Abstract
Pharmacogenomics is defined as the study of the impacts of heritable traits on pharmacology and toxicology. Candidate genes with potential pharmacogenomic importance include drug transporters involved in absorption and excretion, phase I enzymes (e.g., cytochrome P450-dependent mixed-function oxidases) and phase II enzymes (e.g., glucuronosyltransferases) contributing to metabolism, and those molecules (e.g., albumin, A1-acid glycoprotein, and lipoproteins) involved in the distribution of antifungal compounds. By using the tools of population genetics to define interindividual differences in drug absorption, distribution, metabolism, and excretion, pharmacogenomic models for genetic variations in antifungal pharmacokinetics can be derived. Pharmacogenomic factors may become especially important in the treatment of immunocompromised patients or those with persistent or refractory mycoses that cannot be explained by elevated MICs and where rational dosage optimization of the antifungal agent may be particularly critical. Pharmacogenomics has the potential to shift the paradigm of therapy and to improve the selection of antifungal compounds and adjustment of dosage based upon individual variations in drug absorption, metabolism, and excretion.
INTRODUCTION
For decades, amphotericin B was the only choice for treating invasive fungal infections. The introduction of fluconazole and itraconazole offered alternative options for antifungal chemotherapy, which broadened further with the development of new, more potent azoles, such as voriconazole and posaconazole, as well as the discovery of the new class of echinocandins (123). Despite these advances, mortality rates for invasive fungal infections can approach 90%, particularly in the immunocompromised host (64, 104, 190). Moreover, a significant number of patients experience adverse effects, necessitating the termination of treatment (101). Progression of infection despite antifungal chemotherapy is often observed, and therefore, alternative therapeutic approaches are employed in order to reverse the clinical outcome. The clinical outcome is dependent on factors that include host defenses, the virulence of the fungal pathogen, and drug efficacy/toxicity, as well as drug interactions (148, 277). Pharmacokinetic studies of antifungal agents have shown variability of at least 50% between individuals (45, 49, 101, 103, 192, 206). For instance, interindividual variability in voriconazole plasma levels ranges from 74% to 100% (121). These differences certainly can contribute to a lack of efficacy and adverse side effects. Additional factors, such as age, gender, underlying disease status, and concomitant therapies, can account for these differences, but host genetics probably play important roles in both drug efficacy and toxicity (75).
Pharmacogenomics is defined as the study of the impact of heritable traits on pharmacology and toxicology (213). The association of genetic variations with drug response has been documented for many diseases and drugs (75, 273), leading to impressive progress in this field. While initially the term “pharmacogenetics” was used, it is limited to studies in which single genes are associated with variations in drug metabolism. In contrast, pharmacogenomic studies integrate with genomewide strategies to elucidate the relationship between sets of genetic variation and drug response (181). Furthermore, pharmacogenomics can also refer to the science that focuses on how the genome as a whole influences the actions of drugs (37). When genetic polymorphisms are linked to toxicity rather than to efficacy, the term toxicogenomics is frequently used.
Germ line genetic variation manifests in the genome in different forms, such as structural abnormalities, like chromosomal deletions, insertions, duplications, inversions, and translocations, and by changes in the sequence of DNA, such as single-nucleotide insertions, deletions, substitutions (transition or transversion), or dinucleotide and tandem-repeat deletions/insertions (213). Variations with a prevalence of the minor allele (gene variant) of at least 1% in at least one population are called common polymorphisms. The most abundant source of genetic variation is the single-nucleotide polymorphism (SNP), which accounts for more than 90% of genetic variants and is distributed roughly every 400 bp throughout the genome; there are over 10 million distinct SNPs currently deposited in db-SNP (http://www.ncbi.nlm.nih.gov/SNP) (219). The total number of common SNPs in the human genome is estimated to be more than 10 million (28), and the number of SNPs with minor-allele frequencies of over 10% is estimated to be perhaps as many as 5 million (152).
Most SNPs are distributed throughout the intergenic regions, which comprise over 95% of the genome, yet attention has focused on SNPs in gene-regulatory regions (e.g., promoters, enhancers, silencers, and transcription factor binding sites), coding regions (e.g., exons), noncoding regions (e.g., introns), and untranslated regions (e.g., the 5′ end and 3′ end of mRNA) (Fig. 1) (40, 214). Only a small subset of SNPs actually alter the function of the translated protein (functional SNPs) by affecting the processes of transcription (e.g., no RNA production, wrong splicing, or unstable RNA) and translation (e.g., no protein production, different amino acids, or truncated amino acid chains) (246). It is estimated that there are between 50,000 and 250,000 functional SNPs (40). Studies of genes involved in drug response have shown that the majority of SNPs in coding regions are silent, also known as synonymous (specifying the same amino acid). For the category of nonsynonymous SNPs (i.e., those that alter the amino acid sequence), the majority are conservative, in which there is a replacement of an amino acid by a chemically similar one, but for roughly one-quarter of nonsynonymous SNPs, a radical or nonconservative substitution arises, namely, they are more likely to disrupt the structure/function of the protein. Overall, it is estimated that <1% represent nonsense insertions or deletions, resulting in a premature stop codon (221). SNPs residing in critical cis-acting elements and locus control regions can also be important, particularly if they map to a functional binding domain for a transcription binding factor. Recent studies of the dopamine receptor D2 gene have revealed that a noncoding SNP can alter the expression of a gene, in this case by affecting the stability of the mRNA species (70). Seventy-five percent of nonsynonymous SNPs have minor allele frequencies of less than 15% (180). Recent surveys of SNPs suggest that selective pressure has decreased two classes of SNPS that can be most disruptive, radical nonsynonymous changes and insertions/deletions (126).
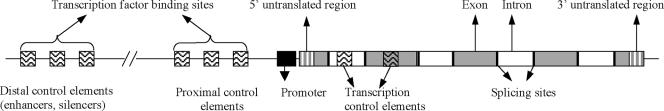
FIG. 1.
Components of eukaryotic genes in which functional SNPs may reside and alter the expression levels and form of the encoded protein.
SNPs are passed from one generation to the next in sets, or blocks. In other words, SNPs are not inherited randomly but in association with one another. This correlation between SNPs is measured as linkage disequilibrium. Linkage disequilibrium across a region of a chromosome is defined on the basis of two or more SNPs cosegregating in a nonrandom manner (89). The challenge of associating common SNPs with outcomes lies in the fact that a single SNP rarely determines an outcome. Thus, the complexity of multigenic factors has to be analyzed carefully and by population parameters. Because SNPs are neither necessary nor sufficient for an outcome, the effect of an SNP is measured as a change in risk. Consequently, sets of SNPs probably act together, usually in a complex pattern. It is possible that the effect of an SNP can follow a dominant or recessive model, but a gene dosage effect is also possible, especially in the context of examining gene-environment or gene-drug interactions (34, 213).
Epigenetic factors, such as DNA methylation and histone modification (79), can also contribute to measured pharmacologic outcomes (15). A phenotype may also be altered in the absence of any structural SNP due to trans-acting elements, which are factors usually considered to be proteins that bind to cis-acting sequences (DNA sequences in the vicinity of the structural portion of a gene that are required for gene expression) and that control gene expression in a specific tissue (spatial regulation) at a specific time (temporal regulation) after modification (phosphorylation), ligand binding, or an appropriate environmental signal. While these factors should be targeted for the study of pharmacogenomics, for the foreseeable future, the emphasis will be on pursuing germ line genetic polymorphisms and drug pharmacokinetics.
GENETIC ASSOCIATION STUDIES
Genetic association studies are conducted to determine if one or more alleles have a nonrandom distribution with a defined outcome (251). Traditionally, there are two types of association studies: one searches with linked markers across the entire genome, and the second analyzes annotated variants in candidate genes, chosen because of their plausibility in influencing pharmacokinetics. In the indirect method, which is used in a whole-genome approach, the search is intended to identify a region or locus, which in turn is further analyzed. The follow-up analysis employs the same method as the classical candidate gene approach, in which known genetic variants are analyzed. The whole-genome approach has been successful for mapping rare, highly penetrant diseases in family pedigrees, but due to technical and analytical challenges, it has been less successful in unrelated subjects. Moreover, although this approach has been successful in identifying genes for monogenic traits, its application might be limited for polygenic traits, which by definition have more complex inheritance patterns (13). As an alternative to family-based linkage analysis, preliminary studies have attempted to detect novel genes associated with complex traits by population-based genomewide approaches (180) using anonymous genetic markers (microsatellites and SNPs) spanning the entire genome (52). Although this approach does not require a priori knowledge of the target gene, the identification and mapping of the thousands of SNPs that would be used as genetic markers is needed (35, 214). It is estimated that a minimum of 300,000 to 500,000 evenly spaced SNP markers would be needed to have a marker within the range of linkage disequilibrium (LD) (35). Whereas this density may be useful for uncovering SNPs in genomic regions with extensive LD genes, in regions with less extensive LD, disease-related variants that are rare will be missed.
Currently, the most commonly employed approach for genetic association studies is based on the choice of candidate genes, in other words, those that have high prior likelihood based on a plausible hypothesis (50). Known variants are analyzed in unrelated subjects in a case control study. In contrast to single gene traits, in the complex-disease paradigm, a particular allele does not determine the characteristic but instead alters risk. Population-based studies can provide adequate power to detect relative risks as low as 1.5, which is usually not possible in family studies (214).
Population-based candidate gene association studies are the most commonly employed approach to explore common genetic polymorphisms and drug response. In designing such studies, there are several important issues to be considered. The choice of SNPs in candidate genes requires a good knowledge of the molecular pharmacology of antifungal agents, as well as the physiological processes involved in drug disposition. Data from knockout animal studies for determining the pharmacokinetics of antifungal drugs in the absence of a gene, from the in vivo effects on antifungal pharmacokinetics of inhibitors of physiological processes involved in drug disposition, from in vitro studies for the interaction of antifungal compounds with human biomolecules, and from microarrays and proteomics can be helpful in deciding which genes are important for the disposition of antifungal agents.
Because of the rapid expansion in genotype databases and the falling costs of genotype analysis, it is now possible to conduct candidate gene association studies with sets of genes within a pathway or process. Thus, it is possible to interrogate sets of genes that differentially confer risk. For example, the study of the metabolism of a specific drug compound is ideally suited to this approach, because it is possible to define the critical genes in the activation and elimination of an antifungal compound.
Another important issue in association studies is the number of cases and controls that need to be recruited to achieve sufficient statistical power to detect differences in frequencies among different phenotypic groups. The sample size of an association study influences the level of significance (the probability of finding a difference by chance, or false positive) based on the power of the study (the probability of detecting a real difference, or true positive) and the frequency of the SNP. The literature has been marked by a plethora of findings that could not be replicated in subsequent studies. These false-positive results can be a consequence of inadequately powered studies (i.e., study sets that are too small), errors in genotyping, faulty selection of cases and controls, and population stratification. The last issue is not significant in Caucasian populations (with rare exceptions in isolated groups) but may be more problematic in populations with more admixture, such as individuals of Hispanic or African ancestry in the United States (84, 176, 264). Recently, a new strategy that is based on the prediction of a false-positive report has been advanced for determining whether a finding is notable (263). This approach looks at the prior probability that a finding could be real, as well as the power of the sample size and the allele frequency.
Another important issue, particularly in population-based genetic association studies, is population stratification. The study populations (cases versus controls) should be homogenous with regard to age, gender, ethnicity, and other socioeconomic factors (283). In order to overcome these problems, a method known as genomic control is used, in which the frequency of polymorphisms in other genes unlikely to be associated with the studied phenotype are compared between subjects in addition to the polymorphisms in the candidate gene of interest; appropriate adjustment is then made for population stratification (12) or association tests are performed within the identified subpopulations (205). Spurious associations may also be obtained in population-based studies due to gene-environment interactions, issues in case/control recruitment, and other biases (50). It has been argued that these pitfalls can be avoided in performing family-based association studies, but this approach is often practically challenging (241).
Finally, the correct assessment of outcome characteristics in cases and control is crucial in order to avoid having undetected individuals who bear the phenotypic characteristic in the control group. In the case of pharmacogenomics studies, the phenotype can be any pharmacokinetic parameter, such as the bioavailability, area under the curve (AUC), maximum plasma concentration (Cmax), time of Cmax, half-life, volume of distribution, clearance, and drug concentrations in serum and tissues, many of which can be derived after pharmacokinetic modeling. Lastly, pharmacogenomics has successfully identified markers that confer a shift in risk for the outcome or toxicity (180).
PHARMACOGENOMICS IN ANTIFUNGAL DRUG DISPOSITION
The relationship between genetics and pharmacokinetics has been apparent in the literature since the 1950s (253). For instance, it was noted that the half-lives of selected drugs were markedly similar in monozygotic twins but, when measured in dizygotic twins, varied widely. This same trend has been extended to studies of unrelated subjects, especially from different populations. A classic example is atypical cholinesterase activity, which can extend the half-life of succinylcholine, the neurotransmitter-blocking agent, and thus result in prolonged muscle paralysis and consequent apnea. The CYP2D6 genetic polymorphisms were originally described in an effort to explain differences in pharmacokinetics of select drugs, such as codeine and debrisoquin (273). Another well-described example has been validated in numerous studies, namely, variation in the thiopurine S-methyltransferase gene (TPMT); variants in the gene decrease enzymatic activity, thus yielding elevated concentrations of active metabolites. In turn, the extended half-lives of metabolites can induce life-threatening myelosuppression, even with standard doses of thiopurines used for treatment of leukemia and autoimmune disorders (183).
Genetic polymorphisms in drug transporters alter drug pharmacokinetics substantially, but to date, only a few examples have been well described (75). Since only a small percentage of the genes in the genome (roughly 30,000) have been analyzed, it is expected that additional genes will be identified. For example, genetic polymorphisms in the P-glycoprotein (P-gp, encoded by ABCB1), an ATP-binding cassette transporter, have been associated with variable expression in the duodenum, resulting in altered bioavailability of drugs such as digoxin. Finally, drug response can be influenced by genetic variation in key genes; for instance, sequence variants in the gene for the b2 adrenoreceptor (BDKRB2), which modulates response to b2 agonists, has been associated with efficacy in pulmonary disease. In some circumstances, a gene, such as the apolipoprotein E gene (APOE), which has been associated with risk for Alzheimer's disease, can also account for differences in therapeutic response (75). Thus, SNPs in fungal targets (e.g., lanosterol 14a-demethylase, 1,3-β-glucan synthase, and fungal drug transporters) may alter antifungal drug response by altering antifungal pharmacodynamics. These SNPs will not be reviewed here.
The analysis of the pharmacokinetics of antifungal compounds includes the administration, absorption, distribution, metabolism, and excretion of the drug, while pharmacodynamics refers to functional effects, namely, growth inhibition and fungicidal activity. Before a drug or its prodrug reaches the site of action, it has to pass through one or more membranes and frequently undergoes alteration. Each of the steps of the processes can be affected by one or more common genetic variations in one or more genes of the critical pathways (Fig. 2). This review discusses notable examples of common genetic variants that affect drug absorption, distribution, metabolism, and excretion. We review selected issues in pharmacokinetics, many of which are suitable targets for subsequent studies aimed at dissecting the contribution of genetic variation to the pharmacologic outcomes related to antifungal compounds. The principles of pharmacogenomics can be applied to the analysis of drug disposition, which in turn can influence the pharmacokinetics and pharmacodynamics of antifungal agents.
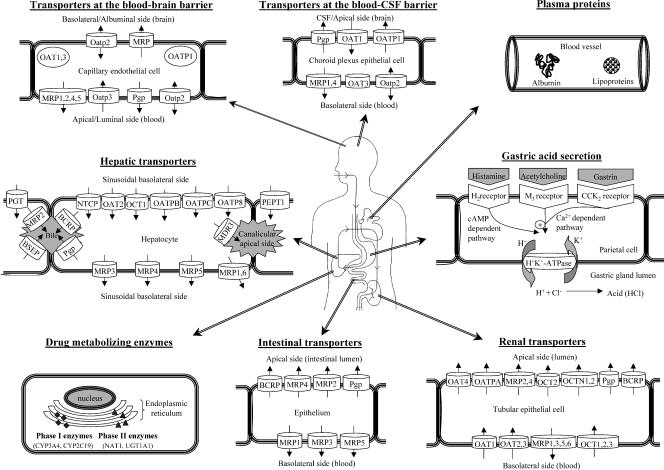
FIG. 2.
A schematic diagram of drug disposition and the physiological factors that play roles in drug pharmacokinetics, such as transporters, metabolizing enzymes, protein binding, and gastric acid excretion (data from references 39, 143, 153, 164, 199, and 248). Any variation in genes encoding proteins involved in the disposition of drugs may have an impact on drug pharmacokinetics. NTCP, sodium-dependent taurocholate transporting polypeptide; BSEP, bile salt export pump; PGT, prostagladin transporter; cAMP, cyclic AMP; NAT, N-acetyltransferase; UGT, UDP-glucuronosyl transferase. The exact localizations and efflux directions of some of these transporters are still under investigation.
Absorption
The oral absorption of drugs is affected by factors such as gastrointestinal motility, splanchnic blood flow, particle size, formulation of the agent, and physiochemical factors (e.g., binding to gastric contents) (232). Bacterial and gastrointestinal (GI) tract enzyme metabolism can reduce the availability of drugs, and extensive metabolism in the intestine and liver (the first-pass effect) may limit the amount of drug entering the systemic circulation. However, a drug must cross the GI mucosal surface before entering the systemic circulation. Although the carrier-mediated transport system may be responsible for transferring large (>500-molecular-weight) lipid-insoluble drug molecules, which resemble natural physiological metabolites (e.g., 5-fluorouracil) (254), efflux of xenobiotics out of the GI epithelial cells also occurs. In this regard, the location of drug transporters in the cell membrane also defines their contribution to the absorption process (Fig. 2).
Among antifungal agents, terbinafine, flucytosine, and most of the azoles can be administered orally (120, 171). Amphotericin B and echinocandins are administered only intravenously, due to their poor absorption when given orally. Absorption rates vary from >80% for flucytosine, fluconazole, and voriconazole and 70 to 80% for terbinafine to 55% for itraconazole (capsule), 8 to 48% for posaconazole (in animals), and 48 to 74% for ravuconazole (in animals), <10% for amphotericin B, and <0.2% for caspofungin and the other echinocandins (Table 1) (54, 60, 62, 74, 101, 102). The absorption of antifungal agents may be strongly affected by conditions such as overall immunosuppression, hypochlorhydria, and concomitant chemotherapy (58, 60). Absorption may also vary among healthy individuals even under the same dietary conditions (93, 281). Patients with similar underlying conditions and treatment regimens also have demonstrated variable (up to 50% coefficient of variation) pharmacokinetic profiles of orally administered drugs, again underscoring the significance of possible genetic variation in key genes (204). However, there are no studies exploring the role of genetic variation in antifungal absorption.
TABLE 1.
Pharmacokinetic characteristics of antifungal drugs in humans
| Antifungal agent | GI absorption (%) | Distribution (vol, % binding) | Metabolism (%) | Excretion (%)
|
|
|---|---|---|---|---|---|
| Renal | Hepatobiliary | ||||
| Amphotericin B | <10 | 4 liters/kg, 91-95 | Minimal | 20.6 (parent drug) | 42.5 (parent drug) |
| Itraconazole | 55-92 | 11 liters/kg, >99 | >80 (oxidation, deakylation) | <0.03 (parent drug) | 3-18 (parent drug) |
| 35 (metabolites) | 54 (metabolites) | ||||
| Fluconazole | >80 | 0.7 liter/kg, 11-12 | <20 | 80 (parent drug) | Minimal |
| 11 (metabolites) | |||||
| Voriconazole | >90 | 4.6 liters/kg, 58 | >98 (N-oxidation) | <2 (unchanged) | 20 (metabolites) |
| 80 (metabolites) | |||||
| Posaconazole | 8-48 | 5 liters/kg, 98-99 | Minimal (oxidation, glucuronidation) | 14 (mostly metabolites) | 77 (mostly parent drug) |
| Terbinafine | 70-80 | 11 liters/kg, >99 | >99 (N-demethylation, alkyl oxidation, aryl oxidation, hydrolysis) | 80 (metabolites) | 20 (metabolites) |
| Caspofungin | <0.2 | 0.2 liter/kg, 96 | >98.6 (hydrolysis, acetylation) | 1.4 (parent drug) | |
| 41 (metabolites) | 35 (metabolites) | ||||
| Micafungin | Poor | 0.2 liter/kg, 99.8 | >99 (arylsulfation, catechol O-methylation) | 0.7 (unchanged) | |
| 7.4 (mostly metabolites) | >90 (mostly metabolites) | ||||
| Anidulafungin | Poor | 0.6 liter/kg, 84 | >90 (not metabolized enzymatically) | <10 (unchanged) | Minimal |
| >90 (degradation products) | |||||
| Flucytosine | 76-89 | 0.6 liter/kg, <5 | <1 | >90 (parent drug) | Minimal |
| 1 (metabolites) | |||||
Gastrointestinal pH.
Because the optimum site for drug absorption is the upper portion of the small intestine (the duodenum region), intestinal pH is very critical for absorption (232). Gastric pH is also important for drug absorption, because it influences drug solubility (227). Intestinal pH may vary from 6 to 6.5, while gastric pH varies from 1 to 6. In one study, there was a 10-fold difference in gastric pH between individual subjects for the 24-h area under the curve (282). The low pH in the gastric lumen is produced by a unique hydrogen-potassium ATPase located on the apical membranes of the parietal cells of the walls of the secretory unit of the gastric mucosa (Fig. 2) (199).
The pH of the gastrointestinal tract significantly affects the absorption of weakly acidic or basic drugs, such as itraconazole and ketoconazole. Both drugs are ionized at very low pH, while at high pH, they are insoluble, resulting in poor penetration of the gastric epithelium (57, 258). This effect is increased by concomitant administration of drugs that raise the gastric pH, such as H2 receptor antagonists (cimetidine, ranitidine, and famotidine), proton pump inhibitors, sucralfate (a weak-base aluminum salt), and didanosine (a buffer that contains magnesium and aluminum) (2). In contrast, the absorption of compounds such as fluconazole, voriconazole, posaconazole, terbinafine, and flucytosine is barely perturbed by the gastric pH (45, 101, 137, 159); caspofungin and amphotericin B are poorly absorbed from the GI epithelium, possibly due to insolubility problems, but absorption can be improved when lipid-bile salts mixed micelles are used as a vehicle (55). Thus, genetic polymorphisms in key genes which are involved in gastric acid secretion may affect itraconazole and ketoconazole absorption but not the absorption of the other antifungal drugs.
Efflux drug transporters.
