Abstract
Major trauma induces marked metabolic changes which contribute to the systemic immune suppression in severely injured patients and increase the risk of infection and posttraumatic organ failure. The hypercatabolic state of polytrauma patients must be recognized early and treated by an appropriate nutritional management in order to avoid late complications. Clinical studies in recent years have supported the concept of "immunonutrition" for severely injured patients, which takes into account the supplementation of Ω-3 fatty acids and essential aminoacids, such as glutamine. Yet many aspects of the nutritional strategies for polytrauma patients remain controversial, including the exact timing, caloric and protein amount of nutrition, choice of enteral versus parenteral route, and duration. The present review will provide an outline of the pathophysiological metabolic changes after major trauma that endorse the current basis for early immunonutrition of polytrauma patients.
Introduction
Severe trauma induces massive changes of the physiological state by alteration of metabolic pathways and activation of the innate immune system [1-5]. The posttraumatic metabolic changes are characterized by hypermetabolism with increased energy expenditure, enhanced protein catabolism, insulin resistance associated with hyperglycemia, failure to tolerate glucose load, and high plasma insulin levels ("traumatic diabetes") [1,2,6-11]. The alterations of the physiological metabolic pathways leads to the development of hyperglycemia and metabolic acidosis with hyperlactatemia [10,12]. The increased oxygen demands of the polytraumatized patient further aggravate the hypermetabolic state by enhanced mitochondrial oxygen utilization [1,10,13,14].
Metabolic changes after trauma were described more than six decades ago by Cuthbertson (Lancet 1942, 1:433–437) and characterized as occurring in two different phases, termed the "ebb" phase and the "flow" phase (table 1). The "ebb" phase is initiated within minutes after trauma and persists for several hours after the initial insult. It is characterized by a decline in body temperature and oxygen consumption, aimed at reducing posttraumatic energy depletion. However, the brief duration of this phase limits its clinical relevance. The "flow" phase, which occurs after compensation of the state of traumatic-hemorrhagic shock, is associated with an increased metabolic turnover, activation of the innate immune system and induction of the hepatic acute-phase response [2,3]. This results in an increase of the catabolic state with a significantly increased consumption of energy and oxygen [2,10,13,14]. The amount of oxygen consumption and demand in patients with traumatic-hemorrhagic shock can be calculated using a formula described by Nunn and Freeman in 1964 (table 2) [15].
Table 1.
Metabolic changes after major trauma.
| "Ebb" phase (hours) | "Flow" phase (days to weeks) |
| Decreased body temperature | Increased body temperature |
| Decreased oxygen consumption | Increased oxygen consumption |
| Lactate acidosis | Negative nitrogen balance |
| Increased stress hormone levels | Increased stress hormone levels |
| Decreased insulin levels | Normal to increased insulin levels |
| Hyperglycaemia, insulin resistance | Hyperglycaemia, insulin resistance |
| Gluconeogenesis | Gluconeogenesis |
| Increased substrate consumption | Proteinolysis ("autocannibalism") |
| Hepatic acute-phase response | Lipolysis |
| Immune activation | Immunosuppression |
Table 2.
Calculation of available oxygen (O2av in ml/min) in bleeding polytrauma patients according to the formula described by Nunn and Freeman in 1964 [15].
| O2av = CO × SaO2 × Hb × 1.34 |
[CO, cardiac output (ml/min); SaO2, arterial oxygen saturation (%); Hb, hemoglobin concentration (g%); 1.34, O2 binding capacity constant (ml O2/g Hb)].
In addition to the acute hypermetabolic state, the systemic inflammatory cascade is initiated as a consequence of trauma, as characterized by the release of pro-inflammatory cytokines and activation of the complement system [4,5,16,17]. The bacterial translocation caused by the traumatic-hemorrhagic shock may further aggravate these metabolic sequelae and inflammatory response [5,10,17-19], but this issue remains controversial [20]. Additionally, the frequent use of vasoactive drug therapy for hemodynamic resuscitation in traumatic-hemorrhagic shock has a profound impact on metabolism and organ energy status of the injured patient [1,10]. Most severely injured patients require inotropic support to promote hemodynamic stability. For example dopamine, a commonly used epinephrine precursor, leads to depression of pituitary function and inhibition of prolactin and growth hormone production [21]. Thus, the use of vasoactive drugs further promotes catabolism by reducing serum levels of anabolic hormones. In contrast, endogenous catecholamines, cortisol and glucagon levels are highly elevated after trauma, leading to increased energy substrate mobilization [3,6]. Interestingly, studies in severe burn patients have shown that exogenous insulin administration can attentuate protein catabolism as indicated by an increase in protein synthesis [11,22,23]. Proteinolysis of skeletal muscle and glycolysis are increased with the aim to provide the substrates for the hepatic gluconeogenesis and the hepatic biosynthesis of acute-phase proteins [2,24]. The metabolic state is reoriented towards supporting the organism's immune response and wound healing at the cost of enhanced proteinolysis of skeletal muscle [1,2]. In addition, the physical and psychological stimulation of the neuroendocrine axis through fear, stress, pain, inflammation and shock increases the caloric turnover significantly above the baseline situation in healthy individuals [6,10]. This leads to increased serum levels of catabolic hormones, such as cortisol, glucagon and catecholamines, and decreased levels of insulin causing the posttraumatic catabolic diabetic phase [10,11,25]. In contrast, the phenomenon of "occult adrenal insufficiency" has been demonstrated to occur in severely injured patients in the ICU, as defined by a serum cortisol below 18 mg/dL [26] or below 25 mg/dL [27] in different publications. However, up to present the clinical implication of posttraumatic adrenal failure with regard to patient outcome remains controversial [26-29].
