Abstract
Daptomycin is a novel cyclic lipopeptide that is approved by the U.S. Food and Drug Administration for the treatment of complicated skin and skin structure infections associated with Staphylococcus aureus and other gram-positive pathogens and also staphylococcal bacteremia, including right-sided endocarditis. The Clinical and Laboratory Standards Institute (CLSI) established “susceptible-only” interpretive criteria for broth microdilution (BMD) and disk diffusion (DD) testing of daptomycin in 2005. However, a series of S. aureus isolates have been recovered with daptomycin MICs in the nonsusceptible range (i.e., MICs of >1 μg/ml). The objective of this study was to determine the ability of the Etest and DD methods to differentiate daptomycin-susceptible from nonsusceptible isolates of S. aureus compared to the results of the CLSI BMD reference method. There was a good correlation between Etest MIC results and the results of BMD among laboratories (r = 0.86 to 0.88), with 95.3% of the Etest MICs within a ±1 log2 dilution of the BMD MIC result. A total of 92 of 102 (90.2%) non-daptomycin-susceptible isolates of S. aureus identified by BMD in two participating laboratories were also classified as nonsusceptible by Etest. However, the very major and major error rates reported by one of the participating laboratories were 13.5 and 4.0%, respectively, primarily due to the absence of an intermediate category. The DD method, however, did not reliably differentiate daptomycin-susceptible from non-daptomycin-susceptible isolates. In 2005, daptomycin disks were voluntarily removed from the market by Cubist Pharmaceuticals. The disk diffusion breakpoints were subsequently removed from the CLSI M100 standard in 2006.
Methicillin-resistant Staphylococcus aureus (MRSA) infections have become increasingly challenging for clinicians to treat since these isolates are often resistant to multiple antimicrobial agents, including, in limited cases, vancomycin (3, 7, 10, 35). In recent years, several new antimicrobial agents, including linezolid, quinupristin-dalfopristin, and daptomycin (6, 8, 31, 33), have been marketed for treating serious gram-positive infections. Daptomycin is a novel, cyclic lipopeptide antimicrobial agent that is approved by the U.S. Food and Drug Administration (FDA) for the treatment of complicated skin and skin structure infections associated with S. aureus, including MRSA, and other gram-positive pathogens (1, 20, 33), and bacteremia, including right-sided endocarditis, for both methicillin-susceptible and methicillin-resistant S. aureus. The activity of daptomycin against a variety of gram-positive pathogens has been documented over several years in a number of large surveillance studies conducted in North America, Europe, and the Far East (2, 9, 15, 18, 26, 34, 36).
The concentration-dependent bactericidal activity of daptomycin requires physiological levels of free calcium ions (50 μg/ml) (28, 33). Similar levels of calcium also are required to achieve accurate in vitro antimicrobial susceptibility testing results (2, 12, 30). This poses a challenge for in vitro agar-based susceptibility tests, since commercially available Mueller-Hinton agar plates used for disk diffusion tests vary in calcium concentration among manufacturers and from lot to lot of media (2, 12, 32). The Clinical and Laboratory Standards Institute (CLSI) sets cation standards for Mueller-Hinton broth but does not set standards for Mueller-Hinton agar. Early studies with daptomycin Etest strips (AB Biodisk, Solna, Sweden) by Fuchs et al. documented the pronounced effect of various calcium concentrations on MIC results (13). However, the results in that study indicated that Mueller-Hinton agar containing >20 μg of calcium/ml generally yielded Etest MIC results within 1 log2 dilution of the MICs obtained using the broth microdilution method. Subsequently, dual-component daptomycin Etest strips were developed that incorporate a constant and optimal level of Ca2+ within the daptomycin gradient enabling the use of standard Mueller-Hinton agar plates (Etest daptomycin package insert; AB Biodisk, Solna, Sweden). Studies comparing the MIC results between the revised Etest method and the results of broth microdilution testing for enterococci and staphylococci have been reported recently (17, 19; A. A. Bolmstrom, A. Engelhardt, A. Karlsson, P. Ho, K. Mills, A. Wanger, and R. Howe, Abstr. 105th Gen. Meet. Am. Soc. Microbiol. 2005, abstr. C317, 2005; L. M. Koeth and J. M. Difranco, Abstr. 45th Intersci. Conf. Antimicrob. Agents Chemother., abstr. D-1641, 2005). The Etest MIC results from these studies were comparable for staphylococci and enterococci, with most results being within 1 log2 dilution of the broth microdilution MICs.
Recently, there have been reports of daptomycin treatment failure among several patients with MRSA or enterococcal infections who were treated with prolonged courses of daptomycin (14, 21, 22, 27). A report by Hayden et al. (14) noted that the zones of inhibition for two MRSA isolates around daptomycin disks remained in the susceptible range (17 to 24 mm; susceptible breakpoint, ≥16 mm) even though the daptomycin MICs for the posttreatment isolates were nonsusceptible (4 μg/ml; susceptible breakpoint, ≤1 μg/ml). These investigators (14) and Sabol et al. (27) expressed concern that the disk diffusion method may not detect non-daptomycin-susceptible strains of staphylococci and enterococci, respectively. On the other hand, a report by Mangili et al. (21) of another daptomycin treatment failure notes that the previously daptomycin-susceptible isolates of MRSA recovered from positive blood cultures after daptomycin therapy yielded nonsusceptible results by both disk diffusion (daptomycin zone diameter = 14 mm) and broth microdilution (MIC = 2 μg/ml). That report indicated that at least some non-daptomycin-susceptible isolates are detected by the disk diffusion method.
