Abstract
This prospective study uses heart-type fatty-acid–binding protein (hFABP) and creatine kinase-MB (CK-MB) release to compare myocardial injury in on-pump versus off-pump coronary artery bypass grafting (CABG).
Fifty patients were randomly assigned to on-pump or off-pump CABG. The hFABP and CK-MB concentrations were measured in serial venous blood samples drawn before heparinization in both groups and after aortic unclamping at 1, 2, 4, 8, 24, 48, and 72 hours in the on-pump group. In the off-pump group, samples were taken after the last distal anastomosis at the same time intervals as in the on-pump group.
The total amount of hFABP and CK-MB released was significantly higher in the on-pump than in the off-pump group (hFABP = 100.43 ± 77.63 vs 3.94 ± 0.36 ng/mL, P <0.0001; CK-MB = 33.33 ± 3.81 vs 28.65 ± 3.91 log units, P <0.001). In all patients, hFABP levels peaked as early as 1 hour after declamping (on-pump group) or 2 hours after the last distal anastomosis (off-pump group), whereas CK-MB peaked only at 4 hours after declamping (on-pump group) or 24 hours after the last distal anastomosis (off-pump group).
The lower release of hFABP and CK-MB in the off-pump CABG group indicates that on-pump CABG with cardioplegic arrest causes more myocardial damage than does off-pump CABG. Heart-type fatty-acid–binding protein is a more rapid marker of perioperative myocardial damage, peaks earlier than CK-MB, and may predict the requirement for intensive monitoring for postoperative myocardial infarction.
Key words: Biological markers/blood; cardiopulmonary bypass; coronary artery bypass/methods; coronary artery bypass, off-pump; creatinine kinase, MB form; fatty acid-binding proteins; intraoperative complications; isoenzymes; myocardial ischemia/blood; myocardial revascularization/adverse effects; surgical procedures, minimally invasive
Coronary artery bypass grafting (CABG) with the aid of cardiopulmonary bypass (CPB) is a routine and safe procedure, associated with a mortality rate of 2% to 3% in elective cases. Cardiopulmonary bypass and cardioplegic arrest enable the performance of coronary artery anastomosis in a still and bloodless field. Nevertheless, notable morbidity remains, mostly because of the whole-body response to the nonphysiologic nature of CPB, which can propagate a systemic inflammatory response. In addition, aortic cross-clamping and cardioplegic arrest can result in myocardial dysfunction, and in some cases myocardial stunning. The introduction of better stabilizing systems, such as the Octopus and the Starfish, has revived interest in performing multivessel CABG on the beating heart. Early results of off-pump CABG suggest that better preservation of left ventricular contraction and mitochondrial function is attained than when cardioplegic arrest is used.1–3
Perioperative myocardial cellular damage is a major problem during CABG. Myocardial ischemia during cardiac surgery results in functional and structural changes and ultimately in release of protein from injured cardiomyocytes. These proteins vary in their release patterns and their cardiospecificity.4 Creatine kinase and its isoform, creatine kinase-MB (CK-MB), have been the most frequently used tools to diagnose myocardial ischemia.5 In recent years, structural myofibrillar proteins, such as troponin T and troponin I and their cardiospecific isoforms, have entered the clinical field and have been used in routine diagnostics, as well as in scientific clinical research.6–8 However, the delay between surgical damage and the detection of a measurable amount of protein in peripheral blood renders difficult the rapid evaluation of the degree of myocardial injury.
Heart-type fatty-acid–binding protein (hFABP), an intracellular molecule engaged in the transport of fatty acids through the myocardial cytoplasm, is a rapid marker of myocardial infarction.9 However, hFABP measurement has so far not achieved widespread clinical use, due to the lack of a test with appropriate availability and tissue specificity.
Petzold and coworkers10 have used this marker in the diagnosis of myocardial damage in conventional CABG. Hasegawa and colleagues11 have evaluated hFABP as a rapid indicator of myocardial damage in pediatric cardiac surgery. To our knowledge, no studies have used hFABP to compare on-pump CABG with off-pump CABG.
We studied the release pattern of hFABP and its relevance to myocardial injury in patients who underwent CABG with or without CPB and compared the results with those of an established marker protein of myocardial ischemia, CK-MB.