Depending on the severity of the initial injury and the quality of the therapeutic regimen for the polytraumatized patients, catabolic changes in posttraumatic metabolism can last for several days or weeks [3].
Metabolic control and immunonutrition
The state of hypercatabolism after severe injury can lead to severe complications associated with posttraumatic hyperglycemia, hypoproteinemia, lactate acidosis, and immunosuppression [2,8,10]. Thus, the presence and significance of these metabolic alterations must be recognized and appreciated in severely injured patients. An optimal therapeutic regimen should include the concept of a "metabolic control" in addition to the initial measures of resuscitation by hemorrhage control and securing airways and oxygenation [2,30,31]. The posttraumatic catabolic state requires an adjusted energetic balance with early protein substitution and hypercaloric nutrition [2,8,30,31]. Patients with major injuries who receive no nutrition during the first few days after trauma can develop cumulative caloric and protein deficits which contribute to the risk of increased complications, such as infections and organ failure [2,8,32]. Consequently, clinical pathways and algorithms for nutritional support of severely injured patients during the intensive care period have been developed in recent years [8,10,12,30,31,33]. These protocols are designed to restore the capacity for optimal immune and inflammatory responses and to facilitate the recovery and healing from trauma and subsequent infections. Early enteral nutrition has been advocated as the concept of choice for nutrition of polytraumatized and severely ill patients. In this regard, prospective randomized controlled trials have clearly demonstrated the positive effect of an early full enteral nutrition with a decreased posttraumatic infection rate, a shorter duration of hospital stay, and an improved overall outcome [32,34-42].
The specialized nutritional support for severely injured patients includes the administration of "immune nutrient cocktails" which have been shown to improve the survival of septic patients during the intensive care period [33,43]. The concept of "immunonutrition" has been established in recent years and exemplified by the enteral supplementation of glutamine, one of the most promising new nutritional concepts for severely injured patients in recent years [32,37,44-47]. Glutamine is an essential aminoacid which exerts metabolic benefits beyond its nutritional value by mediating immunological effects, such as induction of neutrophil phagocytic activity and oxidative burst [32,48,49]. Glutamine was also shown to protect neutrophils from undergoing apoptosis in vivo [50]. In addition, glutamine is a precursor to the reducing agent glutathione and thus contributes to antioxidant effects and cellular protection from ischemia/reperfusion-mediated injury [45,51]. This protective effect of glutamine has been demonstrated in different experimental models of ischemia/reperfusion injury [52,53]. Also, models of experimental starvation have shown the important nutritional effect of glutamine for enterocytes and intestinal mucosa [8]. Furthermore, glutamine has been shown to restore cellular energy reserves to normal levels after hemorrhagic shock and to attenuate the extent of shock-induced cellular apoptosis [54]. This finding is supported by reduced bacterial translocation in rat guts and improved gut immune function after diet supplementation with glutamine [45]. A prospective, randomized, double-blind controlled clinical trial demonstrated that glutamine supplementation reduces the incidence of multiple organ failure and death attributed to infections in critically ill patients [32]. In addition to glutamine, Ω-3 fatty acids have become an important nutritional supplementation for severely injured patients in recent years [55-57]. These long-chain polyunsaturated fatty acids derived from fish oil were shown to exert potent anti-inflammatory properties in trauma patients, such as attenuation of arachidonic acid-derived metabolites like prostaglandin PGE2 and leukotriene LTB4, inhibition of leukocyte activation and chemotaxis, and attenuation of pro-inflammatory gene expression levels [39,57-59].
Other nutritional supplements that promote anabolism in trauma patients include phospholipids, leptins, and anabolic hormones, such as thyroid hormones, growth hormone, and insulin [8,22,23,60,61]. For example, growth hormone substitution has been shown to promote protein anabolism in severely injured patients [62].
Recently published consensus guidelines based on meta-analyses from multiple prospective trials have helped clarify the indication for supplementation of specific nutrients in the clinical setting [31,44,63-65]. Moreover, the use of vasoactive therapy has been shown to influence not only the systemic and regional perfusion and organ blood flow, but also to affect the balance between oxygen and substrate supply [66]. The use and necessity of exogenous catecholamines should therefore be well calculated and balanced against the potential adverse influence on metabolic needs during the catabolic phase of critically ill trauma patients. Furthermore, there is evolving evidence that over-resuscitation, i.e. driving oxygen delivery to supraphysiological levels, may be deleterious [67].
Clinical implications for severely injured patients
Although several studies have shown the positive effect of immunonutrition, its clinical impact remains debated, and the benefit may be specific to certain patient populations [68-70]. Despite this lack of consensus, the concept of early enteral feeding is generally accepted among trauma surgeons and intensive care physicians [32,34-42]. More than a decade ago, Moore and colleagues demonstrated in prospective randomized trials on patients with abdominal injuries [71] the positive effect of early enteral nutrition with a significant reduction of intraabdominal and pulmonary infections [34-36,72]. When compared to total parenteral nutrition, the enteral route is associated with a significantly decreased incidence of septic complications [39]. Although anecdotal reports have been published on the adverse effects and complications of enteral feeding procedures in critically ill patients [73], the overall consensus in the literature clearly advocates for the positive effects of early enteral nutrition in severely injured patients [31,42,43,68,72,74,75]. An issue under debate in clinical practice is the question of when early immunonutrition should be initiated [65]. This question has not been fully adressed in the current literature and requires further analysis with future clinical trials [76].
