Abstract
Objective
Chronic infection with the hepatitis B virus is endemic in Southeast Asian populations, including Vietnamese. Previous research has documented low rates of hepatitis B vaccine coverage among Vietnamese-American children and adolescents ages 3 to 18. To address this problem, we designed and tested in a controlled trial 2 public health outreach “catch-up” campaigns for this population.
Design
In the Houston, Texas metropolitan area, we mounted a media-led information and education campaign, and in the Dallas metropolitan area, we organized a community mobilization strategy. We evaluated the success of these interventions in a controlled trial, using the Washington, DC metropolitan area as a control site. To do so, we conducted computer-assisted telephone interviews with random samples of ~500 Vietnamese-American households in each of the 3 study sites both before and after the interventions. We assessed respondents’ awareness and knowledge of hepatitis B and asked for hepatitis B vaccination dates for a randomly selected child in each household. When possible, we validated vaccination dates through direct contact with each child’s providers.
Results
Awareness of hepatitis B increased significantly between the pre- and postintervention surveys in all 3 areas, and the increase in the media education area (+21.5 percentage points) was significantly larger than in the control area (+9.0 percentage points). At postintervention, significantly more parents knew that free vaccines were available for children in the media education (+31.9 percentage points) and community mobilization (+16.7 percentage points) areas than in the control area (+4.7 percentage points). An increase in knowledge of sexual transmission of hepatitis B virus was significant in the media education area (+14.0 percentage points) and community mobilization (+13.6 percentage points) areas compared with the control area (+5.2 percentage points). Parent- or provider-reported data (n = 783 for pre- and n = 784 for postintervention surveys) suggest that receipt of 3 hepatitis B vaccinations increased significantly in the community mobilization area (from 26.6% at pre- to 38.8% at postintervention) and in the media intervention area (28.5% at pre- and 39.4% at postintervention), but declined slightly in the control community (37.8% at pre- and 33.5% at postintervention). Multiple logistic regression analyses estimated that the odds of receiving 3 hepatitis B vaccine doses were significantly greater for both community mobilization (odds ratio 2.15, 95% confidence interval 1.16–3.97) and media campaign (odds ratio 3.02, 95% confidence interval 1.62–5.64) interventions compared with the control area. The odds of being vaccinated were significantly greater for children who had had at least 1 diphtheria-tetanuspertussis shot, and whose parents were married, knew someone with liver disease, had heard of hepatitis B, and had greater knowledge about hepatitis B. The odds of being vaccinated were significantly lower for older children.
Conclusions
Both community mobilization and media campaigns significantly increased the knowledge of Vietnamese-American parents about hepatitis B vaccination, and the receipt of “catch-up” vaccinations among their children.
Keywords: hepatitis B vaccination, catch-up, Vietnamese-Americans
ABBREVIATIONS: HBV, hepatitis B virus; HepB, hepatitis B vaccine; CDC, Centers for Disease Control and Prevention; DTP, diphtheria, tetanus toxoid and pertussis; VFC, Vaccines for Children; EDCC, East Dallas Counseling Center; OR, odds ratio; CI, confidence interval
Persons with chronic hepatitis B virus (HBV) infection are at increased risk of chronic hepatitis, cirrhosis, and liver cancer.1 Epidemiologic studies have shown that the risk of liver cancer among persons with chronic HBV infection is over 200 times greater than for those not infected.2 It is estimated that 25% of those who become chronically infected as infants or young children and 15% of those who become chronically infected as adolescents or adults die prematurely from chronic liver disease.3
Although HBV infection is relatively uncommon in the United States, the disease is endemic in Southeast Asian populations, including Vietnamese. Studies have documented rates of hepatitis B surface antigen positivity ranging from 7% to 14% among Vietnamese adults in the United States.4–7 The high rates of chronic HBV infection among Vietnamese account in large part for their disproportionately high incidence rates of liver cancer. In the United States, Vietnamese-American males have the highest liver cancer incidence rate of any ethnic group (41.8 per 100 000), a rate that is 11 times higher than that among white males (3.7 per 100 000).8
HBV infection and its sequelae can be prevented among individuals who have not been previously infected by administering 3 doses of the hepatitis B vaccine (HepB). Since 1997, the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention (CDC) has recommended universal vaccination of all children ages 0 to 18.9 Currently, 42 states require vaccination of children entering elementary school and 31 states require vaccination of children entering middle school.10 Significant progress has been made in the vaccination of infants. Data from the National Immunization Survey indicate that, in 1996, 84% of all children and 88% of Asian/Pacific Islander children ages 19 to 35 months had received all 3 doses of the HepB.11–12 However, many older children remain unvaccinated and at risk of infection. For example, we have previously documented low rates of hepatitis B vaccinations among Vietnamese-American children ages 3 to 18.13–14 Conducting “catch-up” hepatitis B vaccination programs among older age cohorts, as recommended by the Advisory Committee on Immunization Practices in 1997, could prevent unnecessary infection.
The goal of this project was to improve Vietnamese-American parents’ awareness and knowledge about hepatitis B and their children’s receipt of the series of 3 HepBs. To promote these goals, we tested the effect of 2 public health outreach interventions in 2 different areas of Texas.
METHODS
Intervention Methods
In the metropolitan area of Houston (Harris and Fort Bend Counties), Texas, we mounted a media-led information and education campaign, and in the metropolitan area of Dallas (Dallas and Tarrant Counties), Texas, we organized a community mobilization strategy. All interventions were conducted in the Vietnamese language. We evaluated the success of these interventions in a controlled trial, using as a control site the Washington, DC area (the District of Columbia; Fairfax County and the City of Arlington, Virginia; and Prince Georges County and Montgomery County, Maryland). We selected these 3 areas because they had large Vietnamese-American populations that had not received interventions for hepatitis B vaccination. In the 1990 Census, the Vietnamese-American population of the Houston metropolitan area was 36 348; by the 2000 Census, it had grown to 58 623. In the 1990 Census, the Vietnamese-American population of the Dallas metropolitan area was 18 509; by the 2000 Census, it had grown to 41 591. Finally, in the 1990 Census, the Vietnamese-American population of the Washington, DC metropolitan area was 20 376; by the 2000 Census, it had grown to 38 796.15–16
Media Education Campaign Strategy
We conducted a media-based education and outreach campaign to encourage Vietnamese-American parents to get their children ages 3 to 18 vaccinated with the HepB. The campaign occurred over a 2-year period (from April 1998 through March 2000) in the Houston area. The intervention activities included Vietnamese-language print, electronic (mass), and outdoor media education, emphasizing the need for hepatitis B catch-up vaccinations. The print media included educational booklets about hepatitis B, calendars with incorporated hepatitis B messages, print advertisements, and news articles published in local Vietnamese newspapers; electronic media included radio advertisements, interviews with community health leaders, and telephone “warm-line”. Outdoor media included billboards.
The hepatitis B educational booklet is a 26-page, 4-color booklet entitled, Bao Ve The He Moi: Hay Chich Ngua (“Immunize Against Hepatitis B to Project Future Generations”). The booklet was originally developed in the Vietnamese language, reviewed for readability, acceptability, and medical accuracy by a panel of Vietnamese-American physicians, focus groups of consumers, and the project’s Community Advisory Board. It was then revised and translated into English for review by a non-Vietnamese-speaking project staff. A total of 7000 copies were printed and distributed at various supermarkets and Vietnamese “villages” (housing complexes) in the Houston area. In addition, 8000 copies of the project’s signature calendar bearing hepatitis B vaccination reminder messages for the years 1999 and 2000 were distributed at various venues, such as supermarkets, grocery stores, physicians’ offices, community clinics, pagodas, temples, churches, and health fairs, including the annual Vietnamese Lunar New Year (Tet) Festival.