Previous studies on the activity of daptomycin against multidrug-resistant isolates of staphylococci and enterococci included a series of isolates for which the daptomycin MICs were in the nonsusceptible range (16). This, in conjunction with the reports noted above, prompted us to study the ability of the disk diffusion and Etest susceptibility testing methods to detect isolates for which the daptomycin MICs were in the nonsusceptible range when tested by the broth microdilution reference method. We describe here a multicenter study focused on assessing the reproducibility of daptomycin MICs when tested with multiple lots of Mueller-Hinton broth and the ability of the Etest and disk diffusion testing methods to differentiate daptomycin-susceptible from non-daptomycin-susceptible isolates of S. aureus using multiple lots of Mueller-Hinton agar. Although non-daptomycin-susceptible isolates of enterococci and coagulase-negative staphylococci also have been described (16), relatively few such isolates were available to us at the time of the present study. Thus, we focused our attention on S. aureus isolates.
MATERIALS AND METHODS
Antimicrobial agents.
The daptomycin powder (lot 850753A) used for the present study was provided by Cubist Pharmaceuticals (Lexington, MA). The drug was dissolved and diluted in sterile water. A working stock solution of 1:10 was made by using cation-adjusted Mueller-Hinton broth (CA-MHB). Vancomycin was purchased from Sigma-Aldrich (St. Louis, MO). Sterile water was used as both the diluent and the solvent according to CLSI guidelines (4).
Isolate selection.
A total of 150 nonduplicate clinical isolates of S. aureus were selected for use in the present study. Thirty-two of the isolates demonstrated either elevated daptomycin MICs (≥2 μg/ml; range, 0.5 to 8 μg/ml) or elevated vancomycin MICs (≥4 μg/ml; range, ≤1 to ≥128 μg/ml); 24 showed elevated MICs to both antimicrobial agents. Both MRSA and methicillin-susceptible S. aureus (MSSA) were included in the study. Two vancomycin-resistant S. aureus isolates (vancomycin MICs of 1,024 and 64 μg/ml) from the Centers for Disease Control and Prevention (CDC; Atlanta, GA) were also included.
Of the 150 isolates, 62 were obtained from the culture collection of the CDC and Project ICARE, 23 of which were reported previously as nonsusceptible to daptomycin (MIC range, 2 to 8 μg/ml) (16). Thirteen isolates were obtained from the Network on Antimicrobial Resistance in Staphylococcus aureus administered by Focus Technologies (Herndon, VA). Finally, 75 isolates of daptomycin-susceptible S. aureus were included from the culture collection of the Clinical Microbiology Institute (CMI; Wilsonville, OR).
The following quality control (QC) organisms were tested by each laboratory on each day of testing: S. aureus ATCC 25923 (disk diffusion only), S. aureus ATCC 43300 (disk diffusion only), S. aureus ATCC 29213 (broth microdilution and Etest), and Enterococcus faecalis ATCC 29212 (broth microdilution only) (24, 25). In addition, a known vancomycin-intermediate isolate of S. aureus (QC278) was included in each testing run at the CMI.
Test panels and media.
Four sets of broth microdilution panels were prepared as described by the CLSI (24). CMI panels (prepared in house using CA-MHB [Difco lot 1110003]) contained the following serial twofold dilutions of antimicrobial agents: daptomycin, 0.12 to 128 μg/ml; oxacillin, 1 to 4 μg/ml; and vancomycin, 0.5 to 64 μg/ml. MIC panels prepared by the JMI Laboratories (North Liberty, Iowa) using CA-MHB from BBL had the same antimicrobial agent concentrations as the panels produced in house at the CMI. Panels prepared at TREK Diagnostics, Inc. (Cleveland, OH), contained serial twofold dilutions as follows: daptomycin, 0.03 to 32 μg/ml; oxacillin, 0.06 to 8 μg/ml; and vancomycin, 0.06 to 64 μg/ml. CDC MIC panels were prepared with CA-MHB from Difco (lot 2198184) contained the following dilution ranges: daptomycin, 0.5 to 16 μg/ml; oxacillin, 0.12 to 128 μg/ml; and vancomycin, 0.5 to 1,024 μg/ml. Daptomycin-containing microdilution wells in MIC panels prepared at the four study sites contained a final concentration of approximately 50 μg of calcium/ml. Additional antimicrobial agents were present on each of the MIC panels; however, the data from those antimicrobial agents were not analyzed for this study. For the Etest method, BBL Mueller-Hinton agar was used exclusively.