In daily clinical practice, the individual caloric requirement for severely injured patients should be assessed with defined algorithms, tables and equations. For example, the method of indirect calorimetry by the Weir equation helps to assess the energy expenditure by the parameters oxygen consumption and carbon dioxide production [7,77]. The basic metabolic rate can be calculated by the Harris-Benedict equation using the standard variables of height, weight, age and gender [7,78]. However, it is of key importance not to "overfeed" critically injured patients with calories, since this may contribute to adverse outcome [1,39,79,80]. Early overfeeding of severely injured patients leads to an increase in overall oxygen consumption, carbon dioxide production, hepatic lipogenesis, and hyperglycemia, and thus contributes to secondary immune suppression during the ICU phase [80]. Obese patients are particularly susceptible to the adverse effects of overfeeding. Therefore, a hypocaloric (<20 kcal/kg/day), high-protein nutrition was postulated as a safe protocol for critically injured obese patients and shown to be as effective as eucaloric or hypercaloric feeding (>20 kcal/kg/day) in this specific patient group [81-83]. Current feeding recommendations for morbidly obese ICU patients are about 20 kcal and 2 g of protein per kg ideal body weight per day [83].
The standard daily doses of protein, glucose, fat and amino acid concentrations must be clearly defined and adjusted to the calculated individual patients metabolic needs [77-80,83,84]. An example of a standardized enteral nutrition is Impact®; one of the most commonly used clinical formulas. Multicenter prospective randomized clinical trials on critically ill trauma patients have demonstrated that the administration of Impact® for 7 to 10 days reduced the rates of infection, wound complications, and the risk of multiple organ failure [36,72,75]. Nonetheless, standardized enteral nutrition is not consistently administered to critically ill trauma patients. International clinical guidelines for nutritional support in critically ill patients have been published by the American Society of Parenteral and Enteral Nutrition (ASPEN), the Canadian Society for Clinical Nutrition and more recently the European Society of Parenteral and Enteral Nutrition (ESPEN) [76,85,86].
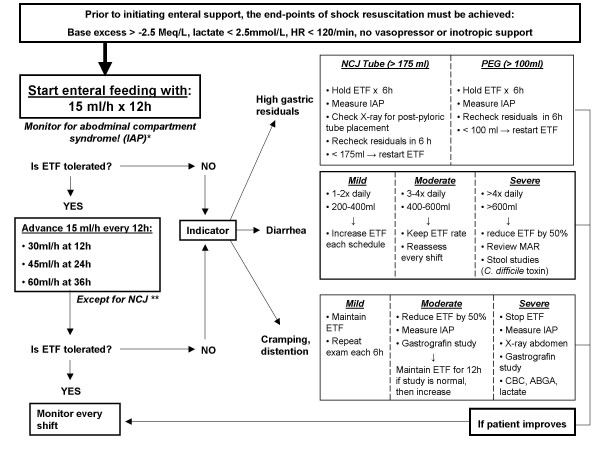
A review by Wernerman provides a detailed analysis of the weaknesses and strengths of the respective recommendations for nutritional support of critically ill patients [87]. Altogether, the guidelines clearly favor the concept of early enteral nutrition within 24–48 hours after admission in the intensive care unit [87]. For daily use in clinical practice, the reader is referred to the published clinical guidelines for nutritional support [39,76,85,86]. The main recommendations derived from the ESPEN guidelines are summarized in table 3. Furthermore, our own institutional protocol for nutritional support of severely injured patients is shown in figure 1. The clinical value of these guidelines is awaiting scientific validation by implementation in future prospective randomized trials.
Table 3.
Summary of the main recommendations from the ESPEN guidelines for enteral nutrition of critically ill patients. Adapted from: [76].
| Recommendations | |
| Indications and application of enteral nutrition (EN) | All patients who are not expected to be on a full oral diet within three days. |
| The expert committee recommends that haemodynamically stable critically ill patients who have a functioning gastrointestinal tract should be fed early (<24 h) using an appropriate amount of nutrition. | |
| Exogenous energy supply (kcal): | |
| • 20–25 kcal/kg body weight/day during the acute and initial phase of critical illness. | |
| • 25–30 kcal/kg body weight/day during the anabolic recovery phase, | |
| Consider parenteral administration of metoclopramide or erythromycin in patients with intolerance to enteral feeding (e.g. with high gastric residuals). | |
| Route of administration | Use EN in all patients who can be fed via the enteral route. |
| There is no significant difference in the efficacy of jejunal versus gastric feeding in critically ill patients. | |
| Avoid additional parenteral nutrition in patients who tolerate EN and can be fed to the target values. | |
| Consider careful parenteral nutrition in patients intolerant to EN. | |
| Type of formula | Whole protein formulae are appropriate in most patients, since peptide-based formulae have not shown clinical advantages. |
| "Immunonutrition": | |
| Glutamine should be added to standard enteral formula in all trauma patients and burn patients. | |
| Formulae enriched with nucleotides and fatty acids are superior to standard enteral formulae in trauma patients, patients with ARDS, and patients with mild, but not severe, sepsis (APACHE II score < 15) | |
| Patients with very severe illness who do not tolerate more than 700 ml enteral formulae per day should not receive an immune-modulating formula. |
Figure 1.