Eight print ads were developed and printed; each ad carried educational messages regarding hepatitis B and vaccination, along with an exhortation to catch up on these vaccinations. All ads contained the telephone number and address of Research and Development Institute, the project’s Houston subcontractor, for area residents to contact for further information. The 8 ads were printed in 5 major Vietnamese newspapers with an estimated total of 261 issues, resulting in an estimate of 1.305 million print media consumer exposures (~5000 copies × 261 issues). Additionally, 2 3-ad series were developed and printed during the first 6 months in 10 newspaper issues. We wrote a total of 6 hepatitis B-related articles, which were published in the same newspapers. The articles discussed hepatitis B epidemiology in the Vietnamese-American population, its modes of transmission, and its prevention by vaccination, including the importance of catch-up vaccinations for older children. The articles also reported where free vaccinations could be obtained through the CDC’s Vaccines for Children (VFC) Program.
Mass media included development of 8 30- to 60-second radio spots that were aired an estimated 3663 times on 2 Vietnamese radio stations. The project also jointly established a “warm-line,” staffed by the Vietnamese-American Community Health Network at Research and Development Institute, where Vietnamese-American residents could telephone with questions about hepatitis B, immunizations, and other health matters. Callers were asked to leave their questions on an answering machine, and later volunteers from Vietnamese-American Community Health Network returned the calls with answers to the questions.
A billboard, designed by a local Vietnamese advertising firm, bore a culturally appropriate design of children reaching up for their hepatitis B shots. It carried a message encouraging parents of children 3 to 18 years old to get them vaccinated. The billboard was strategically posted at various locations during the course of the campaign in proximity to sites with high concentration of Vietnamese commercial activity or residence. A press release was issued and printed in Vietnamese press, marking the posting of the first billboard. The billboard campaign involved a total of 41 billboard months. Two radio ads were developed to disseminate the news regarding the billboard’s existence and the posting locations. The advertising firm also designed print ads based on the billboard’s design.
Community Mobilization Strategy
To improve hepatitis B awareness and knowledge among Vietnamese-American parents and vaccination rates among their children in Dallas/Fort Worth, a community mobilization strategy was undertaken by the East Dallas Counseling Center (EDCC), a Vietnamese-American community-based organization, under a subcontract. EDCC convened a coalition in the Dallas/Fort Worth Metroplex to develop an action plan of activities and timeline with the goal of improving vaccination rates. The Coalition then implemented that plan over the course of the next 3 years (from April 1998 to March 2000).
The 19-member coalition consisted of physicians, dentists, pharmacists, city and county department of public health and education officials, business leaders, veterans, seniors, teachers, researchers, parents, grandparents, homemakers, newspaper editors, and community-based organization representatives. The coalition was formed on June 7, 1998. Coalition members met quarterly to conduct “grass-roots,” person-to-person community organizing activities to promote program goals and objectives.
The coalition members decided on its mission, goals, objectives, and structure. The mission of the coalition was to improve the health status of Vietnamese-American children in Dallas/Fort Worth by promoting the awareness of and responsibility for hepatitis B vaccinations of Vietnamese-American children through families, health care providers, and community organizations. The goals of the coalition were to improve catch-up hepatitis B vaccinations among Vietnamese-American children ages 3 to 18 in Dallas/Fort Worth and surrounding communities. Specific objectives of the coalition were to identify community channels that could be mobilized to promote hepatitis B vaccinations, to develop an action plan of activities and a timeline, and to work through community channels to implement the plan.
The coalition worked through 3 committees: an advisory committee to advise and introduce the project and staff to the community and make sure the health education was appropriate and culturally sensitive; a planning committee to plan and monitor the activities of the project in 2 year-long periods and to ensure that all the activities were conducted within the timeline; and an outreach committee to identify, conduct, and evaluate outreach activities.
A bilingual, bicultural Vietnamese-American project coordinator was hired by EDCC to coordinate this campaign. Intervention activities included efforts to promote physicians’ registration as VFC providers, distribution of referral lists of VFC providers, distribution of health education brochures, conduct of health fairs, targeted mailings, educational presentations, and use of free local media. Staff worked with the VFC coordinator to recruit 6 new Vietnamese-American health care providers. A total of 5300 brochures and pamphlets about hepatitis B in Vietnamese and English, and referral lists were distributed to people at health fairs, community-based organizations, markets, and shopping centers. Coalition members helped in the organizing of 13 health fairs for Vietnamese-Americans in various settings, ranging from shopping centers in Dallas and Arlington, Texas, to community centers, churches, pagodas, Lunar New Year (Tet) events, Mid-Autumn Festivals, and Christmas events. The coalition and staff made a total of 8 oral presentations at the health fairs and at various Vietnamese community-based organizations. In addition, every Sunday staff made presentations to volunteers and children at Vietnamese language schools in Buddhist temples and churches. Staff also conducted home visits to newly immigrated Vietnamese refugees in the area and worked weekly at 2 community clinics to translate and help children receive vaccinations. Staff collected incentives (toys, T-shirts, etc) from charitable agencies, companies, and local businesses to offer “prizes” to children receiving vaccinations. Eight news articles and 8 announcements were printed in 3 Vietnamese-language newspapers. The Coalition chair and staff were interviewed on Vietnamese Public Radio and Vietnamese Broadcasting Network Radio twice. Eight announcements were broadcast 3 times daily for 4 days before health fairs and community events.
Evaluation Methods: Parent Surveys
The survey methods used in this trial have been described in detail elsewhere.12 Briefly, before and after the interventions, we conducted independent computer-assisted telephone interviews of Vietnamese-American adults in the intervention and control sites, using telephone numbers of individuals with Vietnamese surnames randomly selected from area telephone books.17 A potential survey respondent was considered eligible if she or he was at least 18 years old, self-identified as being Vietnamese or Chinese-Vietnamese, was a parent of at least 1 child ages 3 to 18 living in the household, and was the adult in the household most familiar with the child(ren)’s vaccination records. Children ages 3 to 18 were ranked by age, then 1 child was randomly selected by birth order and parents were asked questions about that child’s vaccination status. We made up to 5 attempts to reach each potential survey respondent. Respondents were offered the choice of answering questions in Vietnamese or English. At postintervention, to guarantee potential exposure to the intervention, we surveyed only those who had lived in the experimental or comparison communities for ≥ 2 years.
Survey items included respondents’ age, marital status, year of immigration to the United States, highest level of education, English language proficiency, health insurance status, employment status, and poverty status. Poverty status was determined based on household size, using criteria established by the US Department of Health and Human Services.18 We asked respondents about the age and sex of the selected child, and asked them to find the child’s vaccination record. For those who were able to find it, we asked them to read the dates of any doses of HepB and the dates of the first 3 doses of diphtheria, tetanus toxoid, and pertussis (DTP) vaccine (a marker of access to care). To assess their level of awareness and knowledge about hepatitis B, we asked respondents if they had ever heard of liver disease or HBV infection, whether they knew about possible routes of transmission, and whether or not they knew if free hepatitis B vaccinations were available to low income families or those without health insurance. To create a more comprehensive measure of awareness and knowledge, we generated a knowledge index composed of 7 variables, such as modes of transmission and causal relationship with liver cancer. We assigned each of these variables equal weight, and calculated an index score for each respondent. Respondents were asked about the ethnicity of their physician.