For disk diffusion tests, Mueller-Hinton agar media from three different manufacturers was used: BBL (lot # 4223273; Becton Dickinson, Franklin Lakes, NJ), Remel (lot 435212; Lenexa, KS), and Acumedia (lot 0402-123; Neogen Corp., Lexington, KY). The calcium concentrations of all broth and agar media were determined by using atomic absorption. The 150-mm plates were purchased from BBL, Remel, and Prepared Media Laboratories, respectively.
Broth microdilution.
All 150 isolates were tested in duplicate at the CMI by broth microdilution on two separate days using CMI and JMI Laboratories panels. A subset of 34 isolates was tested in duplicate at the CDC on two separate days using CDC in-house panels and TREK panels. All sites performed broth microdilution in accordance with CLSI guidelines (24).
Etest.
All 150 isolates were tested in duplicate at the CMI by the Etest method on two separate days using prepared agar media from BBL. At the CDC, the same subset of 34 isolates tested by broth microdilution was tested in duplicate by the Etest method on two separate days using prepared agar media from the same lot of BBL dehydrated base media as that used by the CMI. Daptomycin Etest strips with calcium supplementation were obtained from the manufacturer (AB Biodisk, Solna, Sweden) by both the CMI and the CDC. Etest procedures were performed according to manufacturer's guidelines. Etest MICs were rounded up to the next higher log2 dilution corresponding to broth microdilution MICs for the purposes of comparison and analysis.
Disk diffusion.
The CMI performed disk diffusion tests on the complete set of 150 isolates in triplicate on two separate days using media from three manufacturers (BBL, Remel, and Acumedia) and 30-μg daptomycin disks from two manufacturers (BBL and Oxoid [Remel]). The CDC performed disk diffusion tests on the subset of 34 isolates, which were also tested by broth microdilution and the Etest. Disk diffusion was performed in duplicate at the CDC using BBL media with 30-μg daptomycin disks obtained from BBL. The BBL dehydrated media and BBL disk lots used by the CDC were the same as those used by the CMI. Disk diffusion testing was performed in accordance with CLSI guidelines (25).
MBCs.
Minimum bactericidal concentrations (MBCs) for daptomycin and vancomycin were determined on the complete set of 150 isolates at the CMI according to methods outlined by the CLSI (23) using Mueller-Hinton broth (BBL). The MBC was defined as the lowest concentration of the antimicrobial agent that produced a ≥99.9% (e.g., ≥3 log10) drop in CFU/ml compared to the starting inoculum. The ratio of MBC to MIC was determined for each isolate.
Error rates.
Since there is no intermediate interpretive category defined for daptomycin, all categorical errors are either very major errors (false susceptibility, where nonsusceptible values are equated with resistance) or major errors (false nonsusceptibility).
RESULTS
Characterization of study isolates and comparison of broth microdilution results.
Tables 1 and 2 show the cumulative percentage of the 150 S. aureus isolates selected for the present study that were either inhibited (MIC) or killed (MBC) by daptomycin or vancomycin, respectively, using CMI and JMI Laboratories MIC panels. For daptomycin, the MIC and MBC ranges determined at CMI were both 0.25 to 8 μg/ml. The MIC at which 50% of the isolates are inhibited (MIC50) and MIC90 values for daptomycin using the CMI panels were 0.5 to 1.0 μg/ml (depending on the day of testing) and 2 μg/ml, respectively, whereas the MBC90 was 4 μg/ml. Similar MICs were obtained using the JMI Laboratories panels (Table 1). The MIC50 and MIC90 values for daptomycin for the subset of 34 isolates, which had a larger percentage of nonsusceptible isolates, tested at CDC and CMI using the CMI panels were 1.0 μg/ml and 2 to 4 μg/ml, respectively (data not shown). TREK panels tested at the CDC gave comparable MIC50 and MIC90 results. For vancomycin (Table 2), the MIC and MBC ranges were 0.5 to ≥128 μg/ml and 1 to ≥128 μg/ml, respectively. The vancomycin MIC50 and MIC90 values were 2 and 8 μg/ml for the CMI panels and 1 μg/ml and 4 to 8 μg/ml for the JMI Laboratories panels. The MBC90 for vancomycin was 64 μg/ml for the set of 150 isolates. Among these isolates, the vancomycin MICs were higher than usual for S. aureus isolates (typical vancomycin MIC90 = 1 to 2 μg/ml) (2, 12, 26, 32, 34). No significant differences (P > 0.05) were noted between the results from the two test sites when results were analyzed by the MIC panel used, the day of testing, the modal MIC, the MIC range, the MIC50, or the MIC90.
TABLE 1.
