Abstract
Southeast Asians have higher liver cancer rates than any other racial/ethnic group in the US. Approximately 80 percent of liver cancers are etiologically associated with hepatitis B virus (HBV) infection which is endemic in Southeast Asia. An in-person survey of Cambodian women (n = 320) was conducted in Seattle, Washington, during 1999. The questionnaire included items about HBV knowledge, beliefs, and practices. Prior to being provided with a description of the disease, only about one-half (56 percent) of our respondents had heard of HBV infection. Less than one-quarter (23 percent) of the study group thought that asymptomatic individuals can transmit the disease to others. Most thought that HBV infection can cause liver cancer (54 percent) and death (72 percent). However, a minority thought that infection can be lifelong (24 percent) and incurable (15 percent). Only 38 percent reported they had been serologically tested for HBV. Finally, of those who had been tested and thought they were susceptible, two-thirds (67 percent) had not been vaccinated. Lower levels of education were associated with lower levels of HBV knowledge and serologic testing. Our findings suggest that Cambodian immigrants have low levels of HBV knowledge, serologic testing, and vaccination; and demonstrate a need for targeted educational interventions aimed at reducing HBV-related liver cancer mortality among Southeast Asian communities.
Keywords: hepatitis B, liver cancer, Cambodian Americans
INTRODUCTION
By 1990, census data indicate there were over one million Southeast Asians (including approximately 150,000 Cambodians) living in the United States (US).1 The majority of Cambodians left their country as refugees following the political and personal persecution imposed by the Khmer Rouge regime during the mid-1970s, and were relocated to North America from Thailand and the Philippines.2,3 Compared to the general US population as well as other Asian groups, Cambodian immigrants are both economically disadvantaged and linguistically isolated: nearly one-half of Cambodians live below the poverty level and over 90 percent speak Khmer at home.1 Cambodia is a largely agrarian society and, before the revolutionary period, the majority of Cambodians lived in rural or semi-rural settings.4 Therefore, immigrants from Cambodia are particularly unfamiliar with Western culture, institutions, and biomedical concepts of prevention.5,6
While hepatocellular carcinoma (HCC) is an uncommon tumor among individuals born in the US, it is the most common malignancy in many Asian countries.7,8 Emerging cancer registry data show that Southeast Asian men have a substantially elevated risk of liver cancer when compared to all other racial/ethnic groups in the US.9,10 California data for 1988–92 indicate that the incidence rate among Southeast Asian males is 39.4 per 100,000, compared to 3.1 among non-Latino whites.9 The male-to-female HCC incidence ratio is biased toward men in all populations (the reasons for this gender discrepancy are not resolved).11 However, Southeast Asian women are also at increased risk. Specifically, the following female liver cancer incidence rates were reported from the California cancer registry: Southeast Asians, 8.0 per 100,000; all Asian races combined, 5.1; and non-Latina whites, 1.1.9
About 80 percent of HCCs are etiologically associated with hepatitis B virus (HBV) infection which is endemic in Southeast Asia.12–14 Up to 60 percent of immigrants from Southeast Asia have serologic evidence of past HBV infection, while 40 percent remain susceptible to infection (and should be vaccinated against the disease).12 Further, up to 15 percent are chronic carriers (compared to less than 1 percent of the general US population): these individuals can transmit the disease to others and are at considerable risk of developing chronic acute hepatitis and cirrhosis, as well as liver cancer.12,15,16 In Asia, transmission of the virus usually occurs vertically at birth.13,14 However, several serologic studies conducted in the US show that the prevalence of previous HBV infection increases steadily from birth through age 20 in Asian immigrant communities.17,18 Therefore, it is clear that horizontal transmission, through close contact with family members and friends, also contributes to high infection rates among Southeast Asian immigrants.17,19 Finally, Cambodian adults are at considerable risk of HBV infection from sexual activity with other members of their community.20,21
Health education programs for immigrant groups should be based on a thorough understanding of the target population’s knowledge, beliefs, and practices.22 However, there is currently little published information about the hepatitis B-related health behavior of Southeast Asian immigrants. We recently conducted a community-based survey of Cambodian American women in Seattle, Washington. In this report, we describe the respondents’ knowledge and beliefs with respect to the transmission of HBV and the possible sequelae of infection, as well as their hepatitis B serologic testing and vaccination history.