In calculating required sample sizes for the surveys, we used 25% to 35% as the expected preintervention vaccination rate for Vietnamese-American children. The calculations were based on conservative estimates of effect size (h = 10%), with α = 0.05 and β = 0.80. It was determined that a sample size of 376 parents would allow us to detect at least a 10 percentage point difference between groups in the proportion of children who had ever received 3 doses of HepB in each community. Therefore, we set a goal of interviewing at least 500 eligible parents in each area (control and both intervention areas).
Evaluation Methods: Provider Reports
Because many survey respondents could not find vaccination records and because we wished to validate vaccination information by directly contacting providers, we asked permission to record the parent’s name, the child’s name and birthdate, and the names and contact information of up to 3 providers who might have vaccinated the child. We obtained oral consent to contact the child’s providers. The provider validation protocol is described in detail elsewhere.12 Briefly, provider names, addresses, and telephone numbers were located or verified and entered into a database management software program. Then, we generated personalized letters to providers on CDC letterhead, enclosing a computer-generated form with child’s name, date of birth, parent’s name, provider’s name, and space to record the dates of each of the child’s doses of hepatitis B and DTP vaccines. We recontacted nonresponders by telephone or in person, and faxed or hand-delivered duplicate copies of the form. This reminder process was repeated as necessary for a 5-month period from October 2000 to March 2001. When parents said the child had no provider, could not recall the child’s provider, or refused to give consent to contact the provider, we sent similar letters to county health departments. Vaccination dates from the forms returned by providers were matched to those obtained by the parent surveys. When there was disagreement regarding dates, the provider dates were used.
The Committee on Human Research at the University of California, San Francisco, approved the research protocol.
Data Analysis
The major outcomes were the proportion of parents responding correctly to various knowledge questions and the proportion of children who had received 3 doses of HepB. The analyses focused on describing differences between the 2 intervention areas and the control area at pre- and postintervention in sociodemographic characteristics, awareness and knowledge, and vaccination rates. In calculating raw changes in vaccination coverage in the 3 sites, we first used an age standardization procedure to equalize the 3 samples. A standardized age distribution was created based on the entire sample of children by age across all 3 sites. To compare the same birth cohorts, we included only those children ages 3 to 16 at the preintervention survey in 1998 and those children ages 5 to 18 years at the postintervention survey in 2000. We considered those children for whom a parent could provide at least 1 DTP or HepB vaccination date as having had a shot record. These cases were used to calculate the denominators for estimations of the HepB vaccination rates. Statistical tests included t tests of differences in means and χ2 tests of differences in proportions. P values of < .05 were considered significant.
We then conducted multiple logistic regression analyses to assess the impact of the interventions at postintervention and to identify other variables that were significantly associated with vaccine receipt. We conducted primary and secondary analyses of vaccination status using 2 different samples. For both analyses, the samples were constructed by pooling data from the pre- and postintervention surveys and including children for whom we had dates of 3 vaccinations received (HepB × 3) reported from the parents (using children’s shot records) and/or the providers (using medical records). The regression model generated outcome odds ratios (ORs) that we used to calculate relative ORs to measure the controlled effect of the interventions. A relative OR is a ratio of 2 ORs. In this analysis, the numerator was the odds that a child in the intervention area received HepB × 3 at postintervention compared with the odds in the same area at preintervention. The denominator of the relative OR is the odds that a child in the control area received HepB × 3 at postintervention compared with the odds at preintervention.
For the primary regression analysis, we included only those cases for which we had data from a vaccination record in the sample (n = 1567). There were 1488 children for whom we had survey data but could not obtain information about vaccinations from parent handheld records or provider records. For the primary analysis, we classified these cases as undetermined and excluded them from the sample. Recognizing that this sampling criterion affected the sensitivity of the outcome measure, we conducted a secondary analysis using a different sampling criterion. The secondary analysis was conducted under the assumption that the likelihood was low that a child had received hepatitis B vaccination if neither their parents nor their provider could provide us with vaccination record data. We reclassified the cases for which we did not have data on vaccinations as having not been vaccinated with HepB or DTP, and included them in the sample (n = 3055).
The regression models controlled simultaneously for preintervention levels of vaccination and for differences in sociodemographic factors that might account for outcome differences between the 3 sites. The terms entered into the models were selected based on our theoretical assumptions and previous experience12 regarding sociodemographic variables and other factors that might influence each of the dependent variables. In the logistic regression models, we included dummy variables to control for any unmeasured characteristics of the study locations and secular trends:
Site (Houston or Dallas): each case was coded for city of residence; code assignments for Houston and Dallas residents were “1” on the corresponding city variable, and “0” on the other; Washington, DC residents were coded “0” on both variables.
Time (postintervention): each case was coded for the time of the survey (0 = surveyed at preintervention, 1 = surveyed at postintervention).
The effects of each intervention were measured using interaction terms that resulted from multiplying site (Houston or Dallas) by time (postintervention). Specifically, the measure for the effect of the media education campaign was the interaction term Houston × postintervention. For cases surveyed at postintervention in Houston, Houston × postintervention = 1 × 1, while all other cases = 0. The measure of the effect of the community mobilization strategy was Dallas × postintervention. For cases surveyed at postintervention in Dallas, Dallas × postintervention = 1 × 1, while all other cases = 0. The Houston × postintervention and Dallas × postintervention interaction terms compare change in the vaccination rate in each intervention site to change in the control site (eg, OR post:pre in Houston divided by OR post:pre in the control site).
Initially, we ran full models entering the following variables based on parents’ data: self-reported English-language ability, marital status, employment status, educational attainment, income, insurance status, years since immigration, recognition of hepatitis B, knowledge of anyone with liver disease, and knowledge of free vaccine availability. We also entered child’s age and sex, and prior receipt of at least 1 DTP vaccination (≥ 1 DTP), as well as health care provider’s ethnicity. Then, to develop a parsimonious model, we used a backwards elimination procedure to drop variables that were not significant in the full model. We also used χ2 goodness-of-fit tests and classification tables to assess the adequacy of the models. For each covariate, we computed adjusted ORs with a 95% confidence interval (CI), indicating the increase or decrease in contribution made by each characteristic to the odds of attaining the outcome. To check for whether there were unusually high correlations between independent variables (multicollinearity), we computed bivariate Pearson correlations (r) for continuous variables and contingency coefficients for categorical variables. No high correlations were found. Analyses were performed using the Logistic procedure in the SAS 8.0 statistical package (SAS Institute, Inc, Cary, NC).19
RESULTS
At preintervention, 1624 parents were surveyed in the intervention and control areas, and 1508 (93%) responded.12 At postintervention, call attempts were made to 12 937 potential survey respondents. Of these, 3411 (26.4%) reached nonworking numbers. An additional 4359 calls (33.7%) reached families who were not eligible for interview for reasons such as not having age-eligible children in the household (28.4%), not being of Vietnamese or Chinese-Vietnamese ethnicity (5.2%), or not having anyone at least 18 years old in the household (0.1%). It was not possible to determine eligibility for 3494 (27%) call attempts because calls reached busy signals (2%), answering machines (6.8%) or unanswered phones (17%), or because those answering the telephone refused interview before eligibility could be ascertained (0.5%). The remaining call attempts reached 1673 eligible respondents, of which 1547 agreed to complete the interview for a postintervention response rate of 92.5%. All but 11 interviews were conducted in the Vietnamese language.