Even when a drug crosses the apical membrane of the GI epithelium, efflux drug transporters can pump a compound back out (153). Among the well-known efflux drug transporters located at the apical membrane of the gastrointestinal epithelium are P-gp (ABCB1); multidrug resistance protein 2 (MRP2; ABCC2) and MRP4 (ABCC4); and the breast cancer resistance protein (BCRP; ABCG2) (27). However, efflux drug transporters, such as MRP1 (ABCC1), MRP3 (ABCC3), and MRP5 (ABCC5), are located at the basal membrane and are responsible for pumping substrate drugs into the body, thereby enhancing the ability of drugs to enter the systemic circulation (226) (Fig. 2).
The intestinal P-gp transports a wide spectrum of agents, such as etoposide, cyclosporine, vinblastine, taxol, loperamide, domperidone, ondansteron, indinavir, saquinavir, and nelfinavir (85, 167, 235). The same transporter can limit the absorption of a range of other dugs, such as digoxin, tacrolimus, talinol, and fexofenadine (11). The functions of the MRPs and their pharmacological impacts have been shown in both in vitro and in vivo studies (27, 226), although their roles in drug absorption are not well defined.
Genetic variability, which alters the functions of these drug transporters, may have an impact on the absorption of the substrate drugs. In particular, variable expression on P-gp mRNA and protein levels in the gut have been demonstrated, with an estimated 8- to 10-fold variation (11). Thirty percent of the variability in Cmax and 17% of the variability in oral clearance of cyclosporine in humans can be ascribed to interindividual variation in intestinal P-gp levels (170). The multidrug resistance 1 (MDR1; ABCB1) gene, which encodes P-gp, is located on chromosome 7q21.1. It has been suggested that it acts as a “hydrophobic vacuum cleaner,” or flippase, which removes its substrates from the lipid bilayer before they reach the cytoplasm. A correlation has been observed between MDR1 (ABCB1) T3435C SNP in exon 26 and duodenal P-gp oral-digoxin plasma levels (122).
The transport of antifungal agents by P-gp (ABCB1) is well established (267). Itraconazole (4) and ketoconazole, but not fluconazole, miconazole, and amphotericin B, inhibit P-gp function; in fact, this approach has been undertaken to reverse the anticancer resistance of human leukemia cells in vitro (129). However, antifungal agents could also work as substrates of P-gp, given that P-gp mediates the transport of itraconazole across the blood-brain barrier (BBB) and the similarities between P-gp substrates and CYP3A4 substrates/inhibitors, such as itraconazole, fluconazole, and ketoconazole (130, 187, 195). Furthermore, fluconazole resistance in Candida albicans has been associated with overexpression of C. albicans MDR1, an ortholog of the human ABCB1 gene (276). Additional ABC transporters are involved in the efflux of antifungal agents, including terbinafine, azoles (223), and possibly caspofungin (228).
Thus, P-gp genotypes and expression levels may influence the absorption of antifungal drugs, and particularly that of azoles. However, the roles of P-gp expression and genotype in posaconazole pharmacokinetics were recently explored in 28 healthy black and Caucasian volunteers (R. Courtney, A. Sansone, D. Devlin, P. Soni, and M. Laughlin, Abstr. 44th Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-40, 2004). No association was observed between any MDR1 SNPs, including the C3435T and posaconazole AUCs. Furthermore, no correlation was noted between MDR1 mRNA levels and exposure to posaconazole.
Distribution
Once a drug enters the bloodstream, the drug molecules are distributed throughout the body by systemic circulation and reach the tissues mainly via capillaries (232). Because only free drug diffuses between capillaries and tissue sites, protein binding in plasma has a major impact on distribution, as well as metabolism and elimination, particularly of highly bound drugs (169, 232). Binding to macromolecule components in the blood is also critical for transport; well-defined proteins include albumin, A1-acid glycoprotein (AAG), lipoproteins, immunoglobulins, and erythrocytes (Fig. 2). Thus, genetic variation in one or more these could be critical for differences in antifungal pharmacokinetics.
Plasma protein binding rates for antifungal drugs range from 4% for flucytosine and 11% for fluconazole to 58% for voriconazole and >95% for amphotericin B, itraconazole, posaconazole, terbinafine, caspofungin, and micafungin; moreover, anidulafungin protein binding is as high as 84%, mainly to albumin (Table 1) (45, 58, 60, 63, 102, 244). However, A1-acid glycoprotein and lipoproteins can also contribute to drug binding (20, 30, 174, 218). To a lesser degree, antifungal agents can bind to hemoglobin A1 and free fatty acids (10, 225), as well as on red blood cells (171). For instance, extensive uptake by red blood cells was noted for micafungin (63), while coadministration of caspofungin with tacrolimus reduces whole-blood tacrolimus levels by 20%, possibly due to decreased red blood cell binding of the latter (65). In addition, less than 8% of terbinafine is taken up into blood cells (60). Although substantial variation in plasma proteins can occur in pathological situations, such as diabetes (106), levels of proteins can vary up to 10% among healthy individuals (136). Interindividual variation (5%) in drug-protein binding rates for itraconazole and fluconazole has been observed, with a significant association between the binding of drugs and serum protein levels (8). Plasma protein binding of terbinafine had a major effect on brain uptake in rats, varying from 6% to 45% in the presence of plasma, albumin, and very low- (VLDL) and low-density lipoproteins (LDL), A1-acid glycoprotein, and high-density lipoproteins (HDL) (174). Although several studies have investigated the interaction of antifungals with plasma proteins and the roles of drug transporters in antifungal efflux, the importance of pharmacogenomic issues in the distribution of antifungal agents remains to be explored.
Albumin.
Albumin is able to bind, covalently or reversibly, a large number of both endogenous and exogenous compounds, such as metals, fatty acids, amino acids, and metabolites, such as bilirubin, and drugs (232). Albumin interacts reversibly with a broad spectrum of drugs, primarily anionic drugs, by electrostatic and hydrophobic bonds. It has two high-affinity drug binding sites: site I binds dicarboxylic acid drugs and/or bulky heterocyclic negatively charged molecules, such as warfarin and salicylate, and site II (also called the indol-benzodiazepine site) binds aromatic carboxylic drugs, such as ibuprofen and diazepam (150).
Of the common antifungal agents, ketoconazole (177), itraconazole (8), amphotericin B (20, 109), caspofungin (244), and terbinafine (174, 218) bind to albumin, while fluconazole does not (9, 10). Site II is involved in the binding of both amphotericin B and nystatin, while amphotericin B also binds to site I and nystatin binds to the fatty acid binding sites in albumin (216). However, amphotericin B may also interact with lysine residues 199 and 525 (217). Both polyenes can displace bilirubin, probably at a site shared with site I of albumin. Furthermore, ketoconazole displaces valproic acid, which also binds site I of albumin (56), and itraconazole seems to have a minor effect on the pharmacokinetics of diazepam, which binds to site II of albumin (1). Micafungin has not been demonstrated to exhibit drug interactions with other highly protein bound compounds, such as warfarin, diazepam, salicylic acid, and methotrexate (63). Low serum albumin was associated with a modestly reduced concentration 1 h after dosing, possibly due to reduced protein binding of caspofungin in plasma (J. Stone, G. Winchell, S. Bi, P. Wickersham, M. Schartz, N. Kartsonis, and C. Sable, Abstr. 43rd Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-1571, 2003).
The albumin gene (ALB) is located on chromosome 4q11-q13. More than 50 functional SNPs in the albumin gene have been characterized (83, 175). Functional SNPs that affect the affinity of albumin for drugs have been previously described (149, 260). Conformational changes in the 313-to-365 region of albumin are thought to account for diminished binding, whereas an increase in affinity for binding of warfarin has been found for in vitro recombinant mutants of albumin, such as His242Glu and Lys199Ala, while for Try214Ala and Arg218His a small decrease in affinity was observed (272). The last substitution may also alter the pharmacokinetics of warfarin, since the free-drug concentration in individuals homozygous for Arg218His is expected to be elevated, resulting in a reduction in the serum half-life (201). As most of the antifungal agents are highly protein bound, albumin SNPs may affect antifungal-drug disposition.
A1-acid glycoprotein.
AAG (orosomucoid) is a globulin with a molecular mass of 44 kDa consisting of 59% protein and 41% carbohydrate (133). It is synthesized mainly in the hepatocytes and parenchymal cells and then distributed in body fluids, including plasma (232). The plasma concentration is low (0.4 to 1%) and ranges from 55 to 140 mg/dl among healthy adults. It binds steroids and basic (cationic) drugs, such as propranolol and lidocaine. However, both basic and acidic drugs bind to AAG, although recent studies suggest two separate drug binding sites (133). The binding of drugs may be altered, particularly in pathological states, because of altered sialylation and fucosylation, as well as changes in the glycosylation pattern, increased branching of oligosaccharide chains, and a reduced number of bindings sites.
Although the binding of ketoconazole (177) and itraconazole (10) might not be directly related to circulating AAG levels, an increase in binding of fluconazole is associated with higher levels of AAG (8); some have interpreted this to mean that fluconazole has a higher affinity for AAG than for albumin (9). AAG has been found to contribute to amphotericin B (20) and terbinafine (174) binding. Intracarotid injection of terbinafine together with AAG increased brain uptake in rats eightfold compared to injections of the drug together with plasma (174), indicating that AAG might play a major role in the disposition of the drug.
AAG in human plasma is a heterodimer derived from two separate loci, ORM1 and ORM2 (present in 3:1 molar ratio, respectively), mapped to chromosomal region 9q31-34.3. A total of 74 alleles (27 assigned to ORM1 and the others to ORM2) have been identified (287), using immunoblotting and isoelectric focusing. Genetic variants of AAG have different specificities for binding to particular drugs. For example, dysopyramide, imipramine, and methadone bind selectively to the ORM1*A variant, whereas dypiridamole, quinidine, and mifepristone bind preferentially to the ORM1*F1 variant (133). Particularly for quinidine, the unbound fraction of drug in subjects with the ORM1*F1 phenotype is twice as high as that with the ORM1*S phenotype (166). Furthermore, for drugs that bind to variant A, transport into the brain is significantly lower than for those that bind to both variant A and variant F1/S (138). The effects of SNPs within the AAG gene on the distribution of antifungal agents is not well understood.
Lipoproteins.
Lipoproteins are macromolecular complexes in which hydrophobic molecules of triacylglyceride and cholesteryl ester are enveloped within a monolayer of amphipathic molecules of phospholipids, free cholesterol, and apoproteins (95). Lipoproteins are classified according to their densities as chylomicrons, very-low-density lipoprotein (VLDL), intermediate-density lipoprotein, low-density lipoprotein (LDL), and high-density lipoprotein (HDL).
Although plasma proteins can contribute substantially to binding to antifungal drugs, there is increasing evidence that lipoproteins play a significant role in drug binding (268), particularly to highly lipophilic antifungal drugs, such as terbinafine and amphotericin B. More than 60% of terbinafine is associated with human plasma lipoproteins, particularly LDL (28 to 31%) and HDL (25 to 27%), and less with VLDL (8 to 16%) (286). Binding to lipoproteins affects the brain uptake of terbinafine in rats, where a high in vivo affinity of terbinafine for LDL has been found (174). In the case of amphotericin B, although less than 40% of the drug in plasma is associated with lipoproteins, particularly HDL (142), patients with higher serum LDL-cholesterol levels are more susceptible to amphotericin B-induced kidney toxicity (269), and amphotericin B pharmacokinetics is significantly altered in hypercholesterolemic rabbits (208, 255, 270). The same pattern of lipoprotein binding is observed for nystatin, with 17 to 28% and 3 to 7% of the drug associated with HDL and LDL, respectively (36, 271). However, when the liposomal formulations of the latter drug are used, more than 50% of the drug is recovered in HDL fractions while small or undetectable amounts are in LDL and VLDL (36, 142). Finally, nonesterified fatty acids appear to have joint responsibility for ketoconazole protein binding (177).
Differences in lipoprotein-drug interactions have been observed in select studies (142, 286); these differences appear to be attributable to differences in the lipoprotein lipid and protein concentration/composition plasma profile (268), which can vary by up to 310% (142, 269). In particular, increases in HDL coat lipid content resulted in less amphotericin B recovered in this fraction following incubation with liposomal amphotericin B, whereas an increase in the triglyceride/total-protein ratio resulted in more amphotericin B recovered in the fraction following incubation with free amphotericin B (142). In addition, with decreasing HDL protein, nystatin and liposomal nystatin recovered within the fraction decreased (36). The effect of the lipoprotein concentration on drug pharmacokinetics is indicated by the decreased plasma clearance, kidney concentration, and nephrotoxic effects of amphotericin B when plasma HDL/cholesterol levels are elevated following intravenous administration of triglyceride/fatty acid emulsion to rats. The effect of the lipoprotein composition on drug pharmacokinetics is indicated by the increase in the association of nystatin with plasma lipoproteins when nystatin is incubated in plasma treated with dithionitrobenzoate (an enzyme that inhibits the conversion of free cholesterol to cholesteryl ester, resulting in a decrease of the esterified-cholesterol content within HDL and LDL/VLDL) (268). Lipoproteins can also influence the pharmacodynamics of drugs, such as psychotropic drugs, for which lipoprotein levels have been associated with increased clinical response and remission in psychiatric disorders (67, 71). Therefore, genetic polymorphisms that alter lipid metabolism, such as in dyslipidemias (hypo- and hypercholesterolemia and hypertriglyceridemia), may have a great impact on the pharmacokinetics and toxicity of antifungal drugs.
There are four categories of gene products that contribute to the wide spectrum of interindividual variation in plasma lipoproteins (53). These are the apolipoproteins, namely, apo A-I, A-II, A-IV, B, C-I, C-II, C-III, and E and apo (a); the receptors, namely, LDL receptor (LDLR), LDL receptor-related protein (LRP1), macrophage scavenger receptor (MSR1), VLDL receptor (VLDLR), and SR-B1 receptor (SCARB1) for HDL; modifying proteins, namely, lipoprotein lipase (LP; LPL), hepatic lipase (HL; LIPC), lecithin-cholesterol acyltransferase (LCAT; LCAT), and cholesteryl ester transfer protein (CETP; CETP); and factors involved in lipoprotein synthesis or secretion, namely, microsomal triglyceride transfer protein (MTTP; MTP) and the apo B-editing protein (ACF) (113). Several common functional SNPs in these genes that affect lipoprotein metabolism have been described (Table 2) (91, 113, 146, 262, 283).
TABLE 2.
SNPs affecting lipoprotein metabolisma
| Geneb | SNP name | Position | Nucleotide exchange | Frequency (%) | Effectc |
|---|---|---|---|---|---|
| CETP | 1405V | Exon 14 | G+16A | 32.9 | ↑HDL |
| Taq1B | Intron 1 | G+279A | 41.3 | ↑HDL | |
| LPL | S477X | Exon 9 | C/G | 11 | ↓TG, ↑HDL |
| HindIII | Intron 8 | ↓TG | |||
| APOA-I | M1 site | Promoter (−76) | A/G | ||
| M2 site | Promoter (−83) | C/T | 55.6 | ↓LDL | |
| M2 site | Promoter (−83) | G/A | |||
| APOA-IV | His306Glu | G/T | 7-9 | ↓HDL | |
| APOB | Arg3611Gln | Exon 26 | 11-46 | ↑LDL | |
| Glu4154Lys | Exon 29 | 11-46 | ↑LDL | ||
| Thr→Ileu | Exon 4 | 11-46 | ↑LDL | ||
| APOC3 | Promoter (−455) | T/C | ↓TG | ||
| Nucleotide 1100 | C/T | ↑TG | |||
| SstI | 3′ untranslated region | C/G | 14 | ↑TG | |
| APOE | Cys112Arg | Exon 3 | T/C | 15 | ↑LDL |
| Arg158Cys | Exon 3 | C/T | 2 | ↓LDL | |
| HL | Promoter (−480) | C/T | ↑HDL | ||
| FABP-2 | Ala54Thr | Exon 2 | G/A | 27-29 | ↑FA |
| LDLr | PvuII | Intron 16 | A/G | ↑LDL |
Each of these genes may affect the binding of antifungal drugs to lipoproteins, such as the interaction between CETP and amphotericin B (156). Although the majority of lipoprotein-associated amphotericin B is recovered in the HDL fraction, the percentage of amphotericin B recovered in the LDL fraction is increased when the CETP concentration is increased (268). It has been suggested that the ability of CETP to transfer amphotericin B between HDL and LDL is due to its ability to transfer cholesteryl ester between HDL and LDL, because amphotericin B interacts with free cholesterol and cholesteryl ester (26). It will be interesting to study the roles of SNPs in CETP in amphotericin B pharmacokinetics and toxicity (discussed in “Excretion” below).
Drug transporters.
Although the impacts of intestinal transporters on drug absorption have been discussed above, drug transporters located in the liver and kidney contribute to intestinal, hepatobiliary, and renal excretion and therefore play significant roles in drug elimination (see “Excretion” below). Drug transporters in tissues may also be important in drug distribution. The passage of drugs from the systemic blood into the central nervous system is limited by the presence of the BBB and the blood-cerebrospinal-fluid (CSF) barrier; several transport families are critical for this process, including P-gp (ABCB1), MRPs, organic anion transporting proteins (OATPs), and organic anion transporters (OATs) (248). P-gp (ABCB1) is localized to the apical-luminal side of brain capillary endothelial cells and the apical-CSF side of choroid epithelial cells pumping substrates from inside the cells back into the blood or the CSF, respectively (Fig. 2). The localization of MRP1 (ABCC1) is controversial, because it seems to be expressed in astrocytes rather than in capillary endothelial cells (279). MRP5 (ABCC5) and MRP2 (ABCC2) could play significant roles in the brain and possibly at the BBB (155). However, MRP1, -4, -5, and -6 are expressed in freshly isolated bovine brain capillary endothelial cells, and MRP2 (ABCC2) is localized to the luminal membrane of rat brain capillary endothelial cells (Fig. 2). Rat oatp2, which is expressed on both the luminal and abluminal membranes of brain capillary endothelial cells, is involved in efflux transport from the brain and can account for 40% of the total efflux in rats (155). OAT1 (SLC22A6) and OATP-1 (SLCO1A2) have been demonstrated to be on the brush border apical-CSF side membrane, while rat Oatp2, OAT-3 (SLC22A8), and MRP-1 (ABCC1) are found in the blood-basolateral membrane of choroid epithelial cells. In addition, many drugs are substrates of OAT1 (SLC22A6) and OAT3 (SLC22A3) (248).
Although the impacts of most transporters on drug distribution in the brain are not clearly known, the role of P-gp in the brain distribution of various substrates, including antifungals, has been shown in P-gp knockout mice (11). Accumulation of itraconazole in the brain tissue of P-gp knockout mice is significantly increased compared to that in control mice (187). Furthermore, the brain/plasma itraconazole ratio is significantly increased in the presence of the P-gp inhibitors verapamil and ketoconazole, suggesting that P-gp in the brain capillary endothelial cells participates in a process of active efflux of itraconazole from the brain to the blood at the BBB. In addition, GF-120918 (a P-gp inhibitor) in pretreated mice significantly increased the cerebral itraconazole AUC compared to that of untreated mice infected with Cryptococcus neoformans (130). Preclinical studies indicated that caspofungin is not a substrate of P-gp, although the caspofungin AUC is reduced by 20% with coadministration of rifampin, efavirenz, phenytoin, nevirapine, dexamethasone, and carbamazepamine and increased by 35% with coadministration of cyclosporine (65), compounds which are transported by P-gp and MRPs (226). Penetration of antifungal drugs into the brain is poor for amphotericin B (<4% serum concentration [SC]), itraconazole (<10% SC), ketoconazole (<10% SC), caspofungin (6% SC), and micafungin (<10% SC), but not for flucytosine (74% SC), fluconazole (>60% SC), voriconazole (50% plasma concentration), and terbinafine (6 to 43% plasma concentration; undetectable in CSF) (7, 32, 99, 100, 108, 124, 137, 171). Like itraconazole, drug transporters may be responsible for the poor penetration of antifungal drugs despite their high lipophilicity.
SNPs within the P-gp (ABCB1) gene influence drug distribution in the central nervous system (168) (Fig. 3). Higher maximal digoxin plasma concentrations during steady state are found in the 3435TT group in comparison to subjects with the CC genotype (122), while Sakaeda et al. reported higher AUC from 0 to 4 h (AUC0-4) values in Japanese subjects with the 3435CC genotype compared to CT and TT, in accordance with their own data on ABCB1 mRNA expression (220). Furthermore, the reduced levels of ABCB1 mRNA and P-gp in peripheral mononuclear cells of human immunodeficiency virus-infected patients with the TT genotype is associated with enhanced human immunodeficiency virus protease inhibitor penetration into lymphocytes and finally with a greater rise in the CD4 cell count in comparison to the CT and CC groups (80). However, studies with other P-gp substrates did not reveal an association between the 3435TT genotype and increased drug concentrations. Fexofenadine plasma AUC values were lower in the TT group than in the CC group (144). Nelfinavir plasma concentrations were higher in patients with the 3435CC genotype than in patients with CT and TT genotypes (80), supporting findings that show increased P-gp activity in cells stably transfected with the ABCB1-893Ser variant, mostly linked to 3435T (144). The absence of an association with ABCB1 SNPs could be due to differences in diet, which may contribute to a differential expression of drug transporters or to the coordinate activities of P-gp and CYP3A4 (86). The T3435C SNP of the ABCB1 gene may be associated with tissue levels of antifungal drugs, particularly triazoles, and may explain interindividual differences in antifungal efficacies when plasma levels are similar.
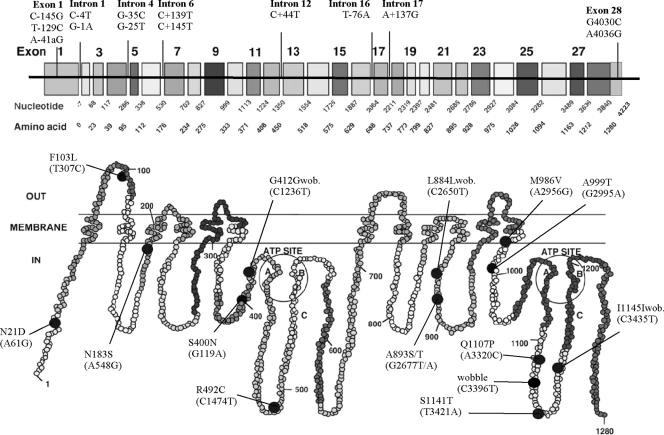
FIG. 3.