METHODS
Overview
The data reported in this article were collected during the course of a randomized controlled trial to evaluate the effect of an intervention to increase Pap testing use among Cambodian refugees. The study design involved surveying Cambodian women, aged 18 and older, on two occasions. At the time of the 1999 follow-up survey, participants were asked to complete a series of questionnaire items about HBV (the intervention did not address hepatitis B or liver cancer). Our baseline survey methods have been reported in detail elsewhere.23 Four hundred and thirteen women completed the baseline questionnaire. The total estimated response rate was 73 percent and the cooperation rate (i.e., the response rate among reachable and eligible households) was 89 percent. Three hundred and twenty (77 percent) of the 413 women who participated in the baseline survey also completed the follow-up survey. Therefore, the estimated overall response rate with respect to the hepatitis B questions was 56 percent (i.e., 77 percent of 73 percent).
Study Sample
In Seattle, the Cambodian population is concentrated in the central and south regions of the city.24 In this project, we sought to recruit a representative sample of Cambodian women living in these regions. We developed a sampling frame using multiple sources of data on households located in the target areas. Households were identified from the following sources: electronic listings of all Asian clients of the Seattle Housing Authority and King County Housing Authority, a computer database of motor vehicle licenses from the State of Washington, and two CD-ROM telephone directory databases. From these sources, we selected households with zip codes corresponding to the target regions and linked the records to a database of Cambodian last names.
Survey Recruitment
We followed the same recruitment procedures for the baseline and follow-up surveys. Firstly, the surveys were publicized through Khmer-language posters distributed in community settings (e.g., Cambodian owned grocery stores and laundromats). Additionally, introductory letters, printed in both Khmer and English, were mailed to each household. All interviews were conducted in respondents’ homes by bilingual, bicultural Cambodian women. Survey participants were given a small token of appreciation for their time (a calendar featuring traditional Cambodian scenes at baseline, and $5 at follow-up), and were given the option of completing questionnaire items in either Khmer or English.
Survey Items
Three demonstration projects, aimed at increasing childhood HBV immunization rates among Asian and Pacific Islander populations, were recently funded by the Centers for Disease Control and Prevention.17 These projects, which are based in Hawaii, Philadelphia, and San Diego, all developed survey instruments for program evaluation purposes. Many of our hepatitis B questions were either taken verbatim or adapted from these instruments. Our HBV questionnaire was developed in English, translated into Khmer, back-translated to ensure lexical equivalence, reconciled, then pretested.25
Previous pilot work with the Seattle Cambodian community, conducted in 1990, showed that translations of the term hepatitis B were unfamiliar to Cambodians, while the symptoms of infection were well known.16 Therefore, we first asked about recognition of the term hepatitis, and then reframed the question in terms of its symptoms. Specifically, participants were asked whether they had ever heard about a disease or virus called hepatitis B. If they responded no or were unsure, they were read the following statement before the interviewer continued with other questions: “The disease or infection called hepatitis B is a liver problem that makes the skin and eyes go yellow.” Respondents were queried about previous serologic testing for HBV as well as vaccination against the disease. Eight questions addressed knowledge about the transmission of HBV, and four items addressed the possible sequelae of infection with the virus (Table 2). Participants were also asked if any of their family members were chronically infected with HBV, and whether they would want to be treated with traditional Cambodian medicine, Western medicine, or both types of medicine if they had liver disease. Finally, the questionnaire included several sociodemographic (i.e., age, marital status, and education) and acculturation (i.e., years in US and age at immigration) items. Because most Cambodian women have little formal education, we made the response options for our survey items as simple as possible. Specifically, with a few exceptions, the response options were as follows: yes, no, and don’t know/not sure.