We were able to obtain vaccination reports from providers for 694 of the 1508 children in the preintervention survey.12 At postintervention, parents gave us the names of 1944 providers to contact regarding the vaccination status of 1547 children. Obtaining reports from providers proved to be time-consuming, involving repeated follow-up calls (≥4 attempts for each provider for each child) and re-mailing and/or refaxing the validation forms and accompanying letter. In our attempts to obtain the children’s vaccination status from the providers, we received responses from 1101 providers, resulting in a provider response rate of 56.6%. Of the total 1944 providers, 915 (47.1%) providers (for 838 children) acknowledged that the child identified in the form we had mailed to them was their patient; however, despite being assured that parents had given oral consent, 83 (4.3%) of these providers required written consent from the parents before they would release the child’s vaccination status. In addition, 172 (8.9%) of the 1944 providers denied that the child was their patient or, in the case of county public health departments, said that there was no record for the child in the county system, and 13 (0.7%) stated that the information about the child which we had furnished to them was insufficient to allow them to identify the child accurately. We were unable to obtain information from the remaining 844 (43.4%) providers because parents had provided insufficient contact information or because providers never responded despite multiple telephone, fax, or in-person follow-ups. For example, 1 physician who had 35 of the children as patients never responded to our repeated inquiries. Thus, we were able to obtain vaccination reports from providers for 660 children in the postintervention survey.
Sociodemographic Characteristics of Survey Respondents (Parents)
Sociodemographic characteristics for all respondents to the pre- and postintervention surveys are shown in Table 1. The preintervention sample has been characterized previously.12 In the postintervention sample, 90.9% of the respondents were parents or legal guardians of the child about whom we requested vaccination data. Therefore, we refer to respondents as “parents” (the remainder were grandparents, other relatives, or other household members). The average age of the parents was 42.5 years, ranging from 18 to 79 years. Most parents had immigrated to the United States in the 1980s and 1990s (median year of immigration was 1990), although immigration ranged from 1965–1996. Overall, 31.2% reported limited English-language ability and 20.7% had less than a high school education. One third (33.4%) of respondents reported incomes below the poverty line. Most of the respondents were employed and the vast majority were married. About three quarters (76.4%) had health insurance (private or public) and about half (48%) reported that their child’s provider was Vietnamese-American. Only 21.8% of parents said they could supply vaccination data from a vaccination record, but 67.8% gave oral consent to contact the child’s provider.
TABLE 1.
Sociodemographic Characteristics of Vietnamese-American Parents and Their Children by Site, at Preintervention (1998) and Postintervention (2000), % (95% CIs)
| Variable | Community Mobilization at Preintervention (Dallas; N = 500) | Community Mobilization at Postintervention (Dallas; N = 513) | Media Education Campaign at Preintervention (Houston; N = 523) | Media Education Campaign at Postintervention (Houston; N = 521) | Control at Preintervention (Washington DC; N = 503) | Control at Postintervention (Washington DC; N = 503) |
|---|---|---|---|---|---|---|
| Mean year of immigration | 1987 | 1988 | 1985 | 1986 | 1986 | 1987 |
| Speaks English poorly/not-at-all (%)* | 41.2 (36.9,45.6) | 34.1 (30.0,38.2) | 32.9 (28.9,36.9) | 39.7 (35.5,43.9) | 28.4 (24.5,32.3) | 27.9 (24.0,31.8) |
| Education < 12 y (%)*§ | 48.1 (43.7,52.5) | 24.0 (20.3,27.7) | 34.6 (30.5,38.7) | 17.3 (14.1,20.5) | 33.8 (29.7,37.9) | 20.8 (17.3,24.3) |
| Income was below poverty level (%)‡ | 30.4 (26.3,34.4) | 22.6 (19.0,26.2) | 27.7 (23.9,31.5) | 18.4 (15.1,21.7) | 19.7 (16.2,23.2) | 16.1 (12.9,19.3) |
| Employed (%) | 69.8 (65.8,73.8) | 72.9 (69.1,76.7) | 67.3 (63.3,71.3) | 75.6 (71.9,79.3) | 72.4 (68.5,76.3) | 80.3 (76.8,83.8) |
| Married (%) | 86.0 (83.0,89.0) | 87.8 (85.0,90.6) | 87.1 (84.2,90.0) | 89.1 (86.4,91.8) | 83.3 (80.0,86.6) | 87.5 (84.6,90.4) |
| Mean age (y), respondents | 41.2 (22.1,60.3) | 41.5 (19.8,63.2) | 41.6 (22.9,60.3) | 42.6 (22.5,62.7) | 41.5 (21.7,61.3) | 42.5 (21.9,63.1) |
| Mean age (y), children | 9.8 (1.1,18.0) | 10.6 (1.9,18.0) | 10.1 (1.3,18.0) | 11.0 (1.8,18.0) | 9.6 (1.4, 17.8) | 11.0 (2.3,18.0) |
| Sex of child was female (%) | 50.8 (46.4,55.2) | 54.1 (49.8,58.4) | 48.5 (44.2,52.8) | 51.8 (47.5,56.1) | 49.7 (45.3,54.1) | 52.7 (48.3,57.1) |
| Had health insurance (%)*§ | 65.8 (61.6,70.0) | 75.3 (71.6,79.0) | 63.6 (59.5,67.7) | 70.8 (66.9,74.7) | 76.7 (73.0,80.4) | 80.7 (77.3,84.1) |
| Child’s provider was Vietnamese (%)* | 18.8 (15.4,22.2) | 36.7 (32.5,40.9) | 27.1 (23.3,30.9) | 57.4 (53.2,61.6) | 30.6 (26.6,34.6) | 49.9 (45.5,54.3) |
Comparison among 3 sites at preintervention by χ2 test, P = .001.
Comparison among 3 sites at preintervention by χ2 test, P = .009.
Comparison among 3 sites at postintervention by χ2 test, P = .05.
Several differences between the intervention and control communities and between the pre- and postintervention survey populations are shown in Table 1. At preintervention, fewer parents in the control group spoke English poorly, had less than a 12th grade education, or reported having household incomes below the poverty line, compared with parents in the intervention groups. More parents in the control group had health insurance. In addition, at preintervention more children living in the control area had a Vietnamese-American provider than children in the intervention groups.12 At postintervention, more parents in the community mobilization area had less than a 12th grade education than those in the media campaign or control areas. Fewer parents in the media education area had health insurance than those in the community mobilization and control areas. Differences between parents interviewed in 1998 and 2000, regardless of their region of residence, suggest that Vietnamese-Americans are attaining more education, more employment, and more health insurance coverage.
Parents’ Awareness and Knowledge
The analyses of preintervention data on parents’ awareness of, and knowledge about liver cancer and hepatitis B have been reported previously.12 Changes in parents’ awareness and knowledge at postintervention are compared by site in Table 2. Parents’ awareness of hepatitis B did increase: significantly more parents had heard of hepatitis B at postintervention compared with preintervention in all 3 areas, but only the increase in the media education area (+21.5 percentage points) was significantly larger than in the control area (+9.0 percentage points; P = .001). At postintervention, significantly more parents knew that free vaccines were available for children in the media education (+31.9 percentage points) and community mobilization (+16.7 percentage points) areas than in the control area (+4.7 percentage points; P = .001 for both).
TABLE 2.