Cumulative percent of Staphylococcus aureus inhibited or killed by daptomycin
| MIC (μg/ml) | Daptomycin MIC
|
Daptomycin MBC (CMI)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Day 1 CMI panels
|
Day 2 CMI panels
|
Day 1 JMI panelsa
|
Day 2 JMI panelsa
|
|||||||
| MIC frequency | Cumulative % inhibited | MIC frequency | Cumulative % inhibited | MIC frequency | Cumulative % inhibited | MIC frequency | Cumulative % inhibited | MBC frequency | Cumulative % killed | |
| 0.06 | ||||||||||
| 0.12 | ||||||||||
| 0.25 | 1 | 1 | 2 | 1 | 28 | 19 | 27 | 19 | 1 | 1 |
| 0.5 | 79 | 53 | 72 | 49 | 65 | 64 | 61 | 61 | 38 | 26 |
| 1 | 34 | 76 | 38 | 75 | 36 | 89 | 37 | 87 | 56 | 63 |
| 2 | 25 | 93 | 28 | 93 | 11 | 97 | 12 | 95 | 32 | 85 |
| 4 | 10 | 99 | 9 | 99 | 5 | 100 | 7 | 100 | 15 | 95 |
| 8 | 1 | 100 | 1 | 100 | 8 | 100 | ||||
| 16 | ||||||||||
| 32 | ||||||||||
| 64 | ||||||||||
| ≥128 | ||||||||||
| Total | 150 | 100 | 150 | 100 | 145 | 100 | 144 | 100 | 150 | 100 |
Several MIC panels were not readable.
TABLE 2.
Cumulative percent of Staphylococcus aureus inhibited or killed by vancomycin
| MIC (μg/ml) | Vancomycin MIC
|
Vancomycin MBC (CMI)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Day 1 CMI panels
|
Day 2 CMI panels
|
Day 1 JMI panelsa
|
Day 2 JMI panelsa
|
|||||||
| MIC frequency | Cumulative % inhibited | MIC frequency | Cumulative % inhibited | MIC frequency | Cumulative % inhibited | MIC frequency | Cumulative % inhibited | MBC frequency | Cumulative % killed 0.016 | |
| 0.06 | ||||||||||
| 0.12 | ||||||||||
| 0.25 | ||||||||||
| 0.5 | 1 | 1 | 2 | 1 | ||||||
| 1 | 70 | 47 | 67 | 45 | 78 | 54 | 74 | 51 | 65 | 43 |
| 2 | 25 | 63 | 33 | 67 | 15 | 65 | 19 | 64 | 26 | 61 |
| 4 | 34 | 86 | 30 | 87 | 36 | 90 | 31 | 85 | 24 | 77 |
| 8 | 19 | 99 | 18 | 99 | 13 | 99 | 18 | 97 | 10 | 83 |
| 16 | 2 | 100 | 2 | 99 | 3 | 85 | ||||
| 32 | 1 | 99 | 4 | 88 | ||||||
| 64 | 1 | 99 | 1 | 99 | 6 | 92 | ||||
| ≥128 | 1 | 100 | 1 | 100 | 1 | 100 | 1 | 100 | 12 | 100 |
| Totals | 150 | 100 | 150 | 100 | 146 | 100 | 148 | 100 | 150 | 100 |
Several MIC panels were not readable.
Atomic absorption assays were used to assess the calcium concentration of the daptomycin-containing wells for the plates prepared at the CMI, JMI Laboratories, and the CDC. The calcium ion concentrations of the MIC panels prepared at the CMI and JMI Laboratories were all 50 μg/ml, whereas the CDC MIC panels had slightly lower calcium concentrations (range, 41 to 42 μg/ml). The calcium concentrations of panels prepared at TREK were not available for testing, but all daptomycin quality control results for these panels were all within the acceptable ranges (4).
Etest evaluation.
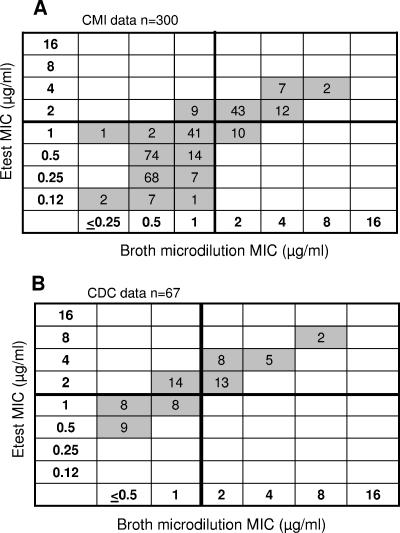
There was good agreement among the day-to-day and institution-to-institution daptomycin MICs obtained with the Etest method and those obtained by broth microdilution for the full set of 150 isolates tested in duplicate at the CMI (correlation coefficient [r] = 0.86; Fig. 1A) and the subset of 34 isolates tested in duplicate at the CDC (r = 0.88; Fig. 1B) and the CMI. The comparisons at lower MICs were limited since the CDC MIC panels did not evaluate daptomycin concentrations of <0.5 μg/ml. Testing performed at the CMI yielded daptomycin Etest MIC50 and MIC90 values corresponding to those obtained by broth microdilution (i.e., MIC50 = 1 μg/ml; MIC90 = 2 μg/ml). At the CMI, 94.7% of the Etest MICs were within ±1 log2 dilution of the broth microdilution values, although the Etest MICs tended to be lower. For example, 35.3% of the MICs were 1 log2 dilution lower, and 5.0% were 2 or 3 log2 dilutions lower. At the CDC, among the subsets of broth microdilution MICs of ≥1 μg/ml (i.e., on-scale values), 22 of 40 (55%) of the Etest values were 1 log2 dilution higher than those observed with broth microdilution; none were lower.