TABLE 2.
Hepatitis B Knowledge (n = 320)
| Knowledge Variable | “Correct” Answer | Percent |
|---|---|---|
| Transmission | ||
| Which do you think is more easily spread from person to person: hepatitis B or AIDS?a | HBV | 1.6 |
| If someone is infected with hepatitis B but they look and feel healthy, do you think that person can spread hepatitis B?b | Yes | 23.1 |
| Do you think hepatitis B can be spread by eating food prepared by an infected person?c | No | 23.5 |
| Do you think hepatitis B can be spread by sharing a toothbrush with an infected person?b | Yes | 69.3 |
| Do you think hepatitis B can be spread by eating food that has been prechewed by an infected person?b | Yes | 67.0 |
| Do you think hepatitis B can be spread by being coughed on by an infected person?c | No | 10.7 |
| Do you think hepatitis B can be spread by having sexual intercourse with an infected person?b | Yes | 47.5 |
| Do you think hepatitis B can be spread by holding hands with an infected person?c | No | 69.0 |
| Sequelae | ||
| Do you think people with hepatitis B can be infected for life?b | Yes | 24.4 |
| Do you think hepatitis B can cause liver cancer?b | Yes | 53.8 |
| Do you think someone can die from hepatitis B?b | Yes | 72.4 |
| Do you think hepatitis B disease can be cured?c | No | 14.7 |
HBV versus AIDS, both equally, or not sure.
Yes versus no or not sure.
No versus yes or not sure.
Data Analysis
We computed a knowledge summary score for the 12 questions addressing disease transmission and the sequelae of infection. These scores consisted of the total number of correct answers; therefore, the maximum possible score was 12. Bivariate associations were examined using either a Student’s t-test or chi-square test (or a Fisher’s exact test, when necessary).26
RESULTS
Study Group Characteristics
The mean age of the study group was 49 years. On average, the survey participants had only three years formal education, had lived in the US for 15 years, and were 34 years old at the time of immigration. Just under one-half (46 percent) were currently married. Ninety percent thought liver disease should be treated with Western medicine and 8 percent reported they had family members chronically infected with HBV (Table 1).
TABLE 1.
Characteristics of Study Group (n = 320)
| Age (years): mean (SD) | 49.2 (13.5) |
| Education (years): mean (SD) | 2.5 (3.2) |
| Years in US: mean (SD) | 15.0 (3.8) |
| Age at immigration (years): mean (SD) | 34.2 (13.4) |
| Marital status: percent | |
| Currently married | 45.7 |
| Previously married | 38.2 |
| Never married | 16.1 |
| Type of medicine that should be used to treat liver disease: percent | |
| Western | 89.7 |
| Traditional Cambodian or both | 10.3 |
| Family member(s) infected with hepatitis B: percent | |
| Yes | 7.8 |
| No | 92.2 |
Hepatitis B Knowledge
Prior to being provided with a description of the disease, only 56 percent of the respondents reported they had ever heard of HBV infection. Table 2 summarizes responses to the questions addressing transmission and sequelae. Less than one-quarter (23 percent) of the study group knew that asymptomatic individuals can transmit the disease to others, and only 2 percent knew that HBV is more easily spread than the AIDS virus. Proportions of correct responses to other items addressing methods of transmission ranged from 11 percent to 69 percent. The majority of our survey participants knew that HBV infection can cause liver cancer (54 percent) and death (72 percent). However, only a minority knew that infection can be lifelong (24 percent) and incurable (15 percent). The average summary knowledge score was 4.8 (standard deviation: 2.6).