Denver Health Medical Center institutional protocol for early enteral nutrition of severely injured patients. Adapted from: [39]. Abbreviations: ABGA, arterial blood gas analysis; ATI, Abdominal Trauma Index; CBC, complete blood count; HR, heart rate; ETF, enteral tube feeding; IAP, intraabdominal pressure (bladder pressure); ISS, Injury Severity Score; MAR, medicine administration record; NCJ, needle catheter jejunostomy; PEG, percutaneous endoscopic gastrostomy; PRBC, packed red blood cells. * Monitoring of IAP for high risk patients with severe pelvic ring injuries, lumbar spine fractures, polytrauma with ISS > 17, hemorrhagic shock with > 6 units PRBC in 12 h. ** In massively injured patients (ISS>40, ATI>40, PRBC mass transfusions), administer low dose enteral feeding (15–30 ml/h) for the first 3 days due to anticipated intolerance to full-dose enteral feeding. Advance per protocol on the 4th day post injury.
Conclusion
Dramatic metabolic changes occur in severely injured patients which must be acknowledged early and monitored during the posttraumatic phase. Appropriate immunonutrition should be started in the ICU, preferably by enteral route, in order to counteract the potentially devastating effects of the massive hypermetabolic state after major trauma. Recently published international guidelines on enteral nutrition concepts in critically ill patients are available for implementation in clinical practice and future prospective studies.
Competing interests
None.
Authors' contributions
EH, AW, IL, SJM, WRS, EEM, and PFS contributed equally to the conception and design, literature appraisal and writing of this manuscript. The final version of this paper was approved by all authors.
Acknowledgments
Acknowledgements
PFS is supported by grants from the German Research Foundation (DFG) No. STA635/1-1, STA635/1-2, STA635/2-1, STA635/2-2 and TR742/1-1.
Contributor Information
Erik Hasenboehler, Email: Erik.Hasenboehler@dhha.org.
Allison Williams, Email: Allison.Williams@dhha.org.
Iris Leinhase, Email: Iris.Leinhase@charite.de.
Steven J Morgan, Email: Steven.Morgan@dhha.org.
Wade R Smith, Email: Wade.Smith@dhha.org.
Ernest E Moore, Email: Ernest.Moore@dhha.org.
Philip F Stahel, Email: Philip.Stahel@dhha.org.
References
- Plank LD, Hill GL. Energy balance in critical illness. Proc Nutr Soc. 2003;62:545–552. doi: 10.1079/PNS2003259. [DOI] [PubMed] [Google Scholar]
- Griffiths RD, Hinds CJ, Little RA. Manipulating the metabolic response to injury. Brit Med Bull. 1999;55:181–195. doi: 10.1258/0007142991902204. [DOI] [PubMed] [Google Scholar]
- Keel M, Trentz O. Pathophysiology of polytrauma. Injury. 2005;36:691–709. doi: 10.1016/j.injury.2004.12.037. [DOI] [PubMed] [Google Scholar]
- Schlag G, Redl H. Mediators of injury and inflammation. World J Surg. 1996;20:406–410. doi: 10.1007/s002689900064. [DOI] [PubMed] [Google Scholar]
- Redl H, Bahrami S, Fürst W, Schiesser A, Schlag G, Mollnes TE. Evidence for early bacteremia/endotoxemia and inflammatory responses after trauma: hemorrhage and complement activation in a nonhuman primate model. Eur J Trauma. 2000;26:300–307. doi: 10.1007/PL00002455. [DOI] [Google Scholar]
- Frankenfield DC, Wiles CEIII, Bagley S, Siegel JH. Relationships between resting and total energy expenditure in injured and septic patients. Crit Care Med. 1994;22:1796–1804. [PubMed] [Google Scholar]
- Branson RD, Johanniqman JA. The measurement of energy expenditure. Nutr Clin Pract. 2004;19:622–636. doi: 10.1177/0115426504019006622. [DOI] [PubMed] [Google Scholar]
- Lavery GG, Glover P. The metabolic and nutritional response to critical illness. Curr Opin Crit Care. 2000;6:233–238. doi: 10.1097/00075198-200008000-00001. [DOI] [PubMed] [Google Scholar]
- Weekers F, Giulietti AP, Michalaki M, Coopmans W, Van Herck E, Mathieu C, Van den Berghe G. Metabolic, endocrine, and immune effects of stress hyperglycemia in a rabbit model of prolonged critical illness. Endocrinology. 2003;144:5329–5338. doi: 10.1210/en.2003-0697. [DOI] [PubMed] [Google Scholar]
- Träger K, DeBacker D, Radermacher P. Metabolic alterations in sepsis and vasoactive drug-related metabolic effects. Curr Opin Crit Care. 2003;9:271–278. doi: 10.1097/00075198-200308000-00004. [DOI] [PubMed] [Google Scholar]