Patients and Methods
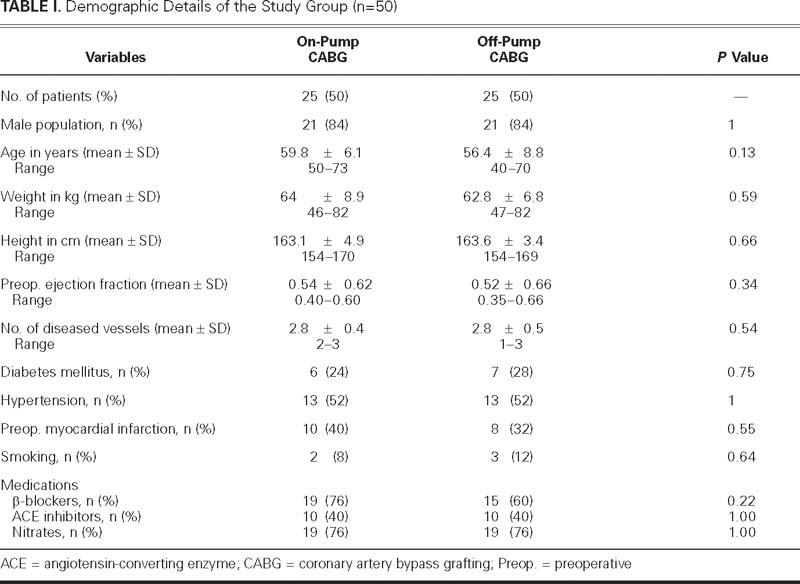
Patient Selection Criteria. We received institutional review board approval of our study protocol in October 2003 and thereafter obtained informed consent from all patients. Fifty adult patients of either sex who were scheduled to undergo CABG at our institution were randomly distributed to 1 of 2 groups: on-pump (n= 25), in which coronary revascularization was done with the use of CPB and moderate hypothermia; and off-pump (n=25), in which surgery was performed without the use of CPB. The groups' demographic and clinical profiles are presented in Table I. There were no significant differences between the 2 groups in age, sex, weight, height, comorbidities, or medications. According to cardiac catheterization data, the numbers of diseased vessels were comparable in the 2 population groups. All patients were eligible for either off-pump or on-pump revascularization.
TABLE I. Demographic Details of the Study Group (n=50)
Patients with aortic incompetence, poor ventricular function (ejection fraction ≤0.30), concomitant heart valve disease, unstable angina, renal disease, or chronic obstructive pulmonary disease were excluded, as were those on steroid therapy and those undergoing reoperation.
Anesthetic Technique. Anesthetic technique was standardized for all patients. Premedication of all patients in both groups was done with morphine (0.1 mg/kg) and promethazine (0.25 mg/kg), both injected intramuscularly 1 hour before surgery.
Anesthesia was induced with fentanyl/thiopental sodium, and orotracheal intubation was facilitated with rocuronium (0.6 mg/kg). Anesthesia was maintained with isoflurane (end-tidal concentration <1 minimum alveolar concentration) and additional doses of fentanyl, midazolam, and pancuronium in all patients.
Heparin and Protamine Management. In the on-pump group, heparin was administered at a dosage of 3 mg/kg to achieve a target activated clotting time (ACT) of 480 seconds or longer before the start of CPB. The ACT was monitored during the bypass period (every 30 minutes), and an additional 0.5 mg/kg of heparin was administered if required. In the off-pump group, heparin (1.5 mg/kg) was administered before the start of the 1st anastomosis or before the division of the left internal mammary artery. The target ACT in this group was 250 to 300 seconds. Protamine was used to reverse the effect of heparin at a dose ratio of 1.5:1.
Surgical Technique
On-Pump Group. All patients in the on-pump group underwent surgery on CPB by means of aortoatrial cannulation and moderate systemic hypothermia. The extracorporeal device consisted of a roller pump, a reservoir, and a membrane oxygenator. The circuit was primed with 1,500 mL of Ringer's lactate, containing 0.5 g/kg of mannitol and 5,000 IU of heparin. The pump flows were adjusted to maintain a cardiac index of more than 2.4 L/min/m2. Myocardial protection was achieved by intermittent antegrade administration of a cold-blood, St. Thomas-based cardioplegic solution.