Awareness and Knowledge of Vietnamese-American Parents by Site, at Preintervention (1998) and Postintervention (2000), (95% CIs)
| Variable | Community Mobilization at Preintervention (N = 500) | Community Mobilization at Postintervention (N = 523) | χ2 Test of Change Compared to Control (P Value) | Media Education Campaign at Preintervention ( N = 505) | Media Education Campaign at Postintervention (N = 521) | χ2 Test of Change Compared to Control (P Value) | Control at Preintervention (N = 503) | Control at Postintervention (N = 503) |
|---|---|---|---|---|---|---|---|---|
| Awareness | ||||||||
| Knew someone with liver disease | 32.4 (28.3,36.5) | 32.1 (28.1,36.1)
−0.3 |
−7.1 (.09) | 32.5 (28.4,36.6) | 33.8 (29.7,37.9)
+1.3 |
−5.5 (.19) | 30.2 (26.2,34.2) | 37.0 (32.8,41.2)
+6.8** |
| Had heard about HBV infection§ | 46.2 (41.8,50.6) | 52.2 (47.9,56.5)
+6.0* |
−3.0 (.50) | 54.9 (50.6,59.2) | 76.4 (72.8,80.0)
+21.5*** |
12.5 (.00) | 49.9 (45.5,54.3) | 58.9 (54.6,63.2)
+9.0*** |
| Knew that free hepatitis B shots were availableठ| 20.0 (16.5,23.5) | 36.7 (32.5,40.9) +16.7*** | 12.0 (.00) | 25.9 (22.1,29.7) | 57.2 (53.0,61.4) +31.9*** | 26.6 (.00) | 24.1 (20.4,27.8) | 28.8 (24.8,32.8) +4.7 |
| Correct knowledge | ||||||||
| Agreed that one can get hepatitis B from | ||||||||
| Sharing a toothbrush | 48.0 (43.6,52.4) | 65.2 (61.1,69.3)
+17.2*** |
+0.5 (.91) | 52.3 (48.0,56.6) | 63.0 (58.9,67.1)
+10.7*** |
+7.0 (.11) | 45.3 (41.0,49.7) | 63.0 (58.8,67.2)
+17.7*** |
| Sexual intercourse | 30.0 (26.0,34.0) | 43.6 (39.3,47.9)
+13.6*** |
8.4 (.05) | 32.5 (28.5,36.5) | 46.5 (42.2,50.8)
+14.0*** |
8.8 (.04) | 36.6 (32.4,40.8) | 41.8 (37.5,46.1)
+5.2** |
| Agreed that hepatitis B causes | ||||||||
| Liver cancer | 64.8 (60.5,69.0) | 77.1 (73.5,80.7)
+12.3*** |
−2.3 (.57) | 69.3 (65.3,73.3) | 81.4 (78.1,84.7)
+12.1*** |
−2.5 (.52) | 63.4 (59.2,67.6) | 78.0 (74.4,81.6)
+14.6*** |
| Incorrect knowledge | ||||||||
| Agreed that one can get hepatitis B from: | ||||||||
| Smoking cigarettes | 36.0 (31.8,40.2) | 37.3 (33.1,41.5)
+1.3 |
−3.5 (.41) | 35.8 (31.7,39.9) | 38.4 (34.2,42.6)
+2.6 |
−2.2 (.60) | 32.2 (28.1,36.3) | 37.0 (32.8,41.2)
+4.8 |
| Exposure to another’s coughing/sneezing | 46.0 (41.6,50.4) | 43.6 (39.3,47.9)
−2.4 |
−8.0 (.07) | 41.4 (37.2,45.6) | 40.9 (36.7,45.1)
−0.5 |
−6.1 (.16) | 36.6 (32.4,40.8) | 42.2 (37.9,46.5)
+5.6 |
| Agreed that hepatitis B causes: | ||||||||
| Lung cancer | 28.4 (24.4,32.4) | 30.8 (26.8,34.8)
+2.4 |
−2.3 (.56) | 25.2 (21.5,28.9) | 26.7 (22.9,30.5)
+1.5 |
−3.2 (.41) | 22.3 (18.7,25.9) | 27.0 (23.1,30.9)
+4.7 |
Bold numbers indicate estimated percentage differences from pre- to postintervention (post- minus pre-).
Comparison of 3 sites at preintervention by χ2 test, P < .01.
Comparison of 3 sites at postintervention by χ2 test, P < .001.
Comparison between pre- and postintervention by χ2 test, P < .05.
Comparison between pre- and postintervention by χ2 test, P < .01.
* Comparison between pre- and postintervention by χ2 test, P < .001.
Parents’ knowledge also increased. In all 3 areas, significantly more parents knew at postintervention compared with preintervention that sharing a toothbrush and sexual intercourse were possible modes of HBV transmission. However, only the increase in knowledge of transmission by sexual intercourse was significant in the media education area (+14.0 percentage points) and community mobilization (+13.6 percentage points) areas compared with the control area (+5.2 percentage points; P < .05 for both). Rates did not change for incorrect responses (smoking cigarettes, coughing/sneezing). The number of parents who knew that liver cancer is a potential sequel to HBV infection increased significantly between pre- and postintervention in all 3 areas (P < .001), but there was no significant difference between intervention and control sites in the change. Rates did not change significantly for the incorrect response (lung cancer).
Children’s Receipt of HepB
We compared estimates of the raw changes in rates of vaccine receipt (HepB × 3) using parent-reported data from shot records, provider-reported data from medical records, and parent-or-provider-reported data (Table 3). Very few parents could find records from which to report vaccination dates in the pre-(n = 225) and postintervention (n = 238) surveys. Samples based on parents’ reports were too small in all 3 sites to allow for reliable calculations of rates.
TABLE 3.
Receipt of 3 Doses of HepB by Vietnamese-American Children by Intervention Site, Ages 3 to 16 at Preintervention (1998) and 5 to 18 at Postintervention (2000), % (95% CIs), Parent-Reported, Provider-Reported, and Parent-or Provider-Reported Data‡
| Community Mobilization at Preintervention | Community Mobilization at Postintervention | χ2 Test of Change Compared to Control (P Value) | Media Education at Preintervention | Media Education at Postintervention | χ2 Te st of Change Compared to Control (P Value) | Control at Preintervention | Control at Postintervention | |
|---|---|---|---|---|---|---|---|---|
| Parent-reported | N = 102 | N = 92 | N = 93 | N = 93 | N = 30 | N = 53 | ||
| 3 doses HepB | 40.5 (31.0,50.0) | 51.6 (41.4,61.8)
+11.1 |
9.4 (.49) | 43.1 (33.0,53.2) | 77.1 (68.5,85.6)
+34.0** |
+32.3 (.01) | 49.9 (32.0,67.7) | 51.6 (38.1,65.0)
+1.7 |
| Provider-reported | N = 273 | N = 174 | N = 189 | N = 270 | N = 232 | N = 216 | ||
| 3 doses HepB | 21.7 (16.8,26.6) | 28.7 (22.0,35.5)
+7.1 |
+14.1 (.02) | 21.3 (15.5,27.1) | 23.8 (18.7,28.9)
+2.5 |
+9.6 (.11) | 36.2 (30.1,42.4) | 29.2 (23.1,35.2)
−7.1 |
| Parent-or-provider-reported | N = 307 | N = 225 | N = 233 | N = 315 | N = 243 | N = 244 | ||
| 3 doses HepB | 26.6 (21.7,31.6) | 38.8 (32.4,45.2)
+12.2** |
+ 16.4 (.01) | 28.5 (22.7,34.3) | 39.4 (34.0,44.8)
+10.9* |
+15.2 (.01) | 37.8 (31.7,43.9) | 33.5 (27.6,39.4)
+4.3 |
Bold numbers indicate estimated percentage differences from pre- to postintervention (post- minus pre-).
For these pre-post comparisons an age adjustment was conducted to control for slight differences in the age distributions in pre- and post- samples.
Excluding those people who do not have records.
Comparison between pre- and postintervention by χ2 test, P < .05.
Comparison between pre- and postintervention by χ2 test, P < .01.