Two-dimensional (2D) structure of P-gp showing the distribution of coding SNPs (black-filled circles) (229). The amino acid substitutions are presented, together with nucleotide changes (in parentheses). At the top, 28 exons of the MDR1 (ABCB1) gene are shown with the cDNA nucleotide and amino acid positions, together with noncoding SNPs at the promoter, introns, and untranslated regions. The region of P-gp encoded by a given exon is also highlighted in similar shading on the predicted 2D P-gp structure. The positions of the polymorphisms correspond to the positions of MDR1 (ABCB1) cDNA, with the first base of the ATG start codon set to 1. Mutations located in introns are given as the position downstream (−) or upstream (+) of the respective exon according to the genomic organization of MDR1 (ABCB1) (41). wob., wobble. (Modified from reference 3 by permission from Macmillan Publishers Ltd.)
Additional transporters (Table 3) localize to specific tissues that may in turn influence the extravascular levels of antifungal drugs. Most antifungal drugs are distributed throughout most tissues. Amphotericin B is predominantly distributed to the liver, spleen, bone marrow, kidney, and lung (98), while its lipid formulations are preferentially distributed to organs of the mononuclear phagocytic system, which functionally spares the kidney (117). Fluconazole distributes evenly into virtually all tissue sites and body fluids, including the CSF, brain tissue, and the eye (32). Itraconazole concentrations in nonproteinaceous body fluids are negligible, but tissue concentrations in many organs, including the brain, may exceed corresponding plasma levels by 2 to 10 times (58). Tissue and CSF levels of voriconazole exceed trough plasma levels by severalfold (98). Echinocandins distribute into all major organ sites, including the brain; however, concentrations in uninfected CSF are low (98). Terbinafine is widely distributed in tissues, accumulating in adipose tissue, sebum, skin, hair, and nail plate (60, 101).
TABLE 3.
Human transporter proteins
| Transporter | Gene | Chromosome | Size (aa)a | Tissue distributionb | Membrane localizationc |
|---|---|---|---|---|---|
| P-gp (MDR1) | ABCB1 | 7q21.1 | 1,280 | Ubiquitous | A |
| MRP1 | ABCC1 | 16p13.1 | 1,531 | Ubiquitous (low in L) | BL |
| MRP2 | ABCC2 | 10q24 | 1,545 | L, K, I | A |
| MRP3 | ABCC3 | 17q22 | 1,527 | L, A, P, K, I | BL |
| MRP4 | ABCC4 | 13q32 | 1,325 | Pr, Lu, M, P, T, O, Bl, G | A |
| MRP5 | ABCC5 | 3q27 | 1,437 | Ubiquitous | BL |
| MRP6 | ABCC6 | 16p13.1 | 1,503 | L, K | BL? |
| MRP7 | ABCC10 | 6p21.1 | 1,492 | L, Lu, M | ? |
| BCRP | ABCG2 | 4q22 | 655 | Pl, L, I, Br | A |
| OATP-A | SLCO1A2 | 12 | 670 | B, L | BL |
| OATP-B | SLCO2B1 | 11q13 | 709 | K, L, B, I | BL |
| OATP-C | SLCO1B1 | 12p | 691 | L, Pl | BL |
| OATP-D | SLCO3A1 | 15q26 | 710 | Ubiquitous | ? |
| OATP-E | SLCO4A1 | 20q13.33 | 722 | Ubiquitous | BL? |
| OATP-F | SLCO1C1 | 12p12.3-p14.3 | 712 | B, T | ? |
| OATP8 | SLCO1B3 | 12p12 | 702 | L | BL |
| OATPRP4 | SLCO5A1 | 8q13.1 | 848 | ? | ? |
| OCT1 | SLC22A1 | 6q26 | 554 | L, K (low), I (low) | BL |
| OCT2 | SLC22A2 | 6q26 | 555 | K, B, Pl, I (low), S (low) | BL |
| OCT3 | SLC22A3 | 6q26-q27 | 556 | L, I, H | BL |
| OCTN1 | SLC22A4 | 5q31.1 | 551 | K, L, Lu, I | A |
| OCTN2 | SLC22A5 | 5q31 | 557 | B, K, M, Pr, Pl | A, BL |
| OAT1 | SLC22A6 | 11q13.1-q13.2 | 550 | K | BL |
| OAT2 | SLC22A7 | 6p21.1-p21.2 | 546 | L, K (low) | A |
| OAT3 | SLC22A8 | 11q11 | 542 | K, B (low) | BL |
| OAT4 | SLC22A9/A11 | 11q13.1 | 552 | K, Pl | A |
| OAT5 | SLC22A10 | 11q12.3 | 541 | L | A |
| PEPT1 | SLC15A1 | 13q33-q34 | 708 | K, I, L, Pl | A, BL |
| PEPT2 | SLC15A2 | 3q13.3-q21 | 729 | K, B | A, BL |
| CNT1 | SLC28A1 | 15q25-26 | 649 | K, I, L | A |
| CNT2 | SLC28A2 | 15q15 | 658 | Ubiquitous | A, BL |
aa, amino acids.
L, liver; K, kidney; B, brain; I, intestine; A, adrenals; P, pancreas; Pr, prostate; Pl, placenta; Lu, lung; M, muscle; T, testis; O, ovaries; Bl, bladder; G, gallbladder; S, spleen; H, hippocampus; Br, breast.
BL, basolateral; A, apical/luminal.
Drug transporters show broad specificity because substrate recognition is based on physicochemical properties, such as hydrophobicity, aromaticity, hydrogen binding capacity, and an ionizable character (within a given spatial environment), rather than on defined chemical properties, such as enzyme-substrate or ligand-receptor recognition (257). Azoles are weak bases, with pKas of 1.6 to 2.0 for fluconazole and voriconazole and 2.9 to 3.7 for itraconazole and ketoconazole (24, 57, 179) and 3.6 to 4.6 for posaconazole (45). There is little ionization at higher pH levels compared to their pKas (i.e., in most of the body fluids except gastric juice, where due to low pH, they may have a positive charge). Terbinafine and caspofungin are bases with a predicted pKa of 7.1 (Novartis, Inc., Dorval, Quebec, Canada, Lamisil product insert). Amphotericin B is zwitterionic, because it contains a carboxyl group that can be charged negatively and an amino group that can be charged positively.
P-gp substrates are usually hydrophobic amphipathic organic molecules ranging in mass from 0.2 to 1.9 kDa; they contain aromatic groups, although nonaromatic linear or circular molecules are also transported, and are uncharged or weakly basic, although acidic compounds can also be transported at lower rates (226). The physicochemical properties of azoles resemble the profiles of P-gp substrates. MRP1 to -3 (ABCC1 to -3) substrates include organic amphipathic anions and drugs conjugated to glutathione, glucoronate, or sulfate and might be important for the transport of amphotericin B and metabolites of antifungal drugs. MRP4 (ABCC4) and MRP5 (ABCC5) may function as nucleoside analogue transporters (27, 226) and therefore may play roles in the efflux of flucytosine. OATP substrates are mainly anionic amphipathic molecules with high molecular masses (>450 kDa) that under physiological conditions are bound to proteins (mostly albumin); small hydrophilic compounds with low molecular weights and protein binding are substrates for OATs and organic cation transporters (OCTs) (107). Peptide transporter 1 (PEPT1; SLC15A1) and PEPT2 (SLC15A2) and concentrative nucleoside transporter 1 (CNT1; SLC28A1) and CNT2 (SLC28A2) mediate the uptake of peptide drugs and nucleosides, respectively, and may be important in the disposition of peptide antifungal drugs, possibly echinocandins, which are cyclic hexapeptides.
However, given the high protein binding rates of antifungal agents, the electric charge of antifungal drugs may be less important for transportation across membranes of endothelial cells. Drug uptake from endothelial cells might be associated with (i) a receptor-mediated process for the drug-protein complex, such as albumin uptake from the proximal tubular cells (33); (ii) a conformation change in albumin upon contact with cell surfaces that facilitates the release of ligands (210); or (iii) the presence within the capillary bed of a noncompetitive inhibitor of ligand binding to the plasma protein (44).
Metabolism
Most antifungal agents are metabolized primarily in the liver, although many tissues, such as the gastrointestinal tract, the lungs, the skin, and the kidneys, contribute to elimination. The hepatic biotransformation phase I and II reaction enzymes play important roles in the inactivation and subsequent elimination of drugs that are often not easily cleared through the kidney (232). Frequently, biotransformation results in the formation of a more polar metabolite that is pharmacologically inactive and is eliminated rapidly. Drug metabolism involves two classes of biochemical reactions (Fig. 2): phase I reactions (Table 4), which consist of oxidation (e.g., aromatic hydroxylation; side chain hydroxylation; N-, O-, and S-dealkylation; deamination; sulfoxidation; N-oxidation; and N-hydroxylation), reduction (e.g., azoreduction, nitroreduction, and alcohol dehydrogenase), or hydrolysis (e.g., ester and amine hydrolysis), and phase II reactions, which consist of conjugation with endogenous substances, such as glucuronide, peptide, sulfate, methyl, acetyl, glycyl, or glutathione groups.
TABLE 4.
Major human drug-metabolizing cytochrome P450 enzymesa
| CYP | Chromosome | Expression | Relative protein abundance in liver (%) | % of drugs metabolized by enzyme (antifungal drugs) | Major variant allele(s) | Mutation | Consequence |
|---|---|---|---|---|---|---|---|
| CYP1A1 | 15q22-q24 | Inducible | <1 | CYP1A1*2A&B | 3801T>C I462V | Increased inducibility Increased activity | |
| CYP1A2 | 15q22qter | Inducible | 8-15 | 11 (terbinafine) | CYP1A2*1F | −164C>A | Higher inducibility |
| CYP2A6 | 19q13.2 | Constitutive | 5-12 | 3 | CYP2A6*2 | L160H | Inactive enzyme |
| CYP2A6*4 | Gene deletion | No enzyme | |||||
| CYP2A6*9 | TATA-mut | Less enzyme | |||||
| CYP2B6 | 19q13.2 | Inducible? | 1-5 | 3 | CYP2B6*5 | R487C | Less enzyme |
| CYP2B6*7 | Q172H; K262R; R487C | Less enzyme | |||||
| CYP2C8 | 10q24.1 | Constitutive | 10 | CYP2C8*2 | 1269F | Decreased activity | |
| CYP2C8*3 | R139K, K399R | Decreased activity | |||||
| CYP2C8*4 | 1264M | Decreased activity | |||||
| CYP2C9 | 10q24 | Constitutive | 15-20 | 16 (voriconazole, terbinafine) | CYP2C9*2 | R144C | Reduced affinity for P450 reductase |
| CYP2C9*3 | I359L | Altered substrate specificity | |||||
| CYP2C19 | 10q24.1-q24.3 | Constitutive | <5 | 8 (voriconazole, terbinafine) | CYP2C19*2 | Altered splice site | Inactive enzyme |
| CYP2C19*3 | Stop codon | Inactive enzyme | |||||
| CYP2D6 | 22q13.1 | Constitutive | 2 | 19 | CYP2D6*2xn | Gene duplication | Increased activity |
| CYP2D6*4 | Defective splicing | Inactive enzyme | |||||
| CYP2D6*5 | Gene deletion | No enzyme | |||||
| CYP2D6*6 | 1707T>del P34S | No enzyme | |||||
| CYP2D6*10 | S486T T107I | Unstable enzyme | |||||
| CYP2D6*17 | R296C S486T | Reduced affinity for substrates | |||||
| CYP2E1 | 10q24.3-qter | Constitutive/inducible | 7-11 | 4 | CYP2E1*2 | R76H | Less enzyme expressed |
| CYP2E1*3 | V389I | No effects | |||||
| CYP2E1*4 | V179I | No effects | |||||
| CYP3A4 | 7q21.1 | Constitutive | 30-40 | 36 (itraconazole, ketoconazole, voriconazole, terbinafine) | CYP3A4*2 | S222P | Higher Km for substrate |
| CYP3A4*3 | M445T | Unknown | |||||
| CYP3A4*4 | I118V | Decreased | |||||
| CYP3A4*5 | P218R | Decreased | |||||
| CYP3A4*6 | 831 insA | Decreased | |||||
| CYP3A5 | 7q21.1 | Constitutive | <1 | CYP3A5*3 | Splicing defect | No enzyme | |
| CYP3A5*6 | Splicing defect | No enzyme |
Modified from reference 68 with permission of the publisher and from reference 215 with permission of Elsevier; includes data from http://www.cypalleles.ki.se.
The antifungal drugs terbinafine, itraconazole, voriconazole, ketoconazole, and caspofungin are extensively metabolized (>80% of the dose) (Table 1). The primary pathways of ketoconazole metabolism are oxidative O-dealkylation and aromatic hydroxylation (60). Ketoconazole is a strong inhibitor of CYP3A4, and it has been shown to moderately inhibit CYP2E1, CYP1A2-2c, and CYP2D6 in vitro (2). Voriconazole metabolism involves primarily N-oxidation by CYP2C19, CYP2C9, and CYP3A4 (Table 4), with CYP2C19 being the major metabolic CYP450 isoenzyme (93), although glucuronide conjugates (15% of the dose) are also detected in urine (78). The main metabolic pathways of itraconazole are oxidations and N-dealkylation (116) with CYP3A4, resulting in the formation of several metabolites, including the major metabolite, hydroxyitraconazole. In addition, barbiturates, carbamazepine, phenytoin, and rifampin, known CYP3A4 inducers, accelerate the metabolism of ketoconazole, itraconazole, and miconazole, and, to a lesser extent, fluconazole (2); antiretroviral protease inhibitors, such as ritonavir, are CYP3A4 substrates and reduce the clearance of itraconazole in pediatric patients (103). Particularly for fluconazole, coadministration with rifampin decreased the AUC and half-life of the antifungal (2).
At least seven CYP enzymes (Table 4), which represent four major pathways (60), are involved in terbinafine metabolism: N-demethylation, primarily mediated by CYP2C9, CYP2C8, and CYP1A2; deamination by CYP3A4; alkyl side chain oxidation by CYP2C9, CYP2C8, CYP2C19, and CYP1A2; and dihydrodiol formation by CYP2C9 and CYP1A2 (261), resulting in 15 metabolites. Caspofungin is slowly metabolized by peptide hydrolysis and N-acetylation (16, 102). Caspofungin does not influence the plasma pharmacokinetics of indinavir, a substrate and inhibitor of CYP3A4, nor of ketoconazole, a potent CYP3A4 inhibitor (102). Posaconazole is minimally metabolized by both the CYP450 and uridine diphosphateglucuronotransferase (UGT1A4) (94, 151). Although posaconazole is not a major substrate of CYP3A4, it is an inhibitor of this important drug-metabolizing enzyme. Finally, micafungin is metabolized by aryl sulfatases with further metabolism by catechol O-methyl transferases, while some products undergo hydroxylation by phase I drug-metabolizing enzymes (111).
Population differences in drug metabolism are clearly associated with phenotypic classification of patients in the categories of poor, intermediate, extensive, and ultrarapid extensive metabolizers (215). Patients who express dysfunctional or inactive drug-metabolizing enzymes are considered poor metabolizers and are at high risk for toxicity and perhaps poor treatment outcome (197). Intermediate metabolizers, with decreased drug-metabolizing enzyme activity, differ in outcomes from extensive metabolizers, who have normal drug-metabolizing enzyme activity (the anticipated medication response would be seen with standard doses). Ultrarapid extensive metabolizers have increased drug-metabolizing enzyme activity, usually due to larger quantities of expressed drug-metabolizing enzymes (215). Many genetic polymorphisms in drug-metabolizing enzymes, which produce enzyme products with abolished, reduced, altered, or increased enzyme activities, have been associated with the aforementioned phenotypic polymorphisms. There are few studies in which the roles of genetic polymorphisms of drug-metabolizing enzymes in antifungal-drug metabolism have been investigated.
Phase I reactions.
Both members of the CYP1A family, CYP1A1 and CYP1A2, have major roles in the biotransformation of a variety of xenobiotics, including a number that may be commonly encountered in food and environmental pollutants, such as tobacco and procarcinogens. Thus, genetic polymorphisms in these genes have been associated with susceptibility to cancer, particularly lung cancer (51). Unlike CYP1A1, which is extrahepatic, CYP1A2 is expressed in the liver and has an additional role in the metabolism of commonly prescribed drugs, including the antipsychotics clozapamine and olanzapamine, and participates in the oxidation of paracetamol and theophylline (110). Both are induced by a range of compounds via the nuclear aryl hydrocarbon receptor (51). Terbinafine is metabolized by CYP1A1, while ketoconazole is a strong inhibitor of the family. CYP2A6 has a limited range of specific xenobiotic substrates, such as nicotine, coumarin, and the drug SM-12502, but there are a number of other substrates that are also metabolized by additional CYPs, including halothane, several nitrosamines, and disulfiram (209). At least 16 distinct CYP2A6 alleles have been described (http://www.cypalleles.ki.se), some of which are population specific. For example, the major variant CYP2A6*4, with a frequency of 20% in the Pacific Rim, is rare in European Caucasians (51). CYP2B6 has a role in the biotransformation of cyclophosphamide, bupropion, and various nitrosamines, although its importance in drug metabolism is recognized when its expression is induced by exposure to phenobarbital-type inducers (73). Nine common alleles have been described for CYP2B6; alleles *5 and *7 together have a frequency of approximately 14% in Europeans and are functionally associated with decreased enzyme activity (158).
The CYP2C family consists of four homologous genes, CYP2C8, CYP2C9, CYP2C18, and CYP2C19, on chromosome 10 but with distinctive substrate specificities. Voriconazole and terbinafine are metabolized by members of this family. Substrates of CYP2C8 include paclitalex, all-trans retinoic acid, cerivastatin, rosiglitazone, and amodiaquine (96). The variant alleles, *2 (I269F), *3 (R139K, K399R), and *4 (I264M) (Table 4), are associated with decreased activity of paclitaxel in human liver microsomes (14), while in vitro the variant P404A is less effective in N-deethylation of amiodarone (238), as well as in paclitaxel metabolism (239). CYP2C9 has a major role in the metabolism of S-warfarin, phenytoin, tolbutamide, and nonsteroidal anti-inflammatory drugs (162). Eleven alleles have been described for CYP2C9, 10 of which are nonsynonymous base substitutions and base deletions (http://www.cypalleles.ki.se). The major variant alleles are *2 (R144C) and *3 (I359L), which are associated with impaired enzyme activity. Individuals expressing either of these two alleles have reduced warfarin clearance and thus altered daily dose requirements, increased phenytoin serum concentrations, increased half-life of tolbutamide, <1% conversion of a losartan dose to its pharmacologically active metabolite E3174, profound symptoms of hypoglycemia after a glipizide dose, and complications from bleeding after warfarin administration (162, 215).
CYP2C19 is responsible for the metabolism of proton pump inhibitors (e.g., omeprazole), anticonvulsants and hypnosedatives (e.g., diazepam), anti-infectives (e.g., proguanil), and antidepressants (66). Alleles *2 (splicing defect in exon 5) and *3 (stop codon in exon 4) are the most frequent (Table 4) and have been associated with better response to omeprazole treatment of peptic ulcer due to higher drug levels (88) and prolonged sedation after diazepam therapy due to increased half-life of diazepam (22). In addition, poor, intermediate, and rapid CYP2C19 metabolizers respond at rates of 100%, 60%, and 28.6%, respectively (88), while addition of clarithromycin increased Helicobacter pylori eradication in the last two groups but had little effect in poor metabolizers (6).
CYP2D6 metabolizes antidepressants, antipsychotics, beta-blockers, and antiarrhythmics (172). Forty-two alleles have been described as nonsynonymous SNPs, frameshifts, and splicing defects (Table 4). Intermediate metabolizers may be either heterozygous for one of the inactivating mutations or homozygous for alleles associated with impaired metabolism, while ultrarapid metabolizers may have up to 13 copies of a tandem repeat in CYP2D6, although the ultrarapid phenotype is more commonly associated with single-gene duplication (51). In poor metabolizers, codeine is an ineffective analgesic due to inadequate conversion to morphine by CYP2D6 (200). Poor metabolizers may experience increased adverse effects from the antiarrhythmic propafenone, because of elevated concentration (42), and from tricyclic antidepressants, while low plasma levels and rapid clearance of the latter are observed for ultrarapid metabolizers (23). Finally, ethanol-inducible CYP2E1 metabolizes low-molecular-weight compounds, such acetone, ethanol, benzene, and nitrosamines, while paracetamol, halothane, and enflurane are also substrates (51). Ketoconazole may potentially inhibit CYP2E1 and CYP2D6, resulting in dose-dependent adverse reactions. Most of the genetic polymorphisms identified lie in upstream sequences or in introns, but of the three nonsynonymous SNPs described, only one (R76H) has been associated with decreased enzyme activity (125).
CYP3A isoenzymes are the predominant subfamily of drug-metabolizing enzymes with the widest range of drug substrates; they are primarily expressed in the liver and intestine. Itraconazole, voriconazole, terbinafine, and possibly ketoconazole are metabolized by CYP3A enzymes. CYP3A activity is the sum of the activities of four CYP3A isoenzymes: CYP3A4, CYP3A5, CYP3A7, and CYP3A43 (157). Levels of CYP3A4 activity vary considerably in individuals, while CYP3A5 is expressed in 10 to 20% of adult livers and CYP3A7 is universally expressed in the fetal liver and in some adult livers (51). Eighteen alleles of CYP3A4, many nonsynonymous SNPs, have been identified, but some give rise to alterations in catalytic activity and most are too rare to explain the interindividual variation in CYP3A4 activity (157). Polymorphisms in one of its transcriptional regulators, pregnane X receptor, may affect levels of CYP3A4 (51). Seven alleles of CYP3A5 have been identified (Table 4), with the majority of them resulting in absence of CYP3A5 expression due to abnormal splicing or nonsense SNPs (157). Several genetic polymorphisms have been found in the promoter region of CYP3A7 associated with CYP3A7 mRNA expression in the adult liver (154), while alternative splicing events have been found in CYP3A43, which resulted in production of a CYP3A4-CYP3A43 hybrid (81).
Because the CYP system is involved in biotransformation of antifungal agents, genetic polymorphisms in CYP genes may play significant roles in the pharmacokinetics of antifungal drugs. However, despite the extensive body of literature available addressing SNPs in the CYP family, only CYP2C19 has been studied in voriconazole (128). Analysis in healthy-volunteer data has demonstrated that the CYP2C19*2 genotype is the most important covariate determining plasma levels of voriconazole (78). The mean average plasma concentrations of voriconazole in homozygous extensive metabolizers are four times lower than in homozygous poor metabolizers, while the heterozygous individuals have intermediate levels (Fig. 4).
FIG. 4.
Influence of the CYP2C19 (allele *2) genotype on average steady-state plasma voriconazole concentrations as determined by a population pharmacokinetics analysis. The box-and-whisker plots display the box locations of the median, upper, and lower quartiles, with whiskers extending to the furthest data point within 1.5 times the interquartile range. The scatter of individual data is also displayed. (Reprinted from reference 78).
Phase II reactions.