- Jeschke MG, Klein M, Herndon DH. Insulin treatment improves the systemic inflammatory reaction to severe trauma. Ann Surg. 2004;239:553–560. doi: 10.1097/01.sla.0000118569.10289.ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levraut J, Grimaud D. Treatment of metabolic acidosis. Curr Opin Crit Care. 2003;9:260–265. doi: 10.1097/00075198-200308000-00002. [DOI] [PubMed] [Google Scholar]
- Edwards JD, Redmond AD, Nightingale P, Wilkins RG. Oxygen consumption following trauma: a reappraisal in severely injured patients requiring mechanical ventilation. Br J Surg. 1988;75:690–692. doi: 10.1002/bjs.1800750722. [DOI] [PubMed] [Google Scholar]
- Rixen D, Siegel JH. Metabolic correlates of oxygen debt predict posttrauma early acute respiratory distress syndrome and the related cytokine response. J Trauma. 2000;49:392–403. doi: 10.1097/00005373-200009000-00003. [DOI] [PubMed] [Google Scholar]
- Nunn JF, Freeman J. Problems of oxygenation and oxygen transport during haemorrhage. Anaesthesia. 1964;19:206–216. doi: 10.1111/j.1365-2044.1964.tb00367.x. [DOI] [PubMed] [Google Scholar]
- Stahel PF, Morganti-Kossmann MC, Kossmann T. The role of the complement system in traumatic brain injury. Brain Res Rev. 1998;27:243–256. doi: 10.1016/S0165-0173(98)00015-0. [DOI] [PubMed] [Google Scholar]
- Ertel W, Keel M, Marty D, Hoop R, Safret A, Stocker R, Trentz O. Significance of systemic inflammation in 1,278 trauma patients. Unfallchirurg. 1998;101:520–526. doi: 10.1007/s001130050304. [DOI] [PubMed] [Google Scholar]
- Bauer C, Kuntz W, Bauer M, Larsen R, Marzi I. Evidence for a sustained inflammatory response of the hepatic microcirculation after hemorrhagic shock. Eur J Trauma. 2000;26:176–184. doi: 10.1007/PL00002441. [DOI] [Google Scholar]
- Hietbrink F, Koenderman L, Rijkers GT, Leenen LPH. Trauma: the role of the innate immune system. World J Emerg Surg. 2006;1:15. doi: 10.1186/1749-7922-1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore FA, Moore EE, Poggetti R, McAnena OJ, Peterson VM, Abernathy CM, Parsons PE. Gut bacterial translocation via the portal vein: a clinical perspective with major torso trauma. J Trauma. 1991;31:629–636. doi: 10.1097/00005373-199105000-00006. [DOI] [PubMed] [Google Scholar]
- Van den Berghe G, de Zegher F. Anterior pituitary function during critical illness and dopamine treatment. Crit Care Med. 1996;24:1580–1590. doi: 10.1097/00003246-199609000-00024. [DOI] [PubMed] [Google Scholar]
- Sakurai Y, Aarsland A, Herndon DN, Chinkes DL, Pierre E, Nguyen TT, Patterson BW, Wolfe RR. Stimulation of muscle protein synthesis by long-term insulin infusion in severely burned patients. Ann Surg. 1995;222:283–94; 294-7. doi: 10.1097/00000658-199509000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrando AA, Chinkes DL, Wolf SE, Matin S, Herndon DN, Wolfe RR. A submaximal dose of insulin promotes net skeletal muscle protein synthesis in patients with severe burns. Ann Surg. 1999;229:11–18. doi: 10.1097/00000658-199901000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahn MS, Mitchell RA, Lange MP, Smith S, Jacobs LA. Hepatic metabolic response to injury and sepsis. Surgery. 1995;117:520–530. doi: 10.1016/S0039-6060(05)80251-X. [DOI] [PubMed] [Google Scholar]
- Jeschke MG, Barrow RE, Mlcak RP, Herndon DN. Endogenous anabolic hormones and hypermetabolism: effect of trauma and gender differences. Ann Surg. 2005;241:759–768. doi: 10.1097/01.sla.0000161028.43338.cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Offner PJ, Moore EE, Ciesla D. The adrenal response after severe trauma. Am J Surg. 2002;184:649–653. doi: 10.1016/S0002-9610(02)01101-7. [DOI] [PubMed] [Google Scholar]
- Gannon TA, Britt RC, Weireter LJ, Cole FJ, Collins JN, Britt LD. Adrenal insufficiency in the critically ill trauma population. Am Surg. 2006;72:373–376. [PubMed] [Google Scholar]
- Duggan M, Browne I, Flynn C. Adrenal failure in the critically ill. Br J Anaesth. 1998;81:468–470. doi: 10.1093/bja/81.3.468. [DOI] [PubMed] [Google Scholar]
- Baldwin WA, Allo M. Occult hypoadrenalism in critically ill patients. Arch Surg. 1993;128:673–676. doi: 10.1001/archsurg.1993.01420180075014. [DOI] [PubMed] [Google Scholar]
- Prelack K, Sheridan RL. Micronutrient supplementation in the critically ill patient: strategies for clinical practice. J Trauma. 2001;51:601–620. doi: 10.1097/00005373-200109000-00037. [DOI] [PubMed] [Google Scholar]
- Slone DS. Nutritional support for the critically ill and injured patient. Crit Care Clin. 2004;20:135–157. doi: 10.1016/S0749-0704(03)00093-9. [DOI] [PubMed] [Google Scholar]