Serologic Testing
One hundred and twenty three (38 percent) of the women knew they had been serologically tested for hepatitis B. Of these 123 respondents, 96 (78 percent) reported they had no evidence of HBV infection (i.e., were susceptible to the disease), nine (7 percent) were chronic carriers, and 12 (10 percent) indicated they were immune (i.e., had previously been infected with HBV but were not carriers). The remaining women did not know the results of their blood test. Finally, only one-third (33 percent) of the women who indicated they were susceptible to disease had received the HBV vaccine (Figure 1).
FIGURE 1.
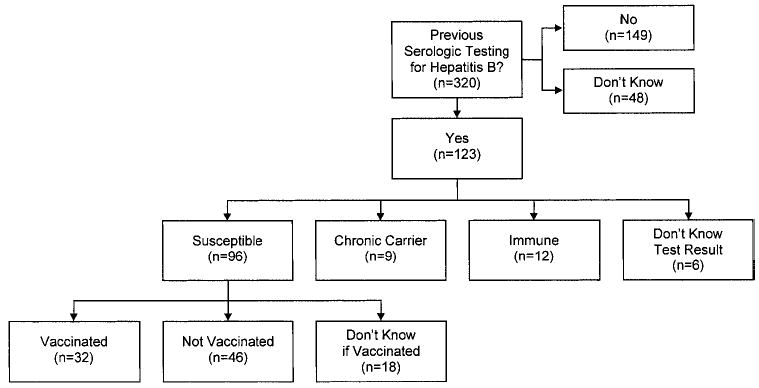
Summary of hepatitis B testing and vaccination.
Bivariate Comparisons
Four variables were associated with having heard of HBV (before the disease was described in terms of symptoms): younger age, higher educational level, younger age at immigration, and having family members who were chronic carriers (Table 3). Table 4 summarizes the bivariate results for the knowledge summary score. The following were associated with higher levels of knowledge: more years of education, preferring Western medicine for the treatment of liver disease, and having family members chronically infected with HBV. As shown in Table 5, only two variables were associated with serologic testing for HBV: higher educational level and having chronically infected family members.
TABLE 3.
Bivariate Results for Heard of Hepatitis B
| Variable | Heard of Hepatitis B (n = 178) | Not Heard of Hepatitis Ba(n = 142) | p-value |
|---|---|---|---|
| Age (years): mean (SD) | 46.9 (13.7) | 52.1 (12.8) | <0.001 |
| Education (years): mean (SD) | 2.9 (3.5) | 2.1 (2.8) | 0.03 |
| Years in US: mean (SD) | 14.8 (3.7) | 15.2 (3.9) | 0.36 |
| Age at immigration (years): mean (SD) | 32.0 (13.2) | 37.0 (13.1) | <0.001 |
| Marital status: percent | |||
| Currently married | 43.2 | 48.9 | 0.32 |
| Previously married | 38.0 | 38.3 | |
| Never married | 18.8 | 12.8 | |
| Type of medicine that should be used to treat liver disease: percent | |||
| Western | 90.8 | 88.2 | 0.46 |
| Traditional Cambodian or both | 9.2 | 11.8 | |
| Family member(s) infected with hepatitis B: percent | |||
| Yes | 12.9 | 1.4 | <0.001 |
| No | 87.1 | 98.6 | |
Includes women who were not sure.
TABLE 4.
Bivariate Results for Knowledge Score (n = 320)
| Variable | Knowledge Score Mean (SD)a | p-value |
|---|---|---|
| Age (years) | ||
| <40 | 4.7 (2.4) | 0.24 |
| 40–59 | 5.0 (2.7) | |
| 60+ | 4.3 (2.6) | |
| Education (years) | ||
| Any | 5.1 (2.5) | 0.01 |
| None | 4.4 (2.7) | |
| Years in US | ||
| <10 | 5.1 (2.5) | 0.39 |
| 10+ | 4.7 (2.6) | |
| Age at immigration (years) | ||
| <40 | 4.9 (2.6) | 0.32 |
| 40+ | 4.5 (2.6) | |
| Marital status | ||
| Currently married | 5.0 (2.6) | 0.23 |
| Previously married | 4.4 (2.6) | |
| Never married | 4.9 (2.6) | |
| Type of medicine that should be used to treat liver disease | ||
| Western | 4.9 (2.6) | 0.04 |
| Traditional Cambodian or both | 3.9 (2.7) | |
| Family member(s) infected with hepatitis B | ||
| Yes | 6.0 (2.0) | 0.01 |
| No | 4.6 (2.6) | |
Number of correct responses ranges from 0 to 12.