Off-Pump Group. In the off-pump group, colloids were administered and body positions and gravity support (Trendelenburg, and right and left table rotation) were changed to stabilize the patient's hemodynamics and to maintain a mean systemic arterial pressure greater than 70mmHg. The distal anastomoses were performed first. Lesions of the left anterior descending coronary artery were bypassed with internal thoracic pedicle grafts where feasible. In general, collateralized vessels were grafted before collateralizing vessels. The sequence of graft construction was as follows: 1) left anterior descending with left internal thoracic artery; 2) diagonal artery; 3) main right coronary artery; 4) posterior descending artery; 5) distal circumflex, 2nd, 3rd obtuse marginal vessels; and 6) ramus intermedius artery. Target artery immobilization and regional myocardial control were achieved through a commercially available Octopus III stabilizer-suction system (Octopus Tissue Stabilizer, Medtronic, Inc.; Eden Prairie, Minn).
Biochemical Analysis. Blood samples were collected from each patient after sternotomy, before systemic heparinization, 1 hour after declamping (or after completion of the last distal anastomosis in the off-pump group), and then at 2, 4, 8, 24, 48, and 72 postoperative hours in both groups. Samples were immediately cooled to 4 °C and centrifuged at 3,000 rpm for 10 minutes at 4 °C. Plasma was stored at –70 °C until assay. Plasma levels of hFABP were measured by ELISA (Hycult Biotechnology; Uden, The Netherlands) and levels of CK-MB were measured by a photometric method (DiaSys Diagnostic Systems GmbH; Holzheim, Germany).
Clinical Variables. In addition to biochemical measurements, we recorded patients' need for inotropic agents, their duration of ventilation, and their duration of intensive care unit (ICU) stay. A patient's inotropic requirement was classified as none (either nitroglycerin or sodium nitroprusside), mild (dopamine, ≤5 μg/kg/min), or moderate (dopamine, >5 μg/kg/min or dobutamine, >5 μg/kg/min; or adrenaline <0.1 μg/kg/min).
Twelve-lead electrocardiography was performed preoperatively, at 2 hours postoperatively, and then daily for at least the first 3 postoperative days. All patients had continuous electrocardiographic monitoring until they were discharged from the ICU. Clinical diagnostic criteria for perioperative myocardial infarction were the development of new Q waves longer than 0.04 msec or a reduction in R waves of more than 25% in at least 2 leads.
A single cardiologist, who was blinded to the study, performed transthoracic 2-dimensional echocardiography in all patients to evaluate left ventricular function, at 8 hours postoperatively and again before discharge. Left ventricular function was defined as moderate (ejection fraction, 0.30–0.50) or good (ejection fraction, >0.50).
Data Analysis. Data were analyzed with the SPSS version 10.0 statistical package (SPSS Inc.; Chicago, Ill). Continuous and interval-related data were presented as mean ± standard deviation, whereas categorical variables were presented as frequency distribution and percentages. Continuous variables were analyzed using an independent t-test, and categorical variables were analyzed using a 2 test. Analysis of variance (ANOVA) was used to compare the differences in means for hFABP between the groups over a period of time, and this was followed by Bonferroni post hoc analysis. Data for CK-MB were transformed using natural logarithms, because they were not following normal distribution.
Results
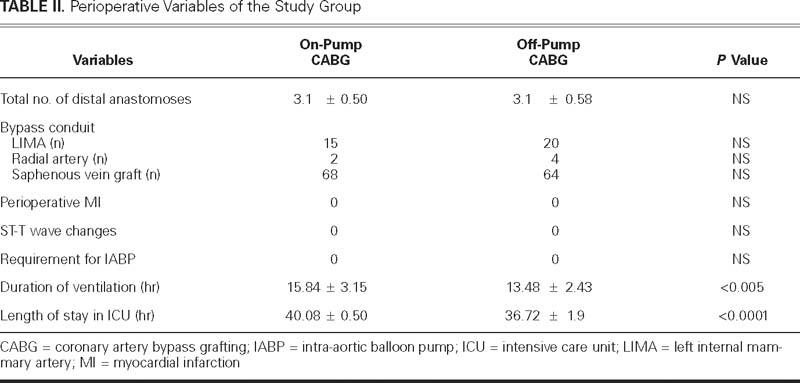
In the on-pump group, CPB time was 103.4 ± 28.6 minutes, and the aortic cross-clamp time was 53.4 ± 16.1 minutes. The numbers of distal anastomoses performed in the 2 groups were marginally different in the 2 groups and did not reach statistical significance (3.1 ± 0.50 vs 3.1 ± 0.58, P=1). There were significant differences between the on-pump and off-pump CABG groups in duration of mechanical ventilation (15.84 ± 3.15 vs 13.48 ± 2.43 hours, P <0.005) and ICU stay (40.08 ± 2.54 vs 36.72 ± 1.90 hours, P <0.0001) (Table II).