- Grifftiths RD, Allen KD, Andrews FJ, Jones C. Infection, multiple organ failure, and survival in the intensive care unit: influence of glutamine-supplemented parenteral nutrition on acquired infection. Nutrition. 2002;18:546–552. doi: 10.1016/S0899-9007(02)00817-1. [DOI] [PubMed] [Google Scholar]
- Griffiths RD. Specialized nutrition support in critically ill patients. Curr Opin Crit Care. 2003;9:249–259. doi: 10.1097/00075198-200308000-00001. [DOI] [PubMed] [Google Scholar]
- Moore EE, Jones TN. Benefits of immediate jejunostomy feeding after major abdominal trauma - a prospective randomized study. J Trauma. 1986;26:874–881. doi: 10.1097/00005373-198610000-00003. [DOI] [PubMed] [Google Scholar]
- Moore FA, Moore EE, Jones TN, McCroskey BL, Peterson VM. TEN vs. TPN following major abdominal trauma - reduced septic morbidity. J Trauma. 1989;29:916–922. doi: 10.1097/00005373-198907000-00003. [DOI] [PubMed] [Google Scholar]
- Moore FA, Moore EE, Kudsk KA, Brown RO, Bower RH, Koruda MJ, Baker CC, Barbul A. Clinical benefits of an immune-enhancing diet for early postinjury enteral feeding. J Trauma. 1994;37:607–615. doi: 10.1097/00005373-199410000-00014. [DOI] [PubMed] [Google Scholar]
- Jones C, Palmer TE, Griffiths RD. Randomized clinical outcome study of critically ill patients given glutamine-supplemented enteral nutrition. Nutrition. 1999;15:108–115. doi: 10.1016/S0899-9007(98)00172-5. [DOI] [PubMed] [Google Scholar]
- Taylor SJ, Fettes SB, Jewkes C, Nelson RJ. Prospective, randomized controlled trial to determine the effect of early enhanced enteral nutrition on clinical outcome in mechanically ventilated patients suffering head injury. Crit Care Med. 1999;27:2525–2531. doi: 10.1097/00003246-199911000-00033. [DOI] [PubMed] [Google Scholar]
- Biffl WL, Moore EE, Haenel JB. Nutrition support of the trauma patient. Nutrition. 2002;18:960–965. doi: 10.1016/S0899-9007(02)00987-5. [DOI] [PubMed] [Google Scholar]
- Spain DA. When is the seriously ill patient ready to be fed? JPEN J Parenter Enteral Nutr. 2002;26:S62–5; discussion S65-8. doi: 10.1177/014860710202600610. [DOI] [PubMed] [Google Scholar]
- Schmidt H, Martindale R. The gastrointestinal tract in critical illness: nutritional implications. Curr Opin Clin Nutr Metab Care. 2003;6:587–591. doi: 10.1097/00075197-200309000-00014. [DOI] [PubMed] [Google Scholar]
- Zaloga GP, Knowles R, Black KW, Prielipp R. Total parenteral nutrition increases mortality after hemorrhage. Crit Care Med. 1991;19:54–59. doi: 10.1097/00003246-199101000-00015. [DOI] [PubMed] [Google Scholar]
- Galban C, Montejo JC, Mesejo A, Marco P, Celaya S, Sanchez-Segura JM, Farre M, Bryg DJ. An immune-enhancing enteral diet reduces mortality rate and episodes of bacteremia in septic intensive care unit patients. Crit Care Med. 2000;28:643–648. doi: 10.1097/00003246-200003000-00007. [DOI] [PubMed] [Google Scholar]
- Heyland DK, Novak F, Drover JW, Jain M, Su X, Suchner U. Should immunonutrition become routine in critically ill patients? A systematic review of the evidence. Jama. 2001;286:944–953. doi: 10.1001/jama.286.8.944. [DOI] [PubMed] [Google Scholar]
- Wernerman J. Glutamine and acute illness. Curr Opin Crit Care. 2003;9:279–285. doi: 10.1097/00075198-200308000-00005. [DOI] [PubMed] [Google Scholar]
- Minard G, Janu P. Status and clinical utility of pharmaconutrients. Curr Opin Crit Care. 1996;2:253–259. [Google Scholar]
- Montejo JC, Zarazaga A, Lopez-Martinez J, Blesa AL, Celaya S, Conejero R, Galban C, Garcia De Lorenzo A, Grau T, Mesejo A, Ortiz-Leyba C, Planas M, Ordonez J, Jimenez FJ. Immunonutrition in critically ill patients. JPEN J Parenter Enteral Nutr. 2004;28:192–3; author reply 193-4. doi: 10.1177/0148607104028003192. [DOI] [PubMed] [Google Scholar]
- Castell L, Vance C, Abbott R, Marquez J, Eggleton P. Granule localization of glutaminase in human neutrophils and the consequence of glutamine utilization for neutrophil activity. J Biol Chem. 2004;279:13305–13310. doi: 10.1074/jbc.M309520200. [DOI] [PubMed] [Google Scholar]
- Moinard C, Caldefie-Chezet F, Walrand S, Vasson MP, Cynober L. Evidence that glutamine modulates respiratory burst in stressed rat polymorphonuclear cells through its metabolism into arginine. Br J Nutr. 2002;88:689–695. doi: 10.1079/BJN2002724. [DOI] [PubMed] [Google Scholar]
- Lagranha CJ, Senna SM, de Lima TM, Silva EP, Doi SQ, Curi R, Pithon-Curi TC. Beneficial effect of glutamine on exercise-induced apoptosis of rat neutrophils. Med Sci Sports Exerc. 2004;36:210–217. doi: 10.1249/01.MSS.0000113490.98089.B1. [DOI] [PubMed] [Google Scholar]