FIG. 1.
(A) Comparison of daptomycin Etest MIC results obtained for 150 isolates of S. aureus tested in duplicate at the CMI and MIC results generated by broth microdilution reference method (n = 300). (B) Comparison of Etest and broth microdilution MIC results for 34 S. aureus isolates tested in duplicate at the CDC. One MIC test at the CDC was not readable (n = 67). The susceptible breakpoints for daptomycin are ≤1 μg/ml for MIC testing.
Using the CMI data set (n = 300), 10 of 74 isolates reported as nonsusceptible by broth microdilution were reported as susceptible by Etest for a very major error rate of 13.5%, and 9 of 226 isolates reported as susceptible based on broth microdilution isolates were reported as nonsusceptible by the Etest for a major error rate of 4.0%. On the other hand, CDC Etest results (which examined a set of isolates that was biased toward non-daptomycin-susceptible organisms) produced a major error rate of 35.9% but no very major errors were observed. A review of the quality control data from the CMI and CDC showed that all quality control results were within the ranges defined by CLSI. There was no demonstrable trend toward higher or lower MICs in either the CMI or the CDC data set.
Disk diffusion results.
There was a high level of agreement between the zone diameters produced by BBL and Oxoid disks for the 150 study isolates tested at the CMI; 99.3% of the zone diameter values were within a ±3-mm range (data not shown). There was also >99% agreement among the zone diameters observed on BBL, Remel, and Acumedia Mueller-Hinton agar (data not shown), demonstrating the overall reproducibility of the method. The calcium ion concentrations of the Mueller-Hinton agar lots used for disk diffusion ranged from 22 to 26 μg/ml, which is considered acceptable for the daptomycin Etest method (Etest package insert) and is typical of BBL lots of Mueller-Hinton agar (data not shown).
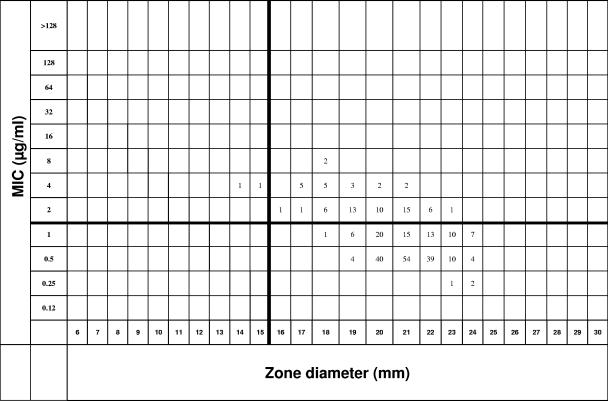
Since there is no intermediate MIC range for daptomycin, all of the categorical errors observed in the present study were defined as very major errors (nonsusceptible values were equated with resistance). The very major error rate obtained at the CMI for daptomycin when comparing the categorical interpretation results for broth microdilution (using CMI panels) and disk diffusion was 24% for the set of 150 isolates. A scattergram of the CMI data showing the comparison of disk diffusion zone diameters to broth microdilution MICs is presented in Fig. 2. Additional tests comparing broth microdilution MICs and disk diffusion zones performed at CMI using a variety of media (BBL, Remel, and Acumedia) and disks (BBL and Oxoid) yielded very major rates ranging from 24 to 25%. Comparisons of the daptomycin MIC interpretations using JMI Laboratories MIC panels versus the interpretations for disk diffusion (BBL media and BBL disks), yielded a very major error rate of only 13%, since the MICs tended to be 1 log2 dilution lower but with essentially the same MIC50 and MIC90 values.
FIG. 2.
Scattergram of daptomycin MIC results (in μg/ml) from CMI-prepared panels and daptomycin zone diameter results (using BBL disks, BBL agar media) for 150 isolates of S. aureus tested in duplicate at CMI. The susceptible breakpoints for daptomycin are ≤1 μg/ml for MIC testing and ≥16 mm for disk diffusion (indicated by horizontal and vertical lines). Values above the MIC breakpoint or smaller than the disk diffusion breakpoint are interpreted as nonsusceptible (4).
DISCUSSION
Interpretive criteria for daptomycin testing for both broth microdilution and disk diffusion testing were approved by the FDA in 2004 and published by the CLSI in 2005 (4). Previous studies indicated that isolates of S. aureus for which the daptomycin MICs were in the nonsusceptible range (i.e., MICs of >1 μg/ml) were appearing in the United States (16). Preliminary studies suggested that these isolates were not detected as nonsusceptible by disk diffusion. Thus, we undertook the present study to assess the accuracy of both the Etest and the disk diffusion methods to differentiate daptomycin-susceptible from nonsusceptible isolates of S. aureus.
