In addition to research activities, ongoing monitoring systems—typically managed by public health agencies—are critical to program planning, development, and evaluation. This recommendation includes the use of surveillance systems such as the Pregnancy Risk Assessment and Monitoring System (PRAMS) and the Health Employee Data and Information Set (HEDIS) measures.
Conclusion
Improving preconception health requires changes in the knowledge, attitudes, and behaviors of individuals, families, communities, and institutions (e.g., government, health-care settings). The purpose is to improve the health of each woman before any pregnancy and to thereby affect the future health of the woman, her child, and her family. Through the CDC Preconception Health Initiative and the deliberations of the Select Panel on Preconception Care, a set of goals, recommendations, and specific actions steps have been developed to form a strategic plan. The framework incorporates both an ecological model and a lifespan perspective on health. This work also recognizes the unique contributions and challenges faced by individual women and their families, communities, and institutions. As one Select Panel member put it, “If you raise the level of health of women in a society, you’ve raised the level of health of families and the community at the same time.” The successful implementation of the recommendations will help achieve the vision for preconception health and pregnancy outcomes where
All women and men of childbearing age have high reproductive awareness (e.g., understand risk factors related to childbearing).
All women have a reproductive life plan (e.g., whether or when they wish to have children, how they will maintain their reproductive health).
All pregnancies are intended and planned.
All women of childbearing age have health-care coverage.
All women of childbearing age are screened prior to pregnancy for risks related to the outcomes of pregnancy.
Women with a prior pregnancy loss (e.g., infant death due to very low birthweight or preterm birth) have access to intensive interconception care aimed at reducing their risks.
References
- 1.Moos MK. Preconceptional wellness as a routine object for women's health care: an integrative strategy. JOGNN 2003;32:550–6. [DOI] [PubMed]
- 2.Moos MK. Preconceptional health promotion: progress in changing a prevention paradigm. J Perinat Neonat Nurs 2004;18:2–13. [DOI] [PubMed]
- 3.American College of Obstetrics and Gynecology Committee. The importance of preconception care in the continuum of women's health care [Opinion]. ACOG 2005;106:665–6. [DOI] [PubMed]
- 4.Atrash H, Adams M, Cordero J, Johnson K, Howse J. Time to act on missed opportunities to improve perinatal outcomes: preconception care. Mat Child Health J 2006. [DOI] [PMC free article] [PubMed]
- 5.Frey KA. Preconception care by the nonobstetric provider. Mayo Clin Proc 2002;77:469–73. [DOI] [PubMed]
- 6.Mirsa DP, Grason H, Weisman C. An intersection of women's and perinatal health: the role of chronic conditions. Women's Health Issues 2000;10:256–67. [DOI] [PubMed]
- 7.Centers for Disease Control and Prevention. Recommendations for improving preconception health care. Morb Mortal Wkly Rep 2006.
- 8.American Academy of Pediatrics, American College of Obstetricians and Gynecologists. Guidelines for perinatal care. 5th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2002. Washington, DC: American College of Obstetricians and Gynecologists; 2002.
- 9.American College of Obstetricians and Gynecologists. Guidelines for women's health care. 2nd ed. Washington DC: American College of Obstetricians and Gynecologists; 1996.
- 10.Misra DP, Guyer B, Allston A. Integrated perinatal health framework: a multiple determinants model with a life span approach. Am J Prev Med 2003;25:65–75. [DOI] [PubMed]
- 11.Brundage SC. Preconception Health Care. Washington, DC: American Academy of Family Physicians 2002.
- 12.Korenbrot CC, Steinberg A, Bender C, Newberry S. Preconception care: a systematic review. Mat Child Health J 2002;6(2):75–88. [DOI] [PubMed]
- 13.Carlson KJ. Multidisciplinary women's health care and quality of care. Women's Health Issues 2000;10:219–25. [DOI] [PubMed]
- 14.Czeizel AE, Dudas I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med 1992;327:1832–5. [DOI] [PubMed]
- 15.Werler MM, Shapiro S, Mitchell AA. Periconceptional folic acid exposure and risk of recurrent neural tube defects. JAMA 1993;269:1257–61. [DOI] [PubMed]
- 16.Rogers EM. A prospective and retrospective look at the diffusion of innovation model. J Heal Com 2004;9:13–19. [DOI] [PubMed]