- Flaring UB, Rooyackers OE, Wernerman J, Hammarqvist F. Glutamine attenuates post-traumatic glutathione depletion in human muscle. Clin Sci (London) 2003;104:275–282. doi: 10.1042/CS20020198. [DOI] [PubMed] [Google Scholar]
- Tazuke Y, Wasa M, Shimizu Y, Wang HS, Okada A. Alanyl-glutamine-supplemented parenteral nutrition prevents intestinal ischemia-reperfusion injury in rats. JPEN J Parenter Enteral Nutr. 2003;27:110–115. doi: 10.1177/0148607103027002110. [DOI] [PubMed] [Google Scholar]
- Wischmeyer PE, Vanden Hoek TL, Li C, Shao Z, Ren H, Riehm J, Becker LB. Glutamine preserves cardiomyocyte viability and enhances recovery of contractile function after ischemia-reperfusion injury. JPEN J Parenter Enteral Nutr. 2003;27:116–122. doi: 10.1177/0148607103027002116. [DOI] [PubMed] [Google Scholar]
- Van Way Jr 3rd CW, Dhar A, Morrison DC, Longorio MA, Maxfield DM. Cellular energetics in hemorrhagic shock: restoring adenosine triphosphate to the cells. J Trauma. 2003;54 (Suppl.):S169–S176. doi: 10.1097/01.TA.0000047226.36678.EE. [DOI] [PubMed] [Google Scholar]
- Grimm H, Kraus A. Immunonutrition: supplementary amino acids and fatty acids ameliorate immune deficiency in critically ill patients. Langenbeck's Arch Surg. 2001;386:369–376. doi: 10.1007/s004230100241. [DOI] [PubMed] [Google Scholar]
- Alexander JW. Nutritional pharmacology in surgical patients. Am J Surg. 2002;183:349–352. doi: 10.1016/S0002-9610(02)00807-3. [DOI] [PubMed] [Google Scholar]
- Lee S, Gura KM, Kim S, Arsenault DA, Bistrian BR, Puder M. Current clinical applications of omega-6 and omega-3 fatty acids. Nutr Clin Pract. 2006;21:323–341. doi: 10.1177/0115426506021004323. [DOI] [PubMed] [Google Scholar]
- Calder PC. Long-chain n-3 fatty acids and inflammation: potential application in surgical and trauma patients. Braz J Med Biol Res. 2003;36:433–446. doi: 10.1590/S0100-879X2003000400004. [DOI] [PubMed] [Google Scholar]
- Calder PC. n-3 fatty acids, inflammation, and immunity: relevance to postsurgical and critically ill patients. Lipids. 2004;39:1147–1161. doi: 10.1007/s11745-004-1342-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biolo G, Grimble G, Preiser JC, Leverve X, Jolliet P, Planas M, Roth E, Wernerman J, Pichard C. Position paper of the ESICM Working Group on Nutrition and Metabolism. Metabolic basis of nutrition in intensive care unit patients: ten critical questions. Intensive Care Med. 2002;28:1512–1520. doi: 10.1007/s00134-002-1512-2. [DOI] [PubMed] [Google Scholar]
- Hammarqvist F, Sandgren A, Andersson K, Essen P, McNurlan MA, Garlick PJ. Growth hormone together with glutamine-containing total parenteral nutrition maintains muscle glutamine levels and results in a less negative nitrogen balance after surgical trauma. Surgery. 2001;129:576–586. doi: 10.1067/msy.2001.112593. [DOI] [PubMed] [Google Scholar]
- Petersen SR, Holaday NJ, Jeevanandam M. Enhancement of protein synthesis efficiency in parenterally fed trauma victims by adjuvant recombinant human growth hormone. J Trauma. 1994;36:726–733. doi: 10.1097/00005373-199405000-00022. [DOI] [PubMed] [Google Scholar]
- Montejo JC, Zarazaga A, Lopez-Martinez J, Urrutia G, Roque M, Blesa AL, Celaya S, Conejero R, Galban C, Garcia de Lorenzo A, Grau T, Mesejo A, Ortiz-Leyba C, Planas M, Ordonez J, Jimenez FJ. Immunonutrition in the intensive care unit. A systematic review and consensus statement. Clin Nutr. 2003;22:221–233. doi: 10.1016/S0261-5614(03)00007-4. [DOI] [PubMed] [Google Scholar]
- Sacks GS, Genton L, Kudsk KA. Controversy of immunonutrition for surgical critical-illness patients. Curr Opin Crit Care. 2003;9:300–305. doi: 10.1097/00075198-200308000-00008. [DOI] [PubMed] [Google Scholar]
- McCowen KC, Bistrian BR. Immunonutrition: problematic or problem solving? Am J Clin Nutr. 2003;77:764–770. doi: 10.1093/ajcn/77.4.764. [DOI] [PubMed] [Google Scholar]
- Holmes CL. Vasoactive drugs in the intensive care unit. Curr Opin Crit Care. 2005;11:413–417. doi: 10.1097/01.ccx.0000176696.70013.da. [DOI] [PubMed] [Google Scholar]
- Cotton BA, Guy JS, Morris JAJ, Abumrad NN. The cellular, metabolic, and systemic consequences of aggressive fluid resuscitation strategies. Shock. 2006;26:115–121. doi: 10.1097/01.shk.0000209564.84822.f2. [DOI] [PubMed] [Google Scholar]