Since the calcium concentration of the media has a critical impact on testing (2, 12, 30), we compared the reproducibility of several batches of MIC panels prepared in different locations. Essential agreement and day-to-day reproducibility was high among the MIC panels produced by the four institutions (CDC, CMI, JMI Laboratories, and TREK); however, the panels produced by JMI Laboratories tended to produce slightly lower MICs compared to the other three MIC panels, despite having 50 μg of calcium/ml per well. This suggests that factors other than the calcium concentration may also influence daptomycin testing results.
Early daptomycin Etest studies by Fuchs et al. noted the pronounced effect of the calcium concentration of the media on the MIC results (13). More recent daptomycin Etest strips have calcium incorporated in the gradient (19; Bolmstrom et al., Abstr. 105th Gen. Meet. Am. Soc. Microbiol. 2005), although the exact concentration of calcium present is proprietary. In our study, the Etest method performed well in differentiating daptomycin-susceptible from non-daptomycin-susceptible isolates compared to the results of the broth microdilution reference method. Approximately 95% of the values observed with the Etest were within ±1 log2 dilution of the broth microdilution results; although within the susceptible range still, 5% of the Etest results were two or three doubling dilutions lower than the broth microdilution results. A total of 92 of 102 (90.2%) isolates reported to be daptomycin nonsusceptible by broth microdilution were similarly classified as nonsusceptible by the Etest. However, due to the lack of an intermediate category, the very major error rate in the CMI data set was high (13.5%). The major error rate observed at the CDC was even higher (35.9%). The high percentage of very major and major errors can be attributed in part to (i) the absence of an intermediate range for daptomycin, (ii) the fact that the strains tested were selected to contain a very high percentage of isolates with elevated MICs to daptomycin, and (iii) the fact that the population of strains tested at the CDC was small (34 isolates). Surveillance studies have indicated that nonsusceptible values would normally represent ≤1% of the total isolates seen. Interestingly, the CMI Etest values tended to be 1 log2 dilution lower than broth microdilution MICs, but in the CDC data set the values tended to be 1 log2 dilution higher. This may reflect lot-to-lot variation in calcium levels or perhaps reader-to-reader variation in interpreting the Etest results. Although none of the participants that read the Etest results reported difficulty in interpreting the Etest ellipses, no efforts were made to standardize reading prior to initiating the study. This may be a source of variability that deserves additional study.
The results of disk diffusion testing were disappointing. Disk diffusion did not consistently identify isolates of S. aureus for which the daptomycin MICs were >1 μg/ml, even though the calcium concentrations of the agar used were >20 μg/ml (12). Based in part on these data, the daptomycin disk test was withdrawn from the market in early 2005. However, using the Etest results as a model, it may be possible in the future to incorporate calcium into the daptomycin disk, much like glucose-6-phosphate has been incorporated in fosfomycin disks, to allow accurate disk diffusion testing (4). Until such disks can be manufactured and evaluated, clinical laboratories will have to use the broth microdilution reference method, the Etest, or the JustOne method (TREK) (19) or an alternate MIC method to assess the susceptibility of S. aureus isolates to daptomycin. Daptomycin testing using several automated susceptibility testing methods has been cleared recently by the U.S. FDA (R. Rennie, C. Brosnikoff, S. Shokoples, L. Turnbull, S. Mirrett, L. B. Reller, P. C. Iwen, R. K. Noel, M. Bacsafra, S. Connell, J. Johnston, and B. Zimmer, 15th Eur. Cong. Clin. Microbiol. Infect. Dis., abstr. P-1883, 2005; S. Messina-Powell, D. Pyse, K. Englehard, J. Moore, J. Slaughter, R. Griffith, A. Doan, and M. Ullery, Abstr. 105th Gen. Meet. Am. Soc. Microbiol. 2005, abstr. C-005, 2005), although the panels are not yet widely available.
Finally, the vancomycin MIC50 and MIC90 values of the non-daptomycin-susceptible isolates used in the present study were clearly above the values normally observed for S. aureus (2, 12, 26, 32, 34). In a previous report (16), we suggested the possible linkage of reduced susceptibility to vancomycin and nonsusceptibility of organisms to daptomycin. However, not all S. aureus isolates with reduced susceptibility to vancomycin showed a similar decrease in susceptibility to daptomycin. While 24 of the 150 study isolates showed decreased susceptibility to both drugs, 7 showed deceased susceptibility to vancomycin only, and 1 showed deceased susceptibility to daptomycin only. The mechanism of the purported linkage between reduced susceptibility to both drugs is unclear at this time. However, recent studies suggest that the thickened cell walls (5) characteristic of S. aureus strains with reduced susceptibility to vancomycin, the metabolic changes that accompany the formation of thickened cell walls (29), and mutations in the mprF and yycG loci (11) may play a role in reduced susceptibility to daptomycin. Thus, clinical microbiologists and infectious disease clinicians should be aware that isolates of S. aureus that show reduced susceptibility to vancomycin may demonstrate reduced susceptibility to daptomycin as well.
Acknowledgments
The findings and conclusions presented here are those of the authors and do not necessarily represent the views of the funding agency. The use of trade names in this study is for identification purposes only and does not constitute endorsement by the Public Health Service or the U.S. Department of Health and Human Services.