Samples generated using provider-reported data from pre- (n = 694) and postintervention (n = 660) surveys were larger. However, many physicians we contacted could not provide any shot records. When we excluded the unknown cases, without controlling for differences in site or factors associated with hepatitis B vaccination, provider-reported data show that rates declined slightly in the control community (−7.1 percentage points), but increased significantly in the community mobilization area (+7.1 percentage points, P = .01) and slightly in the media education area (+2.5 percentage points, P = not significant).
Given that both parent-reported data and provider-reported data came from written records, we pooled these data to create larger pre- (n = 783) and postintervention (n = 784) samples. When we included only those cases for which the parents or providers could find records, the data show that, without controlling for other factors, vaccination rates decreased slightly in the control area (−4.3 percentage points, P = not significant) while increasing significantly in both the community mobilization (+12.2 percentage points, P < .01) and media education (+10.9 percentage points, P < .05) areas. When we classified the unknown cases as having not been vaccinated and included them in the sample, parent-or-provider data showed that there was a slight decline in the control area (−1.8% percentage points), no significant increase in the community mobilization area (+1.7% percentage points), but a significant increase in the media education area (+12.6 percentage points, P < .01).
Figure 1 shows the change in vaccination rate as reported by parents or providers between pre- and postintervention by matched birth cohorts, in the media education, community mobilization, and control areas. In the media education area, there was a 10 to 30 percentage point increase in vaccination rates among older children (ages 10 –17 in the year 2000) compared with some decrease among the controls. In the community mobilization area, vaccination rates also increased by 10 to 30 percentage points among older children (ages 11–17), with substantial increases for children ages 11, 12, and 14.
Fig 1.
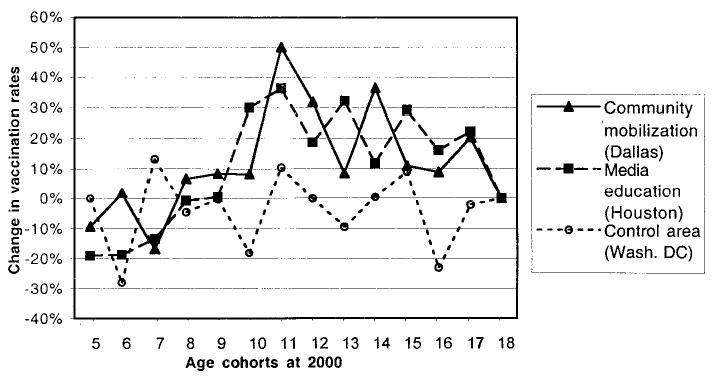
Change in vaccination rates between pre- and postintervention, parent-or-provider-reported data, by intervention site, or by birth cohort.
Results of Multivariate Analyses
As stated above, the primary analysis was conducted using a sample of pooled data from the pre-and postintervention surveys that we obtained from parents and/or providers, and that excluded the indeterminate cases (n = 1567). The dichotomous outcome was receipt of 3 doses of HepB (HepB × 3) = 1 (n = 515), or not = 0 (n = 968). The parsimonious model estimated the independent effects of the interventions on HepB × 3 and identified other predictors of vaccination status that were significant at P < .05 (Table 4). The model was highly significant (log likelihood ratio for model P < .0001) and accurately predicted the HepB × 3 status of 79.7% of the cases. Model parameters are shown as adjusted ORs and 95% CIs for each variable.
TABLE 4.
Multiple Logistic Regression Analysis: Parsimonious Model of Predictors of Vietnamese-American Children Having Received 3 Doses of HepB (HepB × 3), Pooled Data from Pre- and Postintervention, Parent-or-Provider Reported (N = 1483*)
| HepB × 3
|
||
|---|---|---|
| Independent Variable | Adjusted OR | 95% CI |
| Residence in the community mobilization area (Dallas) compared to residence in the control area at pre-intervention | 0.66 | 0.43–1.02 |
| Residence in the media education campaign area (Houston) compared to residence in the control area at pre-intervention | 0.64 | 0.40–1.02 |
| Residence in the control area at postintervention compared to residence in the control area at preintervention | 1.37 | 0.86–2.16 |
| Residence in the community mobilization area at post- intervention compared to preintervention | 2.94 | 1.88–4.59 |
| Residence in the media education campaign area at postintervention compared to preintervention | 4.14 | 2.58–6.60 |
| Community mobilization intervention effect (Dallas × postintervention): change in HepB × 3 controlling for change in the control area | 2.15 | 1.16–3.97 |
| Media education campaign intervention effect (Houston × postintervention): change in HepB × 3 controlling for change in the control area | 3.02 | 1.62–5.64 |
| Child’s age | 0.79 | 0.76–0.81 |
| Parents married | 1.72 | 1.10–2.67 |
| Years since parents immigrated to United States | 0.98 | 0.96–0.99 |
| Household income above the poverty line | 0.72 | 0.54–0.95 |
| Child received ≥ 1 DTP vaccination | 4.08 | 3.13–5.31 |
| Know someone with liver disease | 1.67 | 1.27–2.18 |
| Heard of hepatitis B | 1.61 | 1.22–2.12 |
| Index of parents’ knowledge about hepatitis B | 1.10 | 1.01–1.19 |
| Have Medicaid | 0.64 | 0.41–0.99 |
A total of 84 observations were deleted because of missing values for predictor variables.
The variables that control for site (Dallas and Houston) show that, independent of the interventions, children who lived in the Dallas or Houston area were somewhat less likely to have received HepB × 3 as children living in the control (Washington, DC) area, although this was not statistically significant. The variable that controls for secular trends (postintervention) shows that, independent of the interventions, children in the group surveyed after the intervention were no more likely to have received HepB than those surveyed before the intervention.
The variables that estimate the impact of community mobilization (Dallas × postintervention) and the media campaign (Houston × postintervention) suggest that both interventions produced significant effects that were roughly equivalent (Table 4). A child living in the Dallas area during the community mobilization intervention was more than twice as likely (OR = 2.15, 95% CI 1.16 –3.97) to have received 3 shots of HepB compared with a child living in the control area. Similarly, a child living in the Houston area during the media education campaign was 3 times as likely (OR = 3.02, 95% CI 1.62–5.64) to have received 3 shots of HepB compared with a child living in the control area.
The model identified 4 sociodemographic predictors of HepB × 3. Independent of any intervention effects, child’s age was strongly associated with HepB × 3 such that older children were less likely to have been vaccinated (OR × 0.79 for each additional year of age). Parents’ marital status was significantly associated with HepB × 3 (OR × 1.72 if married). The number of years since the parent had immigrated (OR × 0.98 for each additional year since immigration), household income above the poverty line (OR × 0.72), and having Medicaid (OR × 0.64) were negatively associated with HepB × 3, although these predictors were only marginally significant. In addition, a child who had received at least 1 DTP shot was > 4 times as likely to have received HepB × 3 (OR × 4.08).
Parents’ awareness and knowledge was also predictive of receipt of HepB × 3. Children were more likely to have received HepB × 3 if their parents knew someone who had liver disease (OR = 1.67) or had heard of hepatitis B (OR = 1.61). Children whose parents had higher scores on the index of knowledge about hepatitis B were slightly more likely to have received HepB × 3 (OR = 1.10), although this predictor was only marginally significant.
