A 75-year-old white man without cardiac symptoms was referred to our cardiology clinic with a long history of abnormal electrocardiographic findings. Cardiac risk factors included hyperlipidemia and a family history of heart disease. Upon physical examination, his heart rate was 49 beats/min and his blood pressure was 106/70 mmHg. No extra heart sounds or murmurs were heard, even after provocative maneuvers. His electrocardiogram showed sinus bradycardia, left ventricular (LV) hypertrophy, and negative T waves in derivations from the precordium and the extremities (Fig. 1). Results of his Holter monitor studies were normal. Echocardiography revealed a preserved LV systolic function (ejection fraction, 0.55) with normal LV wall motion and thickness.
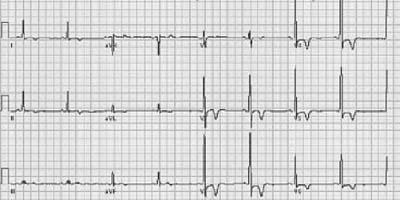
Fig. 1 A 12-lead electrocardiogram shows sinus bradycardia, left ventricular hypertrophy with effort, and T-wave inversions.
To investigate the cause of the abnormalities on the electrocardiogram, we performed cardiac magnetic resonance imaging (MRI). We obtained cardiac-gated, multiplanar cine images, which demonstrated a marked concentric thickening of the LV apex that gradually decreased to normal levels at the base (Fig. 2). There was no regional LV wall-motion abnormality (Fig. 2A).
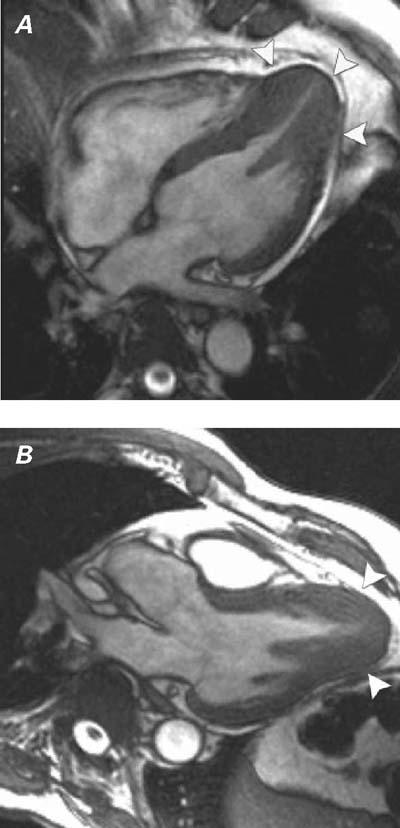
Fig. 2 Cardiac-gated, breath-hold, gradient-echo magnetic resonance images of the heart in A) 4-chamber and B) left ventricular outflow tract views show a marked hypertrophy of the left ventricle, which is more pronounced in the apex (arrowheads).
Real-time motion image of Fig. 2A is available at texasheart.org/journal.
Comment
Apical hypertrophic cardiomyopathy (HCM) is characterized by hypertrophy of the myocardium, predominantly in the left ventricular apex.1–5 This relatively rare variant of HCM, first described in Japan, constituted 13% to 25% of all cases of HCM in Japan1,2; however, it is seen much less often in non-Japanese populations.5 Despite a relatively good prognosis for apical HCM, long-term observations have occasionally included sudden cardiac death, severe arrhythmias, and apical infarctions with apical aneurysms.5 A “spade-shaped” configuration of the LV cavity at end-diastole on ventriculography and “giant” T-wave negativity in the electrocardiogram have been reported as the typical findings for this abnormality.1,2
Echocardiography has been the 1st-line imaging method for patients with suspected HCM, but its shortcomings in evaluating the apex are well known.4 A cardiac MRI should be performed if the electrocardiogram raises suspicion of apical HCM and if echocardiographic results are inconclusive or technically inadequate.3
Some echocardiographers will miss the diagnosis of apical thickening if the apex is not clearly seen, or if a thickened apex is mistaken for apical foreshortening on planar imaging.4 Cardiac MRI avoids this problem because it is less dependent on operators, is not subject to acoustic-window limitations, has multiplanar capability, and displays excellent soft-tissue contrast.3–5
Supplementary Material
Footnotes
Address for reprints: Servet Tatli, MD, Department of Radiology, Brigham and Women's Hospital, 75 Francis St., Boston, MA 02115 E-mail: statli@partners.org
References
- 1.Sakamoto T, Tei C, Murayama M, Ichiyasu H, Hada Y. Giant T wave inversion as a manifestation of asymmetrical apical hypertrophy (AAH) of the left ventricle. Echocardiographic and ultrasono-cardiotomographic study. Jpn Heart J 1976;17:611–29. [DOI] [PubMed]
- 2.Yamaguchi H, Nishiyama S, Nakanishi S, Nishimura S. Electrocardiographic, echocardiographic and ventriculographic characterization of hypertrophic non-obstructive cardiomyopathy. Eur Heart J 1983;4 Suppl F:105–19. [DOI] [PubMed]
- 3.Suzuki J, Shimamoto R, Nishikawa J, Yamazaki T, Tsuji T, Nakamura F, et al. Morphological onset and early diagnosis in apical hypertrophic cardiomyopathy: a long term analysis with nuclear magnetic resonance imaging [published erratum appears in J Am Coll Cardiol 1999;33:1750]. J Am Coll Cardiol 1999;33:146–51. [DOI] [PubMed]
- 4.Prasad K, Atherton J, Smith GC, McKenna WJ, Frenneaux MP, Nihoyannopoulos P. Echocardiographic pitfalls in the diagnosis of hypertrophic cardiomyopathy. Heart 1999;82 Suppl 3:III8-III15. [DOI] [PMC free article] [PubMed]
- 5.Eriksson MJ, Sonnenberg B, Woo A, Rakowski P, Parker TG, Wigle ED, Rakowski H. Long-term outcome in patients with apical hypertrophic cardiomyopathy. J Am Coll Cardiol 2002;39:638–45. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