Glutathione conjugation is an important metabolic pathway for detoxification of hydrophobic and electrophilic drugs and is performed by the class of glutathione S-transferases. They are encoded by eight distinct classes of genes: alpha, kappa, mu, omega, pi, sigma, theta, and zeta. Genetic polymorphisms in GSTM1 and GSTT1 result in decreased catalytic activity (278), and large-scale gene deletion is associated with absent enzyme activity (230). Although genetic polymorphisms have also been described for GSTM3, GSTP1, and GSTA1, their roles in the pharmacogenomics of chemotherapeutic outcomes are unclear (51).
Acetylation of amino, hydroxyl, and sulfhydryl groups is performed by the enzyme N-acetyltransferase, of which there are two isoforms, NAT-1 and NAT-2. NAT enzymes may be involved in caspofungin metabolism. Multiple alleles have been described for NAT1 (114) and selected variants. NAT1*14 (R187Q), -*15 (R187Stop), -*17 (R64W), -*19 (R33Stop), and -*22 (D251V) are associated with absent or low enzyme activity (115), although interindividual variation in NAT-1 levels has been reported with 4-aminobenzoic acid (48), and low-activity alleles are probably rare (51). Nonsynonymous SNPs with functional consequences, which result in absence of catalytic activity in vitro, have been described for NAT2 (114); three variant alleles, NAT2*5 (I114T), NAT2*6 (R197Q), and NAT2*7 (G286E), account for the majority of the slow acetylators among Caucasians (51). NAT2 polymorphisms correlated with adverse effects with isoniazide, dapsone, and sulfoniazide (240). The population frequency of the slow-acetylator phenotype varies from 40 to 70% of Caucasians and African-Americans and more than 80% of Egyptians to 10 to 20% of Japanese and Canadian Eskimos (172).
Methylation reactions using S-adenosylmethionine for a methyl group donor are important in the metabolism of endogenous substances and xenobiotics; at least four separate enzymes can carry out S-, N-, and O-methylation reactions (274). Thiopurine S-methyltransferase (TPMT) is an enzyme that metabolizes thiopurine drugs, such as mercaptopurine, used clinically as immunosuppressants. In addition, TPMT deficiency is associated with increased risk for therapy-limiting toxicity and second malignancies in patients with acute lymphoblastic anemia treated with 6-mercaptopurine. The most common defective allele, TPMT*3, is associated with two amino acid substitutions that result in complete absence of activity (182). Catechol-O-methyltransferase (COMT) is an enzyme present in mammalian cells as both membrane bound (MB) and soluble (S) cytosolic forms and plays an important role in the metabolism of catecholamine transmitters and catechol drugs used to treat hypertension, asthma, and Parkinson's disease (275). COMT enzymes may be involved in micafungin biotransformation. Family studies of red blood cell COMT activity show a bimodal frequency distribution with the trait of low-level COMT activity being associated with decreased enzyme thermal stability associated with an SNP at codon 108 in S-COMT (158 in MB-COMT) (233).
Other phase II drug-metabolizing enzymes are UDP-glucuronotransferases encoded by the UGT family of genes and sulfotransferases encoded by the SULT family of genes. A TA insertion in the TATA box and specific nonsynonymous SNPs results in decreased expression of UGT1A1, the gene encoding the main enzyme responsible for glucuronidation of bilirubin; these variants are associated with decreased clearance of a number of different drugs, including tolbutamide, paracetamol, and rifampin (105). SNPs in other UGT genes may alter the kinetics of some substrates. Genetic polymorphisms that might be functionally significant have also been described for SULT genes (191).
The roles of SNPs of phase II drug-metabolizing enzymes in the pharmacokinetics of antifungal drugs, and in particular for caspofungin, micafungin, and posaconazole, remain to be explored. Preliminary information points to population-based differences in the metabolism of posaconazole, perhaps by genetic variation in the family of UGT genes (R. Courtney, A. Sansone, B. Kantesaria, P. Soni, and M. Laughlin, Abstr. 43rd Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-1564, 2003). The roles of SNPs in the COMT gene in micafungin metabolism are unknown.
Excretion
Drug metabolites can be excreted by the hepatobiliary system or by the kidneys via the urine (232). Other pathways for drug excretion include the saliva, gut, milk, sweat, and tears or via the lungs into expired air. Among antifungal drugs, flucytosine (259) and fluconazole (32) are primarily (>90% of a given dose) excreted unchanged in the urine; interestingly, for fluconazole, 80% is the parent drug and 11% is in the form of known metabolites (Table 1). Fluconazole can be detected in saliva (32) and in breast milk (61) at levels comparable to those in plasma and in sweat (levels in sweat can be 2.5 times higher than those in plasma) (280) following oral administration. Amphotericin B is excreted unchanged through the kidney and bile, with 90% of the dose detected in urine (20.6%) and feces (42.5%), amounting to 75% of the total clearance (19). Unchanged itraconazole is mainly excreted from bile, since 3 to 18% of the dose is detected in the feces and no drug is detected in the urine (58); 35% of the metabolized form of itraconazole is secreted in urine and 54% in feces (60). Itraconazole is also detected in sweat at levels lower than those in plasma (38) and in saliva at levels higher than those in plasma (211) after oral administration. In the case of voriconazole, less than 5% of the drug is excreted unchanged in the urine (137), while 80% of the original dose is excreted in the urine and 20% in the feces (93). Voriconazole can be detected in saliva at levels half those detected in plasma (206). The primary excretion route of posaconazole in rats is the bile, since more 70% of the intravenous dose is detected in feces and bile while the remainder is found in the GI tract and only 7% in urine (120). Overall, biliary excretion is also the major route of elimination in humans, since the majority of the radioactivity (77%) is excreted into the feces as the parent drug while the urine contains minor amounts (14%) of posaconazole and its metabolites (151).
Caspofungin is excreted in urine and feces, accounting for 40.4% and 34.4% of the dose, respectively, with the unchanged form comprising 9% of urinary extracts (16); these data confirm animal studies, in which <1 to 3% of the total dose was recovered in urine (108). Vechinocandin, a semisynthetic echinocandin B derivative, is detected in rabbit saliva at levels approximately 1% of those in plasma, whereas fluconazole and amphotericin B are not detectable (202). Urinary excretion of anidulafungin is negligible, while fecal excretion accounts for the entire dose as intact anidulafungin (<10%) and tertiary degradation products (>90% of the dose) (69). For micafungin, 7.4% and 43.8% are recovered in urine and feces at 168 h postdose, while the parent drug is not detectable in plasma after 72 h (87). Terbinafine is excreted at 80% in metabolized form in the urine and 20% in feces (60); 2 to 4% of ketoconazole is excreted unchanged, mainly through the bile (60), and less than 1% in the urine (171). Terbinafine is not detected in sweat (76), while ketoconazole is detected in sweat (212), in breast milk (189), and in saliva (82). There are no studies exploring the pharmacogenomic aspects of antifungal-drug excretion.
Renal excretion.
Many drugs are excreted via the kidneys by one of several mechanisms, glomerular filtration, active tubular secretion, or endocytosis; however, tubular reabsorption can limit renal excretion (178). Up to 20% of the renal plasma flow is filtered through the glomerulus, where drug molecules and their metabolites are passively diffused into the glomerular filtrate due to high hydrostatic pressure within the glomerular capillaries. Drug molecules of low molecular weight and high lipophilicity diffuse more easily. The remaining 80% of the delivered drug passes through the peritubular capillaries of the tubule, where drug molecules and their metabolites can be transported to the tubular lumen and vice versa by two independent carrier systems (Fig. 2); the organic anion transport system, which is selective for acidic drugs (substrates with carbonyl and carboxyl groups) and involves, among others, the OAT1 (SLC22A6), OAT3 (SLC22A8), MRP1 (ABCC1), MRP3-6 (ABCC3-6), sodium dicarboxylate transporter 2 (SDCT2; SLC13A3), and sulfate anion transporter 1 (SAT1; SLC26A1), located in the basolateral membrane; rat Oatp1 (slc21a1), Oatp3 (slco1a5), Oatk-1, and Oatk-2 or human OAT4 (SLC22A11) and MRP2 (ABCC4), located in the luminal membrane; and the OCT system, which is selective for basic drugs (secondary and tertiary amines and quaternary ammonium salts) and involves OCT2 (SLC22A2), located in the basolateral membrane, and OCTN1 (SLC22A4), the carnitine transporter OCTN2 (SLC22A5), and P-gp (ABCB1), located in the luminal membrane (256). However, in contrast with P-gp (ABCB1), their specific activities in the overall handling of drugs are not yet well defined (178).
Unlike glomerular filtration, carrier-mediated transport can eliminate drugs even when they are bound to plasma proteins. Drugs with high lipid solubility may be reabsorbed mainly by passive diffusion across the renal tubule, although carrier-mediated tubular reabsorption has been reported. Reabsorption can be affected by the urine flow rate and urine pH if the drug is a weak acid or base. Finally, endocytosis has also been reported to be involved in the uptake of drugs such as aminoglycosides, because they bind to phospholipids in the brush border membrane (178).
Renal excretion is the primary excretion route for fluconazole and flucytosine (Table 1). Glomerular filtration is the mechanism of excretion for flucytosine (259) and fluconazole (32). Flucytosine is neither reabsorbed nor secreted via the tubular epithelium (259). By comparison, fluconazole is extensively reabsorbed (approximately 80%) from the tubular lumen (61, 135). Tubular reabsorption is important for amphotericin B (77), because urinary clearance is approximately 4% of the glomerular filtration rate (19). However, for both drugs, urine concentrations are much higher than those in blood (19, 32), and tubular reabsorption might occur as passive back diffusion rather than a carrier-mediated process. Nevertheless, if the main mechanism of transport of antifungal compounds through the renal membranes is passive diffusion, genetic polymorphisms in genes encoding drug transporters located in tubular cells would likely have a small impact on the renal clearance of current antifungal drugs.
Hepatobiliary excretion.
Hepatobiliary excretion involves the uptake of drugs from blood into the hepatocyte through the sinusoidal (basolateral) membrane by passive diffusion or carrier-mediated transport. Transfer of drugs to the biliary canalicular membrane is mediated by intracellular transfer proteins and passive diffusion, but excretion at the canalicular membrane is mediated mainly by carrier proteins (Fig. 2) (11, 39). Members of the OATP transporters, such as OATP-A (SLCO1A2), -B (SLCO2B1), -C (SLCO1B1), and -8 (SLCO1B3), have been shown to be located on the sinusoidal membrane (Table 3) and to be responsible for the transport of many drugs, including pravastatin, benzylpenicillin, digoxin, and fexofenadine (143). It is believed that OATP-C (SLCO1B1) and OATP-8 (SLCO1B3) transport acidic compounds, whereas OATP-A (SLCO1A2) and -B (SLCO2B1) transport basic, zwitterionic, and neutral compounds. OCT1 (SLC22A1), -2 (SLC22A2), and -3 (SLC22A3) are also found in the sinusoidal membrane (288), although their roles in the hepatic uptake of drugs are not clear. Substrates of OCT proteins are small organic cations, such as TEA and N-methylnicotinamide (25). The OAT2 (SLC22A2) and OAT3 (SLC22A3) proteins are expressed in the liver, and although active renal excretion of substrates such as cimetidine, methotrexate, cidofovir, and adefovir substrates have been shown (11, 155), their roles in hepatobiliary excretion remain to be elucidated. P-gp (ABCB1) and MRP2 (ABCC2) are located in the canalicular membrane and are involved in the active secretion of drug into bile (11).
MRP1 (ABCC1) is also localized in the lateral membrane and mediates transport of anticancer drugs, as well as anionic conjugates, with glutathione, sulfate, or glucuronide (11). P-gp (ABCB1) is one of the major cation carriers responsible for the biliary excretion of amphiphilic drugs (186, 236, 237). MRP2 (ABCC2) has been shown to mediate the transport of endobiotics, such as bilirubin, as well as many anionic drugs, such as grepafloxacin, pravastatin, cefodizime, methotrexate, and irinotecan, and drug conjugates, such as glucuronide conjugates (11). In the livers of patients whose MRP2 (ABCC2) function is deficient, the expression of MRP3 (ABCC3) is localized on the sinusoidal membrane of human hepatocytes and is upregulated (147). This mechanism for protection of the hepatocytes from drug and endobiotic exposure operates by pumping the drugs out of the hepatocytes into the blood (27).
For antifungal agents, hepatobiliary excretion is the main route of elimination. In particular, amphotericin B and posaconazole, and to lesser degrees itraconazole and ketoconazole, are excreted directly. Fluconazole is also excreted into the bile, since the drug is detected in bile at levels equal to those in the blood (29).
Very little is known about the hepatic transporters involved in biliary excretion of antifungal agents. In guinea pigs, itraconazole interacts with P-gp to reduce digoxin excretion in bile (196). In addition, the combination of itraconazole and verapamil (P-gp substrates) is reported to have caused a severe and slowly reversible cholestasis in a 74-year-old woman (250). Hepatobiliary excretion of fluconazole might not be regulated by P-gp, given that cyclosporine A, a P-gp inhibitor, did not affect the blood/bile ratio of fluconazole when coadministered in rats (161). Interaction between caspofungin and rifampin results in elevated exposure to both drugs, probably because of delayed biliary excretion (63). Posaconazole is usually (>77%) excreted via the hepatobiliary system as intact drug, but an increase in posaconazole clearance by P-gp inducers, such as phenytoin and rifabutin (5), suggests that P-gp is involved in posaconazole excretion. The liver-specific transporter OATP1B1 (SC21A6) is involved in hepatic uptake of caspofungin (222).
Genetic polymorphisms in genes encoding hepatic transporters can alter the hepatobiliary excretion of drugs. A cogent example of impaired biliary excretion due to altered function of a hepatic transporter is the Dubin-Johnson syndrome, an autosomal recessive disorder attributed to the absence of MRP2 (ABCC2) at the canalicular membrane; patients with this syndrome exhibit hyperbilirubinemia due to impaired biliary excretion of bilirubin conjugates (139). The absence of MRP2 (ABCC2) is due to the deletion of six nucleotides, encoding Arg at 1392 and Met at 1393 (141), as well as to I1173F and R1150H substitutions (188). SNP analysis of MRP2 (ABCC2) in Japanese subjects identified more than 30 SNPs, including C24T (untranslated region), G1249A (exon 10) associated with Val417Ile, and C3972T (exon 28) (249). Up to a 15-fold difference in the expression level of MRP2 (ABCC2) mRNA was observed in 13 patients undergoing resection of liver metastasis (289) and in 18 hepatitis patients (118). In addition to food and drugs that induce MRP2 (ABCC2) expression, it has been suggested that the CAAT enhancer binding protein beta binding sequence located between −356 and −343 and hepatic nuclear factor 1 binding and upstream stimulatory factor-like elements located between +81 and +248 may also be important in the basal expression of human MRP2 (ABCC2) (249).
At least 14 nonsynonymous SNPs in OATP-C (SLCO1B1) have been identified (252). Overall, functional assessment of 16 OATP-C (SLCO1B1) alleles in vitro revealed that selected variants exhibited markedly reduced uptake of the OATP-C (SLCO1B1) substrates estrone, sulfate, and estradiol 17-β-d-glucuronide. Specifically, alterations in transport were associated with SNPs that introduced amino acid changes within the transmembrane-spanning domains (T217C [Phe73Leu], T245C [Val82Ala], T521C [Val174Ala], and T1058C [Ile353Thr]) and also with those that modified extracellular loop 5 (A1294G [Asn432Asp], A1385G [Asp462Gly], and A1463C [Gly488Ala]) (252). In the case of OAT-B, the nonsynonymous SNP S486F affects [(3)H]estrone-3-sulfate uptake from embryonic kidney cells (198). Eight nonsynonymous SNPs in OCT2 (SLC22A2) have been identified in ethnically diverse DNA samples, four of which (M165I, A270S, R400C, and K432Q) occurred with frequencies higher than 1% and altered transporter function in Xenopus laevis oocytes for metformin, phenformin, procainamide, and quinidine (160). Genetic polymorphisms in the MDR1 (ABCB1) gene and their roles in pharmacokinetics have been identified, although their impacts, particularly on hepatobiliary excretion, remain to be elucidated (168, 229). Whether genetic polymorphisms in hepatic drug transporters alter hepatobiliary excretion of antifungal drugs is unknown.
OTHER FACTORS THAT AFFECT PHARMACOKINETICS OF ANTIFUNGAL DRUGS
Although genetic polymorphisms may help us to partially explain interindividual variability in the pharmacokinetics of antifungal drugs and response, additional factors can influence drug levels; these include physiological, pathophysiological, and environmental changes. It is likely that genomics can provide partial predictive value, though the degree will vary according to individual circumstances; some have argued that genetics accounts for as much as 50% of response or toxicity, while estimates by other are substantially lower (132).
Age
The process of aging is particularly important in drug disposition (112, 140). For instance, drug absorption is different in children because of higher intragastric pH, the increased gastric emptying and propagating contractions, the developing intestinal surface, and the age-associated changes in splanchnic blood flow in the neonatal period. The distributions of drugs are markedly different in neonates and young infants than in adults; factors include larger extracellular and total-body water spaces; a higher water-to-lipid ratio in adipose stores; reduction in the quantity of total plasma proteins; the presence of fetal albumin, which has reduced binding affinity for weak acids; the increase in endogenous substances, e.g., bilirubin and free fatty acids, capable of displacing a drug from albumin binding sites; variability in regional splanchnic blood flow; organ perfusion; permeability of cell membranes; changes in acid-base balance; and more dynamic cardiac output (72, 234). For instance, P-gp and phase I and II drug-metabolizing enzyme expression appears to be different in neonates than in adults (140). Finally, pharmacokinetics may also be different in elderly individuals (284) due to differences in absorption (increased gastric pH and decreased absorptive surface, splanchnic blood flow, and gastrointestinal motility), distribution (decreased cardiac output, total-body water, lean body mass, and plasma albumin and increased AAG and body fat), metabolism (decreased hepatic mass, enzyme activity, and hepatic blood flow), and excretion (decreased renal blood flow, glomerular filtration rate, and tubular secretion) (112).
There are sentinel examples of the influence of age on the pharmacokinetics of antifungal drugs (60). A significant negative correlation between the mean blood concentration of ketoconazole and age has been reported (185). Terbinafine AUC values are significantly higher in children than in young adults (194), although in a separate study, higher plasma concentrations and lower half-lives of the terminal elimination phase were reported (127). For fluconazole, the volume of distribution is greater in neonates and decreases in young adults (31), the mean plasma half-life in children (22 h) is shorter than in adults (37 h) (59), and total clearance is greater in children (1.16 liters/h) than in adults (1.07 liters/h) (163). In addition, the half-life of azole is slightly prolonged in elderly people compared to the middle aged (224) and terbinafine AUC values are higher in the elderly than in young adults (193). Pharmacokinetics of itraconazole in elderly (116) and pediatric patients do not appear to be different (103); lower plasma concentrations in children and longer half times in elderly individuals have been observed in preliminary studies (58, 116). The pharmacokinetics of terbinafine are similar in elderly and young subjects (134). Neonates and children have lower Cmax values (134), higher clearances, and longer serum half-lives of amphotericin B than older children (21, 242, 266). In neonates, the pharmacokinetics of flucytosine are as follows: slightly increased half-lives, decreased body clearance, and greater volume of distribution than in adults (17). The Cmax and AUC of voriconazole in elderly males were 61% and 86% higher, respectively, than in young males, a difference that, interestingly, is not observed in females (78). Compared with the young control subjects, the elderly subjects had higher mean caspofungin concentrations, 26% longer mean half-lives, and 28% mean increase in AUC (244). The mean clearance and volume values of micafungin are 33% and 26%, respectively, greater in the pediatric population than in the adult population, while no significant differences in AUC, elimination half-life, distribution volume, plasma protein binding ratio, or total clearance have been found between elderly and nonelderly subjects (87).
Gender
Gender is yet another factor that could contribute to interindividual variability in drug pharmacokinetics (18). Oral absorption might be different in men and women, since women empty solids from the stomach more slowly and have higher gastric pH, and the efficacy of stomach alcohol dehydrogenase is lower in women than in men (285). In the case of drug distribution, although the concentration of albumin is largely unaffected by gender (18), the concentrations of AAG and various lipoproteins are slightly lower in women as a result of a decrease induced by endogenous estrogen (145). Although this difference may not be important for drugs that are loosely bound to plasma proteins (285), it may have a great impact on pharmacokinetics, particularly for highly protein binding drugs, such as the common antifungals. Furthermore, the activities of efflux transporters and drug-metabolizing enzymes are different in men and women. Regarding drug excretion, gender might also have some influence on tubular secretion, since the clearance of amantadine, an organic anion secreted by the kidney, is lower in women than in men and the elimination of amantadine is inhibited by quinine and quinidine in men but not in women (92).
Gender does not appear to influence fluconazole pharmacokinetics (49), and amphotericin B nephrotoxicity is not related to gender (243). Although terbinafine overall is as effective as itraconazole for treating toenail onychomycosis, stratification analysis according to age and gender reveals that terbinafine treatment is superior to itraconazole for females and patients 55 years old and older (43). Furthermore, there is no significant influence of gender on treatment results for patients with onychomycosis treated with oral itraconazole (119). The Cmax and AUC of voriconazole in young males were 83% and 113% higher, respectively, than in young females (a difference, however, which is not observed in elderly individuals), and children have higher elimination capacity than adults on a body weight basis (78). Plasma concentrations of caspofungin are similar in men and women, but women have a mean increase in AUC of 22% over men (244). Gender has been found to influence clearance of anidulafungin (69).
Physiological Factors
Physiological factors, such as body size and composition, gastrointestinal physiology, hepatic status, and renal excretion, as well as other physiological processes involved in drug disposition, may also influence the pharmacokinetics of drugs (184). Many of the pharmacokinetic differences between men and women can be of physiological origin. For example, females generally have a lower body weight and thus smaller organ size and lower blood flow. Women also have a higher percentage of body fat (48% versus 36% in the elderly and 33% versus 18% in adults) (97), which results in a greater volume of distribution and in a decreased plasma concentration and a prolonged half-life of lipophilic drugs, such as diazepam and trazodone (285). Gastric acid secretion has been reported to be lower in women than in men, probably due to reduced gastric emptying time (203). Lastly, the glomerular filtration rate is known to be proportional to body weight, and thus, body weight might play an important role in the clearance of drugs that are eliminated from the kidneys (184).
Body weight influences the pharmacokinetics of fluconazole, since a positive correlation has been found between clearance and volume of distribution and body weight (49). Higher AUC values for voriconazole are obtained with subjects who weigh less (78). Weight has been found to be a statistically significant determinant of caspofungin pharmacokinetics, since plasma concentrations are greater in patients with lower body weights (265). Body habitus probably influences the pharmacokinetics of anidulafungin, since the clearance and volume of distribution increases with increasing body weight (69). Obesity shifts the pharmacokinetic profile of amphotericin B; in a hyperlipidemic rat model, obese animals had a twofold-increased AUC and a lower weight-corrected volume of distribution and total body clearance than lean rats (255).