- Peter JV, Moran JL, Phillips-Hughes J. A metaanlysis of treatment outcomes of early enteral versus early parenteral nutrition in hospitalized patients. Crit Care Med. 2005;33:213–220. doi: 10.1097/01.CCM.0000150960.36228.C0. [DOI] [PubMed] [Google Scholar]
- Heyland DK, Dhaliwal R. Early enteral nutrition vs. early parenteral nutrition: an irrelevant question for the critically ill? Crit Care Med. 2005;33:260–261. doi: 10.1097/01.CCM.0000150749.13940.37. [DOI] [PubMed] [Google Scholar]
- Martindale R, Miles J. Is immunonutrition ready for prime time? Two points of view. Nutr Clin Pract. 2003;18:489–496. doi: 10.1177/0115426503018006489. [DOI] [PubMed] [Google Scholar]
- Borlase BC, Moore EE, Moore FA. The abdominal trauma index; a critical reassessment and validation. J Trauma. 1990;30:1340–1344. doi: 10.1097/00005373-199011000-00006. [DOI] [PubMed] [Google Scholar]
- Moore FA, Moore EE. The benefits of enteric feeding. Adv Surg. 1996;30:141–154. [PubMed] [Google Scholar]
- Melis M, Fichera A, Ferguson MK. Bowel necrosis associated with early jejunal tube feeding: a complication of postoperative enteral nutrition . Arch Surg. 2006;141:701–704. doi: 10.1001/archsurg.141.7.701. [DOI] [PubMed] [Google Scholar]
- Zaloga GP. Bedside method for placing small bowel feeding tubes in critically ill patients. A prospective study. Chest. 1991;100:1643–1646. doi: 10.1378/chest.100.6.1643. [DOI] [PubMed] [Google Scholar]
- Bower RH, Cerra FB, Bershadsky B, Licari JJ, Hoyt DB, Jensen GL, van Buren CT, Rothkopf MM, Daly JM, Adelsberg BR. Early enteral administration of a formula (Impact) supplemented with arginine, nucleotides, and fish oil in intensive care unit patients: results of a multicenter, prospective, randomized, clinical trial. Crit Care Med. 1995;23:436–449. doi: 10.1097/00003246-199503000-00006. [DOI] [PubMed] [Google Scholar]
- Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet P, Kazandjiev G, Nitenberg G, van den Berghe G, Wernerman J, Ebner C, Hartl W, Heymann C, Spies C. ESPEN Guidelines on Enteral Nutrition: Intensive care . Clin Nutr. 2006;25:210–223. doi: 10.1016/j.clnu.2006.01.021. [DOI] [PubMed] [Google Scholar]
- Mansell PI, Macdonald IA. Reappraisal of the Weir equation for calculation of metabolic rate. Am J Physiol. 1990;258:R1347–R1354. doi: 10.1152/ajpregu.1990.258.6.R1347. [DOI] [PubMed] [Google Scholar]
- Miles JM. Energy expenditure in hospitalized patients: implications for nutritional support. Mayo Clin Proc. 2006;81:809–816. doi: 10.4065/81.6.809. [DOI] [PubMed] [Google Scholar]
- Baudouin SV, Evans TW. Nutritional support in critical care. Clin Chest Med. 2003;24:633–644. doi: 10.1016/S0272-5231(03)00101-1. [DOI] [PubMed] [Google Scholar]
- Reid C. Frequency of under- and overfeeding in mechanically ventilated ICU patients: causes and possible consequences. J Hum Nutr Diet. 2006;19:13–22. doi: 10.1111/j.1365-277X.2006.00661.x. [DOI] [PubMed] [Google Scholar]
- Dickerson RN, Rosato EF, Mullen JL. Net protein anabolism with hypocaloric parenteral nutrition in obese stressed patients. Am J Clin Nutr. 1986;44:747–755. doi: 10.1093/ajcn/44.6.747. [DOI] [PubMed] [Google Scholar]
- Burge JC, Goon A, Choban PS, Flancbaum L. Efficacy of hypocaloric total parenteral nutrition in hospitalized obese patients: a prospective, double-blind randomized trial. J Parenter Enteral Nutr. 1994;18:203–207. doi: 10.1177/0148607194018003203. [DOI] [PubMed] [Google Scholar]
- Dickerson RN, Boschert KJ, Kudsk KA, Brown RO. Hypocaloric enteral tube feeding in critically ill obese patients. Nutrition. 2002;18:241–246. doi: 10.1016/S0899-9007(01)00793-6. [DOI] [PubMed] [Google Scholar]
- Trahan K, Gore DC. Nutritional support. Chest Surg Clin N Am. 2002;12:227–249. doi: 10.1016/S1052-3359(02)00009-1. [DOI] [PubMed] [Google Scholar]
- Fuhrman MP, Winkler M, Biesemeier C. The American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) standards of practice for nutrition support dietitians. J Am Diet Assoc. 2001;101:825–832. doi: 10.1016/S0002-8223(01)00203-6. [DOI] [PubMed] [Google Scholar]
- Heyland DK, Dhaliwal R, Drover JW, Gramlich L, Dodek P. Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients. J Parenter Enteral Nutr. 2003;27:355–373. doi: 10.1177/0148607103027005355. [DOI] [PubMed] [Google Scholar]
- Wernerman J. Guidelines for nutritional support in intensive care unit patients: a critical analysis. Curr Opin Clin Nutr Metab Care. 2005;8:871–875. doi: 10.1097/00075197-200503000-00011. [DOI] [PubMed] [Google Scholar]