TABLE II. Perioperative Variables of the Study Group
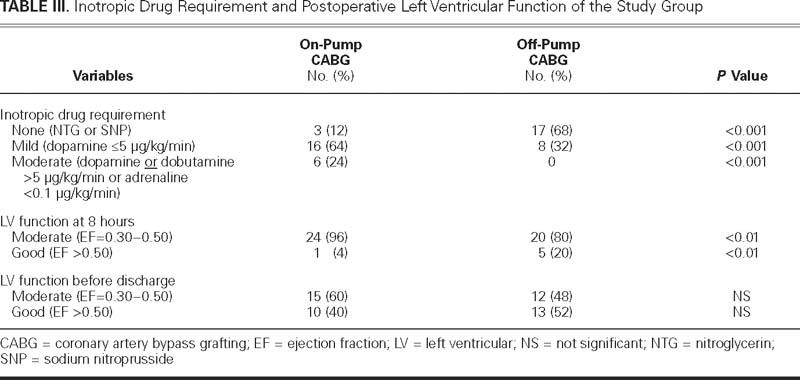
Three patients in the on-pump group and 17 in the off-pump group required no inotropic drug support. Six patients in the on-pump group required moderate inotropic support, whereas no patient required such support in the off-pump group (Table III). There was no perioperative myocardial infarction in either group as defined by electrocardiographic criteria or by in-hospital death. The postoperative course was smooth in all patients. There was transient moderate impairment of left ventricular ejection fraction (0.30–0.50) at 8 hours in all but 2 patients who underwent on-pump CABG (96% on-pump vs 80% off-pump, P <0.01). However, there was no noticeable difference in this regard at discharge (Table III).
TABLE III. Inotropic Drug Requirement and Postopera tive Left Ventricular Function of the Study Grou
Time Course of Mean Concentration of Biomarkers. Each marker protein displayed a typical laboratory pattern. The mean values rose from a baseline concentration preoperatively to a postoperative peak, indicating myocardial damage of a certain degree in all cases.
The total amount of hFABP released was higher in the on-pump CABG group than in the off-pump CABG group (100.43 ± 77.63 vs 3.94 ± 0.36 ng/mL, P <0.0001). For each sample drawn, hFABP concentrations were significantly higher in the on-pump group than in the off-pump group at 1,2,4, 8, 24, 48, and 72 hours (P <0.0001) (Table IV, Fig. 1).
TABLE IV. Perioperative Values of Cardiac Biomarkers after Coronary Artery Bypass Performed with 2 Different Techniques
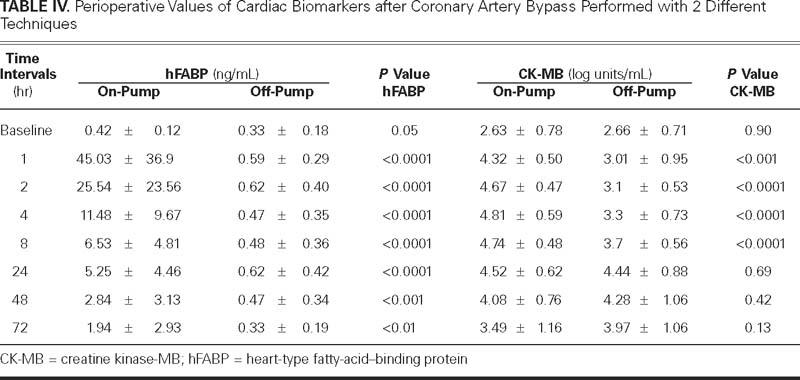
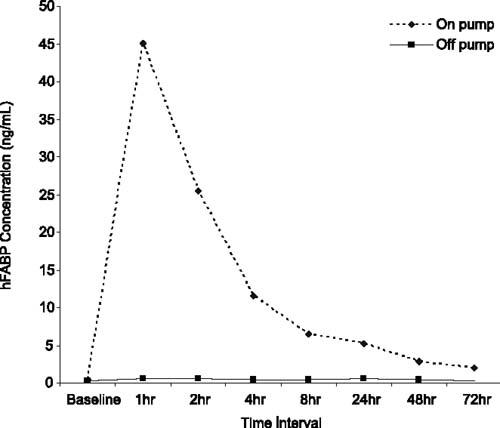
Fig. 1 Time course of hFABP concentrations, broken down by surgical procedure. The 2 curves differ significantly (P <0.0001). The hFABP concentration was significantly higher in the on-pump group than in the off-pump group at 1, 2, 4, 8, 24, 48, and 72 hours (P <0.0001).