Pathological Conditions
In pathological processes, such as renal or hepatic insufficiency, the pharmacokinetics of antifungal compounds can be changed, leading to toxicity or decreased efficacy. Moreover, the oral absorption of itraconazole capsules is 50% reduced as a result of hypochlorhydria; mean plasma concentrations of itraconazole and ketoconazole are lower in AIDS patients than in healthy people, though this probably reflects chronic illness (58, 224). Unbound amphotericin B levels can be higher in uremic patients than in healthy volunteers (4.15% versus 3.55%), while hepatic and renal failure does not influence blood levels, although there are reports of serum levels being correlated with creatinine values (90). The half-life of itraconazole in patients with liver cirrhosis is prolonged to 37 h, and an average reduction of 64% in peak plasma concentrations has been detected in patients undergoing chronic ambulatory peritoneal dialysis (224). Elimination of fluconazole is delayed in patients with renal impairment, while in patients on chronic ambulatory peritoneal dialysis, peritoneal clearance of fluconazole is below the renal clearance observed in patients with normal kidney function. Terbinafine metabolism is impaired in patients with liver and renal disease (224). Impaired hepatic function decreases plasma clearance by approximately 30%, resulting in markedly increased AUC values, while impaired renal function prolongs the terminal plasma elimination half-life and doubles the AUC compared to healthy volunteers (134). The AUC of caspofungin is increased from 30% to 49% in patients with renal insufficiency and from 55% to 76% in patients with mild and moderate hepatic insufficiency, respectively (244). Although protein binding of voriconazole is not affected by impaired hepatic function, AUC after a single (but not multiple) oral dose of voriconazole is 233% higher in patients with mild and moderate hepatic cirrhosis than in subjects with normal hepatic function (78). Renal insufficiency alters flucytosine pharmacokinetics, since it slows absorption, prolongs the serum half-life, and decreases clearance (259). Neither renal impairment (D. Thye, T. Marbury, T. Kilfoil, G. Kilfoil, and T. Henkel, Abstr. 42nd Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-1391, 2002) nor hemodialysis (D. Thye, T. Marbury, T. Kilfoil, G. Kilfoil, and T. Henkel, Abstr. 42nd Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-1390, 2002) significantly alters the pharmacokinetics of anidulafungin and posaconazole (46), while plasma concentrations are decreased and plasma clearance is increased in patients with severe hepatic impairment (D. Thye, T. Kilfoil, G. Kilfoil, and T. Henkel, Abstr. 42nd Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-1392, 2002).
Drug Interactions
Drug interaction is a major factor that alters the pharmacokinetics of antifungal drugs. Thus, genetic variants that alter the clearance of a competing drug can have an indirect effect on the toxicity and efficacy profile of an antifungal agent. Antacids and H2 receptor antagonists delay and reduce the absorption of flucytosine, ketoconazole, and itraconazole (2, 224). Plasma ketoconazole, itraconazole, and miconazole, and to a lesser extent fluconazole, concentrations are markedly reduced by concomitant administration of drugs that induce liver enzymes, such as phenytoin, carbamazepine, or rifampin. Voriconazole levels are also increased with coadministration of CYP450 inhibitors, such as omeprazole, phenytoin, warfarin, tacrolimus, sirolimus, and rifabutin (78). Rifabutin, phenytoin, and cimetidine decrease plasma levels and increase the clearance of posaconazole (5; R. Courtney, D. Wexler, P. Statkevich, J. Lim, V. Batra, and M. Laughlin, Abstr. 42nd Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-1838, 2002). Terbinafine concentrations are decreased by coadministration of rifampin but, interestingly, increase after coadministration with cimetidine (224). Concomitant administration of aluminum hydroxide or magnesium hydroxide suspensions delays the absorption of flucytosine. However, this effect is minor for total bioavailability, whereas amphotericin B, which impairs glomerular filtration, could lead to an increase in the serum concentration and the half-life of flucytosine (259). Cyclosporine increases the AUC of caspofungin by 35%, while the concentration of caspofungin may be reduced by coadministration of inducers or mixed inducers/inhibitors of CYP450 isoenzymes, such as efavirenz, nelfinavir, nevirapine, phenytoin, rifampin, dexamethasone, and carbamazepine (244). However, a more complicated interaction with rifampin has been observed recently due to both inhibitory and induction effects of rifampin on caspofungin disposition, with a net effect of slight induction at steady state (245).
Environmental Factors
Environmental factors, such as pollutants or diet, can alter the pharmacokinetics of antifungal drugs. The absorption of itraconazole capsules is increased by 31% to 163% when taken with a meal, while the absorption of itraconazole solution is enhanced in the fasting state and reduced when taken with food (227). The bioavailability of ketoconazole tends to be increased by the intake of a high-fat meal but to be reduced by the intake of a high-carbohydrate meal (165). Food substantially enhanced the rate and extent of posaconazole absorption in healthy subjects (47), while the bioavailability of voriconazole is reduced by approximately 22% as measured by AUC within a dosing interval (AUCτ) after multiple dosing when taken with food compared with fasting (207). Grapefruit juice increased plasma levels of itraconazole in guinea pigs (173) and of voriconazole in mice (247).
Chemical Properties
Stereoselectivity may also alter the pharmacokinetics of antifungal drugs, particularly those that are administered in racemic mixtures. For example, ketoconazole and itraconazole are chiral drugs, which are administered as racemic (1:1) mixtures of (+) and (−) enantiomers. Although the antifungal activities of these enantiomers are the same, the (−) enantiomers are more potent CYP3A4 inhibitors. For (−)-ketoconazole, the AUC0-12 is threefold higher while the half-life is shorter than for the (+)-ketoconazole (J. G. Gerber, S. Dilmaghanian, and J. Gal, Abstr. 43rd Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-1569, 2003). The AUC0-48 and Cmax of (−)-itraconazole were three to four times higher than those of (+)-itraconazole in healthy individuals (C. Pyrgaki, J. Gal, S. Bannister,and J. G. Gerber, Abstr. 44th Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-36, 2005).
CONCLUDING REMARKS
Antifungal pharmacogenomics is an exciting area of medical mycology that may lead to individual-patient-based management of antifungal drugs by facilitating the choice of the optimal compound, dosage, and schedule. Furthermore, antifungal pharmacogenomics may be important for determining the individual risk of drug toxicity and for minimizing the risk of potential side effects. In order to achieve this goal, genomics can be applied to the study of pharmacology in directed ways, using the tools of population genetics to define interindividual differences. Pharmacogenomic models can then be derived for genetic variation in absorption, distribution, metabolism, and excretion, which would be linked with antifungal pharmacokinetics.
Although the field of antifungal pharmacogenomics is in its infancy, with few genetic association studies having been conducted, there are many data indicating the importance of genetic polymorphisms in the disposition of antifungal drugs. Thus far, genetic polymorphisms in CYP2C19 have been associated with voriconazole plasma levels and the importance of genetic polymorphisms of the UGT and MDR1 genes has been shown for posaconazole pharmacokinetics in humans. These findings are of clinical importance, since subtherapeutic levels in fast metabolizers may explain clinical resistance despite microbiological susceptibility of the pathogens, whereas overexposure in slow metabolizers may be associated with toxicity. Finally, many in vitro and in vivo data have shown the roles of drug transporters and other biomolecules in antifungal-drug disposition. Whether the genetic variants of these biomolecules have different properties in transporting, binding, and metabolizing of antifungal drugs remains to be seen in order to define the real dimensions of antifungal pharmacogenomics.
Potential candidate genes for antifungal pharmacogenomic studies are summarized in Table 5. They include drug transporters involved in absorption and excretion, phase I and II enzymes involved in metabolism, albumin, AAG, and lipoproteins involved in the distribution of antifungal drugs. However, more studies are required to elucidate the contributions of allelic polymorphisms to the disposition of antifungal drugs. Appropriately designed genetic association studies in well-defined populations are important in order to characterize the outcomes with respect to variation in pathways. Finally, these models should incorporate environmental, drug interaction, pathophysiological, and other factors that could influence drug pharmacokinetics. By taking into account these variables, pharmacogenomics holds the promise of mechanistically elucidating variation in antifungal drug disposition and assessing the risk of drug response or failure. Pharmacogenomics has the potential to shift the paradigm of therapy, but the complex challenge ahead will be to address how we use information derived from population-based studies to guide the management of individual patients.
TABLE 5.
Potential targets for analyzing genetic polymorphisms important for pharmacokinetics of antifungal drugsa
| Drug | Absorption
|
Distribution
|
Metabolism
|
Excretion
|
|||||
|---|---|---|---|---|---|---|---|---|---|
| GI pH (ATPase) | Efflux drug transporters (P-gp, MRP1+0 -5, BCRP) | Albumin | AAG | Lipoproteins | Phase I (CYP450) | Phase II (NAT, UGT) | Renal (OATs, MRPs, OCTs) | Hepatobiliary (P-gp, MRPs, OATPs, OCTs) | |
| Triazoles | |||||||||
| Itraconazole | + | + | + | − | − | + | − | − | − |
| Fluconazole | − | + | − | + | − | − | − | + | − |
| Voriconazole | − | + | ? | ? | − | + | − | − | − |
| Posaconazole | + | + | + | ? | ? | + (?) | + (?) | − | + |
| Polyenes | |||||||||
| Amphotericin Bb | − | + | + | + | + | − | − | + | + |
| Allylamines | |||||||||
| Terbinafine | − | + | + | + | + | + | − | − | − |
| Echinocandins | |||||||||
| Caspofungin | − | + | + | − | − | + | + | − | − |
| Micafungin | − | ? | + | − | − | − | + | − | − |
| Anidulafungin | − | ? | + | − | − | − | − | − | − |
| Pyrimidines | |||||||||
| Flucytosine | − | + | − | − | − | − | − | − | − |
+, probable; −, improbable.
Few data exist for amphotericin B lipid formulations.
Acknowledgments
This research was supported by the Intramural Research Program of the Center for Cancer Research, National Cancer Institute, NIH.
REFERENCES
- 1.Ahonen, J., K. T. Olkkola, and P. J. Neuvonen. 1996. The effect of the antimycotic itraconazole on the pharmacokinetics and pharmacodynamics of diazepam. Fundam. Clin. Pharmacol. 10:314-318. [DOI] [PubMed] [Google Scholar]
- 2.Albengres, E., H. Le Louet, and J. P. Tillement. 1998. Systemic antifungal agents. Drug interactions of clinical significance. Drug Saf. 18:83-97. [DOI] [PubMed] [Google Scholar]
- 3.Ambudkar, S. V., C. Kimchi-Sarfaty, Z. E. Sauna, and M. M. Gottesman. 2003. Pglycoprotein: from genomics to mechanism. Oncogene 22:7468-7485. [DOI] [PubMed] [Google Scholar]
- 4.Angirasa, A. K., and A. Z. Koch. 2002. P-glycoprotein as the mediator of itraconazoledigoxin interaction. J. Am. Podiatr. Med. Assoc. 92:471-472. [DOI] [PubMed] [Google Scholar]
- 5.Anonymous. 2003. Posaconazole: SCH 56592. Drugs R D 4:258-263. [DOI] [PubMed] [Google Scholar]
- 6.Aoyama, N., Y. Tanigawara, T. Kita, T. Sakai, K. Shirakawa, D. Shirasaka, F. Kodama, K. Okumura, and M. Kasuga. 1999. Sufficient effect of 1-week omeprazole and amoxicillin dual treatment for Helicobacter pylori eradication in cytochrome P450 2C19 poor metabolizers. J. Gastroenterol. 34(Suppl. 11):80-83. [PubMed] [Google Scholar]
- 7.Arndt, C. A., T. J. Walsh, C. L. McCully, F. M. Balis, P. A. Pizzo, and D. G. Poplack. 1988. Fluconazole penetration into cerebrospinal fluid: implications for treating fungal infections of the central nervous system. J. Infect. Dis. 157:178-180. [DOI] [PubMed] [Google Scholar]
- 8.Arredondo, G., R. Calvo, F. Marcos, R. Martinez-Jorda, and E. Suarez. 1995. Protein binding of itraconazole and fluconazole in patients with cancer. Int. J. Clin. Pharmacol. Ther. 33:449-452. [PubMed] [Google Scholar]
- 9.Arredondo, G., R. Martinez-Jorda, R. Calvo, C. Aguirre, and E. Suarez. 1994. Protein binding of itraconazole and fluconazole in patients with chronic renal failure. Int. J. Clin. Pharmacol. Ther. 32:361-364. [PubMed] [Google Scholar]
- 10.Arredondo, G., E. Suarez, R. Calvo, J. A. Vazquez, J. Garcia-Sanchez, and R. Martinez-Jorda. 1999. Serum protein binding of itraconazole and fluconazole in patients with diabetes mellitus. J. Antimicrob. Chemother. 43:305-307. [DOI] [PubMed] [Google Scholar]
- 11.Ayrton, A., and P. Morgan. 2001. Role of transport proteins in drug absorption, distribution and excretion. Xenobiotica 31:469-497. [DOI] [PubMed] [Google Scholar]
- 12.Bacanu, S. A., B. Devlin, and K. Roeder. 2000. The power of genomic control. Am. J. Hum. Genet. 66:1933-1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bader, J. S. 2001. The relative power of SNPs and haplotype as genetic markers for association tests. Pharmacogenomics 2:11-24. [DOI] [PubMed] [Google Scholar]
- 14.Bahadur, N., J. B. Leathart, E. Mutch, D. Steimel-Crespi, S. A. Dunn, R. Gilissen, J. V. Houdt, J. Hendrickx, G. Mannens, H. Bohets, F. M. Williams, M. Armstrong, C. L. Crespi, and A. K. Daly. 2002. CYP2C8 polymorphisms in Caucasians and their relationship with paclitaxel 6α-hydroxylase activity in human liver microsomes. Biochem. Pharmacol. 64:1579-1589. [DOI] [PubMed] [Google Scholar]
- 15.Baker, E. K., and A. El-Osta. 2003. The rise of DNA methylation and the importance of chromatin on multidrug resistance in cancer. Exp. Cell Res. 290:177-194. [DOI] [PubMed] [Google Scholar]
- 16.Balani, S. K., X. Xu, B. H. Arison, M. V. Silva, A. Gries, F. A. DeLuna, D. Cui, P. H. Kari, T. Ly, C. E. Hop, R. Singh, M. A. Wallace, D. C. Dean, J. H. Lin, P. G. Pearson, and T. A. Baillie. 2000. Metabolites of caspofungin acetate, a potent antifungal agent, in human plasma and urine. Drug Metab. Dispos. 28:1274-1278. [PubMed] [Google Scholar]
- 17.Baley, J. E., C. Meyers, R. M. Kliegman, M. R. Jacobs, and J. L. Blumer. 1990. Pharmacokinetics, outcome of treatment, and toxic effects of amphotericin B and 5-fluorocytosine in neonates. J. Pediatr. 116:791-797. [DOI] [PubMed] [Google Scholar]
- 18.Beierle, I., B. Meibohm, and H. Derendorf. 1999. Gender differences in pharmacokinetics and pharmacodynamics. Int. J. Clin. Pharmacol. Ther. 37:529-547. [PubMed] [Google Scholar]
- 19.Bekersky, I., R. M. Fielding, D. E. Dressler, J. W. Lee, D. N. Buell, and T. J. Walsh. 2002. Pharmacokinetics, excretion, and mass balance of liposomal amphotericin B (AmBisome) and amphotericin B deoxycholate in humans. Antimicrob. Agents Chemother. 46:828-833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bekersky, I., R. M. Fielding, D. E. Dressler, J. W. Lee, D. N. Buell, and T. J. Walsh. 2002. Plasma protein binding of amphotericin B and pharmacokinetics of bound versus unbound amphotericin B after administration of intravenous liposomal amphotericin B (AmBisome) and amphotericin B deoxycholate. Antimicrob. Agents Chemother. 46:834-840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benson, J. M., and M. C. Nahata. 1989. Pharmacokinetics of amphotericin B in children. Antimicrob. Agents Chemother. 33:1989-1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bertilsson, L., T. A. Baillie, and J. Reviriego. 1990. Factors influencing the metabolism of diazepam. Pharmacol. Ther. 45:85-91. [DOI] [PubMed] [Google Scholar]
- 23.Bertilsson, L., M. L. Dahl, P. Dalen, and A. Al-Shurbaji. 2002. Molecular genetics of CYP2D6: clinical relevance with focus on psychotropic drugs. Br. J. Clin. Pharmacol. 53:111-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blum, R. A., D. T. D'Andrea, B. M. Florentino, J. H. Wilton, D. M. Hilligoss, M. J. Gardner, E. B. Henry, H. Goldstein, and J. J. Schentag. 1991. Increased gastric pH and the bioavailability of fluconazole and ketoconazole. Ann. Intern. Med. 114:755-757. [DOI] [PubMed] [Google Scholar]
- 25.Bohan, A., and J. L. Boyer. 2002. Mechanisms of hepatic transport of drugs: implications for cholestatic drug reactions. Semin. Liver Dis. 22:123-136. [DOI] [PubMed] [Google Scholar]
- 26.Bolard, J., M. Seigneuret, and G. Boudet. 1980. Interaction between phospholipid bilayer membranes and the polyene antibiotic amphotericin B: lipid state and cholesterol content dependence. Biochim. Biophys. Acta 599:280-293. [DOI] [PubMed] [Google Scholar]
- 27.Borst, P., R. Evers, M. Kool, and J. Wijnholds. 2000. A family of drug transporters: the multidrug resistance-associated proteins. J. Natl. Cancer Inst. 92:1295-1302. [DOI] [PubMed] [Google Scholar]
- 28.Botstein, D., and N. Risch. 2003. Discovering genotypes underlying human phenotypes: past successes for Mendelian disease, future approaches for complex disease. Nat. Genet. 33(Suppl):228-237. [DOI] [PubMed] [Google Scholar]
- 29.Bozzette, S. A., R. L. Gordon, A. Yen, M. Rinaldi, M. K. Ito, and J. Fierer. 1992. Biliary concentrations of fluconazole in a patient with candidal cholecystitis: case report. Clin. Infect. Dis. 15:701-703. [DOI] [PubMed] [Google Scholar]
- 30.Brajtburg, J., S. Elberg, J. Bolard, G. S. Kobayashi, R. A. Levy, R. E. Ostlund, Jr., D. Schlessinger, and G. Medoff. 1984. Interaction of plasma proteins and lipoproteins with amphotericin B. J. Infect. Dis. 149:986-997. [DOI] [PubMed] [Google Scholar]
- 31.Brammer, K. W., and P. E. Coates. 1994. Pharmacokinetics of fluconazole in pediatric patients. Eur. J. Clin. Microbiol. Infect. Dis. 13:325-329. [DOI] [PubMed] [Google Scholar]
- 32.Brammer, K. W., P. R. Farrow, and J. K. Faulkner. 1990. Pharmacokinetics and tissue penetration of fluconazole in humans. Rev. Infect. Dis. 12(Suppl. 3):S318-S326. [DOI] [PubMed] [Google Scholar]
- 33.Brunskill, N. 2001. Mechanisms of albumin uptake by proximal tubular cells. Am. J. Kidney Dis. 37:S17-S20. [DOI] [PubMed] [Google Scholar]
- 34.Caporaso, N. E., C. Lerman, J. Audrain, N. R. Boyd, D. Main, H. J. Issaq, B. Utermahlan, R. T. Falk, and P. Shields. 2001. Nicotine metabolism and CYP2D6 phenotype in smokers. Cancer Epidemiol. Biomarkers Prev. 10:261-263. [PubMed] [Google Scholar]
- 35.Carlson, C. S., M. A. Eberle, M. J. Rieder, J. D. Smith, L. Kruglyak, and D. A. Nickerson. 2003. Additional SNPs and linkage-disequilibrium analyses are necessary for whole-genome association studies in humans. Nat. Genet. 33:518-521. [DOI] [PubMed] [Google Scholar]
- 36.Cassidy, S. M., F. W. Strobel, and K. M. Wasan. 1998. Plasma lipoprotein distribution of liposomal nystatin is influenced by protein content of high-density lipoproteins. Antimicrob. Agents Chemother. 42:1878-1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cattaneo, D., N. Perico, and G. Remuzzi. 2004. From pharmacokinetics to pharmacogenomics: a new approach to tailor immunosuppressive therapy. Am. J. Transplant. 4:299-310. [DOI] [PubMed] [Google Scholar]
- 38.Cauwenbergh, G., H. Degreef, J. Heykants, R. Woestenborghs, P. Van Rooy, and K. Haeverans. 1988. Pharmacokinetic profile of orally administered itraconazole in human skin. J. Am. Acad. Dermatol. 18:263-268. [DOI] [PubMed] [Google Scholar]
- 39.Chandra, P., and K. L. Brouwer. 2004. The complexities of hepatic drug transport: current knowledge and emerging concepts. Pharm. Res. 21:719-735. [DOI] [PubMed] [Google Scholar]
- 40.Chanock, S. 2001. Candidate genes and single nucleotide polymorphisms (SNPs) in the study of human disease. Dis. Markers 17:89-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen, C. J., D. Clark, K. Ueda, I. Pastan, M. M. Gottesman, and I. B. Roninson. 1990. Genomic organization of the human multidrug resistance (MDR1) gene and origin of P-glycoproteins. J. Biol. Chem. 265:506-514. [PubMed] [Google Scholar]