TABLE 5.
Bivariate Results for Serologic Testing
| Variable | Serologic Testing (n = 123) | No Serologic Testinga(n = 197) | p-value |
|---|---|---|---|
| Age (years): mean (SD) | 47.5 (13.3) | 50.3 (13.6) | 0.07 |
| Education (years): mean (SD) | 3.2 (4.0) | 2.1 (2.5) | 0.002 |
| Years in US: mean (SD) | 14.8 (3.4) | 15.1 (4.0) | 0.55 |
| Age at immigration (years): mean (SD) | 32.7 (13.5) | 35.1 (13.2) | 0.11 |
| Marital status: percent | |||
| Currently married | 43.8 | 46.9 | 0.71 |
| Previously married | 38.0 | 38.3 | |
| Never married | 18.2 | 14.8 | |
| Type of medicine that should be used to treat liver disease: percent | |||
| Western | 87.4 | 91.1 | 0.30 |
| Traditional Cambodian or both | 12.6 | 8.9 | |
| Family member(s) infected with hepatitis B: percent | |||
| Yes | 16.3 | 2.5 | <0.001 |
| No | 83.7 | 97.5 | |
Includes women who were not sure.
DISCUSSION
Our results document low levels of knowledge about HBV infection among Cambodian women living in Seattle, Washington. Specifically, we found that nearly one-half of the survey respondents were not familiar with “the disease or virus called hepatitis B” until it was explained to them in terms of “a liver problem that makes the skin and eyes go yellow.” In a previous ethnographic study, Cambodian refugees could describe the symptom complexes associated with acute and chronic hepatitis, but were not familiar with biomedical terminology.16 Further, the majority of our respondents did not know that asymptomatic individuals can spread HBV or that sexual intercourse with an infected person can result in hepatitis B. Finally, less than one-quarter thought hepatitis B infection can be lifelong or that HBV disease can be incurable.
We have previously reported our findings from a telephone survey of 75 Vietnamese men and women in Seattle. This study focused on HBV knowledge and did not address serologic testing and vaccination. Levels of knowledge among the Vietnamese sample, while low, were somewhat higher than among this Cambodian study group. For example, 67 percent of the Vietnamese respondents had heard of HBV, 27 percent knew hepatitis B is more easily spread than AIDS, and 58 percent knew asymptomatic individuals can spread HBV.27 McPhee et al. found that 52 percent of Vietnamese in northern California and 56 percent of Vietnamese who responded to a survey conducted in Houston, Dallas, and Washington DC had ever heard of hepatitis B.28
Vaccines that are effective in preventing hepatitis B infection and its chronic carrier state have been available since 1982.21,29,30 The US Preventive Services Task Force has proposed a comprehensive strategy for interrupting the transmission of HBV through vaccine use. This group’s recommendations include screening pregnant women for evidence of chronic HBV infection (to identify infants needing specific immunoprophylaxis), routine immunization of infants, and HBV vaccine for adolescents and young adults not previously immunized. The recommendations also specify that adults from high risk groups (e.g., immigrants from areas of high HBV endemicity) should be serologically tested for hepatitis B and then immunized, if susceptible to infection.29 However, recent studies indicate that the majority of Asian American children in the 5–18 age-group have not received the HBV immunization series.17,28 We found that only 38 percent of the Cambodian women in our study reportedly had been serologically tested for HBV, and the majority of susceptible women had not been vaccinated.