In the secondary analysis, we used a sample that included the undetermined cases, classifying them as not having been vaccinated. To determine if the intervention had a greater effect on older or younger children, we included a variable that classified the cases into 2 age cohorts (born 1989 –1995 = 1, 1982–1988 = 0). We specified 2-way and 3-way interaction terms between cohort and the intervention variables (Dallas × postintervention × COHORT 89 –95 and Houston × postintervention × COHORT 89 –95). All of the predictor variables found the parsimonious model in the primary analysis appeared in the model for the secondary analysis sample with similar ORs, except for “household income above poverty line,” and “index of parent’s knowledge about hepatitis B,” which were not significant. The secondary analysis showed that older children who lived in the media campaign area were more likely (OR = 4.89, 95% CI 1.82–13.18) to have received HepB × 3 than younger children in that area (OR = 2.42, 95% CI 1.20 –4.88). Similarly, in the community mobilization area, we found that the older cohort was more likely to have received HepB × 3 (OR = 4.66, 95% CI 1.58 –13.78) than younger children (OR = 1.10, 95% CI 0.56 –2.18). However, the OR for the ≥ 1 DTP variable was substantially higher in the secondary analysis (OR = 11.44, 95% CI 9.00 –14.53) than in the primary analysis (OR = 3.58, 95% CI 2.74 –4.66). Given that we treated all reclassified cases (those without records) as having had no DTP shots and no hepatitis B shots, the ≥1 DTP variable was highly correlated with the HepB × 3 variable.
DISCUSSION
The community mobilization and media education campaigns were equally effective in increasing hepatitis B vaccination among Vietnamese-American children. The regression results suggest that community mobilization strategy doubled, and the media education trebled, the likelihood of a child receiving the HepB series. Against the backdrop of a slightly declining secular trend in vaccination rates observed in the control site, both interventions produced significant, although not enormous, increases in vaccination.
During the period of our study, there were no mandates for hepatitis B vaccination before entry into middle school in either of the intervention communities, so the interventions’ effects cannot be attributed to such laws. A middle school entry law went into effect in Texas after the intervention period in August 2000. A middle school entry law was in effect during the intervention period in a portion of the control area, the District of Columbia, although not in the neighboring counties of Maryland and Virginia, which comprised the remainder of the control area. However, any effect of the Washington, DC law would have been to increase vaccination rates between pre- and postintervention in the control area, and this was not observed. Community informants monitored public health activities and confirmed that there were no other large-scale promotional hepatitis B vaccination efforts for Vietnamese-American children conducted in the study areas during 1998 –2000.
The media education campaign appears to have produced significantly greater increases in general awareness of hepatitis B and immunization than the community mobilization strategy. This was expected because mass media ads can distribute general information broadly. Both the media education and community mobilization strategies increased parents’ specific awareness about the availability of free shots. Results from the regression models suggest that, even when Vietnamese-American parents were exposed to the broader effects of the interventions, those who knew someone with liver disease or had heard of hepatitis B were more likely to have their children vaccinated.
Regarding parents’ knowledge, large increases were also observed in the control group, probably because the information our media campaign presented was “picked up” by Vietnamese language media outlets in the Washington, DC area, as we have found to be common practice elsewhere in the United States, and thus “contaminated” the control group. Still, both interventions appear to have been effective in significantly increasing parents’ understanding of specific modes of transmission. In particular, after the interventions, significantly more parents’ understood that sexual intercourse was a mode of virus transmission. This finding is especially important because sexuality is a taboo subject in Vietnamese culture, making it difficult for researchers to convey information about the risks of sexual transmission of hepatitis B and other diseases. Yet within this cultural context, we were able to present information about sexual transmission to which people paid attention.
Unfortunately, fairly large percentages of parents maintained inaccurate knowledge about other modes of transmission, believing that smoking cigarettes or another person’s coughing or sneezing transmitted the virus (Table 2). Neither intervention had an impact on reducing the number of people who held these beliefs. Similarly, despite the interventions, about one quarter of parents in all 3 sites maintained the incorrect belief that HBV causes lung cancer.
We believe that both strategies were successful because the approaches were culturally appropriate for reaching Vietnamese-American immigrant communities. In every community where Vietnamese-Americans have settled in large numbers, they have established vibrant Vietnamese-language print, radio, and television media. These media have flourished because Vietnamese-Americans are avid consumers of news, community information, and advertising. It is likely that the media education campaign, in raising awareness, shaped social norms about hepatitis B vaccination for children. The campaign also was highly effective in providing families with specific information about how and where to have their children vaccinated. This aspect of the campaign addressed a significant barrier this immigrant population faces—difficulty gaining access to information in Vietnamese about preventive health care services.20 The community mobilization strategy brought people together to work on an issue, and in doing so, stimulated group enthusiasm. This approach was effective because it built on a cultural pattern among Vietnamese-Americans to form groups to create social supports and a sense of connectedness with others. In our experience, we have found that these social groups play a vital role in helping recent immigrants maintain their culture while adapting to life in America. Vietnamese-American service organizations help facilitate the difficult transition from refugee or immigrant to resident or citizen. They orient the recently arrived immigrant to an unfamiliar and complex American health care system, and have a long history of mobilizing their members to obtain services.
There are several limitations to this study. First, the populations studied may not represent the nationwide Vietnamese-American population. Second, the cities in which we conducted our programs may not be representative of other US cities, including others in which targeted catch-up hepatitis B vaccination programs, have been conducted.21 Nonetheless, we believe these 2 strategies could be used to promote catch-up vaccinations against other communicable diseases (eg, DTP or varicella) in the Vietnamese-American population, and potentially in other ethnic enclaves with their own media. Third, the smaller target population in Dallas undoubtedly made the community mobilization task easier; the much larger population in Houston was more efficiently reached by a media education intervention. Fourth, the study design was limited in not having a third intervention arm combining the elements of the media education campaign with those of the community mobilization intervention. Although more expensive to conduct, a combined intervention might be even more effective; future studies could perhaps test a combined approach. Fifth, we cannot discount the possibility that some of the information from our media education campaign in Houston may have seeped into the Dallas media market. The community mobilization program possibly benefited from a “boost” from the media campaign because families travel between the 2 cities, ~240 miles apart. Finally, biases may have resulted from a loss of randomness in sampling, nonrespondents whose children’s vaccination rates differed from respondents, and missing parent or provider vaccination records that may have caused inaccurate coverage estimates.21
Measurement of vaccination status remains a major challenge for vaccination projects focused on reaching immigrant populations. Using dates from vaccination records, while highly reliable, is a stringent standard for measurement. The reality is that Vietnamese-Americans, like most Americans, do not keep their children’s vaccination records handy, if at all. Furthermore, their health care providers, many of whom were extremely busy and not focused on research, often did not have the resources or interest to have their staff dig out vaccination dates from patient records. Immunization registries would most certainly address this problem and contribute to achieving universal vaccination.22
The effects of measurement criteria are revealed in the comparison of the primary and secondary multivariate analyses. The criterion used to classify cases for which there are no records produces tradeoffs. Using a sample that excludes the cases for which there was no vaccination data increases the sensitivity of the analysis, but is based on a sample that undercounts the number of unvaccinated children. Classifying all of the cases for which there is no data as having not been vaccinated increases the specificity of the analysis, but misclassifies some children who were vaccinated. This problem is complicated further when these same children are, for lack of a record, classified as unvaccinated for DTP because we know DTP vaccination rates are much higher than this classification would suggest. When DTP is included in the model, some unknown distortion of the estimated coefficients occurs.
Nevertheless, both analyses show that, regardless of whether the undetermined cases were included or not, the interventions increased the odds of a child being vaccinated. Although somewhat less reliable, the secondary analysis adds to this picture. It suggests that both interventions had a greater impact on the cohort of older children who, as the primary analysis shows, were far less likely to have been vaccinated before intervention. The data presented in Fig 1 show that the interventions were more effective in achieving catch-up vaccinations for almost all children older than age 10, the age of middle school entry.