- 42.Chow, M. S., C. M. White, C. P. Lau, C. Fan, and M. O. Tang. 2001. Evaluation of CYP2D6 oxidation of dextromethorphan and propafenone in a Chinese population with atrial fibrillation. J. Clin. Pharmacol. 41:92-96. [DOI] [PubMed] [Google Scholar]
- 43.Cohen, A. D., E. Medvesovsky, R. Shalev, A. Biton, T. Chetov, S. Naimer, A. Shai, and D. A. Vardy. 2003. An independent comparison of terbinafine and itraconazole in the treatment of toenail onychomycosis. J. Dermatolog. Treat. 14:237-242. [DOI] [PubMed] [Google Scholar]
- 44.Cornford, E. M., C. P. Diep, and W. M. Pardridge. 1985. Blood-brain barrier transport of valproic acid. J. Neurochem. 44:1541-1550. [DOI] [PubMed] [Google Scholar]
- 45.Courtney, R., E. Radwanski, J. Lim, and M. Laughlin. 2004. Pharmacokinetics of posaconazole coadministered with antacid in fasting or nonfasting healthy men. Antimicrob. Agents Chemother. 48:804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Courtney, R., A. Sansone, W. Smith, T. Marbury, P. Statkevich, M. Martinho, M. Laughlin, and S. Swan. 2005. Posaconazole pharmacokinetics, safety, and tolerability in subjects with varying degrees of chronic renal disease. J. Clin. Pharmacol. 45:185-192. [DOI] [PubMed] [Google Scholar]
- 47.Courtney, R., D. Wexler, E. Radwanski, J. Lim, and M. Laughlin. 2004. Effect of food on the relative bioavailability of two oral formulations of posaconazole in healthy adults. Br. J. Clin. Pharmacol. 57:218-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cribb, A. E., R. Isbrucker, T. Levatte, B. Tsui, C. T. Gillespie, and K. W. Renton. 1994. Acetylator phenotyping: the urinary caffeine metabolite ratio in slow acetylators correlates with a marker of systemic NAT1 activity. Pharmacogenetics 4:166-170. [PubMed] [Google Scholar]
- 49.Csajka, C., L. A. Decosterd, T. Buclin, J. L. Pagani, K. Fattinger, J. Bille, and J. Biollaz. 2001. Population pharmacokinetics of fluconazole given for secondary prevention of oropharyngeal candidiasis in HIV-positive patients. Eur. J. Clin. Pharmacol. 57:723-727. [DOI] [PubMed] [Google Scholar]
- 50.Daly, A. K. 2003. Candidate gene case-control studies. Pharmacogenomics 4:127-139. [DOI] [PubMed] [Google Scholar]
- 51.Daly, A. K. 2003. Pharmacogenetics of the major polymorphic metabolizing enzymes. Fundam. Clin. Pharmacol. 17:27-41. [DOI] [PubMed] [Google Scholar]
- 52.Daly, A. K., and C. P. Day. 2001. Candidate gene case-control association studies: advantages and potential pitfalls. Br. J. Clin. Pharmacol. 52:489-499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dammerman, M., and J. L. Breslow. 1995. Genetic basis of lipoprotein disorders. Circulation 91:505-512. [DOI] [PubMed] [Google Scholar]
- 54.Daneshmend, T. K., and D. W. Warnock. 1983. Clinical pharmacokinetics of systemic antifungal drugs. Clin. Pharmacokinet. 8:17-42. [DOI] [PubMed] [Google Scholar]
- 55.Dangi, J. S., S. P. Vyas, and V. K. Dixit. 1998. Effect of various lipid-bile salt mixed micelles on the intestinal absorption of amphotericin-B in rat. Drug Dev. Ind. Pharm. 24:631-635. [DOI] [PubMed] [Google Scholar]
- 56.Dasgupta, A., and M. Luke. 1997. Valproic acid-ketoconazole interaction in normal, hypoalbuminemic, and uremic sera: lack of interaction in uremic serum caused by the presence of inhibitor. Ther. Drug Monit. 19:281-285. [DOI] [PubMed] [Google Scholar]
- 57.Dean, R. P. 1994. Food and drug interactions affecting itraconazole absorption. Top. Drug Ther. 36:1-5. [Google Scholar]
- 58.De Beule, K., and J. Van Gestel. 2001. Pharmacology of itraconazole. Drugs 61(Suppl. 1):27-37. [DOI] [PubMed] [Google Scholar]
- 59.Debruyne, D. 1997. Clinical pharmacokinetics of fluconazole in superficial and systemic mycoses. Clin. Pharmacokinet. 33:52-77. [DOI] [PubMed] [Google Scholar]
- 60.Debruyne, D., and A. Coquerel. 2001. Pharmacokinetics of antifungal agents in onychomycoses. Clin. Pharmacokinet. 40:441-472. [DOI] [PubMed] [Google Scholar]
- 61.Debruyne, D., and J. P. Ryckelynck. 1993. Clinical pharmacokinetics of fluconazole. Clin. Pharmacokinet. 24:10-27. [DOI] [PubMed] [Google Scholar]
- 62.Denning, D. W. 2003. Echinocandin antifungal drugs. Lancet 362:1142-1151. [DOI] [PubMed] [Google Scholar]
- 63.Denning, D. W. 2002. Echinocandins: a new class of antifungal. J. Antimicrob. Chemother. 49:889-891. [DOI] [PubMed] [Google Scholar]
- 64.Denning, D. W., A. Marinus, J. Cohen, D. Spence, R. Herbrecht, L. Pagano, C. Kibbler, V. Kcrmery, F. Offner, C. Cordonnier, U. Jehn, M. Ellis, L. Collette, R. Sylvester, et al. 1998. An EORTC multicentre prospective survey of invasive aspergillosis in haematological patients: diagnosis and therapeutic outcome. J. Infect. 37:173-180. [DOI] [PubMed] [Google Scholar]
- 65.Deresinski, S. C., and D. A. Stevens. 2003. Caspofungin. Clin. Infect. Dis. 36:1445-1457. [DOI] [PubMed] [Google Scholar]
- 66.Desta, Z., X. Zhao, J. G. Shin, and D. A. Flockhart. 2002. Clinical significance of the cytochrome P450 2C19 genetic polymorphism. Clin. Pharmacokinet. 41:913-958. [DOI] [PubMed] [Google Scholar]
- 67.Diebold, K., G. Michel, J. Schweizer, M. Diebold-Dorsam, W. Fiehn, and B. Kohl. 1998. Are psychoactive-drug-induced changes in plasma lipid and lipoprotein levels of significance for clinical remission in psychiatric disorders? Pharmacopsychiatry 31:60-67. [DOI] [PubMed] [Google Scholar]
- 68.Donato, M. T., and J. V. Castell. 2003. Strategies and molecular probes to investigate the role of cytochrome P450 in drug metabolism: focus on in vitro studies. Clin. Pharmacokinet. 42:153-178. [DOI] [PubMed] [Google Scholar]
- 69.Dowell, J. A., W. Knebel, T. Ludden, M. Stogniew, D. Krause, and T. Henkel. 2004. Population pharmacokinetic analysis of anidulafungin, an echinocandin antifungal. J. Clin. Pharmacol. 44:590-598. [DOI] [PubMed] [Google Scholar]
- 70.Duan, J., M. S. Wainwright, J. M. Comeron, N. Saitou, A. R. Sanders, J. Gelernter, and P. V. Gejman. 2003. Synonymous mutations in the human dopamine receptor D2 (DRD2) affect mRNA stability and synthesis of the receptor. Hum. Mol. Genet. 12:205-216. [DOI] [PubMed] [Google Scholar]
- 71.Dursun, S. M., A. Szemis, H. Andrews, and M. A. Reveley. 1999. The effects of clozapine on levels of total cholesterol and related lipids in serum of patients with schizophrenia: a prospective study. J. Psychiatry Neurosci. 24:453-455. [PMC free article] [PubMed] [Google Scholar]
- 72.Ehrnebo, M., S. Agurell, B. Jalling, and L. O. Boreus. 1971. Age differences in drug binding by plasma proteins: studies on human foetuses, neonates and adults. Eur. J. Clin. Pharmacol. 3:189-193. [DOI] [PubMed] [Google Scholar]
- 73.Ekins, S., and S. A. Wrighton. 1999. The role of CYP2B6 in human xenobiotic metabolism. Drug Metab. Rev. 31:719-754. [DOI] [PubMed] [Google Scholar]
- 74.Ernst, E. J. 2001. Investigational antifungal agents. Pharmacotherapy 21:165S-174S. [DOI] [PubMed] [Google Scholar]
- 75.Evans, W. E., and H. L. McLeod. 2003. Pharmacogenomics—drug disposition, drug targets, and side effects. N. Engl. J. Med. 348:538-549. [DOI] [PubMed] [Google Scholar]
- 76.Faergemann, J., H. Zehender, T. Jones, and I. Maibach. 1991. Terbinafine levels in serum, stratum corneum, dermis-epidermis (without stratum corneum), hair, sebum and eccrine sweat. Acta Derm. Venereol. 71:322-326. [PubMed] [Google Scholar]
- 77.Fanos, V., and L. Cataldi. 2001. Renal transport of antibiotics and nephrotoxicity: a review. J. Chemother. 13:461-472. [DOI] [PubMed] [Google Scholar]
- 78.FDA Antiviral Advisory Committee. 4. October 2001. Briefing document for voriconazole (oral and intravenous formulations). [Online.] http://www.fda.gov/ohrms/dockets/ac/01/briefing/3792b2_01_Pfizer.pdf.
- 79.Feinberg, A. P., and B. Tycko. 2004. The history of cancer epigenetics. Nat. Rev. Cancer 4:143-153. [DOI] [PubMed] [Google Scholar]
- 80.Fellay, J., C. Marzolini, E. R. Meaden, D. J. Back, T. Buclin, J. P. Chave, L. A. Decosterd, H. Furrer, M. Opravil, G. Pantaleo, D. Retelska, L. Ruiz, A. H. Schinkel, P. Vernazza, C. B. Eap, and A. Telenti. 2002. Response to antiretroviral treatment in HIV-1-infected individuals with allelic variants of the multidrug resistance transporter 1: a pharmacogenetics study. Lancet 359:30-36. [DOI] [PubMed] [Google Scholar]
- 81.Finta, C., and P. G. Zaphiropoulos. 2002. Intergenic mRNA molecules resulting from trans-splicing. J. Biol. Chem. 277:5882-5890. [DOI] [PubMed] [Google Scholar]
- 82.Force, R. W., and M. C. Nahata. 1995. Salivary concentrations of ketoconazole and fluconazole: implications for drug efficacy in oropharyngeal and esophageal candidiasis. Ann. Pharmacother. 29:10-15. [DOI] [PubMed] [Google Scholar]
- 83.Franco, M. H., S. O. Brennan, E. K. Chua, U. Kragh-Hansen, S. M. Callegari-Jacques, M. Z. Bezerra, and F. M. Salzano. 1999. Albumin genetic variability in South America: population distribution and molecular studies. Am. J. Hum. Biol. 11:359-366. [DOI] [PubMed] [Google Scholar]
- 84.Freedman, M. L., D. Reich, K. L. Penney, G. J. McDonald, A. A. Mignault, N. Patterson, S. B. Gabriel, E. J. Topol, J. W. Smoller, C. N. Pato, M. T. Pato, T. L. Petryshen, L. N. Kolonel, E. S. Lander, P. Sklar, B. Henderson, J. N. Hirschhorn, and D. Altshuler. 2004. Assessing the impact of population stratification on genetic association studies. Nat. Genet. 36:388-393. [DOI] [PubMed] [Google Scholar]
- 85.Fromm, M. F. 2000. P-glycoprotein: a defense mechanism limiting oral bioavailability and CNS accumulation of drugs. Int. J. Clin. Pharmacol. Ther. 38:69-74. [DOI] [PubMed] [Google Scholar]
- 86.Fromm, M. F. 2002. The influence of MDR1 polymorphisms on P-glycoprotein expression and function in humans. Adv. Drug Deliv. Rev. 54:1295-1310. [DOI] [PubMed] [Google Scholar]
- 87.Fromtling, R. A. 2002. Micafungin sodium (FK-463). Drugs Today 38:245-257. [DOI] [PubMed] [Google Scholar]
- 88.Furuta, T., K. Ohashi, T. Kamata, M. Takashima, K. Kosuge, T. Kawasaki, H. Hanai, T. Kubota, T. Ishizaki, and E. Kaneko. 1998. Effect of genetic differences in omeprazole metabolism on cure rates for Helicobacter pylori infection and peptic ulcer. Ann. Intern. Med. 129:1027-1030. [DOI] [PubMed] [Google Scholar]
- 89.Gabriel, S. B., S. F. Schaffner, H. Nguyen, J. M. Moore, J. Roy, B. Blumenstiel, J. Higgins, M. DeFelice, A. Lochner, M. Faggart, S. N. Liu-Cordero, C. Rotimi, A. Adeyemo, R. Cooper, R. Ward, E. S. Lander, M. J. Daly, and D. Altshuler. 2002. The structure of haplotype blocks in the human genome. Science 296:2225-2229. [DOI] [PubMed] [Google Scholar]
- 90.Gallis, H. A., R. H. Drew, and W. W. Pickard. 1990. Amphotericin B: 30 years of clinical experience. Rev. Infect. Dis. 12:308-329. [DOI] [PubMed] [Google Scholar]
- 91.Garcia, C. K., G. Mues, Y. Liao, T. Hyatt, N. Patil, J. C. Cohen, and H. H. Hobbs. 2001. Sequence diversity in genes of lipid metabolism. Genome Res. 11:1043-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gaudry, S. E., D. S. Sitar, D. D. Smyth, J. K. McKenzie, and F. Y. Aoki. 1993. Gender and age as factors in the inhibition of renal clearance of amantadine by quinine and quinidine. Clin. Pharmacol. Ther. 54:23-27. [DOI] [PubMed] [Google Scholar]
- 93.Ghannoum, M. A., and D. M. Kuhn. 2002. Voriconazole—better chances for patients with invasive mycoses. Eur. J. Med. Res. 7:242-256. [PubMed] [Google Scholar]
- 94.Ghosal, A., N. Hapangama, Y. Yuan, J. Achanfuo-Yeboah, R. Iannucci, S. Chowdhury, K. Alton, J. E. Patrick, and S. Zbaida. 2004. Identification of human UDP-glucuronosyltransferase enzyme(s) responsible for the glucuronidation of posaconazole (Noxafil). Drug Metab. Dispos. 32:267-271. [DOI] [PubMed] [Google Scholar]
- 95.Ginsberg, H. N. 1998. Lipoprotein physiology. Endocrinol. Metab. Clin. N. Am. 27:503-519. [DOI] [PubMed] [Google Scholar]
- 96.Goldstein, J. A. 2001. Clinical relevance of genetic polymorphisms in the human CYP2C subfamily. Br. J. Clin. Pharmacol. 52:349-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Greenblatt, D. J., E. M. Sellers, and R. I. Shader. 1982. Drug therapy: drug disposition in old age. N. Engl. J. Med. 306:1081-1088. [DOI] [PubMed] [Google Scholar]
- 98.Groll, A. H., J. C. Gea-Banacloche, A. Glasmacher, G. Just-Nuebling, G. Maschmeyer, and T. J. Walsh. 2003. Clinical pharmacology of antifungal compounds. Infect. Dis. Clin. N. Am. 17:159-191, ix. [DOI] [PubMed] [Google Scholar]
- 99.Groll, A. H., N. Giri, V. Petraitis, R. Petraitiene, M. Candelario, J. S. Bacher, S. C. Piscitelli, and T. J. Walsh. 2000. Comparative efficacy and distribution of lipid formulations of amphotericin B in experimental Candida albicans infection of the central nervous system. J. Infect. Dis. 182:274-282. [DOI] [PubMed] [Google Scholar]
- 100.Groll, A. H., D. Mickiene, V. Petraitis, R. Petraitiene, K. H. Ibrahim, S. C. Piscitelli, I. Bekersky, and T. J. Walsh. 2001. Compartmental pharmacokinetics and tissue distribution of the antifungal echinocandin lipopeptide micafungin (FK463) in rabbits. Antimicrob. Agents Chemother. 45:3322-3327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Groll, A. H., S. C. Piscitelli, and T. J. Walsh. 1998. Clinical pharmacology of systemic antifungal agents: a comprehensive review of agents in clinical use, current investigational compounds, and putative targets for antifungal drug development. Adv. Pharmacol. 44:343-500. [DOI] [PubMed] [Google Scholar]
- 102.Groll, A. H., and T. J. Walsh. 2001. Caspofungin: pharmacology, safety and therapeutic potential in superficial and invasive fungal infections. Exp. Opin. Investig. Drugs 10:1545-1558. [DOI] [PubMed] [Google Scholar]
- 103.Groll, A. H., L. Wood, M. Roden, D. Mickiene, C. C. Chiou, E. Townley, L. Dad, S. C. Piscitelli, and T. J. Walsh. 2002. Safety, pharmacokinetics, and pharmacodynamics of cyclodextrin itraconazole in pediatric patients with oropharyngeal candidiasis. Antimicrob. Agents Chemother. 46:2554-2563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Grossi, P., C. Farina, R. Fiocchi, and D. Dalla Gasperina, et al. 2000. Prevalence and outcome of invasive fungal infections in 1,963 thoracic organ transplant recipients: a multicenter retrospective study. Transplantation 70:112-116. [PubMed] [Google Scholar]
- 105.Guillemette, C. 2003. Pharmacogenomics of human UDP-glucuronosyltransferase enzymes. Pharmacogenomics J. 3:136-158. [DOI] [PubMed] [Google Scholar]
- 106.Gwilt, P. R., R. R. Nahhas, and W. G. Tracewell. 1991. The effects of diabetes mellitus on pharmacokinetics and pharmacodynamics in humans. Clin. Pharmacokinet. 20:477-490. [DOI] [PubMed] [Google Scholar]
- 107.Hagenbuch, B., and P. J. Meier. 2003. The superfamily of organic anion transporting polypeptides. Biochim. Biophys. Acta 1609:1-18. [DOI] [PubMed] [Google Scholar]
- 108.Hajdu, R., R. Thompson, J. G. Sundelof, B. A. Pelak, F. A. Bouffard, J. F. Dropinski, and H. Kropp. 1997. Preliminary animal pharmacokinetics of the parenteral antifungal agent MK-0991 (L-743,872). Antimicrob. Agents Chemother. 41:2339-2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hartsel, S. C., B. Baas, E. Bauer, L. T. Foree, Jr., K. Kindt, H. Preis, A. Scott, E. H. Kwong, M. Ramaswamy, and K. M. Wasan. 2001. Heat-induced superaggregation of amphotericin B modifies its interaction with serum proteins and lipoproteins and stimulation of TNF-alpha. J. Pharm. Sci. 90:124-133. [DOI] [PubMed] [Google Scholar]
- 110.Hasler, J. A. 1999. Pharmacogenetics of cytochromes P450. Mol. Aspects Med. 20:12-24, 25-137. [DOI] [PubMed] [Google Scholar]
- 111.Hebert, M. F., H. E. Smith, T. C. Marbury, S. K. Swan, W. B. Smith, R. W. Townsend, D. Buell, J. Keirns, and I. Bekersky. 2005. Pharmacokinetics of micafungin in healthy volunteers, volunteers with moderate liver disease, and volunteers with renal dysfunction. J. Clin. Pharmacol. 45:1145-1152. [DOI] [PubMed] [Google Scholar]
- 112.Heft, M. W., and A. J. Mariotti. 2002. Geriatric pharmacology. Dent. Clin. N. Am. 46:869-885, xii. [DOI] [PubMed] [Google Scholar]
- 113.Hegele, R. A. 1997. Small genetic effects in complex diseases: a review of regulatory sequence variants in dyslipoproteinemia and atherosclerosis. Clin. Biochem. 30:183-188. [DOI] [PubMed] [Google Scholar]
- 114.Hein, D. W. 2002. Molecular genetics and function of NAT1 and NAT2: role in aromatic amine metabolism and carcinogenesis. Mutat. Res. 506-507:65-77. [DOI] [PubMed] [Google Scholar]
- 115.Hein, D. W., M. A. Doll, A. J. Fretland, M. A. Leff, S. J. Webb, G. H. Xiao, U. S. Devanaboyina, N. A. Nangju, and Y. Feng. 2000. Molecular genetics and epidemiology of the NAT1 and NAT2 acetylation polymorphisms. Cancer Epidemiol. Biomarkers Prev. 9:29-42. [PubMed] [Google Scholar]
- 116.Heykants, J., A. Van Peer, V. Van de Velde, P. Van Rooy, W. Meuldermans, K. Lavrijsen, R. Woestenborghs, J. Van Cutsem, and G. Cauwenbergh. 1989. The clinical pharmacokinetics of itraconazole: an overview. Mycoses 32(Suppl. 1):67-87. [DOI] [PubMed] [Google Scholar]
- 117.Hiemenz, J. W., and T. J. Walsh. 1996. Lipid formulations of amphotericin B: recent progress and future directions. Clin. Infect. Dis. 22(Suppl. 2):S133-S144. [DOI] [PubMed] [Google Scholar]
- 118.Hinoshita, E., K. Taguchi, A. Inokuchi, T. Uchiumi, N. Kinukawa, M. Shimada, M. Tsuneyoshi, K. Sugimachi, and M. Kuwano. 2001. Decreased expression of an ATP-binding cassette transporter, MRP2, in human livers with hepatitis C virus infection. J. Hepatol. 35:765-773. [DOI] [PubMed] [Google Scholar]
- 119.Hiruma, M., A. Matsushita, M. Kobayashi, and H. Ogawa. 2001. One week pulse therapy with itraconazole (200 mg day−1) for onychomycosis. Evaluation of treatment results according to patient background. Mycoses 44:87-93. [PubMed] [Google Scholar]
- 120.Hoffman, H. L., E. J. Ernst, and M. E. Klepser. 2000. Novel triazole antifungal agents. Exp. Opin. Investig. Drugs. 9:593-605. [DOI] [PubMed] [Google Scholar]
- 121.Hoffman, H. L., and R. C. Rathbun. 2002. Review of the safety and efficacy of voriconazole. Exp. Opin. Investig. Drugs 11:409-429. [DOI] [PubMed] [Google Scholar]
- 122.Hoffmeyer, S., O. Burk, O. von Richter, H. P. Arnold, J. Brockmoller, A. Johne, I. Cascorbi, T. Gerloff, I. Roots, M. Eichelbaum, and U. Brinkmann. 2000. Functional polymorphisms of the human multidrug-resistance gene: multiple sequence variations and correlation of one allele with P-glycoprotein expression and activity in vivo. Proc. Natl. Acad. Sci. USA 97:3473-3478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Hossain, M. A., and M. A. Ghannoum. 2000. New investigational antifungal agents for treating invasive fungal infections. Exp. Opin. Investig. Drugs 9:1797-1813. [DOI] [PubMed] [Google Scholar]
- 124.Hosseini-Yeganeh, M., and A. J. McLachlan. 2001. Tissue distribution of terbinafine in rats. J. Pharm. Sci. 90:1817-1828. [DOI] [PubMed] [Google Scholar]
- 125.Hu, Y., M. Oscarson, I. Johansson, Q. Y. Yue, M. L. Dahl, M. Tabone, S. Arinco, E. Albano, and M. Ingelman-Sundberg. 1997. Genetic polymorphism of human CYP2E1: characterization of two variant alleles. Mol. Pharmacol. 51:370-376. [PubMed] [Google Scholar]
- 126.Hughes, A. L., B. Packer, R. Welch, A. W. Bergen, S. J. Chanock, and M. Yeager. 2003. Widespread purifying selection at polymorphic sites in human protein-coding loci. Proc. Natl. Acad. Sci. USA 100:15754-15757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Humbert, H., J. Denouel, M. D. Cabiac, H. Lakhdar, and A. Sioufi. 1998. Pharmacokinetics of terbinafine and five known metabolites in children, after oral administration. Biopharm. Drug Dispos. 19:417-423. [DOI] [PubMed] [Google Scholar]
- 128.Hyland, R., B. C. Jones, and D. A. Smith. 2003. Identification of the cytochrome P450 enzymes involved in the N-oxidation of voriconazole. Drug Metab. Dispos. 31:540-547. [DOI] [PubMed] [Google Scholar]
- 129.Iida, N., K. Takara, N. Ohmoto, T. Nakamura, T. Kimura, A. Wada, M. Hirai, T. Sakaeda, and K. Okumura. 2001. Reversal effects of antifungal drugs on multidrug resistance in MDR1-overexpressing HeLa cells. Biol. Pharm. Bull. 24:1032-1036. [DOI] [PubMed] [Google Scholar]
- 130.Imbert, F., M. Jardin, C. Fernandez, J. C. Gantier, F. Dromer, G. Baron, F. Mentre, L. Van Beijsterveldt, E. Singlas, and F. Gimenez. 2003. Effect of efflux inhibition on brain uptake of itraconazole in mice infected with Cryptococcus neoformans. Drug Metab. Dispos. 31:319-325. [DOI] [PubMed] [Google Scholar]
- 131.Reference deleted.