A strength of the reported study is that we used a community-based sample. However, there are several limitations that should be recognized. First, it is unclear to what extent our findings would be generalizable to other geographic regions or Cambodians who do not live in neighborhoods with a high proportion of Southeast Asians. Second, it is possible that women who chose not to participate in our study may have had different HBV knowledge and practices than our respondents. Last, self-reports of hepatitis B serologic testing and vaccination may be inaccurate due to faulty recall.
There is a clear need for effective interventions to reduce HBV-related liver disease and cancer mortality in Southeast Asian communities. McPhee and his colleagues recently developed, implemented, and evaluated a multifaceted HBV intervention program targeting one Vietnamese community in northern California. This program included a media-based, community outreach campaign combined with a physician office intervention. Following a one-year intervention, the percentage of adults who had heard of hepatitis B increased from 52 percent to 85 percent (p < 0.001) and the percentage who had received serologic testing increased from 24 percent to 48 percent (p < 0.001). Additionally, the childhood hepatitis B immunization rates increased from 41 percent to 61 percent (p < 0.05) as a result of the intervention.28 Future research should examine alternative methods for delivering contextually and linguistically appropriate health education messages about HBV infection to Cambodian populations in the US. Our findings suggest that such efforts might usefully focus on modes of HBV transmission as well as the importance of serologic testing and vaccination, particularly among the least educated.
Footnotes
Supported by grant #CA70922 and cooperative agreement #CA86322 from the National Cancer Institute.
References
- 1.US Department of Commerce. We the Asian Americans. Washington DC: US Department of Commerce; 1993. [Google Scholar]
- 2.Rumbaut RG, Weeks JR. Fertility and adaptation: Indochinese refugees in the United States. Int Migrat Rev. 1986;20:428–465. [PubMed] [Google Scholar]
- 3.Kulig JC. Sexuality beliefs among Cambodians: implications for health professionals. Health Care Women Int. 1994;15:69–76. doi: 10.1080/07399339409516096. [DOI] [PubMed] [Google Scholar]
- 4.Kiernan B. Genocide and Democracy in Cambodia: the Khmer Rouge, the United States, and the International Community. New Haven: Yale University Press; 1993. [Google Scholar]
- 5.Muecke MA. Caring for Southeast Asian refugee patients in the USA. Am J Public Health. 1983;73:544–548. doi: 10.2105/ajph.73.4.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uba L. Cultural barriers to health care for Southeast Asian refugees. Public Health Rep. 1992;107:544–546. [PMC free article] [PubMed] [Google Scholar]
- 7.Di Bisceglie AM, Rustgi VK, Hoofnagle TH, Dusheiko GM, Lotze ML. NIH conference: hepatocellular carcinoma. Ann Intern Med. 1988;108:390–401. doi: 10.7326/0003-4819-108-3-390. [DOI] [PubMed] [Google Scholar]
- 8.London WT, McGlynn KA. Liver cancer. In: Scottenfeld D, Fraumeni JF, editors. Cancer Epidemiology and Prevention. New York: Oxford University Press; 1996. pp. 772–793. [Google Scholar]
- 9.Perkins CL, Morris JR, Wright WE, Young JL. Sacramento: California Department of Health Services; 1995. Cancer Incidence and Mortality in California by Detailed Race/ethnicity, 1988–92. [Google Scholar]
- 10.Miller BA. Bethesda: National Cancer Institute; 1996. Racial/ethnic Patterns of Cancer in the United States, 1988–1992. [Google Scholar]
- 11.Johnson PJ. The epidemiology of hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 1996;8:845–849. [PubMed] [Google Scholar]