We thank David Lonsway and Jana Swenson for helpful discussions.
This study was supported by Cubist Pharmaceuticals, Inc. Phase 5 of Project ICARE is supported in part by unrestricted grants to the Rollins School of Public Health of Emory University by Astra-Zeneca Pharmaceuticals, Wilmington, DE; bioMérieux, Inc., Durham, NC; Elan Pharmaceuticals, San Diego, CA; and Pfizer Inc., New York, NY.
REFERENCES
- 1.Arbeit, R. D., D. Maki, F. P. Tally, E. Campanaro, B. I. Eisenstein, and the Daptomycin 98-01 and 99-01 Investigations. 2004. The safety and efficacy of daptomycin for the treatment of complicated skin and skin-structure infections. Clin. Infect. Dis. 38:1673-1681. [DOI] [PubMed] [Google Scholar]
- 2.Barry, A. L., P. C. Fuchs, and S. D. Brown. 2001. In vitro activities of daptomycin against 2,789 clinical isolates from 11 North American medical centers. Antimicrob. Agents Chemother. 45:1919-1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chambers, H. 2001. The changing epidemiology of Staphylococcus aureus? Emerg. Infect. Dis. 7:178-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clinical and Laboratory Standards Institute. 2005. Performance standards for antimicrobial susceptibility testing; CLSI approved standard M100-S16. Clinical and Laboratory Standards Institute, Wayne, Pa.
- 5.Cui, L., E. Tominaga, H.-M. Neoh, and K. Hiramatsu. 2006. Correlation between reduced daptomycin susceptibility and vancomycin resistance in vancomycin-intermediate Staphylococcus aureus. Antimicrob. Agents Chemother. 50:1079-1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cunha, B. A. 2005. Methicillin-resistant Staphylococcus aureus: clinical manifestations and antimicrobial therapy. Clin. Microbiol. Infect. 11:33-42. [DOI] [PubMed] [Google Scholar]
- 7.Deresinski, S. 2005. Methicillin-resistant Staphylococcus aureus: an evolutionary, epidemiologic, and therapeutic odyssey. Clin. Infect. Dis. 40:526-573. [DOI] [PubMed] [Google Scholar]
- 8.Eliopoulos, G. M. 2003. Quinupristin-dalfopristin and linezolid: evidence and opinion. Clin. Infect. Dis. 36:473-481. [DOI] [PubMed] [Google Scholar]
- 9.Fluit, A. C., F. Schmitz, J. Verhoef, and D. Milatovic. 2004. In vitro activity of daptomycin against gram-positive European clinical isolates with defined resistance determinants. Antimicrob. Agents Chemother. 48:1007-1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fridkin, S. K. 2001. Vancomycin-intermediate and -resistant Staphylococcus aureus: what the infectious disease specialist needs to know. Clin. Infect. Dis. 32:108-115. [DOI] [PubMed] [Google Scholar]
- 11.Friedman, L., J. D. Alder, and J. A. Silverman. 2006. Genetic changes that correlate with reduced susceptibility to daptomycin in Staphylococcus aureus. Antimicrob. Agents Chemother. 50:2137-2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fuchs, P. C., A. L. Barry, and S. D. Brown. 2000. Daptomycin susceptibility tests: interpretive criteria, quality control, and effect of calcium on in vitro tests. Diagn. Microbiol. Infect. Dis. 38:51-58. [DOI] [PubMed] [Google Scholar]
- 13.Fuchs, P. C., A. L. Barry, and S. D. Brown. 2001. Evaluation of daptomycin susceptibility testing by Etest and the effect of different batches of media. J. Antimicrob. Chemother. 48:557-561. [DOI] [PubMed] [Google Scholar]
- 14.Hayden, M. K., K. Rezai, R. A. Hayes, K. Lolans, J. P. Quinn, and R. A. Weinstein. 2005. Development of daptomycin resistance in vivo in methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 43:5285-5287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsueh, P., W. H. Chen, L. J. Teng, and K. T. Luh. 2005. Nosocomial infections due to methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci at a university hospital in Taiwan from 1991 to 2003: resistance trends, antibiotic usage and in vitro activities of newer antimicrobial agents. Int. J. Antimicrob. Agents 26:43-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jevitt, L. A., A. J. Smith, P. P. Williams, P. M. Raney, J. E. McGowan, Jr., and F. C. Tenover. 2003. In vitro activities of daptomycin, linezolid, and quinupristin-dalfopristin against a challenge panel of staphylococci and enterococci, including vancomycin-intermediate Staphylococcus aureus and vancomycin-resistant Enterococcus faecium. Microb. Drug Resist. 9:298-306. [DOI] [PubMed] [Google Scholar]
- 17.Johnson, A. P., S. Mushtaq, M. Warner, and D. M. Livermore. 2004. Calcium-supplemented daptomycin Etest strips for susceptibility testing on Iso-Sensitest agar. J. Antimicrob. Chemother. 53:860-862. [DOI] [PubMed] [Google Scholar]