- 132.Ingelman-Sundberg, M. 2001. Pharmacogenetics: an opportunity for a safer and more efficient pharmacotherapy. J. Intern. Med. 250:186-200. [DOI] [PubMed] [Google Scholar]
- 133.Israili, Z. H., and P. G. Dayton. 2001. Human alpha-1-glycoprotein and its interactions with drugs. Drug Metab. Rev. 33:161-235. [DOI] [PubMed] [Google Scholar]
- 134.Jain, S., and V. N. Sehgal. 2000. Terbinafine, a unique oral antifungal: current perceptions. Int. J. Dermatol. 39:412-423. [DOI] [PubMed] [Google Scholar]
- 135.Jezequel, S. G. 1994. Fluconazole: interspecies scaling and allometric relationships of pharmacokinetic properties. J. Pharm. Pharmacol. 46:196-199. [DOI] [PubMed] [Google Scholar]
- 136.Johnson, J. A., and T. N. Livingston. 1997. Differences between blacks and whites in plasma protein binding of drugs. Eur. J. Clin. Pharmacol. 51:485-488. [DOI] [PubMed] [Google Scholar]
- 137.Johnson, L. B., and C. A. Kauffman. 2003. Voriconazole: a new triazole antifungal agent. Clin. Infect. Dis. 36:630-637. [DOI] [PubMed] [Google Scholar]
- 138.Jolliet-Riant, P., M. F. Boukef, J. C. Duche, N. Simon, and J. P. Tillement. 1998. The genetic variant A of human alpha 1-acid glycoprotein limits the blood to brain transfer of drugs it binds. Life Sci. 62:PL219-PL226. [DOI] [PubMed] [Google Scholar]
- 139.Kartenbeck, J., U. Leuschner, R. Mayer, and D. Keppler. 1996. Absence of the canalicular isoform of the MRP gene-encoded conjugate export pump from the hepatocytes in Dubin-Johnson syndrome. Hepatology 23:1061-1066. [DOI] [PubMed] [Google Scholar]
- 140.Kearns, G. L., S. M. Abdel-Rahman, S. W. Alander, D. L. Blowey, J. S. Leeder, and R. E. Kauffman. 2003. Developmental pharmacology—drug disposition, action, and therapy in infants and children. N. Engl. J. Med. 349:1157-1167. [DOI] [PubMed] [Google Scholar]
- 141.Keitel, V., J. Kartenbeck, A. T. Nies, H. Spring, M. Brom, and D. Keppler. 2000. Impaired protein maturation of the conjugate export pump multidrug resistance protein 2 as a consequence of a deletion mutation in Dubin-Johnson syndrome. Hepatology 32:1317-1328. [DOI] [PubMed] [Google Scholar]
- 142.Kennedy, A. L., and K. M. Wasan. 1999. Preferential distribution of amphotericin B lipid complex into human HDL3 is a consequence of high density lipoprotein coat lipid content. J. Pharm. Sci. 88:1149-1155. [DOI] [PubMed] [Google Scholar]
- 143.Kim, R. B. 2002. Transporters and xenobiotic disposition. Toxicology 181-182:291-297. [DOI] [PubMed] [Google Scholar]
- 144.Kim, R. B., B. F. Leake, E. F. Choo, G. K. Dresser, S. V. Kubba, U. I. Schwarz, A. Taylor, H. G. Xie, J. McKinsey, S. Zhou, L. B. Lan, J. D. Schuetz, E. G. Schuetz, and G. R. Wilkinson. 2001. Identification of functionally variant MDR1 alleles among European Americans and African Americans. Clin. Pharmacol. Ther. 70:189-199. [DOI] [PubMed] [Google Scholar]
- 145.Kishino, S., A. Nomura, Z. S. Di, M. Sugawara, K. Iseki, S. Kakinoki, A. Kitabatake, and K. Miyazaki. 1995. Alpha-1-acid glycoprotein concentration and the protein binding of disopyramide in healthy subjects. J. Clin. Pharmacol. 35:510-514. [DOI] [PubMed] [Google Scholar]
- 146.Knoblauch, H., A. Bauerfeind, C. Krahenbuhl, A. Daury, K. Rohde, S. Bejanin, L. Essioux, H. Schuster, F. C. Luft, and J. G. Reich. 2002. Common haplotypes in five genes influence genetic variance of LDL and HDL cholesterol in the general population. Hum. Mol. Genet. 11:1477-1485. [DOI] [PubMed] [Google Scholar]
- 147.Konig, J., D. Rost, Y. Cui, and D. Keppler. 1999. Characterization of the human multidrug resistance protein isoform MRP3 localized to the basolateral hepatocyte membrane. Hepatology 29:1156-1163. [DOI] [PubMed] [Google Scholar]
- 148.Kontoyiannis, D. P., and R. E. Lewis. 2002. Antifungal drug resistance of pathogenic fungi. Lancet 359:1135-1144. [DOI] [PubMed] [Google Scholar]
- 149.Kragh-Hansen, U., S. O. Brennan, M. Galliano, and O. Sugita. 1990. Binding of warfarin, salicylate, and diazepam to genetic variants of human serum albumin with known mutations. Mol. Pharmacol. 37:238-242. [PubMed] [Google Scholar]
- 150.Kragh-Hansen, U., V. T. Chuang, and M. Otagiri. 2002. Practical aspects of the ligand-binding and enzymatic properties of human serum albumin. Biol. Pharm. Bull. 25:695-704. [DOI] [PubMed] [Google Scholar]
- 151.Krieter, P., B. Flannery, T. Musick, M. Gohdes, M. Martinho, and R. Courtney. 2004. Disposition of posaconazole following single-dose oral administration in healthy subjects. Antimicrob. Agents Chemother. 48:3543-3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kruglyak, L., and D. A. Nickerson. 2001. Variation is the spice of life. Nat. Genet. 27:234-236. [DOI] [PubMed] [Google Scholar]
- 153.Kruijtzer, C. M., J. H. Beijnen, and J. H. Schellens. 2002. Improvement of oral drug treatment by temporary inhibition of drug transporters and/or cytochrome P450 in the gastrointestinal tract and liver: an overview. Oncologist 7:516-530. [DOI] [PubMed] [Google Scholar]
- 154.Kuehl, P., J. Zhang, Y. Lin, J. Lamba, M. Assem, J. Schuetz, P. B. Watkins, A. Daly, S. A. Wrighton, S. D. Hall, P. Maurel, M. Relling, C. Brimer, K. Yasuda, R. Venkataramanan, S. Strom, K. Thummel, M. S. Boguski, and E. Schuetz. 2001. Sequence diversity in CYP3A promoters and characterization of the genetic basis of polymorphic CYP3A5 expression. Nat. Genet. 27:383-391. [DOI] [PubMed] [Google Scholar]
- 155.Kusuhara, H., and Y. Sugiyama. 2002. Role of transporters in the tissue-selective distribution and elimination of drugs: transporters in the liver, small intestine, brain and kidney. J. Control Release 78:43-54. [DOI] [PubMed] [Google Scholar]
- 156.Kwong, M., and K. M. Wasan. 2002. Cholesteryl ester transfer protein facilitates the movement of water-insoluble drugs between lipoproteins: a novel biological function for a well-characterized lipid transfer protein. Biochem. Pharmacol. 64:1669-1675. [DOI] [PubMed] [Google Scholar]
- 157.Lamba, J. K., Y. S. Lin, E. G. Schuetz, and K. E. Thummel. 2002. Genetic contribution to variable human CYP3A-mediated metabolism. Adv. Drug Deliv. Rev. 54:1271-1294. [DOI] [PubMed] [Google Scholar]
- 158.Lang, T., K. Klein, J. Fischer, A. K. Nussler, P. Neuhaus, U. Hofmann, M. Eichelbaum, M. Schwab, and U. M. Zanger. 2001. Extensive genetic polymorphism in the human CYP2B6 gene with impact on expression and function in human liver. Pharmacogenetics 11:399-415. [DOI] [PubMed] [Google Scholar]
- 159.Lazar, J. D., and K. D. Wilner. 1990. Drug interactions with fluconazole. Rev. Infect. Dis. 12(Suppl. 3):S327-S333. [DOI] [PubMed] [Google Scholar]
- 160.Leabman, M. K., C. C. Huang, M. Kawamoto, S. J. Johns, D. Stryke, T. E. Ferrin, J. DeYoung, T. Taylor, A. G. Clark, I. Herskowitz, and K. M. Giacomini. 2002. Polymorphisms in a human kidney xenobiotic transporter, OCT2, exhibit altered function. Pharmacogenetics 12:395-405. [DOI] [PubMed] [Google Scholar]
- 161.Lee, C. H., P. H. Yeh, and T. H. Tsai. 2002. Hepatobiliary excretion of fluconazole and its interaction with cyclosporin A in rat blood and bile using microdialysis. Int. J. Pharm. 241:367-373. [DOI] [PubMed] [Google Scholar]
- 162.Lee, C. R., J. A. Goldstein, and J. A. Pieper. 2002. Cytochrome P450 2C9 polymorphisms: a comprehensive review of the in-vitro and human data. Pharmacogenetics 12:251-263. [DOI] [PubMed] [Google Scholar]
- 163.Lee, J. W., N. L. Seibel, M. Amantea, P. Whitcomb, P. A. Pizzo, and T. J. Walsh. 1992. Safety and pharmacokinetics of fluconazole in children with neoplastic diseases. J. Pediatr. 120:987-993. [DOI] [PubMed] [Google Scholar]
- 164.Lee, W., and R. B. Kim. 2004. Transporters and renal drug elimination. Annu. Rev. Pharmacol. Toxicol. 44:137-166. [DOI] [PubMed] [Google Scholar]
- 165.Lelawongs, P., J. A. Barone, J. L. Colaizzi, A. T. Hsuan, W. Mechlinski, R. Legendre, and J. Guarnieri. 1988. Effect of food and gastric acidity on absorption of orally administered ketoconazole. Clin. Pharm. 7:228-235. [PubMed] [Google Scholar]
- 166.Li, J. H., J. Q. Xu, X. M. Cao, L. Ni, Y. Li, Y. Y. Zhuang, and J. B. Gong. 2002. Influence of the ORM1 phenotypes on serum unbound concentration and protein binding of quinidine. Clin. Chim. Acta 317:85-92. [DOI] [PubMed] [Google Scholar]
- 167.Lin, J. H., M. Chiba, and T. A. Baillie. 1999. Is the role of the small intestine in first pass metabolism overemphasized? Pharmacol. Rev. 51:135-158. [PubMed] [Google Scholar]
- 168.Lin, J. H., and M. Yamazaki. 2003. Role of P-glycoprotein in pharmacokinetics: clinical implications. Clin. Pharmacokinet. 42:59-98. [DOI] [PubMed] [Google Scholar]
- 169.Lovich, M. A., C. Creel, K. Hong, C. W. Hwang, and E. R. Edelman. 2001. Carrier proteins determine local pharmacokinetics and arterial distribution of paclitaxel. J. Pharm. Sci. 90:1324-1335. [DOI] [PubMed] [Google Scholar]
- 170.Lown, K. S., R. R. Mayo, A. B. Leichtman, H. L. Hsiao, D. K. Turgeon, P. Schmiedlin-Ren, M. B. Brown, W. Guo, S. J. Rossi, L. Z. Benet, and P. B. Watkins. 1997. Role of intestinal P-glycoprotein (mdr1) in interpatient variation in the oral bioavailability of cyclosporine. Clin. Pharmacol. Ther. 62:248-260. [DOI] [PubMed] [Google Scholar]
- 171.Lyman, C. A., and T. J. Walsh. 1992. Systemically administered antifungal agents. A review of their clinical pharmacology and therapeutic applications. Drugs 44:9-35. [DOI] [PubMed] [Google Scholar]
- 172.Ma, M. K., M. H. Woo, and H. L. McLeod. 2002. Genetic basis of drug metabolism. Am. J. Health Syst. Pharm. 59:2061-2069. [DOI] [PubMed] [Google Scholar]
- 173.MacCallum, D. M., and F. C. Odds. 2002. Influence of grapefruit juice on itraconazole plasma levels in mice and guinea pigs. J. Antimicrob. Chemother. 50:219-224. [DOI] [PubMed] [Google Scholar]
- 174.Machard, B., P. Misslin, and M. Lemaire. 1989. Influence of plasma protein binding on the brain uptake of an antifungal agent, terbinafine, in rats. J. Pharm. Pharmacol. 41:700-704. [DOI] [PubMed] [Google Scholar]
- 175.Madison, J., M. Galliano, S. Watkins, L. Minchiotti, F. Porta, A. Rossi, and F. W. Putnam. 1994. Genetic variants of human serum albumin in Italy: point mutants and a carboxyl-terminal variant. Proc. Natl. Acad. Sci. USA 91:6476-6480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Marchini, J., L. R. Cardon, M. S. Phillips, and P. Donnelly. 2004. The effects of human population structure on large genetic association studies. Nat. Genet. 36:512-517. [DOI] [PubMed] [Google Scholar]
- 177.Martinez-Jorda, R., J. M. Rodriguez-Sasiain, E. Suarez, and R. Calvo. 1990. Serum binding of ketoconazole in health and disease. Int. J. Clin. Pharmacol. Res. 10:271-276. [PubMed] [Google Scholar]
- 178.Masereeuw, R., and F. G. Russel. 2001. Mechanisms and clinical implications of renal drug excretion. Drug Metab. Rev. 33:299-351. [DOI] [PubMed] [Google Scholar]
- 179.May, D. B., R. H. Drew, K. C. Yedinak, and J. A. Bartlett. 1994. Effect of simultaneous didanosine administration on itraconazole absorption in healthy volunteers. Pharmacotherapy 14:509-513. [PubMed] [Google Scholar]
- 180.McCarthy, J. J., and R. Hilfiker. 2000. The use of single-nucleotide polymorphism maps in pharmacogenomics. Nat. Biotechnol. 18:505-508. [DOI] [PubMed] [Google Scholar]
- 181.McLeod, H. L., and W. E. Evans. 2001. Pharmacogenomics: unlocking the human genome for better drug therapy. Annu. Rev. Pharmacol. Toxicol. 41:101-121. [DOI] [PubMed] [Google Scholar]
- 182.McLeod, H. L., and C. Siva. 2002. The thiopurine S-methyltransferase gene locus—implications for clinical pharmacogenomics. Pharmacogenomics 3:89-98. [DOI] [PubMed] [Google Scholar]
- 183.McLeod, H. L., and J. Yu. 2003. Cancer pharmacogenomics: SNPs, chips, and the individual patient. Cancer Invest. 21:630-640. [DOI] [PubMed] [Google Scholar]
- 184.Meibohm, B., I. Beierle, and H. Derendorf. 2002. How important are gender differences in pharmacokinetics? Clin. Pharmacokinet. 41:329-342. [DOI] [PubMed] [Google Scholar]
- 185.Meyer, J. C., C. Burri, P. Ruf, and U. W. Schnyder. 1989. Factors affecting plasma levels of ketoconazole during long-term treatment. Dermatologica 178:29-32. [DOI] [PubMed] [Google Scholar]
- 186.Milne, R. W., L. A. Larsen, K. L. Jorgensen, J. Bastlund, G. R. Stretch, and A. M. Evans. 2000. Hepatic disposition of fexofenadine: influence of the transport inhibitors erythromycin and dibromosulphothalein. Pharm. Res. 17:1511-1515. [DOI] [PubMed] [Google Scholar]
- 187.Miyama, T., H. Takanaga, H. Matsuo, K. Yamano, K. Yamamoto, T. Iga, M. Naito, T. Tsuruo, H. Ishizuka, Y. Kawahara, and Y. Sawada. 1998. P-glycoprotein-mediated transport of itraconazole across the blood-brain barrier. Antimicrob. Agents Chemother. 42:1738-1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Mor-Cohen, R., A. Zivelin, N. Rosenberg, M. Shani, S. Muallem, and U. Seligsohn. 2001. Identification and functional analysis of two novel mutations in the multidrug resistance protein 2 gene in Israeli patients with Dubin-Johnson syndrome. J. Biol. Chem. 276:36923-36930. [DOI] [PubMed] [Google Scholar]
- 189.Moretti, M. E., S. Ito, and G. Koren. 1995. Disposition of maternal ketoconazole in breast milk. Am. J. Obstet. Gynecol. 173:1625-1626. [DOI] [PubMed] [Google Scholar]
- 190.Morrison, V. A., R. J. Haake, and D. J. Weisdorf. 1994. Non-Candida fungal infections after bone marrow transplantation: risk factors and outcome. Am. J. Med. 96:497-503. [DOI] [PubMed] [Google Scholar]
- 191.Nagata, K., and Y. Yamazoe. 2000. Pharmacogenetics of sulfotransferase. Annu. Rev. Pharmacol. Toxicol. 40:159-176. [DOI] [PubMed] [Google Scholar]
- 192.Nath, C. E., A. J. McLachlan, P. J. Shaw, R. Gunning, and J. W. Earl. 2001. Population pharmacokinetics of amphotericin B in children with malignant diseases. Br. J. Clin. Pharmacol. 52:671-680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Nedelman, J., J. A. Cramer, B. Robbins, E. Gibiansky, C. T. Chang, S. Gareffa, A. Cohen, and J. Meligeni. 1997. The effect of food on the pharmacokinetics of multiple dose terbinafine in young and elderly healthy subjects. Biopharm. Drug Dispos. 18:127-138. [DOI] [PubMed] [Google Scholar]
- 194.Nejjam, F., M. Zagula, M. D. Cabiac, N. Guessous, H. Humbert, and H. Lakhdar. 1995. Pilot study of terbinafine in children suffering from tinea capitis: evaluation of efficacy, safety and pharmacokinetics. Br. J. Dermatol. 132:98-105. [DOI] [PubMed] [Google Scholar]
- 195.Neuvonen, P. J., and K. M. Jalava. 1996. Itraconazole drastically increases plasma concentrations of lovastatin and lovastatin acid. Clin. Pharmacol. Ther. 60:54-61. [DOI] [PubMed] [Google Scholar]
- 196.Nishihara, K., J. Hibino, H. Kotaki, Y. Sawada, and T. Iga. 1999. Effect of itraconazole on the pharmacokinetics of digoxin in guinea pigs. Biopharm. Drug Dispos. 20:145-149. [DOI] [PubMed] [Google Scholar]
- 197.Norton, R. M. 2001. Clinical pharmacogenomics: applications in pharmaceutical R&D. Drug Discov. Today 6:180-185. [DOI] [PubMed] [Google Scholar]
- 198.Nozawa, T., M. Nakajima, I. Tamai, K. Noda, J. Nezu, Y. Sai, A. Tsuji, and T. Yokoi. 2002. Genetic polymorphisms of human organic anion transporters OATP-C (SLC21A6) and OATP-B (SLC21A9): allele frequencies in the Japanese population and functional analysis. J. Pharmacol. Exp. Ther. 302:804-813. [DOI] [PubMed] [Google Scholar]
- 199.Olbe, L., E. Carlsson, and P. Lindberg. 2003. A proton-pump inhibitor expedition: the case histories of omeprazole and esomeprazole. Nat. Rev. Drug Discov. 2:132-139. [DOI] [PubMed] [Google Scholar]
- 200.Persson, K., S. Sjostrom, I. Sigurdardottir, V. Molnar, M. Hammarlund-Udenaes, and A. Rane. 1995. Patient-controlled analgesia (PCA) with codeine for postoperative pain relief in ten extensive metabolisers and one poor metaboliser of dextromethorphan. Br. J. Clin. Pharmacol. 39:182-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Petersen, C. E., C. E. Ha, K. Harohalli, D. S. Park, and N. V. Bhagavan. 2000. Familial dysalbuminemic byperthyroxinemia may result in altered warfarin pharmacokinetics. Chem. Biol. Interact. 124:161-172. [DOI] [PubMed] [Google Scholar]
- 202.Petraitis, V., R. Petraitiene, A. H. Groll, T. Sein, R. L. Schaufele, C. A. Lyman, A. Francesconi, J. Bacher, S. C. Piscitelli, and T. J. Walsh. 2001. Dosage-dependent antifungal efficacy of V-echinocandin (LY303366) against experimental fluconazole-resistant oropharyngeal and esophageal candidiasis. Antimicrob. Agents Chemother. 45:471-479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Pollock, B. G. 1997. Gender differences in psychotropic drug metabolism. Psychopharmacol. Bull. 33:235-241. [PubMed] [Google Scholar]
- 204.Prentice, A. G., and P. Donnelly. 2001. Oral antifungals as prophylaxis in haematological malignancy. Blood Rev. 15:1-8. [DOI] [PubMed] [Google Scholar]
- 205.Pritchard, J. K., M. Stephens, N. A. Rosenberg, and P. Donnelly. 2000. Association mapping in structured populations. Am. J. Hum. Genet. 67:170-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Purkins, L., N. Wood, P. Ghahramani, K. Greenhalgh, M. J. Allen, and D. Kleinermans. 2002. Pharmacokinetics and safety of voriconazole following intravenous to oral-dose escalation regimens. Antimicrob. Agents Chemother. 46:2546-2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Purkins, L., N. Wood, D. Kleinermans, K. Greenhalgh, and D. Nichols. 2003. Effect of food on the pharmacokinetics of multiple-dose oral voriconazole. Br. J. Clin. Pharmacol. 56(Suppl. 1):17-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Ramaswamy, M., K. D. Peteherych, A. L. Kennedy, and K. M. Wasan. 2001. Amphotericin B lipid complex or amphotericin B multiple-dose administration to rabbits with elevated plasma cholesterol levels: pharmacokinetics in plasma and blood, plasma lipoprotein levels, distribution in tissues, and renal toxicities. Antimicrob. Agents Chemother. 45:1184-1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Raunio, H., A. Rautio, H. Gullsten, and O. Pelkonen. 2001. Polymorphisms of CYP2A6 and its practical consequences. Br. J. Clin. Pharmacol. 52:357-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Reed, R. G., and C. M. Burrington. 1989. The albumin receptor effect may be due to a surface-induced conformational change in albumin. J. Biol. Chem. 264:9867-9872. [PubMed] [Google Scholar]
- 211.Reynes, J., C. Bazin, F. Ajana, A. Datry, J. P. Le Moing, E. Chwetzoff, and J. C. Levron. 1997. Pharmacokinetics of itraconazole (oral solution) in two groups of human immunodeficiency virus-infected adults with oral candidiasis. Antimicrob. Agents Chemother. 41:2554-2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Rheney, C. C., and C. M. Saddler. 1998. Oral ketoconazole in cutaneous fungal infections. Ann. Pharmacother. 32:709-711. [DOI] [PubMed] [Google Scholar]
- 213.Rioux, P. P. 2000. Clinical trials in pharmacogenetics and pharmacogenomics: methods and applications. Am. J. Health Syst. Pharm. 57:887-898. [DOI] [PubMed] [Google Scholar]
- 214.Risch, N. J. 2000. Searching for genetic determinants in the new millennium. Nature 405:847-856. [DOI] [PubMed] [Google Scholar]
- 215.Rogers, J. F., A. N. Nafziger, and J. S. Bertino, Jr. 2002. Pharmacogenetics affects dosing, efficacy, and toxicity of cytochrome P450-metabolized drugs. Am. J. Med. 113:746-750. [DOI] [PubMed] [Google Scholar]
- 216.Romanini, D., G. Avalle, B. Farruggia, B. Nerli, and G. Pico. 1998. Spectroscopy features of the binding of polyene antibiotics to human serum albumin. Chem. Biol. Interact. 115:247-260. [DOI] [PubMed] [Google Scholar]
- 217.Romanini, D., G. Muller, and G. Pico. 2002. Use of amphotericin B as optical probe to study conformational changes and thermodynamic stability in human serum albumin. J. Protein Chem. 21:505-514. [DOI] [PubMed] [Google Scholar]
- 218.Ryder, N. S., and I. Frank. 1992. Interaction of terbinafine with human serum and serum proteins. J. Med. Vet. Mycol. 30:451-460. [DOI] [PubMed] [Google Scholar]
- 219.Sachidanandam, R., D. Weissman, S. C. Schmidt, J. M. Kakol, L. D. Stein, G. Marth, S. Sherry, J. C. Mullikin, B. J. Mortimore, D. L. Willey, S. E. Hunt, C. G. Cole, P. C. Coggill, C. M. Rice, Z. Ning, J. Rogers, D. R. Bentley, P. Y. Kwok, E. R. Mardis, R. T. Yeh, B. Schultz, L. Cook, R. Davenport, M. Dante, L. Fulton, L. Hillier, R. H. Waterston, J. D. McPherson, B. Gilman, S. Schaffner, W. J. Van Etten, D. Reich, J. Higgins, M. J. Daly, B. Blumenstiel, J. Baldwin, N. Stange-Thomann, M. C. Zody, L. Linton, E. S. Lander, and D. Altshuler. 2001. A map of human genome sequence variation containing 1.42 million single nucleotide polymorphisms. Nature 409:928-933. [DOI] [PubMed] [Google Scholar]
- 220.Sakaeda, T., T. Nakamura, M. Horinouchi, M. Kakumoto, N. Ohmoto, T. Sakai, Y. Morita, T. Tamura, N. Aoyama, M. Hirai, M. Kasuga, and K. Okumura. 2001. MDR1 genotype-related pharmacokinetics of digoxin after single oral administration in healthy Japanese subjects. Pharm. Res. 18:1400-1404. [DOI] [PubMed] [Google Scholar]
- 221.Salisbury, B. A., M. Pungliya, J. Y. Choi, R. Jiang, X. J. Sun, and J. C. Stephens. 2003. SNP and haplotype variation in the human genome. Mutat. Res. 526:53-61. [DOI] [PubMed] [Google Scholar]
- 222.Sandhu, P., W. Lee, X. Xu, B. F. Leake, M. Yamazaki, J. A. Stone, J. H. Lin, P. G. Pearson, and R. B. Kim. 2005. Hepatic uptake of the novel antifungal agent caspofungin. Drug Metab. Dispos. 33:676-682. [DOI] [PubMed] [Google Scholar]
- 223.Sanglard, D., F. Ischer, M. Monod, and J. Bille. 1996. Susceptibilities of Candida albicans multidrug transporter mutants to various antifungal agents and other metabolic inhibitors. Antimicrob. Agents Chemother. 40:2300-2305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Schafer-Korting, M. 1993. Pharmacokinetic optimisation of oral antifungal therapy. Clin. Pharmacokinet. 25:329-341. [DOI] [PubMed] [Google Scholar]
- 225.Schafer-Korting, M., H. C. Korting, W. Rittler, and W. Obermuller. 1995. Influence of serum protein binding on the in vitro activity of anti-fungal agents. Infection 23:292-297. [DOI] [PubMed] [Google Scholar]
- 226.Schinkel, A. H., and J. W. Jonker. 2003. Mammalian drug efflux transporters of the ATP binding cassette (ABC) family: an overview. Adv. Drug Deliv. Rev. 55:3-29. [DOI] [PubMed] [Google Scholar]
- 227.Schmidt, L. E., and K. Dalhoff. 2002. Food-drug interactions. Drugs 62:1481-1502. [DOI] [PubMed] [Google Scholar]
- 228.Schuetzer-Muehlbauer, M., B. Willinger, G. Krapf, S. Enzinger, E. Presterl, and K. Kuchler. 2003. The Candida albicans Cdr2p ATP-binding cassette (ABC) transporter confers resistance to caspofungin. Mol. Microbiol. 48:225-235. [DOI] [PubMed] [Google Scholar]
- 229.Schwab, M., M. Eichelbaum, and M. F. Fromm. 2003. Genetic polymorphisms of the human mdr1 drug transporter. Annu. Rev. Pharmacol. Toxicol. 43:285-307. [DOI] [PubMed] [Google Scholar]
- 230.Seidegard, J., W. R. Vorachek, R. W. Pero, and W. R. Pearson. 1988. Hereditary differences in the expression of the human glutathione transferase active on trans-stilbene oxide are due to a gene deletion. Proc. Natl. Acad. Sci. USA 85:7293-7297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Reference deleted.