- 12.Centers for Disease Control. Screening for hepatitis B virus infection among refugees arriving in the United States, 1979–1991. MMWR. 1991;45:784–787. [PubMed] [Google Scholar]
- 13.Conjeevaram HS, Di Bisceglie AM. Management of chronic viral hepatitis in children. J Pediatr Gastroenterol Nutr. 1995;20:365–375. doi: 10.1097/00005176-199505000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Margolis HS. Prevention of acute and chronic liver disease through immunization: hepatitis B and beyond. J Infect Dis. 1993;168:9–14. doi: 10.1093/infdis/168.1.9. [DOI] [PubMed] [Google Scholar]
- 15.Haan HWL, Hepatitis B. In: Confronting Critical Health Issues of Asian and Pacific Islander Americans. Zane NWS, Takeuchi DT, Young KNJ, editors. Thousand Oaks: Sage Publications; 1994. pp. 148–173. [Google Scholar]
- 16.Jackson JC, Rhodes LA, Inui TS, Buchwald D. Explaining hepatitis B to Cambodian refugees: incorporating patient experience into medical translation. J Gen Intern Med. 1997;12:292–298. doi: 10.1046/j.1525-1497.1997.012005292.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Euler GL. Asian and Pacific Islander child hepatitis B vaccination catch-up: why now is the best time. Asian Am Pacific Isl J Health. 1997;5:40–45. [PubMed] [Google Scholar]
- 18.Gjerdingen DK, Lor V. Hepatitis B status of Hmong patients. JABFP. 1997;10:322–328. [PubMed] [Google Scholar]
- 19.Franks AL, Berg CJ, Kane MA, et al. Hepatitis B infection among children born in the United States to Southeast Asian refugees. N Engl J Med. 1989;321:1301–1305. doi: 10.1056/NEJM198911093211905. [DOI] [PubMed] [Google Scholar]
- 20.Alter MJ, Hadler SC, Margolis HS, et al. The changing epidemiology of hepatitis B in the United States. JAMA. 1990;263:1218–1222. [PubMed] [Google Scholar]
- 21.US Department of Health and Human Services. Clinician’s Handbook of Preventive Services. Washington DC: US Department of Health and Human Services; 1994. [Google Scholar]
- 22.Hubbell FA, Chavez LR, Mishra SI, Magona JR, Valdez RB. From ethnography to intervention: developing a breast cancer control program for Latinas. Monogr Natl Cancer Inst. 1995;18:109–115. [PubMed] [Google Scholar]
- 23.Taylor VM, Schwartz SM, Jackson JC, et al. Cervical cancer screening among Cambodian-American women. Cancer Epidemiol Biomarkers Prev. 1999;8:541–546. [PubMed] [Google Scholar]
- 24.Department of Commerce. 1990 Census of Population and Housing: Population and Housing Characteristics for Census Tracts and Block Numbering Areas: Seattle, WA PMSA. Washington DC: United States Department of Commerce; 1993. [Google Scholar]
- 25.Eyton J, Neuwirth G. Cross-cultural validity: ethnocentrism in health studies with special reference to the Vietnamese. Soc Sci Med. 1984;18:447–453. doi: 10.1016/0277-9536(84)90061-3. [DOI] [PubMed] [Google Scholar]
- 26.Rosner B. Fundamentals of Biostatistics. Boston: Duxbury; 1986. [Google Scholar]
- 27.Taylor VM, Jackson JC, Pineda M, Pham P, Fischer M, Yasui Y. Hepatitis B knowledge among Vietnamese immigrants: implications for prevention of hepatocellular carcinoma. J Cancer Educ. 2000;15:51–55. doi: 10.1080/08858190009528654. [DOI] [PubMed] [Google Scholar]
- 28.McPhee SJ, Nguyen TT. Cancer, cancer risk factors, and community-based cancer control trials in Vietnamese Americans. Asian Am Pac Isl J Health. 2000;8:19–31. [PMC free article] [PubMed] [Google Scholar]
- 29.US Preventive Services Task Force. Guide to Clinical Preventive Services. Baltimore: Williams and Wilkins; 1996. [Google Scholar]
- 30.Hill LL, Hovell M, Berenson AS. Prevention of hepatitis B transmission in Indo-Chinese refugees with active and passive immunization. Am J Prev Med. 1991;7:29–32. [PubMed] [Google Scholar]