- 18.Johnson, A. P., S. Mushtaq, M. Warner, and D. M. Livermore. 2004. Activity of daptomycin against multi-resistant gram-positive bacteria including enterococci and Staphylococcus aureus resistant to linezolid. Int. J. Antimicrob. Agents 24:315-319. [DOI] [PubMed] [Google Scholar]
- 19.Jorgensen, J. H., and S. A. Crawford. 2006. Assessment of two commercial susceptibility test methods for determinant of daptomycin MICs. J. Clin. Microbiol. 44:2126-2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lipsky, B. A., and U. Stoutenburgh. 2005. Daptomycin for treating infected diabetic foot ulcers: evidence from a randomized, controlled trial comparing daptomycin with vancomycin or semi-synthetic penicillins for complicated skin and skin-structure infections. J. Antimicrob. Chemother. 55:240-245. [DOI] [PubMed] [Google Scholar]
- 21.Mangili, A., I. Bica, D. R. Snydman, and D. H. Hamer. 2005. Daptomycin-resistant, methicillin-resistant Staphylococcus aureus bacteremia. Clin. Infect. Dis. 40:1058-1060. [DOI] [PubMed] [Google Scholar]
- 22.Munoz-Price, L. S., K. Lolans, and J. P. Quinn. 2005. Emergence of resistance to daptomycin during treatment of vancomycin-resistant Enterococcus faecalis infection. Clin. Infect. Dis. 41:565-566. [DOI] [PubMed] [Google Scholar]
- 23.National Committee for Clinical Laboratory Standards. 1999. Methods for determining bactericidal activity of antimicrobial agent. Approved guideline M26-A, vol. 19, no. 18. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 24.National Committee for Clinical Laboratory Standards. 2003. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A6. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 25.National Committee for Clinical Laboratory Standards. 2003. Performance standards for antimicrobial disk susceptibility tests. Approved standard M2-A8. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 26.Rybak, M. J., E. Hershberger, T. Moldovan, and R. G. Grucz. 2000. In vitro activities of daptomycin, vancomycin, linezolid, and quinupristin-dalfopristin against staphylococci and enterococci, including vancomycin-intermediate and -resistant strains. Antimicrob. Agents Chemother. 44:1062-1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sabol, K., J. E. Patterson, J. S. Lewis II, A. Owens, J. Cadena, and J. H. Jorgensen. 2005. Emergence of daptomycin resistance in Enterococcus faecium during daptomycin therapy. Antimicrob. Agents Chemother. 49:1664-1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Safdar, N., D. Andes, and W. A. Craig. 2004. In vivo pharmacodynamic activity of daptomycin. Antimicrob. Agents Chemother. 48:63-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sakoulas, G., J. Alder, C. Thauvin-Eliopoulos, R. C. Moellering, Jr., and G. Eliopoulos. 2006. Induction of daptomycin heterogeneous susceptibility in Staphylococcus aureus by exposure to vancomycin. Antimicrob. Agents Chemother. 50:1581-1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Silverman, J. A., N. Oliver, T. Andrew, and T. Li. 2001. Resistance studies with daptomycin. Antimicrob. Agents Chemother. 45:1799-1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith, P. F., B. M. Booker, A. B. Ogundele, and P. Kelchin. 2005. Comparative in vitro activities of daptomycin, linezolid, and quinupristin/dalfopristin against gram-positive bacterial isolates from a large cancer center. Diagn. Microbiol. Infect. Dis. 52:255-259. [DOI] [PubMed] [Google Scholar]
- 32.Snydman, D. R., N. V. Jacobus, L. A. McDermott, J. R. Lonks, and J. M. Boyce. 2000. Comparative in vitro activities of daptomycin and vancomycin against resistant gram-positive pathogens. Antimicrob. Agents Chemother. 44:3447-3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steenbergen, J. N., J. Alder, G. M. Thorne, and F. P. Tally. 2005. Daptomycin: a lipopeptide antibiotic for the treatment of serious gram-positive infections. J. Antimicrob. Chemother. 55:283-288. [DOI] [PubMed] [Google Scholar]
- 34.Streit, J. M., R. N. Jones, and H. S. Sader. 2004. Daptomycin activity and spectrum: a worldwide sample of 6737 clinical gram-positive organisms. J. Antimicrob. Chemother. 53:669-674. [DOI] [PubMed] [Google Scholar]
- 35.Tenover, F. C., L. M. Weigel, P. C. Appelbaum, L. K. McDougal, J. Chaitram, S. McAllister, N. Clark, G. Killgore, C. M. O'Hara, L. Jevitt, J. B. Patel, and B. Bozdogan. 2004. Characterization of a vancomycin-resistant clinical isolate of Staphylococcus aureus from Pennsylvania. Antimicrob. Agents Chemother. 48:275-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wise, R., J. M. Andrews, and J. P. Ashby. 2001. Activity of daptomycin against gram-positive pathogens: a comparison with other agents and the determination of a tentative breakpoint. J. Antimicrob. Chemother. 48:563-567. [DOI] [PubMed] [Google Scholar]