- 232.Shargel, L., and A. Yu. 1999. Applied biopharmaceuticals and pharmacokinetics, 4th ed. Appleton & Lange, Stamford, Conn.
- 233.Shield, A. J., B. A. Thomae, B. W. Eckloff, E. D. Wieben, and R. M. Weinshilboum. 2004. Human catechol O-methyltransferase genetic variation: gene resequencing and functional characterization of variant allozymes. Mol. Psychiatry 9:151-160. [DOI] [PubMed] [Google Scholar]
- 234.Siber, G. R., P. Echeverria, A. L. Smith, J. W. Paisley, and D. H. Smith. 1975. Pharmacokinetics of gentamicin in children and adults. J. Infect. Dis. 132:637-651. [DOI] [PubMed] [Google Scholar]
- 235.Silverman, J. A. 1999. Multidrug-resistance transporters. Pharm. Biotechnol. 12:353-386. [DOI] [PubMed] [Google Scholar]
- 236.Smit, J. W., A. H. Schinkel, M. Muller, B. Weert, and D. K. Meijer. 1998. Contribution of the murine mdr1a P-glycoprotein to hepatobiliary and intestinal elimination of cationic drugs as measured in mice with an mdr1a gene disruption. Hepatology 27:1056-1063. [DOI] [PubMed] [Google Scholar]
- 237.Smit, J. W., A. H. Schinkel, B. Weert, and D. K. Meijer. 1998. Hepatobiliary and intestinal clearance of amphiphilic cationic drugs in mice in which both mdr1a and mdr1b genes have been disrupted. Br. J. Pharmacol. 124:416-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Soyama, A., N. Hanioka, Y. Saito, N. Murayama, M. Ando, S. Ozawa, and J. Sawada. 2002. Amiodarone N-deethylation by CYP2C8 and its variants, CYP2C8*3 and CYP2C8 P404A. Pharmacol. Toxicol. 91:174-178. [DOI] [PubMed] [Google Scholar]
- 239.Soyama, A., Y. Saito, N. Hanioka, N. Murayama, O. Nakajima, N. Katori, S. Ishida, K. Sai, S. Ozawa, and J. I. Sawada. 2001. Non-synonymous single nucleotide alterations found in the CYP2C8 gene result in reduced in vitro paclitaxel metabolism. Biol. Pharm. Bull. 24:1427-1430. [DOI] [PubMed] [Google Scholar]
- 240.Spielberg, S. P. 1996. N-Acetyltransferases: pharmacogenetics and clinical consequences of polymorphic drug metabolism. J. Pharmacokinet. Biopharm. 24:509-519. [DOI] [PubMed] [Google Scholar]
- 241.Spielman, R. S., and W. J. Ewens. 1996. The TDT and other family-based tests for linkage disequilibrium and association. Am. J. Hum. Genet. 59:983-989. [PMC free article] [PubMed] [Google Scholar]
- 242.Starke, J. R., E. O. Mason, Jr., W. G. Kramer, and S. L. Kaplan. 1987. Pharmacokinetics of amphotericin B in infants and children. J. Infect. Dis. 155:766-774. [DOI] [PubMed] [Google Scholar]
- 243.Stein, R. S., K. Albridge, R. K. Lenox, W. Ray, and J. M. Flexner. 1988. Nephrotoxicity in leukemic patients receiving empirical amphotericin B and aminoglycosides. South. Med. J. 81:1095-1099. [DOI] [PubMed] [Google Scholar]
- 244.Stone, E. A., H. B. Fung, and H. L. Kirschenbaum. 2002. Caspofungin: an echinocandin antifungal agent. Clin. Ther. 24:351-377. [DOI] [PubMed] [Google Scholar]
- 245.Stone, J. A., E. M. Migoya, L. Hickey, G. A. Winchell, P. J. Deutsch, K. Ghosh, A. Freeman, S. Bi, R. Desai, S. C. Dilzer, K. C. Lasseter, W. K. Kraft, H. Greenberg, and S. A. Waldman. 2004. Potential for interactions between caspofungin and nelfinavir or rifampin. Antimicrob. Agents Chemother. 48:4306-4314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Stracham, T., and P. R. Andrew. 1999. Human molecular genetics, 2nd ed. John Wiley & Sons Inc., New York. N.Y.
- 247.Sugar, A. M., and X. P. Liu. 2000. Effect of grapefruit juice on serum voriconazole concentrations in the mouse. Med. Mycol. 38:209-212. [DOI] [PubMed] [Google Scholar]
- 248.Sun, H., H. Dai, N. Shaik, and W. F. Elmquist. 2003. Drug efflux transporters in the CNS. Adv. Drug Deliv. Rev. 55:83-105. [DOI] [PubMed] [Google Scholar]
- 249.Suzuki, H., and Y. Sugiyama. 2002. Single nucleotide polymorphisms in multidrug resistance associated protein 2 (MRP2/ABCC2): its impact on drug disposition. Adv. Drug Deliv. Rev. 54:1311-1331. [DOI] [PubMed] [Google Scholar]
- 250.Talwalkar, J. A., R. E. Soetikno, D. L. Carr-Locke, and C. L. Berg. 1999. Severe cholestasis related to intraconazole for the treatment of onychomycosis. Am. J. Gastroenterol. 94:3632-3633. [DOI] [PubMed] [Google Scholar]
- 251.Taylor, J. G., E. H. Choi, C. B. Foster, and S. J. Chanock. 2001. Using genetic variation to study human disease. Trends Mol. Med. 7:507-512. [DOI] [PubMed] [Google Scholar]
- 252.Tirona, R. G., B. F. Leake, G. Merino, and R. B. Kim. 2001. Polymorphisms in OATP-C: identification of multiple allelic variants associated with altered transport activity among European- and African-Americans. J. Biol. Chem. 276:35669-35675. [DOI] [PubMed] [Google Scholar]
- 253.Tsai, Y. J., and H. E. Hoyme. 2002. Pharmacogenomics: the future of drug therapy. Clin. Genet. 62:257-264. [DOI] [PubMed] [Google Scholar]
- 254.Tsuji, A., and I. Tamai. 1996. Carrier-mediated intestinal transport of drugs. Pharm. Res. 13:963-977. [DOI] [PubMed] [Google Scholar]
- 255.Vadiei, K., G. Lopez-Berestein, and D. R. Luke. 1990. Disposition and toxicity of amphotericin-B in the hyperlipidemic Zucker rat model. Int. J. Obes. 14:465-472. [PubMed] [Google Scholar]
- 256.Van Aubel, R. A., R. Masereeuw, and F. G. Russel. 2000. Molecular pharmacology of renal organic anion transporters. Am. J. Physiol. Renal Physiol. 279:F216-F232. [DOI] [PubMed] [Google Scholar]
- 257.Van Bambeke, F., J. M. Michot, and P. M. Tulkens. 2003. Antibiotic efflux pumps in eukaryotic cells: occurrence and impact on antibiotic cellular pharmacokinetics, pharmacodynamics and toxicodynamics. J. Antimicrob. Chemother. 51:1067-1077. [DOI] [PubMed] [Google Scholar]
- 258.Van Der Meer, J. W., J. J. Keuning, H. W. Scheijgrond, J. Heykants, J. Van Cutsem, and J. Brugmans. 1980. The influence of gastric acidity on the bio-availability of ketoconazole. J. Antimicrob. Chemother. 6:552-554. [DOI] [PubMed] [Google Scholar]
- 259.Vermes, A., H. J. Guchelaar, and J. Dankert. 2000. Flucytosine: a review of its pharmacology, clinical indications, pharmacokinetics, toxicity and drug interactions. J. Antimicrob. Chemother. 46:171-179. [DOI] [PubMed] [Google Scholar]
- 260.Vestberg, K., M. Galliano, L. Minchiotti, and U. Kragh-Hansen. 1992. High-affinity binding of warfarin, salicylate and diazepam to natural mutants of human serum albumin modified in the C-terminal end. Biochem. Pharmacol. 44:1515-1521. [DOI] [PubMed] [Google Scholar]
- 261.Vickers, A. E., J. R. Sinclair, M. Zollinger, F. Heitz, U. Glanzel, L. Johanson, and V. Fischer. 1999. Multiple cytochrome P-450s involved in the metabolism of terbinafine suggest a limited potential for drug-drug interactions. Drug Metab. Dispos. 27:1029-1038. [PubMed] [Google Scholar]
- 262.Vincent, S., R. Planells, C. Defoort, M. C. Bernard, M. Gerber, J. Prudhomme, P. Vague, and D. Lairon. 2002. Genetic polymorphisms and lipoprotein responses to diets. Proc. Nutr. Soc. 61:427-434. [DOI] [PubMed] [Google Scholar]
- 263.Wacholder, S., S. Chanock, M. Garcia-Closas, L. El Ghormli, and N. Rothman. 2004. Assessing the probability that a positive report is false: an approach for molecular epidemiology studies. J. Natl. Cancer Inst. 96:434-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Wacholder, S., N. Rothman, and N. Caporaso. 2000. Population stratification in epidemiologic studies of common genetic variants and cancer: quantification of bias. J. Natl. Cancer Inst. 92:1151-1158. [DOI] [PubMed] [Google Scholar]
- 265.Walsh, T. J., P. C. Adamson, N. L. Seibel, P. M. Flynn, M. N. Neely, C. Schwartz, A. Shad, S. L. Kaplan, M. M. Roden, J. A. Stone, A. Miller, S. K. Bradshaw, S. X. Li, C. A. Sable, and N. A. Kartsonis. 2005. Pharmacokinetics, safety, and tolerability of caspofungin in children and adolescents. Antimicrob. Agents Chemother. 49:4536-4545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Walsh, T. J., P. Whitcomb, S. Piscitelli, W. D. Figg, S. Hill, S. J. Chanock, P. Jarosinski, R. Gupta, and P. A. Pizzo. 1997. Safety, tolerance, and pharmacokinetics of amphotericin B lipid complex in children with hepatosplenic candidiasis. Antimicrob. Agents Chemother. 41:1944-1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Wang, E. J., K. Lew, C. N. Casciano, R. P. Clement, and W. W. Johnson. 2002. Interaction of common azole antifungals with P glycoprotein. Antimicrob. Agents Chemother. 46:160-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Wasan, K. M. 1996. Modifications in plasma lipoprotein concentration and lipid composition regulate the biological activity of hydrophobic drugs. J. Pharmacol. Toxicol. Methods 36:1-11. [DOI] [PubMed] [Google Scholar]
- 269.Wasan, K. M., and S. M. Cassidy. 1998. Role of plasma lipoproteins in modifying the biological activity of hydrophobic drugs. J. Pharm. Sci. 87:411-424. [DOI] [PubMed] [Google Scholar]
- 270.Wasan, K. M., A. L. Kennedy, S. M. Cassidy, M. Ramaswamy, L. Holtorf, J. W. Chou, and P. H. Pritchard. 1998. Pharmacokinetics, distribution in serum lipoproteins and tissues, and renal toxicities of amphotericin B and amphotericin B lipid complex in a hypercholesterolemic rabbit model: single-dose studies. Antimicrob. Agents Chemother. 42:3146-3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Wasan, K. M., M. Ramaswamy, S. M. Cassidy, M. Kazemi, F. W. Strobel, and R. L. Thies. 1997. Physical characteristics and lipoprotein distribution of liposomal nystatin in human plasma. Antimicrob. Agents Chemother. 41:1871-1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Watanabe, H., U. Kragh-Hansen, S. Tanase, K. Nakajou, M. Mitarai, Y. Iwao, T. Maruyama, and M. Otagiri. 2001. Conformational stability and warfarin-binding properties of human serum albumin studied by recombinant mutants. Biochem. J. 357:269-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Weinshilboum, R. 2003. Inheritance and drug response. N. Engl. J. Med. 348:529-537. [DOI] [PubMed] [Google Scholar]
- 274.Weinshilboum, R. 1989. Methyltransferase pharmacogenetics. Pharmacol. Ther. 43:77-90. [DOI] [PubMed] [Google Scholar]
- 275.Weinshilboum, R. M., D. M. Otterness, and C. L. Szumlanski. 1999. Methylation pharmacogenetics: catechol O-methyltransferase, thiopurine methyltransferase, and histamine N-methyltransferase. Annu. Rev. Pharmacol. Toxicol. 39:19-52. [DOI] [PubMed] [Google Scholar]
- 276.White, T. C. 1997. Increased mRNA levels of ERG16, CDR, and MDR1 correlate with increases in azole resistance in Candida albicans isolates from a patient infected with human immunodeficiency virus. Antimicrob. Agents Chemother. 41:1482-1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.White, T. C., K. A. Marr, and R. A. Bowden. 1998. Clinical, cellular, and molecular factors that contribute to antifungal drug resistance. Clin. Microbiol. Rev. 11:382-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Widersten, M., W. R. Pearson, A. Engstrom, and B. Mannervik. 1991. Heterologous expression of the allelic variant mu-class glutathione transferases mu and psi. Biochem. J. 276:519-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Wijnholds, J., E. C. deLange, G. L. Scheffer, D. J. van den Berg, C. A. Mol, M. van der Valk, A. H. Schinkel, R. J. Scheper, D. D. Breimer, and P. Borst. 2000. Multidrug resistance protein 1 protects the choroid plexus epithelium and contributes to the blood-cerebrospinal fluid barrier. J. Clin. Investig. 105:279-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Wildfeuer, A., J. Faergemann, H. Laufen, G. Pfaff, T. Zimmermann, H. P. Seidl, and P. Lach. 1994. Bioavailability of fluconazole in the skin after oral medication. Mycoses 37:127-130. [DOI] [PubMed] [Google Scholar]
- 281.Willems, L., R. van der Geest, and K. de Beule. 2001. Itraconazole oral solution and intravenous formulations: a review of pharmacokinetics and pharmacodynamics. J. Clin. Pharm. Ther. 26:159-169. [DOI] [PubMed] [Google Scholar]
- 282.Williams, M. P., J. Sercombe, M. I. Hamilton, and R. E. Pounder. 1998. A placebo-controlled trial to assess the effects of 8 days of dosing with rabeprazole versus omeprazole on 24-h intragastric acidity and plasma gastrin concentrations in young healthy male subjects. Aliment. Pharmacol. Ther. 12:1079-1089. [DOI] [PubMed] [Google Scholar]
- 283.Winkelmann, B. R., and J. Hager. 2000. Genetic variation in coronary heart disease and myocardial infarction: methodological overview and clinical evidence. Pharmacogenomics 1:73-94. [DOI] [PubMed] [Google Scholar]
- 284.Wright, R. M., and R. W. Warpula. 2004. Geriatric pharmacology: safer prescribing for the elderly patient. J. Am. Podiatr Med. Assoc. 94:90-97. [DOI] [PubMed] [Google Scholar]
- 285.Xie, C. X., L. T. Piecoro, and D. P. Wermeling. 1997. Gender-related considerations in clinical pharmacology and drug therapeutics. Crit. Care Nurs. Clin. N. Am. 9:459-468. [PubMed] [Google Scholar]
- 286.Yeganeh, M. H., and A. J. McLachlan. 2002. In-vitro distribution of terbinafine in rat and human blood. J. Pharm. Pharmacol. 54:277-281. [DOI] [PubMed] [Google Scholar]
- 287.Yuasa, I., S. Weidinger, K. Umetsu, K. Suenaga, G. Ishimoto, B. C. Eap, J. C. Duche, and P. Baumann. 1993. Orosomucoid system: 17 additional orosomucoid variants and proposal for a new nomenclature. Vox Sang. 64:47-55. [DOI] [PubMed] [Google Scholar]
- 288.Zhang, L., C. M. Brett, and K. M. Giacomini. 1998. Role of organic cation transporters in drug absorption and elimination. Annu. Rev. Pharmacol. Toxicol. 38:431-460. [DOI] [PubMed] [Google Scholar]
- 289.Zollner, G., P. Fickert, R. Zenz, A. Fuchsbichler, C. Stumptner, L. Kenner, P. Ferenci, R. E. Stauber, G. J. Krejs, H. Denk, K. Zatloukal, and M. Trauner. 2001. Hepatobiliary transporter expression in percutaneous liver biopsies of patients with cholestatic liver diseases. Hepatology 33:633-646. [DOI] [PubMed] [Google Scholar]