Values are expressed as mean ± standard deviation.
hFABP = heart-type fatty-acid–binding protein
The total amount of CK-MB released was higher in the on-pump group than in the off-pump group (33.33 ± 3.81 vs 28.65 ± 3.91 log units, P <0.001). For each sample drawn, CK-MB concentrations were significantly higher in the on-pump group than in the off-pump group at 1, 2, 4, and 8 hours. However, CK-MB concentrations were comparable at 24, 48, and 72 hours (Table IV, Fig. 2).
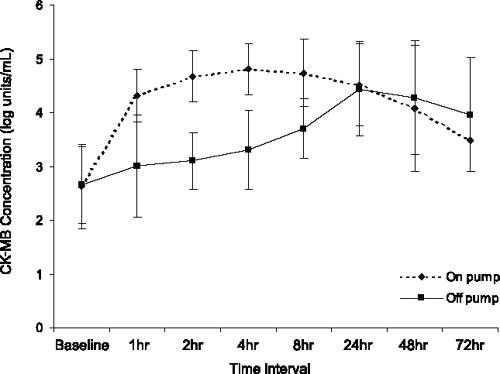
Fig. 2 Time course of CK-MB concentrations, broken down by surgical procedure. The 2 curves differ significantly (P <0.001). The CK-MB concentration was significantly higher in the on-pump group than in the off-pump group at 1, 2, 4, and 8 hours (P <0.001). CK-MB concentrations were comparable at 24, 48, and 72 hours.
Values are expressed as mean ± standard deviation.
CK-MB = creatine kinase-MB
Time to Peak Level. The hFABP reached its peak concentration 1 hour after cross-clamp removal in the on-pump group and 2 hours after distal anastomosis in the off-pump group. Creatine kinase-MB reached its peak concentration at 4 hours after cross-clamp removal in the on-pump group and at 24 hours after distal anastomosis in the off-pump group. The appearance of peak hFABP values occurred earlier than that of CK-MB in both groups (Table IV, Figs. 1 and 2).
Discussion
The major findings in this investigation were consistently higher elevations of hFABP and CK-MB in the onpump group than in the off-pump group. These indicate more myocardial injury in the on-pump group, despite optimal cardiac protection, compared with the off-pump group. One probable cause of the discrepancy is that on-pump CABG results in global ischemia, whereas off-pump CABG results in localized ischemia.
Heart-type fatty-acid–binding protein is a specific and highly sensitive marker of myocardial injury and perioperative myocardial ischemia.9–11 Petzold and coworkers, in their study, investigated hFABP for diagnosis of perioperative myocardial infarction during conventional CABG. They studied the release patterns of hFABP, CK-MB, and troponin I at intervals of 5 and 60 minutes after declamping, and 1, 2, and 10 days thereafter. They concluded that hFABP is a rapid marker of myocardial damage and peaks earlier than CK-MB or troponin I.10 In conventional CABG, serial samples of marker proteins taken immediately after reperfusion are more suitable for the detection of perioperative myocardial infarction than is a single value. Hasegawa and colleagues11 evaluated hFABP and concluded that it might be a rapid and potentially useful prognostic indicator of myocardial damage and clinical outcome in pediatric cardiac surgery.