Hepatitis B vaccination rates for Vietnamese-American children in all 3 locations were unsatisfactory both before and after the interventions. That both interventions achieved only modest increases in vaccination coverage demonstrates the challenges of reaching this group. Dueson et al,23 who conducted an intervention study of hepatitis B catch-up vaccination among 4384 Cambodian-American and Vietnamese-American children in Philadelphia, Pennsylvania, found a preintervention rate of 3.6% for receipt of 3 doses of HepB and a postintervention rate of 15.5%. Their study produced an increase of 11.9% after 1 year of intervention. Annual catch-up vaccination rates of 7% to 11% have also been achieved by interventions targeting Asian children in Milwaukee, Seattle, and St. Paul, compared with 0.7% to 2.6% in cities without such programs (CDC, 2000). Other data from various city and state reports indicate that only 40% of all Asian-Pacific Islander children in the United States ages 7 to 18 years have completed their HepB series.24 This low vaccination rate in a group at high risk for HBV infection indicates a compelling need for continued efforts to reach these children.
CONCLUSIONS
The impact of our interventions illustrates 2 effective approaches, media education and community mobilization strategies, for community-based organizations and public health departments to reach Vietnamese-American immigrant populations. Furthermore, such interventions can prove both cost-effective and cost-beneficial.23,25 The results presented here provide support for further work nationwide to boost very low hepatitis B vaccination rates among Vietnamese-American children. Catch-up hepatitis B vaccination programs should merit the highest priority for these children. It is imperative to implement effective interventions now so that hepatitis B infection and its sequelae can be averted in this generation of Vietnamese-American children, thereby breaking the cycle of transmission to the next generation.
Acknowledgments
This research was supported by funds provided by the CDC under Cooperative Agreement U66/CCU915175. We are deeply indebted to Christopher N. H. Jenkins, MA, MPH (deceased) for project design and direction, and to Yifei Ma, MA, MS, Fangjun Zhou, PhD, and Joyce Bird, PhD, for their invaluable assistance in data analysis.
References
- 1.Beasley RP. Hepatitis B virus as the etiologic agent in hepatocellular carcinoma—epidemiologic considerations. Hepatology. 1982;2:21S–26S. [Google Scholar]
- 2.Beasley RP, Hwang L-Y, Lin C-C, Chien C-S. Hepatocellular carcinoma and hepatitis B virus: a prospective study of 22,707 men in Taiwan. Lancet. 1981;2:1129 –1133. doi: 10.1016/s0140-6736(81)90585-7. [DOI] [PubMed] [Google Scholar]
- 3.Margolis HS, Coleman PJ, Brown RE, Mast EE, Sheingold SH, Arevalo JA. Prevention of hepatitis B virus transmission by immunization: an economic analysis of current recommendations. JAMA. 1995;274:1201–1208. [PubMed] [Google Scholar]
- 4.Klontz KC. A program to provide hepatitis B immunoprophylaxis to infants born to HBsAg-positive Asian and Pacific Islander women. West J Med. 1987;146:195–199. [PMC free article] [PubMed] [Google Scholar]
- 5.Mahoney FJ, Lawrence M, Scott C, Le Q, Lambert S, Farley TA. Continuing risk for hepatitis B virus transmission among Southeast Asian infants in Louisiana. Pediatrics. 1995;96:1113–1116. [PubMed] [Google Scholar]
- 6.Tong MJ, Hwang S-J. Hepatitis B infection in Asian Americans. Gastroenterol Clin North Am. 1994;23:532–536. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Screening for hepatitis B infection among refugees arriving in the United States, 1979 –91. MMWR Morb Mortal Wkly Rep. 1991;40:784 –786. [PubMed] [Google Scholar]
- 8.Miller BA, Kolonel LN, Bernstein L, et al., editors. Bethesda, MD: National Cancer Institute; 1996. Racial/Ethnic patterns of Cancer in the United States: 1988–92. Publ. No. 96-4104 NIH. [Google Scholar]
- 9.Centers for Disease Control and Prevention. Update: recommendations to prevent hepatitis B virus transmission—United States. MMWR Morb Mortal Wkly Rep. 1999;48:33–34. [PubMed] [Google Scholar]
- 10.Anonymous Hepatitis B immunization requirements for school. [Accessed on October 15, 2001];Hepatitis B Prevention Mandates, Immunization Action Coalition. Available at: www.immunize.org/laws/hepb.htm.
- 11.Centers for Disease Control and Prevention. National, state, and urban area vaccination coverage levels among children aged 19 –35 months—United States, 1997. MMWR Morb Mortal Wkly Rep. 1998;47:547–554. [PubMed] [Google Scholar]
- 12.Jenkins CNH, McPhee SJ, Wong C, Nguyen T, Euler GL. Hepatitis B immunization coverage among Vietnamese-American children 3 to 18 years old. Pediatrics. 2000;106(6) doi: 10.1542/peds.106.6.e78. Available at: www.pediatrics.org/cgi/content/full/106/6/e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Vaccination coverage by race/ethnicity and poverty level among children aged 19 –35 months—United States, 1997. MMWR Morb Mortal Wkly Rep. 1998;47:956 –959. [PubMed] [Google Scholar]
- 14.Jenkins CNH, Buu C, Berger W, Do ST. Liver carcinoma prevention among Asian Pacific Islanders. Cancer. 2001;91:252–256. doi: 10.1002/1097-0142(20010101)91:1+<252::aid-cncr14>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 15.U. S. Bureau of the Census. June 12, 1991. Press Release No. CB91-215. [Google Scholar]
- 16.U. S. Bureau of the Census. [Accessed on June 7, 2002];Census 2000. Available at: www.census.gov/prod/cen2000/dp1/2kh00.pdf.
- 17.Jenkins CNH, McPhee SJ, Bird JA, Bonilla N-TH. Cancer risks and prevention behaviors among Vietnamese refugees. West J Med. 1990;153:34 –39. [PMC free article] [PubMed] [Google Scholar]
- 18.Anonymous Annual update of the federal poverty income guidelines. Federal Register. 1997;62:10856 –10859. [PubMed] [Google Scholar]
- 19.SAS Institute. Cary, NC: SAS Institute, Inc; 1999. SAS/STAT User’s Guide. Release 8.0. [Google Scholar]
- 20.McPhee SJ. Caring for a 70-year-old Vietnamese woman [Clinical Crossroads] JAMA. 2002;287:495–504. doi: 10.1001/jama.287.4.495. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Hepatitis B vaccination coverage among Asian and Pacific Islander children—United States, 1998. MMWR Morb Mortal Wkly Rep. 2000;49:616 –619. [PubMed] [Google Scholar]
- 22.Wilcox SA, Koepke CP, Levenson R, Thalheimer JC. Registry-driven, community-based immunization outreach: a randomized controlled trial. Am J Public Health. 2001;91:1507–1511. doi: 10.2105/ajph.91.9.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dueson RR, Brodovicz KG, Barker L, Zhou F, Euler GL. Economic analysis of a child vaccination project among Asian Americans in Philadelphia, PA. Arch Pediatr Adolesc Med. 2001;155:909 –914. doi: 10.1001/archpedi.155.8.909. [DOI] [PubMed] [Google Scholar]
- 24.Euler GL. Changing the legacy for Asian Americans and Pacific Islanders. Asian Am Pacific Isl J Health. 1998;6:304 –310. [PubMed] [Google Scholar]
- 25.Zhou F, Euler GL, McPhee SJ, et al. Economic analysis of promotion of hepatitis B vaccinations among Vietnamese-American children and adolescents in Houston and Dallas. Pediatrics. 2003;111:1289 –1296. doi: 10.1542/peds.111.6.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]