Several other markers have been investigated for the estimation of myocardial injury.4–7,12–14 Creatine kinase-MB has long been used to establish a diagnosis of myocardial infarction, and cardiac troponin T has been evaluated as a marker of myocardial injury and a clinical indicator during follow-up. Khan and colleagues,15in a prospective randomized study, used troponin T to show that off-pump CABG was associated with less myocardial damage than was on-pump CABG (the area under the curve of troponin T levels was higher during the first 72 hours in the on-pump group than in the off-pump group (P <0.001).
Ascione and colleagues16,17 investigated the release pattern of troponin I for 24 hours and found lower troponin I release in off-pump CABG. Similarly, Alwan and associates18 studied the release pattern of troponin I for up to 24 hours and found higher troponin I concentrations in on-pump CABG. Troponin I, although a sensitive and specific marker of myocardial injury, appears late (8 hours) in the circulation after injury. The levels of troponin I peak at 8 to12 hours.18
Our study also disclosed that hFABP concentrations were significantly higher in every sample drawn in the on-pump group, whereas CK-MB concentrations were significantly higher only until the 8-hour mark. At 24, 48, and 72 hours, CK-MB concentrations were comparable in our 2 groups. Maybe CK-MB levels could not detect subtle myocardial damage in the 2 groups, whereas hFABP levels could detect the minor difference. Moreover, hFABP concentrations peaked earlier in both groups, compared with CK-MB concentrations.
The above observations have profound implications for the management of on-pump and off-pump CABG patients during the early postoperative period. Although most patients have an uneventful postoperative period after CABG regardless of technique, and few patients develop clinically significant myocardial infarction, intensive-care specialists see a large number of patients whose clinical situation is borderline (for example, nonspecific electrocardiographic changes, or mild hypotension with or without inotropic agents). Release of hFABP could help identify at an early stage those patients who, due to cardiac damage, could benefit from prolonged monitoring in an ICU. Because hFABP peaks quite a bit earlier than CK-MB, perioperative myocardial damage can be evaluated in the operating room or early in the ICU, and appropriate treatment can be instituted.
Study Limitations
Our study had a limitation in its evaluation of left ventricular function during the postoperative period: transthoracic echocardiography may not be a sufficient tool for the evaluation of left ventricular function because of its poor window in the immediate postoperative period. Radionuclide studies or magnetic resonance imaging for the evaluation of left ventricular function would have solidified our findings, and better distinctions between the 2 groups could have been established.
Second, it is unknown whether the reduction in release of myocardial enzymes in the off-pump group was associated with a reduction in perioperative myocardial stunning (reversible) or in necrosis (irreversible), because enzyme release may be partly due to increased turnover of cytoplasmic pools (which occurs in both stunning and necrosis). Cine- and contrast-enhanced magnetic resonance imaging could have established the functional significance of these biochemical markers through comparative quantification of myonecrosis in patients who underwent multivessel CABG with and without CPB.
Conclusions
We conclude that off-pump CABG provides better myocardial protection than does on-pump CABG, because hFABP and CK-MB protein release is reduced, and the requirement of postoperative inotropic support is lower. Serial determination of serum hFABP levels during the early postoperative period promises to be a useful tool in the rapid evaluation of perioperative myocardial damage.
Acknowledgment
The authors are grateful to Mr. Shankar Sharma for preparation of the manuscript.
Footnotes
Address for reprints: Ujjwal K. Chowdhury, MCh, Diplomate NB, Department of Cardiothoracic and Vascular Surgery, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110029, India. E-mail: ujjwalchow@rediffmail.com
References
- 1.Buffolo E, de Andrade CS, Branco JN, Teles CA, Aguiar LF, Gomes WJ. Coronary artery bypass grafting without cardiopulmonary bypass. Ann Thorac Surg 1996;61:63–6. [DOI] [PubMed]
- 2.Pfister AJ, Zaki MS, Garcia JM, Mispireta LA, Corso PJ, Qazi AG, et al. Coronary artery bypass without cardiopulmonary bypass. Ann Thorac Surg 1992;54:1085–92. [DOI] [PubMed]
- 3.Benetti FJ, Naselli G, Wood M, Geffner L. Direct myocardial revascularization without extracorporeal circulation. Experience in 700 patients. Chest 1991;100:312–6. [DOI] [PubMed]
- 4.Adams JE 3rd. Clinical application of markers of cardiac injury: basic concepts and new considerations. Clin Chim Acta 1999;284:127–34. [DOI] [PubMed]
- 5.Adams JE 3rd, Abendschein DR, Jaffe AS. Biochemical markers of myocardial injury. Is MB creatine kinase the choice for the 1990s? Circulation 1993;88:750–63. [DOI] [PubMed]
- 6.Adams JE 3rd, Bodor GS, Davila-Roman VG, Delmez JA, Apple FS, Ladenson JH, Jaffe AS. Cardiac troponin I. A marker with high specificity for cardiac injury. Circulation 1993;88:101–6. [DOI] [PubMed]
- 7.Carrier M, Pellerin M, Perrault LP, Solymoss BC, Pelletier LC. Troponin levels in patients with myocardial infarction after coronary artery bypass grafting. Ann Thorac Surg 2000; 69:435–40. [DOI] [PubMed]
- 8.Jacquet L, Noirhomme P, El Khoury G, Goenen M, Philippe M, Col J, Dion R. Cardiac troponin I as an early marker of myocardial damage after coronary bypass surgery. Eur J Cardiothorac Surg 1998;13:378–84. [DOI] [PubMed]
- 9.Glatz JF, van der Vusse GJ, Simoons ML, Kragten JA, van Dieijen-Visser MP, Hermens WT. Fatty-acid-binding protein and the early detection of acute myocardial infarction. Clin Chim Acta 1998;272:87–92. [DOI] [PubMed]
- 10.Petzold T, Feindt P, Sunderdiek U, Boeken U, Fischer Y, Gams E. Heart-type fatty acid binding protein (hFABP) in the diagnosis of myocardial damage in coronary artery bypass grafting. Eur J Cardiothorac Surg 2001;19:859–64. [DOI] [PubMed]
- 11.Hasegawa T, Yoshimura N, Oka S, Ootaki Y, Toyoda Y, Yamaguchi M. Evaluation of heart fatty-acid-binding protein as a rapid indicator for assessment of myocardial damage in pediatric cardiac surgery. J Thorac Cardiovasc Surg 2004;127:1697–702. [DOI] [PubMed]
- 12.Metzler H, Gries M, Rehak P, Lang T, Fruhwald S, Toller W. Perioperative myocardial cell injury: the role of troponins. Br J Anaesth 1997;78:386–90. [DOI] [PubMed]
- 13.Bonnefoy E, Filley S, Kirkorian G, Guidollet J, Roriz R, Robin J, Touboul P. Troponin I, troponin T, or creatine kinase-MB to detect perioperative myocardial damage after coronary artery bypass surgery. Chest 1998;114:482–6. [DOI] [PubMed]
- 14.Shiga T, Terajima K, Matsumura J, Sakamoto A, Ogawa R. Minor cardiac troponin T release in patients undergoing coronary artery bypass graft surgery on a beating heart. J Cardiothorac Vasc Anesth 2000;14:151–5. [DOI] [PubMed]
- 15.Khan NE, De Souza A, Mister R, Flather M, Clague J, Davies S, et al. A randomized comparison of off-pump and on-pump multivessel coronary-artery bypass surgery. N Engl J Med 2004;350:21–8. [DOI] [PubMed]
- 16.Ascione R, Caputo M, Angelini GD. Off-pump coronary artery bypass grafting: not a flash in the pan. Ann Thorac Surg 2003;75:306–13. [DOI] [PubMed]
- 17.Ascione R, Lloyd CT, Gomes WJ, Caputo M, Bryan AJ, Angelini GD. Beating versus arrested heart revascularization: evaluation of myocardial function in a prospective randomized study. Eur J Cardiothorac Surg 1999;15:685–90. [DOI] [PubMed]
- 18.Alwan K, Falcoz PE, Alwan J, Mouawad W, Oujaimi G, Chocron S, Etievent JP. Beating versus arrested heart coronary revascularization: evaluation by cardiac troponin I release. Ann Thorac Surg 2004;77:2051–5. [DOI] [PubMed]


